Published online Apr 18, 2016. doi: 10.5312/wjo.v7.i4.244
Peer-review started: June 1, 2015
First decision: August 16, 2015
Revised: December 11, 2015
Accepted: January 5, 2016
Article in press: January 7, 2016
Published online: April 18, 2016
Processing time: 319 Days and 14.1 Hours
Dislocations of the sternoclavicular joint (SCJ) occur with relative infrequency and can be classified into anterior and posterior dislocation, with the former being more common. The SCJ is inherently unstable due to its lack of articular contact and therefore relies on stability from surrounding ligamentous structures, such as the costoclavicular, interclavicular and capsular ligaments. The posterior capsule has been shown in several studies to be the most important structure in determining stability irrespective of the direction of injury. Posterior dislocation of the SCJ can be associated with life threatening complications such as neurovascular, tracheal and oesophageal injuries. Due to the high mortality associated with such complications, these injuries need to be recognised acutely and managed promptly. Investigations such as X-ray imaging are poor at delineating anatomy at the level of the mediastinum and therefore CT imaging has become the investigation of choice. Due to its rarity, the current guidance on how to manage acute and chronic dislocations is debatable. This analysis of historical and recent literature aims to determine guidance on current thinking regarding SCJ instability, including the use of the Stanmore triangle. The described methods of reduction for both anterior and posterior dislocations and the various surgical reconstructive techniques are also discussed.
Core tip: Most anterior sternoclavicular joint (SCJ) dislocations can be managed non-surgically. A small subgroup of these patients develop persistent symptomatic anterior instability. While most tolerate these symptoms well some find this disabling and surgical stabilisation in such cases have shown satisfactory results. Posterior SCJ dislocation can be subtle and needs prompt identification and immediate closed reduction but if unstable will require surgical stabilisation.
- Citation: Morell DJ, Thyagarajan DS. Sternoclavicular joint dislocation and its management: A review of the literature. World J Orthop 2016; 7(4): 244-250
- URL: https://www.wjgnet.com/2218-5836/full/v7/i4/244.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i4.244
Sternoclavicular joint dislocations are rare and represent only 3% of all dislocations around the shoulder[1]. Despite the uncommon nature of these injuries they can present the clinician with uncertainty regarding their investigation and management. Dislocations may be either traumatic or atraumatic. Those that are due to trauma may dislocate anteriorly or posteriorly, with anterior dislocation being approximately nine times more common. The main concern with a posterior dislocation is the risk of compression to the mediastinal structures which may be life threatening, requiring expedient intervention[2]. Atraumatic dislocations and subluxations may occur in patients with collagen deficiency conditions such as generalised hypermobility syndrome and Ehlers-Danlos[3,4], or clavicular deformity, abnormal muscle patterning, infection or arthritis. The purpose of this educational review is clarify the current thinking regarding the diagnosis of all types of sternoclavicular joint (SCJ) dislocation and how these challenging injuries can be managed[5].
The SCJ is the only bony articulation between the axial skeleton and the upper extremity[6]. The clavicle is unique in the sense that it is the first bone in the human body to ossify, usually in the fifth gestational week but the medial end of the clavicle is the last to fuse, between ages 23-25[7]. Therefore in some patients under 25, what is believed to be an SCJ dislocation is actually a fracture of medial clavicular physis and owing to the remodelling potential of such paediatric injuries can usually be managed conservatively[8].
The SCJ is a diarthrodial saddle type synovial joint which is inherently unstable[8,9]. Less than 50% of the medial clavicular surface articulates with its corresponding articular surface on the manubrium sterni. Its stability is therefore derived from intrinsic and extrinsic ligamentous structures surrounding the joint[8]. These structures include the costoclavicular (rhomboid) ligament, which is divided into an anterior and posterior fasciculus. The anterior fasciculus resists superior rotation and lateral displacement and the posterior fasciculus resists inferior rotation and medial displacement. The interclavicular ligament (extrinsic) and the posterior and anterior sternoclavicular ligaments also aid stability along with the anterior and posterior capsular ligaments. In 1967, Bearn[10] conducted an anatomical study looking at the structures which were of paramount importance in maintaining SCJ stability. By dividing all the ligamentous structures except the capsular restraints there was found to be no effect on the position of the clavicle. However dividing the capsular ligaments in isolation resulted in a superior migration of the medial clavicle. This work was repeated by Spencer et al[6] in 2002 and showed that the posterior capsule is the joints strongest ligamentous stabiliser. Sectioning of the posterior capsule resulted in 41% increase in anterior translation and a 106% increase in posterior translation. When the anterior capsule was cut in isolation this resulted in just a 25% increase in anterior translation and 0.7% increase in posterior translation. Therefore in reconstructive surgery close attention should be paid to the posterior capsule whether the dislocation is anterior or posterior[6].
The SCJ contains a fibrocartilagnous disc which is attached to the anterior and posterior sternoclavicular ligaments and capsule, dividing the SCJ into two synovium-lined cavities[8]. This disc degenerates with time and by the patients 70’s or 80’s is incomplete[11]. Tears of this disc can be a cause of pain in the younger patient.
Subclavius arises from the first rib just lateral to the costoclavicular ligament and inserts onto the inferior surface of the clavicle. It is believed to have a protective function with regards to the stability of the SCJ by reducing the rate of upward displacement of the clavicle when it is under lateral compressive loads[8].
Any movement at the shoulder girdle results in some degree of movement at the SCJ. The clavicle elevates about 4 degrees for every 10 degrees of arm forward flexion[12]. When the shoulders are retracted the SCJ translates anteriorly and the reverse for shoulder protraction. With combined movements the clavicle can rotate up to 40 degrees along its longitudinal axis. Patients with a short clavicle can result in significantly more torque at the SCJ[8].
Posterior dislocation of the SCJ can be caused by a direct force over the anteromedial aspect of the clavicle or an indirect force to the posterolateral shoulder, forcing the medial clavicle posteriorly. Anterior dislocation is usually due to a lateral compressive force to the shoulder girdle, which results in sparing of the posterior capsule but rupture of the anterior capsule and often part of the costoclavicular ligament. As with all high energy injuries one should have a high index of suspicion for associated injuries[8].
Patients presenting with these injuries are often in high energy collisions, whether that be sporting or through a motor vehicle accident[13]. Those with anterior dislocations of the SCJ will complain of a painful lump just lateral to the sternum. Care needs to be taken to determine whether this is indeed a true dislocation or a fracture of the medial clavicle. As mentioned previously, if the patient is under 25 then consideration of the possibility of this being a physeal injury should be undertaken[9].
Posterior dislocations present with medial clavicular pain but also may present with compressive symptoms such as dyspnoea or dysphagia or with vascular and neurological compromise. If any of these symptoms are present then urgent reduction is necessary. Patients often have the affected upper limb adducted across their chest to prevent excess glenohumeral or scapulothoracic movements. There will often be minimal swelling but may be some bruising below the medial aspect of the clavicle[8].
On examination patients will have evidence of swelling and reduced upper limb range of movement. They may also present with new onset paraesthesia in the upper limb and/or weakened pulses or signs of venous congestion.
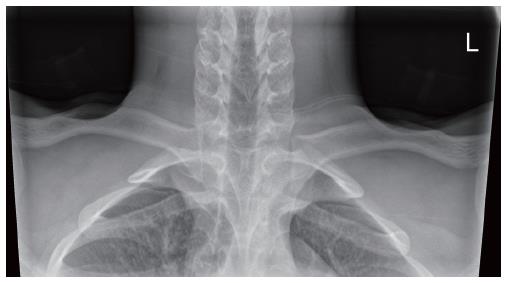
Dislocations of the SCJ are notoriously difficult to visualise on plain radiographs. Routine chest radiographs have a poor sensitivity for picking up dislocations, however they mandatory if there is a suspicion of a posterior dislocation so as to rule out a pneumothorax, pneumomediastinum or haemopneumothorax[8]. In 1975, Rockwood[14] described the “serendipity” view (Figure 1) or 40 degree cephalic tilt which presents the anterior dislocation as a superiorly displaced medial clavicle and the posterior dislocation as an inferiorly displaced medial clavicle. Alternative views include the Heinig view, in which the X-ray beam is directly perpendicular to the SCJ but with an oblique projection in the supine patient[15]. This allows the SCJ to be visualised without underlying vertebral bodies distorting the view.
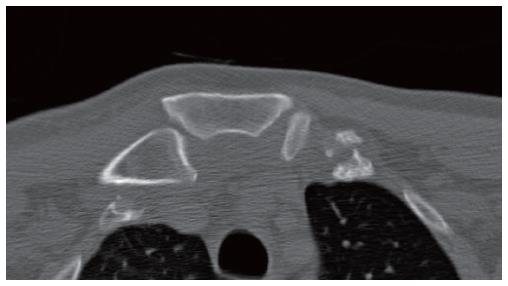
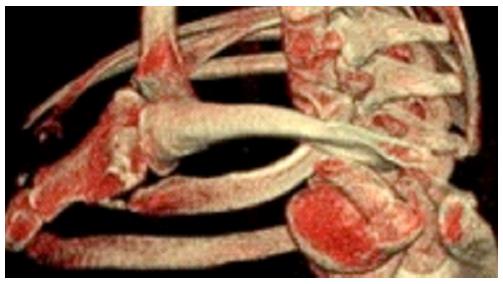
CT imaging is readily available 24 h a day in most trauma units and this is the investigation of choice (Figure 2). It has superior image resolution and allows 3D reconstruction of the SCJ to determine its exact position[16] (Figure 3). MRI has a poorer resolution than CT but can be used to assess ligamentous injury and the condition of the other soft tissues posterior to the SCJ[8].
If there is a suspicion of an intimal tear to the subclavian artery then CT angiography may be necessary.
Dislocations of the SCJ can be broadly classified by the direction of displacement, which may be anterior or posterior, superior or inferior. Dislocation of the SCJ is often not an isolated event and may be due to other structural causes than trauma. It can therefore be thought of as instability, which can be acute, recurrent or persistent. The Stanmore triangle, which is commonly used for glenohumeral instability, has also been applied to instability of the SCJ. The triangle consists of 3 polar groups; type I traumatic structural, type II atraumatic structural and type III muscle patterning, non structural. Patients may move around this triangle with time, for example a patient may initially present with a clear traumatic event but then as a result of abnormal movement due to pain may develop abnormal muscle patterning[8].
With type I instability there is a clear history of trauma, whether this is a fracture of the medial clavicle or SCJ dislocation. With Type II there is no history of trauma but structural change within the capsular tissue, which may be as a result of repetitive microtrauma. In type III there is no structural abnormality and it is the abnormal contraction of muscles, namely pectoralis major, which cause the SCJ to sublux or dislocate[8].
If the patient presents with an acute anterior dislocation of their SCJ (within 7-10 d) then these can be reduced by closed reduction with sedation or under general anaesthetic in the operating room. The patient is placed supine with a bolster placed between their shoulders. Traction is then applied to the affected upper limb in 90 degrees of abduction with neutral flexion and direct pressure is applied over the medial clavicle. Following reduction the arm should be placed in a polysling, maintaining scapular protraction for up to 4 wk. Re-dislocation has found to range between 21% and 100%[17-19] which raises the question whether simple closed reduction without ligament reconstruction is sufficient. One can also question whether reduction of an anterior dislocation is necessary at all.
Bicos et al[20] argues that anterior SCJ instability should primarily be treated conservatively. The patients should be informed there is a high risk of persistent instability with non-operative treatment, but this persistent instability will be well tolerated and have little functional impact in the vast majority. Most anterior SCJ instability can be managed without surgery. However a small sub group of these patients go on to develop persistent symptomatic instability requiring surgical stabilisation.
Although these injuries are rare, complications such as oesophageal, tracheal or neurovascular injury occur in approximately 30% with a mortality rate of 3%-4%[18]. Closed reduction under sedation should be attempted in patients presenting in the acute phase (within 7-10 d). Rockwood[14] described a technique of reduction in which a towel clip is used percutaneously to grasp the medial clavicle and pull it anteriorly.
An alternative reduction tool is the abduction traction technique. The shoulder is abducted to 90 degrees and traction applied. An extension force is then applied to the shoulder resulting in anterior translation of the medial clavicle back into joint[21].
In 1984 Buckerfield et al[22] suggested a technique involving retraction of the shoulders with caudal traction on the adducted arm, while the patient is supported by an interscapular bolster. This achieved reduction in 6 out of 7 patients who had failed reduction through other means.
If closed reduction is not possible or there is on going symptomatic instability of the SCJ, there are numerous surgical techniques that have been described in the literature and there is no evidence that one method is superior over the other. Martínez et al[23] describe a technique used in 1 posterior dislocation using gracilis tendon passed in a figure of 8 through drill holes in the manubrium and clavicle. At 1 year follow-up there was evidence of SCJ subluxation and erosion of both the manubrium and medial clavicle. Despite this patient was asymptomatic.
Booth et al[24] reported a more successful technique in 5 SCJ’s. The sternal origin of the sternocleidomastoid (SCM) with a strip of periosteum is detached and passed under the first rib and back through a drill hole in the clavicle and then tied back onto itself. In this way it has effectively reconstructed the costoclavicular ligament. No complications or failures were noted in this group.
Bae et al[25] presented 15 cases in which either semitendinosus or SCM graft was passed through the medial clavicle and manubrium in a figure of 8. The medial 2-2.5 cm of clavicle was then resected. Results were mixed with 87% of patients achieving stability but 40% of patients complained of persistent pain.
More recently, Abiddin et al[26] had success with the use of suture anchors, avoiding the need for graft. Sutures were placed through drill holes in the medial clavicle and manubrium combined with a capsular repair. He reported 2 failures, one of which was traumatic.
Franck et al[27] reported excellent results with the use of a Balser plate. The hook of this was inserted under the manubrium with the lateral aspect of the plate lying on the medial clavicle. No re-dislocations were reported in any of the 9 patients however metalwork needed to be removed a secondary procedure to prevent migration.
Wallace et al[28] reported their new technique of stabilising the SC joint by reconstructing the costoclavicular ligament using a braided polyester mesh device (Surgilig Lockdown) (Figures 4 and 5). In a separate study they had looked at the histological response of the braided polyester mesh device retrieved from AC joint and found outer capsule formation composed of collagen with fibroblast. This technique recreates the costoclavicular ligament and also stabilises the anterior and the posterior capsule during stabilisation. Their results showed no major or life threatening complication and all patients achieved good functional outcome and patient satisfaction[28-30].
An important lesson was learned through the work of Lyons et al[31]. Rather than a soft tissue procedure they described the use of smooth and threaded k wires to stabilise 21 anterior SCJ dislocations. The results were catastrophic with 8 deaths due to wire migration into major vascular structures. A further 6 patients only survived cardiac tamponade following surgical intervention. In later work Rockwood et al[32] described excision arthroplasty of the medial 1.5 cm of the clavicle. However, he found that in those with a ruptured CCL requiring reconstruction then excision of the medial clavicle was unsatisfactory.
In patients with type II instability of the SCJ, the usual presentation is prominence of the medial clavicle and pain felt on overhead activities. There is often a history of generalised ligamentous laxity. This group of patients can usually be managed with steroid injections and physiotherapy alone. Rockwood et al[33] looked at patients with atraumatic anterior dislocations and found that when treated conservatively 78% of patients had no restriction of lifestyle or activity, however 90% had persistent subluxation and 21% of these had ongoing pain. Patients treated surgically all showed unsatisfactory results. Atraumatic posterior dislocations should be treated in a similar way to traumatic dislocations with open reduction and stabilisation due to the risk of compression to retrosternal structures.
Surgery is rarely indicated in type III instability of the SCJ. The problem is non-structural and due to abnormal muscle patterning. They may be investigated using EMG’s to identify if the pectoralis major is being recruited inappropriately. Management is therefore with biofeedback physiotherapy which requires patient compliance and the re-learning of appropriate muscle contraction and proprioception[34]. Surgery should be reserved for those patients who demonstrate some structural abnormality which has then gone on to develop abnormal muscle patterning (type II/III)[8].
The main recognised complications are associated with traumatic posterior dislocations of the SCJ. Symptoms of compression of retrosternal structures have been reported to occur in up to a third of cases with life threatening consequences[35]. Complications include brachial plexus and vascular injuries, oesophageal ruptures and tracheal compression and there have been 5 known reported cases of deaths[2].
Untreated anterior dislocations will result in a longstanding cosmetic deformity, which some patients may find unsightly. Persistent pain and instability are the main reasons for failure of surgical stabilisation of SCJ injuries[8].
Dislocation of SCJ does not always occur in isolation and may occur in combination with the ACJ. This is known as bipolar clavicular dislocation or the traumatic floating clavicle. Only 40 cases have been described in the literature making this injury rare[13]. The first case was described by Porral[36] in 1831 and since then there has been intermittent reports of this injury, which in the majority of cases is due to high velocity road traffic collisions, falls from height and heavy objects falling onto the shoulder. Management of this injury should be designed on an individual patient basis. All reported an anterior dislocation of the SCJ and posterior dislocation of the ACJ.
More recently the first ever-case report of floating clavicle with a unique combination of posterior SCJ dislocation with Grade III ACJ dislocation was reported. The authors had recommended surgical stabilisation of both SCJ and the ACJ for this injury[37].
Dislocations of the SCJ are rare and may result from direct trauma as an acute occurrence or in the more persistent case of atraumatic structural instability or non structural abnormal muscle patterning. Traumatic structural dislocation should be investigated appropriately with the use of CT if the diagnosis is unclear. The use of acute reduction of anterior dislocations is debatable as up to 100% re-dislocate and reduction techniques are not without risk. Posterior dislocations with compressive symptoms need to be reduced promptly to prevent life threatening complications. Persistent pain and instability can be managed surgically through a variety of means. Surgical stabilisation using braided polyester weave device (Surgilig Lockdown) has shown promising results in the functional outcome studies that I have been involved in. The use of pin transfixation however is absolutely contraindicated due to the high risk of pin migration and death.
Surgical management of SCJ injuries are technically demanding. The surgeon should be familiar with the complex anatomy and it is recommended that these procedures be carried out in large centres with cardiothoracic surgical back up if required to deal with any intra operative or post operative complications.
P- Reviewer: Emara K, Hernandez-Sanchez S, Yamakado K S- Editor: Gong ZM L- Editor: A E- Editor: Wu HL
| 1. | Cave E. Shoulder girdle injuries. Chicago: Year book publishers 1958; 58-259. |
| 2. | Garg S, Alshameeri ZA, Wallace WA. Posterior sternoclavicular joint dislocation in a child: a case report with review of literature. J Shoulder Elbow Surg. 2012;21:e11-e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Iglesias JL, Renard T. Diaphragmatic hernia in an 8-year-old with Ehlers-Danlos syndrome. Pediatr Surg Int. 1998;13:553-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Finsterbush A, Pogrund H. The hypermobility syndrome. Musculoskeletal complaints in 100 consecutive cases of generalized joint hypermobility. Clin Orthop Relat Res. 1982;124-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Medvecky MJ, Zuckerman JD. Sternoclavicular joint injuries and disorders. Instr Course Lect. 2000;49:397-406. [PubMed] |
| 6. | Spencer EE, Kuhn JE, Huston LJ, Carpenter JE, Hughes RE. Ligamentous restraints to anterior and posterior translation of the sternoclavicular joint. J Shoulder Elbow Surg. 2002;11:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 77] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Wirth MA, Rockwood CA. Acute and Chronic Traumatic Injuries of the Sternoclavicular Joint. J Am Acad Orthop Surg. 1996;4:268-278. [PubMed] |
| 8. | Sewell MD, Al-Hadithy N, Le Leu A, Lambert SM. Instability of the sternoclavicular joint: current concepts in classification, treatment and outcomes. Bone Joint J. 2013;95-B:721-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Tepolt F, Carry PM, Heyn PC, Miller NH. Posterior sternoclavicular joint injuries in the adolescent population: a meta-analysis. Am J Sports Med. 2014;42:2517-2524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Bearn JG. Direct observations on the function of the capsule of the sternoclavicular joint in clavicular support. J Anat. 1967;101:159-170. [PubMed] |
| 11. | van Tongel A, MacDonald P, Leiter J, Pouliart N, Peeler J. A cadaveric study of the structural anatomy of the sternoclavicular joint. Clin Anat. 2012;25:903-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Inman VT, Saunders JB, Abbott LC. Observations of the function of the shoulder joint. 1944. Clin Orthop Relat Res. 1996;3-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 205] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 13. | Choo C, Wong H, Nordin A. Traumatic floating clavicle: a case report. Malays Orthop J. 2012;6:57-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Rockwood CA. Dislocations of the sternoclavicular joint. American academy of orthopaedic surgeons instructional course lectures: Volume XXIV. st. Louis: CV Mosby 1975; 144-159. |
| 15. | Robinson CM, Jenkins PJ, Markham PE, Beggs I. Disorders of the sternoclavicular joint. J Bone Joint Surg Br. 2008;90:685-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 94] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 16. | Levinsohn EM, Bunnell WP, Yuan HA. Computed tomography in the diagnosis of dislocations of the sternoclavicular joint. Clin Orthop Relat Res. 1979;12-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Savastano AA, Stutz SJ. Traumatic sternoclavicular dislocation. Int Surg. 1978;63:10-13. [PubMed] |
| 18. | Nettles JL, Linscheid RL. Sternoclavicular dislocations. J Trauma. 1968;8:158-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 112] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Eskola A. Sternoclavicular dislocation. A plea for open treatment. Acta Orthop Scand. 1986;57:227-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 32] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Bicos J, Nicholson GP. Treatment and results of sternoclavicular joint injuries. Clin Sports Med. 2003;22:359-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Rockwood CA, Wirth M. Injuries to the sternoclavicular joint. Rockwood and Green’s fractures in adults. 1996;1415-1471. |
| 22. | Buckerfield CT, Castle ME. Acute traumatic retrosternal dislocation of the clavicle. J Bone Joint Surg Am. 1984;66:379-385. [PubMed] |
| 23. | Martínez A, Rodríguez A, González G, Herrera A, Domingo J. Atraumatic spontaneous posterior subluxation of the sternoclavicular joint. Arch Orthop Trauma Surg. 1999;119:344-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Booth CM, Roper BA. Chronic dislocation of the sternoclavicular joint: an operative repair. Clin Orthop Relat Res. 1979;17-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Bae DS, Kocher MS, Waters PM, Micheli LM, Griffey M, Dichtel L. Chronic recurrent anterior sternoclavicular joint instability: results of surgical management. J Pediatr Orthop. 2006;26:71-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 64] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 26. | Abiddin Z, Sinopidis C, Grocock CJ, Yin Q, Frostick SP. Suture anchors for treatment of sternoclavicular joint instability. J Shoulder Elbow Surg. 2006;15:315-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Franck WM, Jannasch O, Siassi M, Hennig FF. Balser plate stabilization: an alternate therapy for traumatic sternoclavicular instability. J Shoulder Elbow Surg. 2003;12:276-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 59] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 28. | Available from: http//www.sicot.org/.../Final%20Programme%20-%20Hyderabad%20-%20we. |
| 29. | Kocsis G, McCulloch TA, Thyagarajan D, Wallace WA. The biological response to a failed extra-articular polyester ligament used for AC Joint reconstruction at the shoulder girdle: a retrieval analysis of five cases. Bone Joint J. 2015;97-B:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | Thyagarajan D, Kocsis G, Wallace WA. Surgical stabilisation for sternoclavicular joint instability (Unpublised) SECEC congress 17-20 September 2014, Istanbul. Available from: http//www.secec2015.com/wp.../2014/06/SECEC_2014_Congress_Program. |
| 31. | Lyons FA, Rockwood CA. Migration of pins used in operations on the shoulder. J Bone Joint Surg Am. 1990;72:1262-1267. [PubMed] |
| 32. | Rockwood CA, Groh GI, Wirth MA, Grassi FA. Resection arthroplasty of the sternoclavicular joint. J Bone Joint Surg Am. 1997;79:387-393. [PubMed] |
| 33. | Rockwood CA, Odor JM. Spontaneous atraumatic anterior subluxation of the sternoclavicular joint. J Bone Joint Surg Am. 1989;71:1280-1288. [PubMed] |
| 34. | Jaggi A, Lambert S. Rehabilitation for shoulder instability. Br J Sports Med. 2010;44:333-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 35. | Ono K, Inagawa H, Kiyota K, Terada T, Suzuki S, Maekawa K. Posterior dislocation of the sternoclavicular joint with obstruction of the innominate vein: case report. J Trauma. 1998;44:381-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 55] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Porral A. Observation of a double dislocation of the right clavicle. J Univ Hebd Chir Prat. 1831;2:78-82. |
| 37. | Thyagarajan D, Webb M, Wallace WA. A rare case of floating clavicle and a novel technique for stabilizing the sternoclavicular joint. Shoulder & Elbow. 2015;7:44-48. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |