Published online Apr 18, 2016. doi: 10.5312/wjo.v7.i4.258
Peer-review started: May 11, 2015
First decision: July 27, 2015
Revised: December 10, 2015
Accepted: January 5, 2016
Article in press: January 7, 2016
Published online: April 18, 2016
Processing time: 338 Days and 20.2 Hours
AIM: To report ankle fracture configurations and bone quality following arthroscopic-assisted reduction and internal-fixation (ARIF) or open reduction and internal-fixation (ORIF).
METHODS: The patients of ARIF (n = 16) or ORIF (n = 29) to treat unstable ankle fracture between 2006 and 2014 were reviewed retrospectively. Baseline data, including age, sex, type of injury, immediate postoperative fracture configuration (assessed on X-rays and graded by widest gap and largest step-off of any intra-articular site), bone quality [assessed with bone mineral density (BMD) testing] and arthritic changes on X-rays following surgical treatments were recorded for each group.
RESULTS: Immediate-postoperative fracture configurations did not differ significantly between the ARIF and ORIF groups. There were anatomic alignments as 8 (50%) and 8 (27.6%) patients in ARIF and ORIF groups (P = 0.539) respectively. There were acceptable alignments as 12 (75%) and 17 (58.6%) patients in ARIF and ORIF groups (P = 0.341) respectively. The arthritic changes in follow-up period as at least 16 wk following the surgeries were shown as 6 (75%) and 10 (83.3%) patients in ARIF and ORIF groups (P = 0.300) respectively. Significantly more BMD tests were performed in patients aged > 60 years (P < 0.001), ARIF patients (P = 0.021), and female patients (P = 0.029). There was no significant difference in BMD test t scores between the two groups.
CONCLUSION: Ankle fracture configurations following surgeries are similar between ARIF and ORIF groups, suggesting that ARIF is not superior to ORIF in treatment of unstable ankle fractures.
Core tip: There was no significant difference between arthroscopic-assisted reduction and internal-fixation (ARIF) and open reduction and internal-fixation (ORIF) in immediate-postoperative ankle fracture configuration in the present study. Although the use of arthroscopy in orthopaedic trauma is increasing, the effectiveness of ARIF compared with that of ORIF in the management of ankle fractures has yet to be verified. The low rate of bone mineral density testing reflects a lack of awareness of the need for routine post-injury testing for osteoporosis in patients with ankle fractures.
- Citation: Angthong C. Ankle fracture configuration following treatment with and without arthroscopic-assisted reduction and fixation. World J Orthop 2016; 7(4): 258-264
- URL: https://www.wjgnet.com/2218-5836/full/v7/i4/258.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i4.258
Ankle arthroscopy, introduced into the field of ankle surgery for several years is a minimally invasive intra-articular treatment with several advantages[1,2]. Miyamoto et al[3] reported the benefit of arthroscopic examination in the diagnosis of syndesmotic disruption, which occurs mostly with ankle fracture. Imade et al[4] also demonstrated the advantages of arthroscopic procedures for ankle injury combined with Maisonneuve fracture, such as arthroscopic-assisted visualization during syndesmotic screw fixation, and drilling an osteochondral lesion of the talus. Takao et al[5] proposed the role of arthroscopic-assisted reduction and internal fixation for accurate diagnose and treat intra-articular disorders combined with distal fibular fractures. However, there are no reports of fracture configuration and bone quality in patients with unstable ankle fractures treated with arthroscopic-assisted reduction and internal fixation (ARIF) vs open reduction and internal fixation (ORIF).
To address this, the immediate-postoperative configurations of intra-articular ankle fractures, as well as bone quality via postoperative bone mineral density (BMD) testing, were investigated in a series of unstable ankle fractures treated with ARIF or ORIF. Relationships between relevant patient and technical variables and postoperative BMD were also determined. The study tested the hypothesis that there was no difference between ARIF and ORIF; the alternative, that ARIF is superior to ORIF in the treatment of unstable ankle fracture, would be demonstrated by associations between ARIF and superior anatomic fracture configuration. A second aim of the study was to determine the prevalence of post-injury BMD testing in order to evaluate clinicians’ level of awareness regarding the need for investigation of osteoporosis in patients with ankle fractures.
The medical records of patients who underwent fixation of unstable ankle fractures between April 2006 and October 2014 were reviewed retrospectively. After the exclusion of patients with incomplete or unavailable medical records or inadequate radiographic data, 45 ankle fractures in 45 patients [mean age, 46.5 years (range, 18-80 years)] were included in the study. ARIF (n = 16) or ORIF (n = 29) had been performed at the discretion of the attending surgeon. Thirty-three patients (73.3%) had a supination-type[6] ankle fracture and 12 (26.7%) had pronation-type[6] ankle fracture. Baseline data, including demographic information, and the rate of BMD testing, are presented in Table 1. This study was approved by the institutional review board of the medical center where this study (study code: MTU-EC-OT-0-099/54) was performed.
Before each procedure, the operated limb was exsanguinated and a thigh tourniquet was inflated to 250-300 mmHg and deflated after wound closure. All patients in the ARIF group were operated on by the same foot-ankle arthroscopy fellowship-trained surgeon (CA). Fracture configuration was checked after fixation by fluoroscopic and arthroscopic examination and corrected, whenever possible, if the alignment was not acceptable. As recommended by Miyamoto et al[3], direct visualization via arthroscopy was achieved with the use of fluid irrigation via gravity flow (i.e., without a pump), through the anterolateral and anteromedial portals. Arthroscopic assessment was performed after fixation in order to evaluate the stability of the distal tibiofibular syndesmosis, with fixation considered inadequate if an opening of 2 mm could be identified, and to identify and debride any fibrous tissue interposed in the distal tibiofibular joint. Any other intra-articular disorders, such as osteochondral injury and synovitis, which often accompany unstable ankle fracture, were accessed and treated at that time.
In the ORIF group, patients were operated on by the author, other orthopaedic trauma surgeons, or fellowship-trained foot-ankle surgeons. Anteromedial approach was used for medial malleolar reduction and fixation. The reduction was mainly confirmed by the apposition of fracture ridge at the outer rim of ankle joint and not the direct vision in the joint space. It was also confirmed by the fluoroscopic examination. Lateral approach was used for lateral malleolar or distal fibular reduction and fixation. The reduction was mainly confirmed by the apposition of fracture ridge at the outer rim of ankle joint and not the direct vision in the joint space. It was also confirmed by the fluoroscopic examination. The final configuration of fractures and alignments was checked by fluoroscopic examination after all fixation(s) and, if the alignment was not acceptable, corrected if possible. Surgical drains, including a drain set to bulb suction or a Penrose drain, were placed prior to closing the wound at the discretion of the attending surgeon. A posterior short leg splint was applied after wound closure in all cases.
For all patients, independent evaluations of plain radiographs (anteroposterior, mortise, and lateral views) were conducted by trained orthopedic interns to determine immediate-postoperative fracture configuration and arthritic changes following the surgeries. Assessment of step-off and the widest gap at any intra-articular site of fracture involvement was graded according to the following scales: (1) Detailed evaluation of step-off/gap: Fracture configuration was considered anatomic for a step-off/gap of ≤ 1.0 mm, good for 1.1-2.0 mm, fair for 2.1-3.0 mm; and poor for > 3.0 mm); (2) General evaluation of step-off/gap: Fracture configuration was also assigned a general grade of either acceptable (step-off/gap ≤ 2.0 mm) or unacceptable (step-off/gap > 2.0 mm).
Data were analyzed using SPSS for Windows, Version 13.0 (SPSS Inc., Chicago, IL, United States). Categorical variables were compared using the Fisher’s exact test or χ2 test, and continuous variables were compared using Student’s t test for normally distributed data or the Mann-Whitney U test for non-normally distributed data. A P value of < 0.05 was considered statistically significant.
Neither group demonstrated compartment syndrome or significant complications postoperatively. Table 1 presents a comparison of demographic and clinical variables between the ARIF and ORIF groups. The ARIF and ORIF groups did not differ significantly in age or fracture type (Lauge-Hansen supination/pronation[6]). However, there were significantly more female patients in the ARIF group than in the ORIF group (P = 0.035), and significantly more ARIF patients than ORIF patients underwent post-injury BMD testing (P = 0.021).
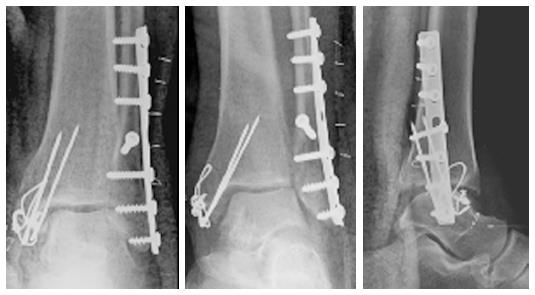
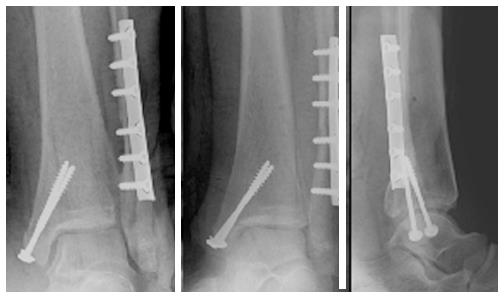
Table 2 presents radiographic outcomes for both groups. There was no significant difference in immediate-postoperative fracture configuration, as assessed by both detailed and general grading systems, between the ARIF (Figure 1) and ORIF (Figure 2) groups. Regarding the arthritic changes of ankle following the fracture, there were 20 patients who had the follow-up period as at least 16 wk following the surgeries (mean follow-up time: 9.8 mo; range 4-22 mo). There were 16 patients (80%) who had mild to significant level of arthritic changes (Table 3). In addition, there were no significant difference of the rates of arthritic changes between ARIF and ORIF groups (P = 0.3) (Table 3). Regarding the postoperative complications, there were two patients who had the available records reporting postoperative complications in overall study (ORIF group: 1 patient with major complications needing additional surgeries; ARIF group: 1 patient with a general complication with no need of additional surgeries). In ORIF group, a mentioned patient had major complications as malaligned fracture and loss of reduction following the initial surgery. In the retrospective review of his initially postoperative radiograph, there was the non-anatomic reduction of medial malleolar fracture with a fracture gap around 1.4 mm (Figure 3) but it was missed during the procedure. He also had the surgical wound inflammation and possible infection that needed the surgical debridement and hardware removal. He was treated with an ankle arthrodesis as a definitive procedure. He could return to recovery uneventfully following the final treatment. In ARIF group, a mentioned patient had a general complication as the surgical wound inflammation and possible infection that needed only intravenous antibiotic medication and local wound care. Her wound had been healed uneventfully following the mentioned treatment. Both major and general complications rates were no significant differences between the two groups (P > 0.05).
| Arthroscopic-assisted reduction and internal fixation | Open reduction and internal fixation | P value | |
| Meticulous grading | |||
| Anatomic (step/gap ≤ 1.0 mm) | 8 (50%) | 8 (27.6%) | 0.539 |
| Good (step/gap = 1.1-2.0 mm) | 4 (25%) | 9 (31.0%) | |
| Fair (step/gap = 2.1-3.0 mm) | 2 (12.5%) | 5 (17.2%) | |
| Poor (step/gap > 3.0 mm) | 2 (12.5%) | 7 (24.1%) | |
| General grading | |||
| Acceptable (step/gap ≤ 2.0 mm) | 12 (75.0%) | 17 (58.6%) | 0.341 |
| Unacceptable (step/gap > 2.0 mm) | 4 (25.0%) | 12 (41.4%) | |
| Treatmentgroups | Arthritic changes1 | ||||
| None | Mild | Moderate | Significance | P value | |
| Arthroscopic- assisted reduction and internal fixation | 2 (25%) | 3 (37.5%) | 0 | 3 (37.5%) | 0.3 |
| Open reduction and internal fixation | 2 (16.7%) | 6 (50%) | 3 (25%) | 1 (8.3%) | |
| Total | 4 (20%) | 9 (45%) | 3 (15%) | 4 (20%) | |
Table 4 compares demographic, clinical, and perioperative data for patients who did and did not undergo BMD testing. Of the 45 study patients, only 10 (22.2%) underwent post-injury BMD testing; 8 of 10 BMD-tested patients had a t score indicative of osteopenia[7,8]. There were significantly higher rates of BMD testing in patients aged > 60 years (P < 0.001), patients who underwent ARIF (P = 0.021), and female patients (P = 0.029). However, bone quality, as assessed by BMD-test t scores, did not differ significantly between the ARIF and ORIF groups. In addition, no significant difference was found in the prevalence of BMD testing between low- and high-energy-fractures (P = 0.341) or among the differences of postoperatively fracture configurations (P = 0.06).
Subgroup analysis of the arthroscopic findings of patients in the ARIF group is presented in Table 5. Osteochondral lesion of the tibial plafond (modified Outerbridge grade II[9]) was found in one patient. The most common locations of talar lesions were the anterolateral (37.6%) and anteromedial (18.8%) areas. Sixty percent of microfractures as described by previous authors[1] were performed for grade III-IV osteochondral lesions.
| Findings | Number of patients (%) |
| Osteochondral lesions | |
| Talus | 10 (62.5%) |
| Tibial plafond | 1 (6.3%) |
| Modified outerbridge classification (talar lesion) | |
| Grade I | 1 (6.3%) |
| Grade II | 4 (25%) |
| Grade III | 3 (18.8%) |
| Grade IV | 2 (12.5%) |
| Synovitis | 15 (93.7%) |
| Lateral | 1 (6.3%) |
| Medial and lateral | 11 (68.8%) |
| Unspecified | 3 (18.8%) |
| Ligamentous injury | |
| None | 6 (37.5%) |
| AITFL | 6 (37.5%) |
| AITFL-PITFL | 2 (12.5%) |
| AITFL-Deep deltoid | 2 (12.5%) |
Over the past decade, the number of orthopedic surgical procedures performed with arthroscopic assistance has increased[3-5]. Indications for ARIF include transchondral talar dome fracture, talar fracture, low-grade fracture of the distal tibia, syndesmotic injury, malleolar fracture, and chronic pain following definitive management of fracture about the ankle[3-5,10]. Among the potential benefits are less extensive exposure, preservation of blood supply, and improved visualization of the pathology. However, data regarding fracture configuration and bone quality in patients with unstable ankle fractures treated with and without ARIF have not been reported.
The present study demonstrates no significant difference in immediate-postoperative configuration or arthritic changes in a short-term follow-up period between groups. Other authors[5], however, have previously shown superior results in the ARIF group. With regard to between-group differences in postoperative fracture configuration, the discrepancy between our results and those of other authors[5] may have been the result of the small number of patients in the ARIF group in the present study. Future prospective studies that include larger numbers of patients with longer term of follow-up and in which clinical scores are recorded in conjunction with the evaluation of postoperative fracture configuration and arthritic changes are necessary to determine whether there is a significant association between ARIF and better postoperative outcomes. However, as an alternative to conventional osteosynthesis, ARIF can facilitate correct assessment of surgical reduction of complex fractures and allow visualization of non-anatomical reductions that would not otherwise be detected under fluoroscopy[11]. This may help to minimize surgical soft-tissue damage and wound extension during surgical reduction[11,12]. Moreover, intra-articular pathology and associated cartilaginous lesions, such as those detected in the present study, can be evaluated and treated as appropriate[11,13].
Regarding the comparison of advantages and disadvantages between ARIF and conventional osteosynthesis or ORIF, the advantages of ARIF were demonstrated as it could directly assess a reduction of an intra-articular fracture and this could provide more anatomic reduction than ORIF. In addition, this procedure was able to perform the debridement to remove the residual hematoma and synovitis debris that might cause pain and limitation of an ankle motion after fixation. It could perform the arthroscopic repair of concomitant injury such as osteochondral lesions[11,13]. Finally, it could also help the surgeon to evaluate syndesmotic widening from the syndesmotic injury during the arthroscopic examination[3] and following syndesmotic fixation if this injury was associated with an ankle fracture. The disadvantages of ARIF could be informed as it might considerably add the operative time by the surgeon with an inadequacy of arthroscopic skills. The longer time of operation might potentially lead to the swelling of surgical wound and compartment syndrome, particularly in some types of ankle fractures such as a Maisonneuve fracture[4]. On the other hand, the advantages of ORIF were explained, as this approach was familiar with any surgeons who had basic skills of the open reduction and fixation of fracture. There was no need of arthroscopic skills to perform this conventional approach. Therefore, this approach is more reproducibility than ARIF. In addition, it has low risk of the compartment syndrome following the operation. However, the disadvantages of ORIF could be as the inability to directly confirm the anatomic reduction of fractures in the joint space. The reduction was routinely checked by the apposition of fracture ridge at the outer rim of ankle joint and by the fluoroscopic examination. These methods could miss some subtle malreduction of fracture in the joint[11] as shown in one patient in ORIF group in the present study. This approach could not perform directly debridement of the residual hematoma included another debris in the joint. It could not perform simultaneously repair of associated lesions, such as osteochondral lesions, or directly assess the syndesmotic widening during the procedure. Surgeons may have to consider these advantages and disadvantages of each approach when they have to make any decision for their patients.
In the present study, only 22.2% of patients received a post-injury BMD test. This suggests a lack of awareness of the need for routine post-injury testing for osteoporosis in ankle-fracture patients; particularly those over the age of 45 (mean age of patients in the present study was 46.5 years). This lack of awareness is consistent with the same parameter in overall low-or high energy fractures in a previous study[7]. No significant difference was found in the prevalence of BMD testing between patients with low and high-energy fractures (P = 0.341) or among the grades of postoperative fracture configuration (P = 0.06). However, age > 60 years and female sex were identified in the present study to be factors significantly associated with post-fracture BMD testing. In ARIF patients, in-patient care by a single foot-ankle surgeon was a significant predictor of post-fracture BMD. Castel et al[14] proposed that many physicians do not recognize osteoporosis as a metabolic condition and thus fail to correlate it with other medical conditions. Suarez-Almazor et al[15] revealed that physician attitudes were vital factors in decisions about screening and treatment of osteoporosis. Female patients were more likely than male patients to receive BMD testing after a low-energy fracture[7]. Castel et al[14] proposed that this bias might be due to the misapprehension that osteoporosis is a problem affecting only females. Improved communication between orthopedic surgeons, specialists, and involved physicians with respect to evidence-based medicine may help to reduce the gap between fracture occurrence and osteoporosis management in both sexes.
In the present study, eight patients in a subgroup of 10 BMD-tested patients had t scores indicative of osteopenia[4,5]. It has been suggested that there is an association between vitamin D deficiency and osteoporosis[16]. The high rate of osteopenia in the present study is consistent with that of a previous study, which demonstrated vitamin D deficiency to be common among patients with foot or ankle fracture[17]. These studies highlight the importance of diagnosing osteoporosis in patients with ankle fractures, particularly in patients who have low energy fractures, in order to prevent subsequent fractures[18,19]. A limitation of the present study was that the small number of patients in the ARIF group might have made a between-group difference difficult to detect.
In conclusion, there was no significant difference between ARIF and ORIF in immediate-postoperative ankle fracture configuration or arthritic changes in a short-term follow-up period. Further study with larger number of patients and longer term of follow-up was needed to validate this conclusion. Although the use of arthroscopy in trauma is increasing, the effectiveness of ARIF compared with that of ORIF in the management of ankle fractures has yet to be verified. The low rate of BMD testing reflects a lack of awareness of the need for routine post-injury testing for osteoporosis in patients with ankle fractures.
The author would like to propose special thanks to Dr. Waroot Pholsawatchai and Dr. Artit Ngiemsuwan who supported about data collection in this study.
Ankle arthroscopy, introduced into the field of ankle surgery for several years is a minimally invasive intra-articular treatment with several advantages. However, there are no reports of fracture configuration, bone quality, arthritic changes in patients with unstable ankle fractures treated with arthroscopic-assisted reduction and internal fixation (ARIF) vs open reduction and internal fixation (ORIF).
The present study is to report ankle fracture configurations, bone quality, and arthritic changes following ARIF or ORIF.
In the past, some concerns arose about safety and efficacy of ARIF. In addition, some surgeons may concern it as difficult to perform for the routinely practice basis. The present study shows that ARIF is comparable to ORIF in terms of postoperative results as immediate-postoperative ankle fracture configuration or arthritic changes or complication rates in a short-term follow-up period. However, ARIF could directly assess a reduction of an intra-articular fracture or syndesmosis and this may provide more anatomic reduction than ORIF in larger study. In addition, arthroscopic treatments for associated intra-articular lesions can be performed in patients with ARIF. This kind of procedure is the advantage in the ARIF group.
Patients with unstable ankle fractures will benefit from ARIF, if treated with cautiously systematic steps as described in the section of operative technique, avoiding untreated intra-articular lesions which commonly associated with ankle fracture and possibly correlated with long term posttraumatic arthritis.
ARIF is referred to the operation that uses an arthroscopic examination to evaluate the stability of the distal tibiofibular syndesmosis, fracture alignment following open reduction and internal fixation, and other intra-articular disorders, such as osteochondral injury and synovitis, which often accompany unstable ankle fracture. The improper alignment of fracture and associated intra-articular lesions can be accessed and treated at that time. ORIF is referred to the conventional operation that uses an open surgery to perform the fracture reduction and internal fixation. This kind of procedure does not include the arthroscopic examination during the procedure. Bone mineral density (BMD) testing is to measure how much calcium and other types of minerals are in a location of bone in each patient. This test helps the health care provider detect osteopenia or osteoporosis and predict the risk of fractures in each patient. The present study used a dual-energy X-ray absorptiometry scan for the BMD-test which would demonstrate the result in a value of “t score”.
It is a well written article and very interesting.
P- Reviewer: Nikolopoulos D S- Editor: Song XX L- Editor: A E- Editor: Wu HL
| 1. | Angthong C, Yoshimura I, Kanazawa K, Takeyama A, Hagio T, Ida T, Naito M. Critical three-dimensional factors affecting outcome in osteochondral lesion of the talus. Knee Surg Sports Traumatol Arthrosc. 2013;21:1418-1426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Zengerink M, Struijs PA, Tol JL, van Dijk CN. Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2010;18:238-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 441] [Cited by in RCA: 409] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 3. | Miyamoto W, Takao M. Management of chronic disruption of the distal tibiofibular syndesmosis. World J Orthop. 2011;2:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Imade S, Takao M, Miyamoto W, Nishi H, Uchio Y. Leg anterior compartment syndrome following ankle arthroscopy after Maisonneuve fracture. Arthroscopy. 2009;25:215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Takao M, Uchio Y, Naito K, Fukazawa I, Kakimaru T, Ochi M. Diagnosis and treatment of combined intra-articular disorders in acute distal fibular fractures. J Trauma. 2004;57:1303-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Lauge-hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. 1950;60:957-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 659] [Cited by in RCA: 568] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 7. | Angthong C, Rodjanawijitkul S, Samart S, Angthong W. Prevalence of bone mineral density testing and osteoporosis management following low- and high-energy fractures. Acta Orthop Traumatol Turc. 2013;47:318-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Levasseur R, Sabatier JP, Guilcher C, Guaydier-Souquières G, Costentin-Pignol V, Jean-Jacques PY, Hulet C, Vielpeau C, Marcelli C. Medical management of patients over 50 years admitted to orthopedic surgery for low-energy fracture. Joint Bone Spine. 2007;74:160-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Uhl M, Allmann KH, Tauer U, Laubenberger J, Adler CP, Ihling C, Langer M. Comparison of MR sequences in quantifying in vitro cartilage degeneration in osteoarthritis of the knee. Br J Radiol. 1998;71:291-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Bonasia DE, Rossi R, Saltzman CL, Amendola A. The role of arthroscopy in the management of fractures about the ankle. J Am Acad Orthop Surg. 2011;19:226-235. [PubMed] |
| 11. | Schoepp C, Rixen D. Arthroscopy-guided fracture management. Ankle joint and calcaneus. Unfallchirurg. 2013;116:318-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Kong C, Kolla L, Wing K, Younger AS. Arthroscopy-assisted closed reduction and percutaneous nail fixation of unstable ankle fractures: description of a minimally invasive procedure. Arthrosc Tech. 2014;3:e181-e184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Turhan E, Doral MN, Demirel M, Atay AO, Bozkurt M, Bilge O, Huri G, Atesok K, Kaya D. Arthroscopy-assisted reduction versus open reduction in the fixation of medial malleolar fractures. Eur J Orthop Surg Traumatol. 2013;23:953-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Castel H, Bonneh DY, Sherf M, Liel Y. Awareness of osteoporosis and compliance with management guidelines in patients with newly diagnosed low-impact fractures. Osteoporos Int. 2001;12:559-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Suarez-Almazor M, Homik JE, Messina D, Davis P. Attitudes and beliefs of family physicians and gynecologists in relation to the prevention and treatment of osteoporosis. J Bone Miner Res. 1997;12:1100-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Zhen D, Liu L, Guan C, Zhao N, Tang X. High prevalence of vitamin D deficiency among middle-aged and elderly individuals in northwestern China: its relationship to osteoporosis and lifestyle factors. Bone. 2015;71:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 17. | Smith JT, Halim K, Palms DA, Okike K, Bluman EM, Chiodo CP. Prevalence of vitamin D deficiency in patients with foot and ankle injuries. Foot Ankle Int. 2014;35:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Lauritzen JB, Lund B. Risk of hip fracture after osteoporosis fractures. 451 women with fracture of lumbar spine, olecranon, knee or ankle. Acta Orthop Scand. 1993;64:297-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 64] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Angthong C, Angthong W, Harnroongroj T, Naito M, Harnroongroj T. Survival times of patients with a first hip fracture with and without subsequent major long-bone fractures. J Nippon Med Sch. 2013;80:42-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |