Published online Feb 18, 2016. doi: 10.5312/wjo.v7.i2.123
Peer-review started: July 9, 2015
First decision: September 30, 2015
Revised: October 10, 2015
Accepted: December 7, 2015
Article in press: December 8, 2015
Published online: February 18, 2016
Processing time: 228 Days and 10.5 Hours
AIM: To compare reverse-total shoulder arthroplasty (RSA) cost-effectiveness with total hip arthroplasty cost-effectiveness.
METHODS: This study used a stochastic model and decision-making algorithm to compare the cost-effectiveness of RSA and total hip arthroplasty. Fifteen patients underwent pre-operative, and 3, 6, and 12 mo post-operative clinical examinations and Short Form-36 Health Survey completion. Short form-36 Health Survey subscale scores were converted to EuroQual Group Five Dimension Health Outcome scores and compared with historical data from age-matched patients who had undergone total hip arthroplasty. Quality-adjusted life year (QALY) improvements based on life expectancies were calculated.
RESULTS: The cost/QALY was $3900 for total hip arthroplasty and $11100 for RSA. After adjusting the model to only include shoulder-specific physical function subscale items, the RSA QALY improved to 2.8 years, and its cost/QALY decreased to $8100.
CONCLUSION: Based on industry accepted standards, cost/QALY estimates supported both RSA and total hip arthroplasty cost-effectiveness. Although total hip arthroplasty remains the quality of life improvement “gold standard” among arthroplasty procedures, cost/QALY estimates identified in this study support the growing use of RSA to improve patient quality of life.
Core tip: Based on industry accepted standards, cost/quality-adjusted life year (QALY) estimates supported both reverse-total shoulder arthroplasty (RSA) and total hip arthroplasty cost-effectiveness. The cost/QALY estimates identified in this study support the growing use of RSA to improve patient quality of life.
- Citation: Bachman D, Nyland J, Krupp R. Reverse-total shoulder arthroplasty cost-effectiveness: A quality-adjusted life years comparison with total hip arthroplasty. World J Orthop 2016; 7(2): 123-127
- URL: https://www.wjgnet.com/2218-5836/full/v7/i2/123.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i2.123
The biomechanical advantage provided by improved deltoid muscle function following reverse-total shoulder arthroplasty (RSA) has led to its increased use for treating patients with massive rotator cuff tear arthropathy, severe shoulder fracture or gleno-humeral joint degeneration. Associated with this increased use is the need to better identify RSA cost-effectiveness with consideration for revision challenges[1], and its true utility in the context of diminishing healthcare financial resources[2]. History has demonstrated that total hip and knee arthroplasty use has progressively increased among patients with widely-ranging ages and diagnoses[3,4]. If patient outcomes prove comparable to these other arthroplasty procedures a similar evolution may develop for RSA.
The cost-effectiveness of RSA in terms of quality-adjusted life years (QALY) within the context of healthcare industry standards is currently unknown[5]. The purpose of this study was to compare RSA cost-effectiveness with total hip arthroplasty cost-effectiveness, widely considered to be the “gold standard” among arthroplasty procedures[6]. The study hypothesis was that both procedures would prove cost effective based on industry accepted standards of a $30000-50000 dollars United States/QALY[1-4]. Information such as this would provide vital insight into the true efficacy of RSA.
Following University of Louisville and Norton Healthcare Medical Institutional Review Board approvals, 15 consecutive patients preparing to undergo RSA underwent pre-operative clinical examination by the same fellowship-trained shoulder surgeon. All patients had severe rotator cuff arthropathy. Given the lack of functional rotator cuff tissue an RSA was selected rather than a standard total shoulder arthroplasty. By reversing humeral head and glenoid component locations, RSA increased deltoid muscle mechanical efficiency during shoulder elevation and improved joint stability. All patients received a Donjoy Orthopaedic Reverse Shoulder Prosthesis (DJO, Vista, CA, United States). Patients also completed the short form-36 Health Survey subscales [physical function (PF), role physical (RP), role emotional (RE), bodily pain (BP), general health (GH), vitality (VT), mental health (MH), and social function (SF)]. Clinical examination and short form-36 surveys were repeated at 3-mo, 6-mo, and at 1-year post-surgery. By the end of the first post-operative year all patients were satisfied with the RSA procedure and had met their pain reduction and functional restoration expectations. These data were compared with the findings of Mangione et al[7] who studied 224 patients of similar age following total hip arthroplasty over the same follow-up time intervals, also collecting 0-100 point scale short form-36 survey data. Short form-36 subscale data from both studies was converted to EuroQual Group Five Dimension Health Outcome Scores using previously reported methods[8] and the following formula (α× PF + β× RP + γ× RE + δ× BP + ε × GH + ζ× VT + η× MH + θ × SF). In this formula the Greek letters signify constants from an accepted conversion algorithm[8]. Short form-36 physical function subscale score values for each follow-up time period were converted to QALY values[8]. Baseline values were then subtracted from follow-up QALY scores to identify condition improvements over time (1, 6 and 12 mo). This accounted for the entire first post-surgical year. For study purposes a 12 mo follow-up period was considered representative of peak quality of life improvement following arthroplasty[9,10].
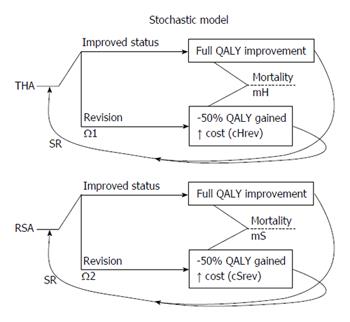
A stochastic model and decision making algorithm[11,12] (Figure 1) incorporated revision rates[13,14] and a standard annual general health reduction to incrementally estimate QALY changes from baseline for each arthroplasty procedure simulating aging over the course of life expectancy[12]. The expected revision rate for each procedure (revisions/patient years followed) was applied to the stochastic model (Ω1, Ω2). Patient revisions/patient years was determined by taking the estimated number of procedural revisions divided by the number of patient follow-up years for total hip[13] and RSA[14]. For the duration of stochastic model application, for a projected revision, then the remainder of projected quality of life was considered to be only 50% improved from baseline state. If the patient required revision surgery 50% of their QALY potential was decreased from that point forward[15]. A 3% annual general health decline representative of aging was also added to the model[16]. Annual quality of life improvement represented the previous year’s quality of life improvement over baseline minus revision rate and standard general health reduction (3%). Collective quality of life improvement over baseline values were summed for the years of projected life for each arthroplasty group. This represented the QALY associated with each arthroplasty procedure.
Stochastic model variable definitions are provided in Table 1. Pre- (Hpreop, Rpreop) and post-operative (Ipostop) costs for each arthroplasty method including implant costs and hospital associated direct costs were determined using previously reported data[9] and data obtained from the hospital where the surgical procedure was performed. The same preoperative assessments were assumed for both arthroplasty surgical groups[9]. The average cost of a revision (Hrev or Rrev) was calculated by summing the non-implant related surgical and hospital costs (Hsurg or Rsurg), and the cost of the revised implant components (Hrevimplant or Rrevimplant), based on historical data[13,14] and post-operative cost estimates[15]. Revision costs calculated by the model represented the proportion of patients expected to undergo a revision multiplied by the average cost of a revision (either Hrev or Rrev). Revision expenses were then added to the primary cost. Cost per QALY were then calculated for each procedure.
| Component | Abbreviation | Value |
| Age of THA patients, yr ± SD[7] | AgeH | 67.9 ± 9.0 |
| Gender of THA patients, % men, % women[7] | %H-M, %H-W | 46%, 54% |
| Age of RSA patient, yr ± SD | AgeS | 69.3 ± 7.7 |
| Gender of reverse shoulder patients, % men, % women | %RSM, %RSW | 60%, 40% |
| Standard reduction in quality of life[9] | SR | -3% |
| 1Pre-operative THA cost, $[7] | Hpreop | 400 |
| Pre-operative RSA cost, $[2] | Rpreop | 600 |
| 1Cost of THA implant, $ | Himplant | 4300 |
| 1THA surgical and hospital costs, $ | Hsurg | 5600 |
| 1Total direct cost of THA, $ | dcTHA | Himplant + Hsurg = 9900 |
| 1Cost of post-operative implant care, $[7] | Ipostop | 1400 |
| 1Cost of primary THA, $ | cTHA | dcTHA + Hpreop + Ipostop = 11700 |
| Cost of THA revision implant, $[13] | Hrevimplant | %cup × cCup + %liner × cLiner + %stem × cStem = 1700 |
| Average cost of THA revision, $[13] | Hrev | Hsurg + Hrevimplant = 7300 |
| 1Cost of RSA implant, $ | Rimplant | 8900 |
| 1RSA surgical, hospital costs, $ | Rsurg | 6100 |
| 1Total direct primary RSA cost, $ | dcRSA | Rimplant + Rsurg = 15000 |
| 1Primary RSA cost, $ | cRSA | dcRSA + Rpreop + Ipostop = 17000 |
| 1RSA revision implant cost, $ | Rrevimplant | %glenoid × cGS + %Stem × cStem + %poly × cPoly %Hemi × cHemi = 4000 |
| 1Average revision RSA cost, $ | Rrev | Rsurg + Rrevimplant |
| The length of first, second, third cycles hip, yr | hCL1, hCL2, hCL3 | 0.083, 0.416, 0.5 |
| The length of first, second, third cycles shoulder, yr | sCL1, sCL2, sCL3 | 0.25, 0.25, 0.5 |
| Length of cycle thereafter both, yr | CL | 1 |
| Age-specific mortality rate male, female[12] | mAgeM, AgeF | 2007 United States life tables |
| Mortality rate, shoulder | mS | mAgeM × %SM + mAgeF × %SF |
| Mortality rate, hip | mH | mAgeM × %HM + mAgeF × %HF |
| THA revision cases[13] | hRev | 44 |
| Published cases[13] | hPC | 211 |
| THA follow-up years[13] | hFY | 13.9 × hPC = 2932 |
| Probability of THA revision/shoulder, yr | Ω1 | hRev/hFY = 0.015 |
| RSA revisions[14] | sRev | 79 |
| Published cases[14] | sPC | 782 |
| RSA follow-up years[14] | sFY | 3.5 × sPC = 2737 |
| RSA revision probability per shoulder, yr | Ω2 | sRev/sFY = 0.029 |
| Utility, quality of llfe improvement, EQ-5D | pQoL, oQoL | α× PF + β× RP + γ× RE + δ× BP + ε × GH + ζ× VT + η× MH + θ × SF |
| Utility hip, shoulder | qHwell, qSwell | oQOL - pQOL |
| The utility associated with a THA revision, QALY | qHrev | 0.5 × qHwell |
| The utility associated with a RSA revision, QALY | qSrev | 0.5 × qSwell |
Further evaluation was performed to determine the influence of short form-36 Health Survey subscale scores on the QALY of patients following total hip arthroplasty and RSA. Similar to the report of March et al[17], pain, physical function, and role-physical subscale scores displayed the greatest influence on QALY score improvement following either surgical procedure. The strongest single influence on QALY score improvement for both total hip arthroplasty and RSA was the physical function subscale. Focused attention to this subscale revealed that of 10 total items, nine related more specifically to ambulation while only three related more specifically to shoulder function. These included item 3a moderate activities such as moving a table, pushing a vacuum cleaner, bowling, or playing golf; item 3c lifting or carrying groceries; and item 3j bathing or dressing yourself[18]. The stochastic model was used to calculate QALY using both aggregate physical function subscale scores and scores based solely on the three more shoulder-specific physical function subscale question items.
Estimated QALY values were 2.0 years for RSA and 3.5 years for total hip arthroplasty. When the stochastic model and decision-making algorithm was applied without standard reductions for revision rates QALY values improved to 2.8 years for RSA and to 4.7 years for total hip arthroplasty. Total direct and indirect hospital cost estimates were $17000 for RSA and $11700 for total hip arthroplasty. Costs increased to $22200 and $13800, respectively, when adjusted for revision. Using these calculations the cost/QALY was $11100 for RSA and $3900 for total hip arthroplasty. Primary and revision implant costs represented 58% of RSA and 43% of total hip arthroplasty costs.
Short form-36 Health Survey physical function subscale scores initially revealed a considerable QALY value disparity between RSA and total hip arthroplasty patient groups. However, when including only shoulder-specific short form-36 physical function questions RSA QALY scores improved from 2.0 to 2.8 (t-test, P = 0.01) and RSA cost/QALY decreased to $8100.
The most important study finding is that the cost/QALY score for RSA is considerably less than the industry accepted standard of $30000-50000 cost/QALY[1-4]. Since only 3 of 10 (30%) short form-36 physical function subscale questions are specific to upper extremity function; this subscale is naturally skewed toward a hip and locomotion focus. When considering solely more shoulder-specific physical function subscale items the RSA QALY score improved significantly and shoulder region-specific estimate validity also improved.
Using a similar stochastic model and decision-making algorithm, Coe et al[5] reported than an implant cost less than $7000 United States dollars would make the RSA slightly more efficacious than shoulder hemiarthroplasty. In our study, total hip arthroplasty was approximately 2-3 times more cost effective than RSA. This finding however, does not preclude RSA cost effectiveness based on current industry accepted standards[1-4]. In a prospective study of 55 patients who were 70.8 (range = 46-88 years) years of age at time of RSA, Virani et al[2] reported that at a mean 48 mo follow-up patients had an 82% shoulder pain reduction and a 70% shoulder function improvement. This study estimated a mean 4-year total cost of $24661, with hospitalization accounting for 92% of the total cost[2]. These findings suggest the need for an earlier transition to a less expensive outpatient care environment as an important step in managing post-RSA costs.
The small sample size of this study necessitated several stochastic modeling assumptions. With the development of more shoulder-specific quality of life measurement tools and additional long-term RSA revision rate data, cost effectiveness estimates will become more accurate[5]. Regardless, identical analytical procedures were performed for both arthroplasty patient groups generating valid, cost/QALY estimates. Since patient outcomes, hospitalization timetables, and implant costs may be influenced by multiple factors including regional differences, patient age and comorbidities, rehabilitation strategies and activity expectations, clinicians are advised to use care when extrapolating these data to individual practice sites.
Based on industry accepted standards, cost/QALY estimates supported both RSA and total hip arthroplasty cost-effectiveness. Although total hip arthroplasty remains the quality of life improvement “gold standard” among arthroplasty procedures, cost/QALY estimates identified in this study support the growing use of RSA to improve patient quality of life.
Comparing the reverse-total shoulder arthroplasty (RSA) with the “gold standard” arthroplasty procedure was a daunting task.
The results of this study confirm the efficacy of RSA for positively impacting patient quality of life.
Since hospitalization accounted for a high percentage of the total cost, future studies should investigate the efficacy of making an earlier transition to a less expensive outpatient care environment.
This is a nice paper.
P- Reviewer: Fenichel I, Hasegawa M S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Boileau P, Melis B, Duperron D, Moineau G, Rumian AP, Han Y. Revision surgery of reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:1359-1370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 173] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 2. | Virani NA, Williams CD, Clark R, Polikandriotis J, Downes KL, Frankle MA. Preparing for the bundled-payment initiative: the cost and clinical outcomes of reverse shoulder arthroplasty for the surgical treatment of advanced rotator cuff deficiency at an average 4-year follow-up. J Shoulder Elbow Surg. 2013;22:1612-1622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Sharkey PF, Austin MS, Hozack W. Total hip arthroplasty in the young patient. Instr Course Lect. 2006;55:173-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Engh GA. Advances in knee arthroplasty for younger patients: traditional knee arthroplasty is prologue, the future for knee arthroplasty is prescient. Orthopedics. 2007;30:55-57. [PubMed] |
| 5. | Coe MP, Greiwe RM, Joshi R, Snyder BM, Simpson L, Tosteson AN, Ahmad CS, Levine WN, Bell JE. The cost-effectiveness of reverse total shoulder arthroplasty compared with hemiarthroplasty for rotator cuff tear arthropathy. J Shoulder Elbow Surg. 2012;21:1278-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Räsänen P, Paavolainen P, Sintonen H, Koivisto AM, Blom M, Ryynänen OP, Roine RP. Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop. 2007;78:108-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 285] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 7. | Mangione CM, Goldman L, Orav EJ, Marcantonio ER, Pedan A, Ludwig LE, Donaldson MC, Sugarbaker DJ, Poss R, Lee TH. Health-related quality of life after elective surgery: measurement of longitudinal changes. J Gen Intern Med. 1997;12:686-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 148] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Ara R, Brazier J. Deriving an algorithm to convert the eight mean SF-36 dimension scores into a mean EQ-5D preference-based score from published studies (where patient level data are not available). Value Health. 2008;11:1131-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 158] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 9. | Rissanen P, Aro S, Sintonen H, Slätis P, Paavolainen P. Quality of life and functional ability in hip and knee replacements: a prospective study. Qual Life Res. 1996;5:56-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 112] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Nilsdotter AK, Lohmander LS. Patient relevant outcomes after total hip replacement. A comparison between different surgical techniques. Health Qual Life Outcomes. 2003;1:21. [PubMed] |
| 11. | Hazen GB. Stochastic trees: a new technique for temporal medical decision modeling. Med Decis Making. 1992;12:163-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009;57:1-134. [PubMed] |
| 13. | Engh CA, Claus AM, Hopper RH, Engh CA. Long-term results using the anatomic medullary locking hip prosthesis. Clin Orthop Relat Res. 2001;137-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 101] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20:146-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 798] [Cited by in RCA: 601] [Article Influence: 42.9] [Reference Citation Analysis (0)] |
| 15. | Dawson J, Fitzpatrick R, Murray D, Carr A. Comparison of measures to assess outcomes in total hip replacement surgery. Qual Health Care. 1996;5:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 133] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 16. | Siegel JE, Torrance GW, Russell LB, Luce BR, Weinstein MC, Gold MR. Guidelines for pharmacoeconomic studies. Recommendations from the panel on cost effectiveness in health and medicine. Panel on cost Effectiveness in Health and Medicine. Pharmacoeconomics. 1997;11:159-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 169] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | March LM, Cross MJ, Lapsley H, Brnabic AJ, Tribe KL, Bachmeier CJ, Courtenay BG, Brooks PM. Outcomes after hip or knee replacement surgery for osteoarthritis. A prospective cohort study comparing patients’ quality of life before and after surgery with age-related population norms. Med J Aust. 1999;171:235-238. [PubMed] |
| 18. | Ware JE, Snow KK, Kosinski M. SF-36® Health Survey: Manual and Interpretation Guide. Lincoln, RI: QualityMetric Incorporated 2000; . |