Published online Dec 18, 2016. doi: 10.5312/wjo.v7.i12.785
Peer-review started: April 18, 2016
First decision: June 14, 2016
Revised: June 29, 2016
Accepted: August 27, 2016
Article in press: August 29, 2016
Published online: December 18, 2016
Processing time: 236 Days and 22.4 Hours
Orthopaedic surgeons specialising in adult hip reconstruction surgery often face the problem of osteoarthritis secondary to congenital hip disease (CHD). To achieve better communication among physicians, better treatment planning and evaluation of the results of various treatment options, an agreed terminology is needed to describe the entire pathology. Furthermore, a generally accepted classification of the deformities is necessary. Herein, the authors propose the use of the term “congenital hip disease” and its classification as dysplasia, low dislocation and high dislocation. Knowledge of the CHD natural history facilitates comprehension of the potential development and progression of the disease, which differs among the aforementioned types. This can lead to better understanding of the anatomical abnormalities found in the different CHD types and thus facilitate preoperative planning and choice of the most appropriate management for adult patients. The basic principles for improved results of total hip replacement in patients with CHD, especially those with low and high dislocation, are: Wide exposure, restoration of the normal centre of rotation and the use of special techniques and implants for the reconstruction of the acetabulum and femur. Application of these principles during total hip replacement in young female patients born with severe deformities of the hip joint has led to radical improvement of their quality of life.
Core tip: This review is based on the knowledge and experience acquired in the long course of the senior author’s surgical practice on the complex problem of congenital deformities of the hip in adults.
- Citation: Hartofilakidis G, Lampropoulou-Adamidou K. Lessons learned from study of congenital hip disease in adults. World J Orthop 2016; 7(12): 785-792
- URL: https://www.wjgnet.com/2218-5836/full/v7/i12/785.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i12.785
Congenital deformities of the hip are the main cause of secondary joint osteoarthritis (OA). Depending on the severity of the deformity, undiagnosed patients or those treated insufficiently in infancy face the problem of OA earlier or later in their adult life.
Initially, before the introduction of total hip replacement (THR), we were treating adult patients with different types of osteotomies, without having enough knowledge of the pathological anatomy and the natural history of the underlying deformity. This explains why the results of osteotomies were not always satisfactory. Later, when we started to treat these patients with THR, we realised that the anatomy of the joint differs between patients, thus requiring adjustment of the surgical technique. Since then, the complex problem of congenital hip deformities became one of the main scientific interests of the senior author (GH). Lessons learned, in the long course of this experience, are summarised in this review article.
The first lesson involves the understanding of the nature of the hip deformities present at birth. The terms used for these deformities were mostly misleading, causing misunderstandings and confusion. We have been concerned about the term “developmental dysplasia of the hip” (DDH) for two reasons: (1) The term “developmental” is not descriptive of the congenital origin of the deformity; and (2) An indiscriminate use of the term “dysplasia” is not in agreement with the variety of the underlying pathology. Therefore, we recommend the use of the term “congenital hip disease” (CHD) for the entire spectrum of related deformities. These deformities are congenital in nature and have the potential to develop.
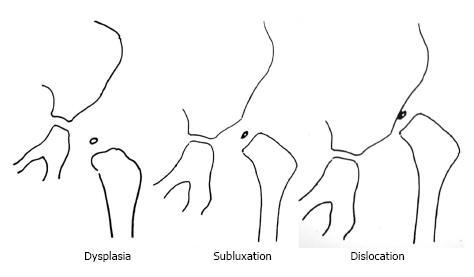
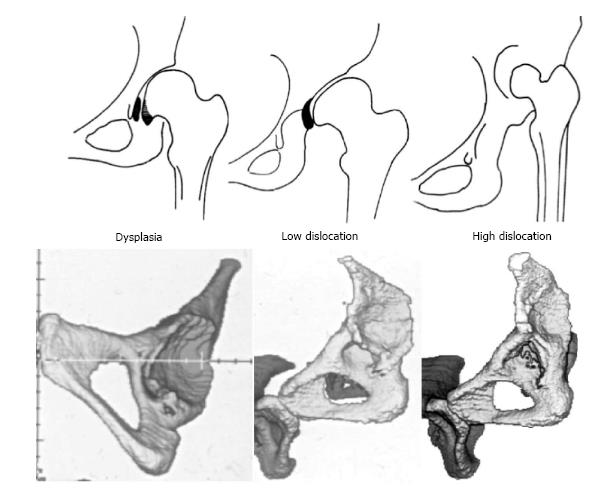
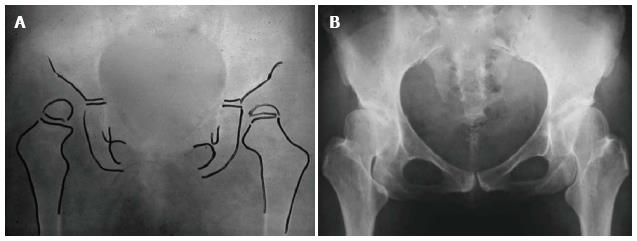
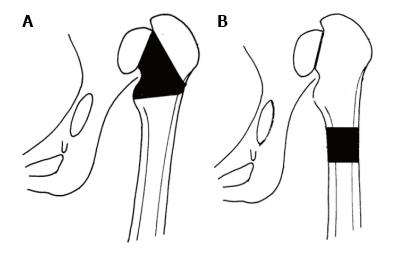
Furthermore, we recognized that for better communication, planning of treatment and evaluation of the results of different treatments, a classification system of general acceptance must be used. Weinstein had classified CHD in infancy in three radiographic types: (1) dysplasia (inclination of the acetabulum with centralized ossification centre - Shenton’s line intact); (2) subluxation (subluxed ossification centre - Shenton’s line broken); and (3) complete dislocation (ossification centre outside the acetabulum) (Figure 1). Based on that classification, we identified in adults three different CHD types of increasing severity: (1) dysplasia; (2) low dislocation; and (3) high dislocation. Depending on the type, adjustment of our surgical technique during THR is required. In dysplasia, the femoral head is contained within the original acetabulum. In low dislocation, the femoral head articulates with a false acetabulum that partially covers the true acetabulum. In high dislocation, the femoral head is migrated superiorly and posteriorly to the hypoplastic true acetabulum. The proximal part of the femur, in dysplasia, is normal. In low dislocation, the femoral neck is short, and shorter still in a high dislocation, with excessive anteversion. The diaphysis, in high dislocation, is hypoplastic with excessive narrowing of the femoral canal and has thin cortices (Figure 2).
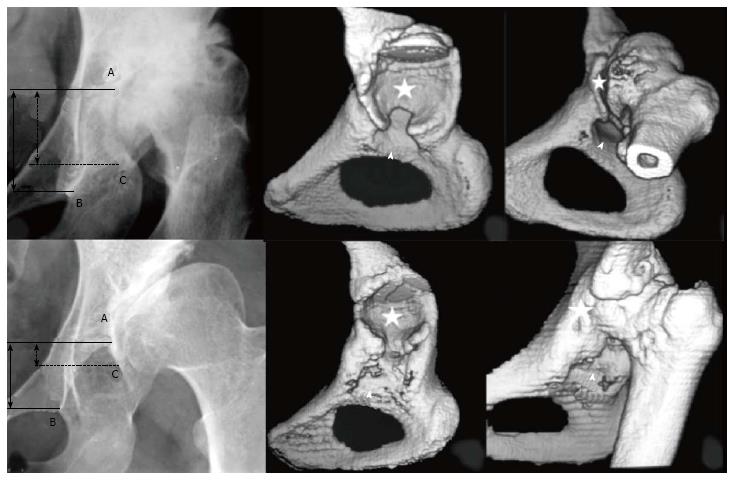
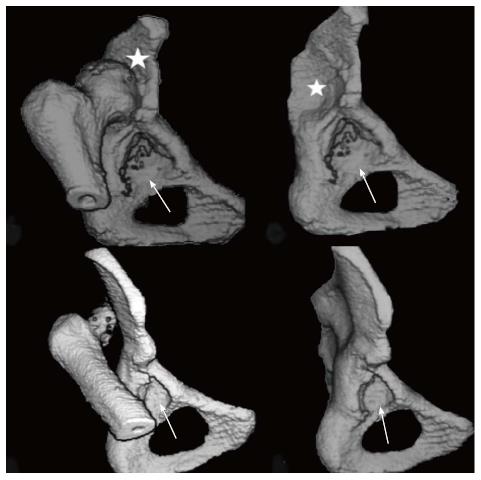
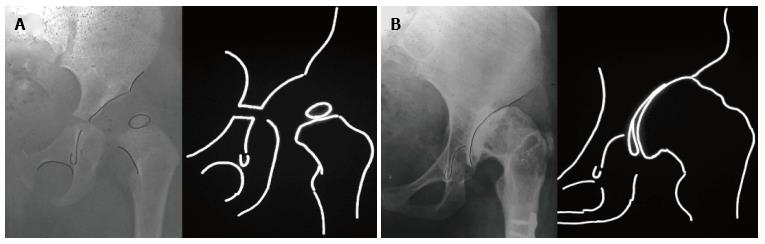
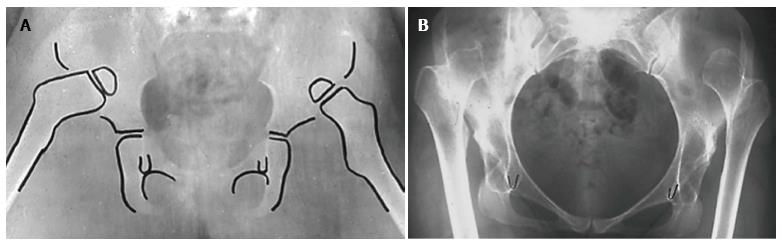
Later, in a refinement of our classification system, we further subdivided low and high dislocation. Low dislocation was subdivided into B1 and B2 subtypes, when the false acetabulum covers more or less than 50% of the true acetabulum, respectively. High dislocation was subdivided into C1 and C2 subtypes, depending on the presence or the absence of a false acetabulum, respectively (Figures 3 and 4). The lesson learned by using this classification system is that “better comprehension of the pathologic anatomy and the specific characteristics of these hips, makes their THR reconstruction easier and more successful”[1-9].
The second lesson learned is that knowledge of the natural history of CHD facilitates comprehension of the potential development and progression of the disease, which differs among the three types. This can lead to better understanding of the anatomical abnormalities found in the different types, thus facilitating preoperative planning and choice of the most appropriate management for adult patients.
In our country, before the introduction of screening systems, the majority of infant dysplastic hips remained undiagnosed until the onset of symptoms, usually at the third decade of a patient’s life. Degenerative changes progress slowly since that time and, usually, THR can be postponed until the age of 45-50 years. Patients with low dislocation, who had not received previous treatment in infancy, limp since childhood and experience pain later in their lives, usually at the age of 25-30 years. In these cases, degenerative changes develop within the false acetabulum and THR, usually becomes necessary earlier than in dysplastic hips. Patients with high dislocation and no previous treatment also limp since early childhood. Limping is more severe in patients with unilateral involvement. Natural history depends on the presence or absence of a false acetabulum. In patients with a false acetabulum pain starts early, usually around 30 years of age, while in patients without a false acetabulum pain starts much later, around the age of 40-45 years, as a consequence of muscle fatigue (Figures 5-7). In unilateral involvement, the leg-length discrepancy ranges between 4-10 cm and increases the disability of the patient. Also, the ipsilateral knee presents valgus deformity, sometimes severe, and the spine thoracolumbar scoliosis.
The indication for a THR not only depends on the degree of pain and disability, but also includes emotional parameters, given that these patients are young females with an active and productive life[10,11].
Another lesson learned is that THR is a difficult operation and should be performed by experienced surgeons and only when there is an absolute indication based on the patient’s symptoms, psychological impact, clinical findings and the potential of disease development; “Not to early, not to late”. Several technical details should be considered[9,12-17].
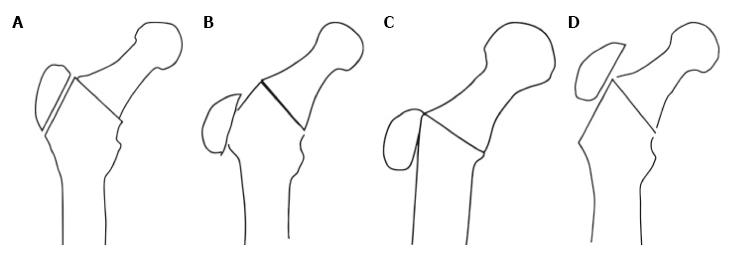
Transtrochanteric approach: Wide exposure is essential for the reconstruction, especially of hips with low and high dislocation. The lateral transtrochanteric approach was introduced by Charnley, who suggested that it would facilitate the access to the joint and the reconstruction of the disturbed anatomy of the acetabulum and the proximal femur. Additionally, lateral reattachment of the trochanter increases the abductor lever arm and minimises the reactive forces acting on the acetabulum. Four categories of the trochanteric reattachment are recognised: (1) reattachment at the original bed of trochanteric osteotomy; (2) distal reattachment in relation to its original bed, the trochanter having contact with the distal part of the original bed; (3) reattachment on the lateral femoral cortex in cases where the femoral neck was resected to the level of the lesser trochanter; and (4) reattachment proximal to its original bed (Figure 8). The ideal reattachment of the trochanter is the distal reattachment retaining contact with the distal part of the original bed. However, this is not always possible mainly due to shortened abductor muscles, an often small and malpositioned trochanter and a lengthened limb[16].
The most common complication of trochanteric osteotomy is the non-union of the trochanteric fragment. Other complications include breakage and migration of the wires, heterotopic ossification and dislocation. We learned that the complications of this exposure were less important than the benefits gained[16].
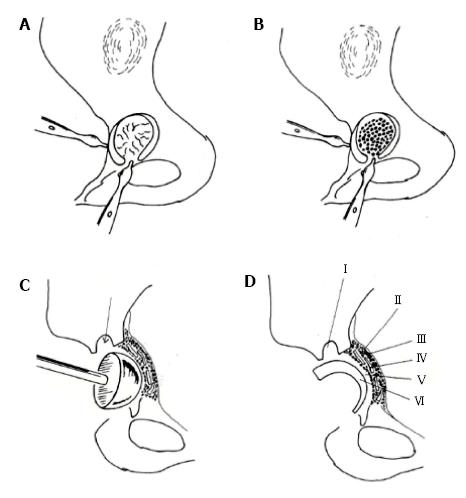
Restoration of the normal centre of rotation of the joint: Placement of the acetabular component at the level of true acetabulum is essential for restoration of the hip biomechanics and improvement of survival of the prosthesis. However, it is not always possible to achieve bony coverage of the acetabular component at this level. Two alternative techniques have been used to solve this problem. When the reamed acetabulum can provide at least 80% osseous coverage of the implant, we use an uncemented small 40-42 mm metal backed acetabular component. If this is not feasible, the cotyloplasty technique is an effective alternative. Cotyloplasty involves medialization of the acetabular floor through creation of a comminuted fracture of the entire medial wall, impaction of autogenous cancellous morselized bone grafts and implantation of a small, all-polyethylene (PE) implant, usually the offset-bore acetabular cup (Figure 9)[3,9,14]. The main mechanical advantage of this technique is that the weight-bearing area is allowed to shift to beneath the acetabular roof, while adequate anterior and posterior coverage of the cup is achieved. Moreover, the host-graft interface is biologically active, which may ensure incorporation of the graft and the anatomical placement of the cup. This, combined with carefully controlled medialization optimizes the mechanical environment and influences the long-term survival of the artificial hip.
On the other hand, augmentation of superior segmental defects with structural autograft or allograft and placement of the acetabular component in the anatomical position had been suggested by Harris et al[18]. Although the short-term results of this technique were excellent, a high failure rate after approximately 12 years has been reported[19]. This may be related to the complex pathological anatomy encountered at the level of the true acetabulum and the abnormal distribution of stresses, combined with the unfavourable long-term biological behaviour of structural grafts[3,9].
Shortening of the femur: For hips with high dislocation, shortening of the femur during THR is inevitable. We favour shortening of the femur by progressive resection of bone at the level of the femoral neck. We argue against leaving the greater trochanter in place and subtrochanteric femoral shortening osteotomy, because, in the majority of hips with high dislocation, the greater trochanter lies above the centre of rotation of the femoral head and its resection and advancement are essential (Figure 10). Besides, subtrochanteric osteotomy resembles an artificial fracture which needs additional osteosynthesis and may subsequently cause undesirable complications[9].
Special implants: Special small implants are needed. We have been using the Charnley’s offset bore cup in most of our cases. It is an extra small all-PE implant with a 35 mm face diameter, offset articular surface and approximately 10 mm PE thickness at the upper weight-bearing part, equal to that of a conventional socket, that decreases to a few millimetres in the lower part. In cases with a narrow femoral canal and short and anteverted neck, for the reconstruction of the femur we have mostly used the stainless steel Charnley CDH stems with polished surface, monoblock and collarless, and the Harris CDH stem made of CoCr, precoated at the proximal part, modular and with collar[20-22]. Currently new cementless designs are used.
Females with congenital dislocation of the hip represent a special cohort of patients with a problematic life since birth. These patients are of young age and may have pain, severe limping and deformation, major leg-length discrepancies and several psychological disorders, such as anxiety and depression, since their early childhood. We evaluated the quality of life (QoL) of 82 female patients, with low and high dislocation, followed for a minimum of 12 years after THR using clinical scores and QoL questionnaires. We concluded that THR radically improves their QoL for a long period of time. Even patients who subsequently underwent revisions had enjoyed pain relief and functional improvement for an appreciable period of time[23].
Letters from these patients, many years after surgery, show their satisfaction for the great changes in their physical and psychological status as well as their social and family life. Short excerpts from this communication are the following[24]: “My childhood was a life of torrent. My mother used to tell me that no man is going to love me. She made me feel useless. My life changed after surgeries at the age of 28. I got married and now I have a 15-year-old son. We are a happy family”; “My childhood and teenage life were very difficult, with many complexities and insecurities. I was feeling like a child of an inferior God. I took the decision to have an arthroplasty at the age of 29. Even though it was necessary to be operated again after 11 years, I am now fully active leading a normal life. I am very pleased”; “My life was an Odyssey. At school, the children were making fun of me for being so different to them because of my pelvic deformity and my movements. When I had the arthroplasties in my hips, I was 47 years old. My life changed. I look at the mirror and I do not believe my eyes. People who knew me did not recognize me. Twenty-four years have gone since I was operated and I have a normal life”.
The most suitable term for the total spectrum of congenital hip deformities is “CHD”, classified in adults into dysplasia (type A), low dislocation (type B) and high dislocation (type C). Types B and C are further subdivided in subtypes B1 and B2, and C1 and C2, respectively, depending on their different anatomic characteristics.
The three types of CHD are the main causes of secondary OA. Degenerative changes develop gradually, usually from the age of 30-35 years, causing pain and increasing functional disability over time. Knowledge of the natural history of the three types of CHD facilitates choosing the most appropriate time for THR.
The transtrochanteric approach is essential in cases with low and high dislocation and in certain dysplastic hips with great limitation of the range of motion.
Restoration of the normal centre of rotation is fundamental for the joint biomechanics and the survival of the prosthesis.
Shortening of the femur, if needed, is better to be performed at the level of the femoral neck.
In the majority of cases, special implants are needed to reconstruct the acetabulum and the femur.
The improvement of the QoL, especially in young females with high dislocation, is impressive. Most of these patients stated that after surgery they feel “like they were born gain”.
Authors would like to thank Dr. Konstantina Stathopoulou for her kind suggestions regarding the writing style of this work.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Fukiage K, Macheras GA, Zahar A S- Editor: Qiu S L- Editor: Wang TQ E- Editor: Lu YJ
| 1. | Hartofilakidis G, Babis GC, Lampropoulou-Adamidou K. Congenital Hip Disease: General Aspects, Terminology and Classification. Congenital Hip Disease in Adults. Italy: Springer-Verlag Italia 2014; 11-27. |
| 2. | Hartofilakidis G, Stamos K, Ioannidis TT. Low friction arthroplasty for old untreated congenital dislocation of the hip. J Bone Joint Surg Br. 1988;70:182-186. [PubMed] |
| 3. | Hartofilakidis G, Stamos K, Karachalios T, Ioannidis TT, Zacharakis N. Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am. 1996;78:683-692. [PubMed] |
| 4. | Hartofilakidis G. Developmental dysplasia of the hip: An unsuitable term. J Bone Joint Surg Am. 2004;86-A(2). |
| 5. | Yiannakopoulos CK, Xenakis T, Karachalios T, Babis GC, Hartofilakidis G. Reliability and validity of the Hartofilakidis classification system of congenital hip disease in adults. Int Orthop. 2009;33:353-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Yiannakopoulos CK, Chougle A, Eskelinen A, Hodgkinson JP, Hartofilakidis G. Inter- and intra-observer variability of the Crowe and Hartofilakidis classification systems for congenital hip disease in adults. J Bone Joint Surg Br. 2008;90:579-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Hartofilakidis G, Yiannakopoulos CK, Babis GC. The morphologic variations of low and high hip dislocation. Clin Orthop Relat Res. 2008;466:820-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Hartofilakidis G, Babis GC. Congenital disease of the hip. Clin Orthop Relat Res. 2009;467:578-579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Karachalios T, Hartofilakidis G. Congenital hip disease in adults: terminology, classification, pre-operative planning and management. J Bone Joint Surg Br. 2010;92:914-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Hartofilakidis G, Babis GC, Lampropoulou-Adamidou K. Epidemiology, Demographics and Natural History. Congenital Hip Disease in Adults. Italy: Springer-Verlag Italia 2014; 29-43. |
| 11. | Hartofilakidis G, Karachalios T, Stamos KG. Epidemiology, demographics, and natural history of congenital hip disease in adults. Orthopedics. 2000;23:823-827. [PubMed] |
| 12. | Hartofilakidis G, Babis GC, Lampropoulou-Adamidou K. Technical Considerations. Congenital Hip Disease in Adults. Italy: Springer-Verlag Italia 2014; 63-75. |
| 13. | Stamos KG, Karachalios T, Papagelopoulos PJ, Xenakis T, Korres DS, Koroneos E, Hartofilakidis G. Long-term mechanical stability of the impacted morselized graft-cement interface in total joint replacement: an experimental study in dogs. Orthopedics. 2000;23:809-814. [PubMed] |
| 14. | Hartofilakidis G, Stamos K, Karachalios T. Treatment of high dislocation of the hip in adults with total hip arthroplasty. Operative technique and long-term clinical results. J Bone Joint Surg Am. 1998;80:510-517. [PubMed] |
| 15. | Hartofilakidis G, Karachalios T. Total hip arthroplasty for congenital hip disease. J Bone Joint Surg Am. 2004;86-A:242-250. [PubMed] |
| 16. | Hartofilakidis G, Babis GC, Georgiades G, Kourlaba G. Trochanteric osteotomy in total hip replacement for congenital hip disease. J Bone Joint Surg Br. 2011;93:601-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Hartofilakidis G, Karachalios T, Georgiades G, Kourlaba G. Total hip arthroplasty in patients with high dislocation: a concise follow-up, at a minimum of fifteen years, of previous reports. J Bone Joint Surg Am. 2011;93:1614-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Harris WH, Crothers O, Oh I. Total hip replacement and femoral-head bone-grafting for severe acetabular deficiency in adults. J Bone Joint Surg Am. 1977;59:752-759. [PubMed] |
| 19. | Mulroy RD, Harris WH. Failure of acetabular autogenous grafts in total hip arthroplasty. Increasing incidence: a follow-up note. J Bone Joint Surg Am. 1990;72:1536-1540. [PubMed] |
| 20. | Ioannidis TT, Zacharakis N, Magnissalis EA, Eliades G, Hartofilakidis G. Long-term behaviour of the Charnley offset-bore acetabular cup. J Bone Joint Surg Br. 1998;80:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Hartofilakidis G, Georgiades G, Babis GC, Yiannakopoulos CK. Evaluation of two surgical techniques for acetabular reconstruction in total hip replacement for congenital hip disease: results after a minimum ten-year follow-up. J Bone Joint Surg Br. 2008;90:724-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Digas G, Georgiades G, Lampropoulou-Adamidou K, Hartofilakidis G. The twenty-year survivorship of two CDH stems with different design features. Eur J Orthop Surg Traumatol. 2013;23:901-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Roidis NT, Pollalis AP, Hartofilakidis GC. Total hip arthroplasty in young females with congenital dislocation of the hip, radically improves their long-term quality of life. J Arthroplasty. 2013;28:1206-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Hartofilakidis G, Babis GC, Lampropoulou-Adamidou K. Quality of Life After Total Hip Replacement. Congenital Hip Disease in Adults. Italy: Springer-Verlag Italia 2014; 131-163. |