Published online Nov 18, 2016. doi: 10.5312/wjo.v7.i11.731
Peer-review started: January 14, 2016
First decision: March 7, 2016
Revised: July 6, 2016
Accepted: August 17, 2016
Article in press: August 18, 2016
Published online: November 18, 2016
Processing time: 307 Days and 13.8 Hours
To determine whether three-dimensional (3D) reconstruction from conventional magnetic resonance imaging (MRI) is able to accurately detect a meniscal tear, and define the configuration.
Thirty-three patients’ 3T MRI scan data were collected and sagittal uni-planar 3D reconstructions performed from the preoperative MRI. There were 24 meniscal tears in 24 patients, and nine controls. All patients had arthroscopic corroboration of MRI findings. Two independent observers prospectively reported on all 33 reconstructions. Meniscal tear presence or absence was noted, and tear configuration subsequently categorised as either radial, bucket-handle, parrot beak, horizontal or complex.
Identification of control menisci or meniscal tear presence was excellent (Accuracy: observer 1 = 90.9%; observer 2 = 81.8%). Of the tear configurations, bucket handle tears were accurately identified (Accuracy observer 1 and 2 = 80%). The remaining tear configurations were not accurately discernable.
Uni-planar 3D reconstruction from 3T MRI knee scan sequences are useful in identifying normal menisci and menisci with bucket-handle tears. Advances in MRI sequencing and reconstruction software are awaited for accurate identification of the remaining meniscal tear configurations.
Core tip: Three-dimensional reconstruction from magnetic resonance imaging (MRI) is an expanding field with potentially great clinical utility, but must be applied with caution when segmenting knee meniscal tears. Tear presence or absence, and the complex configuration of bucket handle tears were accurately distinguishable. The remaining tear configurations could not be correctly identified. Advances in MRI sequencing and reconstruction software need to be made before the remaining meniscal tear configurations will be identifiable.
- Citation: Kruger N, McNally E, Al-Ali S, Rout R, Rees JL, Price AJ. Three-dimensional reconstructed magnetic resonance scans: Accuracy in identifying and defining knee meniscal tears. World J Orthop 2016; 7(11): 731-737
- URL: https://www.wjgnet.com/2218-5836/full/v7/i11/731.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i11.731
The knee menisci are vital to tibiofemoral contact mechanics[1,2] and joint longevity[3-5]. Tears thereof are common injuries[6], occurring both as traumatic tears in younger patients and degenerate tears in older paients[7,8]. Traumatic tears may adopt several different configurations[9], depending predominantly upon the mechanism and extent of injury. By contrast, degenerate tears occur mainly as cleavage tears along the horizontal plane in which myxoid meniscal degeneration is known to occur[10,11]. This variation in tear configuration and extent affects surgical planning regarding reparability or resection, and thus patient management. Accurate preoperative diagnosis is therefor important. Currently magnetic resonance imaging (MRI) is commonly used to preoperatively diagnose a meniscal tear. This however relies heavily on specialist radiological interpretation for diagnosis and adds further burden to a loaded service. Three-dimensional (3D) reconstruction from the MRI presents the data as a single alternative image for analysis. Interpretation of meniscal pathology in this 3D reconstructed meniscus is potentially simpler, as presentation of image data in three dimensions allows for better spatial relationship appreciation, easier object manipulation to view in any plane, and lessens the inferential burden on the observer.
3D meniscal reconstruction has accurately demonstrated meniscal dynamics relative to the tibial plateau[12] and shown encouraging results in tear delineation, suggesting that 3D reconstruction may be particularly beneficial in showing up radial and horizontal tears not visible on the 2D MRI[13]. Meniscal reconstruction has previously been used to investigate tibiofemoral contact[14-16], and in calculating pre- and post-meniscectomy meniscal volumes[17]. With current advancement in 3D reconstruction technology, this study aimed to determine whether 3D reconstruction of meniscal tears using current MRI protocols could accurately identify meniscal tears, and define their configuration.
Cross sectional clinical cohort study.
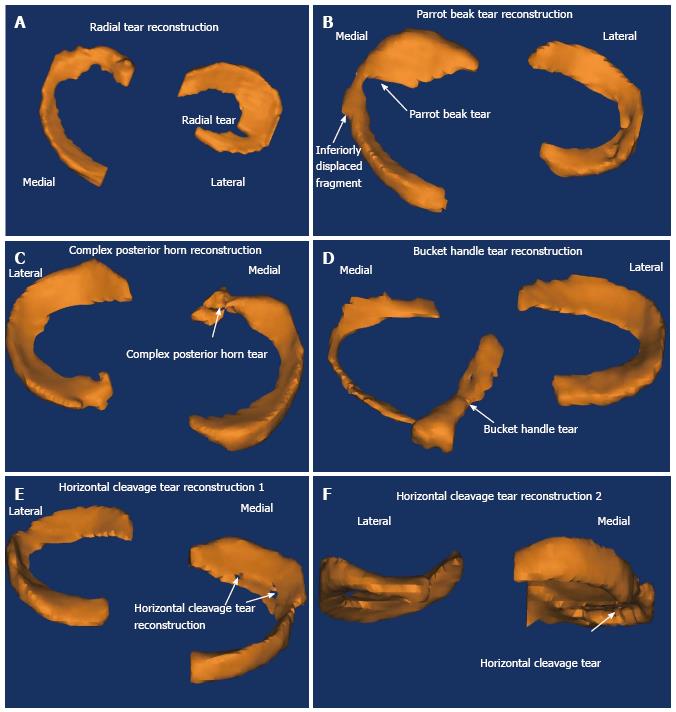
First the five common meniscal tear types were identified and categorised in groups as either radial, bucket handle (longitudinal displaced), parrot beak (oblique), cleavage (horizontal) and complex tears. Following, the operative notes of all arthroscopies undertaken on adult patients (aged over 18 years) by two experienced consultant orthopaedic surgeons at our institution were retrospectively reviewed to gather a minimum of five meniscal tears in each tear category. A further five normal menisci, defined at arthroscopy as having no tear or degeneration, were identified for each surgeon.
Subsequently the scans from these patients with the various tear configurations were retrieved for segmentation. In all cases arthroscopy was performed after preoperative MRI had indicated a potential meniscal tear. All preoperative scans were performed on a 3T MRI scanner (Philips) and reports on each by a subspecialized consultant musculoskeletal (MSK) radiologists were collected. Due to MRI data recording errors and one patient duplication, the final study population consisted of 24 meniscal tears in 24 patients, and nine control menisci.
For all cases, imaging at 3T, and using a Philips Sense extremity Knee Coil, Fast Spin Echo (FSE) sequences were used to obtain Proton Density (PD) Fat Saturated images in the sagittal, coronal and axial planes. Following, a Gradient Recall Echo (GRE) sequence was employed to again image in the sagittal plane. The Time to Repetition (TR) varied from approximately 845 ms (for the GRE) to approximately 2500-7400 ms (for the PD). The Time to Echo (TE) varied from approximately 9 ms (for the GRE) to 30 ms (for the PD). The imaging characteristics were a Field of View (FOV) of 16 cm × 16 cm; a slice thickness of 2-3 mm; an interslice gap of between 2-3.3 mm; a matrix of either 512 × 512 or 1024 × 1024 and an Echo Train Length (ETL) of 14.
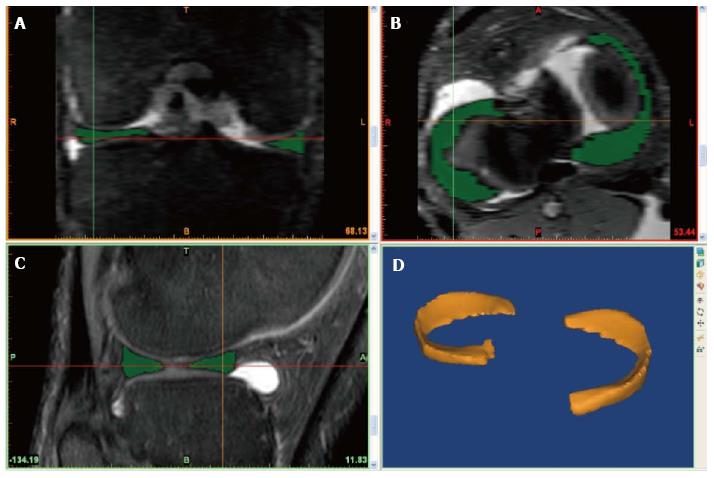
All patient MRI data for the 3T scans were imported into the Materialise Interactive Medical Control System (MIMICS) 3D reconstruction software program (Materialise, Leuven, Belgium) for subsequent reconstruction. All 33 scans were reconstructed from sagittal plane images by the lead author, segmenting both menisci for each knee scanned. This final image was then “wrapped” and stored as a finite element model for future interpretation. Each reconstruction was time consuming, taking approximately 4 h to generate the final model. In order to minimize the inaccuracies in the segmentation and reconstruction, the lead author undertook a two-day training course by the Materialise staff in using the novel software. Further, each reconstruction was reviewed for error in segmentation by a subspecialised MSK radiologist, and the adjacent uninjured meniscus reconstruction served as an innate control (Figure 1).
Two orthopaedic trainees, who were both familiar with the different types of meniscal tears, reported on the reconstructions. Prior to reporting, each observer received a separate training session using this new software and were made familiar with user functions and object manipulation, as well as normal and meniscal tear appearances in 3D. Each training session took no longer than ten minutes, as the user functions to zoom or pan and manipulate the image to view it in any desired plane are intuitive and easy to reproduce. There was hence no learning curve associated with this as the execution of each function is binary, and each surgeon was equipped with all the functions prior to undertaking the reporting.
Both trainees were blinded to the preoperative MRI and operative findings, and were blinded as to the number of tears in each configuration category. All 33 meniscal reconstructions were then brought up in random order in the MIMICS software program for independent reporting. Each observer prospectively reported their findings on a standard pro forma. Inter-observer and intra-observer repeatability were determined. Two primary assessments were made. First, tear presence vs absence was determined and subsequently the meniscal tear configuration was calculated (Figure 2).
Thirty-three patients were included in the final study, 20 were male and 13 were female. There were 14 tears in right knees and 10 tears in left knees. The 9 control patients consisted of 8 right knees and 1 left knee. Nineteen tears were in the medial meniscus and five tears were in the lateral meniscus. The mean time between MRI and arthroscopy was 4 mo (Range 1 mo to one year). All cases had arthroscopic validation of their tear configuration.
The accuracy and predicative values for detecting the presence or absence of a meniscal tear, regardless of tear configuration, were as follows.
Observer 1: The values for detecting tears presence vs absence were: Sensitivity 91.7%, specificity 88.9%, PPV 95.7%, NPV 80.0%, and accuracy 90.9%.
Observer 2: The values for detecting tears presence vs absence were: Sensitivity 87.5%, specificity 66.7%, PPV 87.5%, NPV 66.7%, and accuracy 81.8%. Both the intra- and inter-observer computed Cohen’s Kappa = 0.525, indicating a moderate degree of agreement.
Sub-classification for each tear configuration was then calculated for each observer: (1) Observer 1: Accuracy for detecting different tear configurations (Table 1); (2) Observer 2: Accuracy for detecting different tear configurations (Table 2).
| Observer 1 tear configuration identification accuracy | ||
| Number of each tear correctly identified | Accuracy | |
| Bucket handle | 4 of 5 | 80% |
| Radial | 1 of 6 | 16.7% |
| Cleavage | 3 of 5 | 60% |
| Parrot beak | 2 of 5 | 40% |
| Complex | 1 of 3 | 33.3% |
| Observer 2 tear type identification accuracy | ||
| Number of each tear correctly identified | Accuracy | |
| Bucket handle | 4 of 5 | 80% |
| Radial | 3 of 6 | 50% |
| Cleavage | 0 of 5 | 0% |
| Parrot beak | 1 of 5 | 20% |
| Complex | 2 of 3 | 66.7% |
As can be seen when comparing these results of the 3D reconstructions by meniscal tear configuration with those obtained on 2D MRI sequences from the literature in the table below, only the detection of bucket handle tears compares favourably (Table 3).
| Radial | Bucket-handle | Oblique | Horizontal cleavage | Complex | |
| Jee et al[27] | 8 of 11 (72.7%) | -1 | 3 of 5 (60.0%) | 35 of 44 (79.5%) | 18 of 22 (81.8%) |
| Jung et al[28] | 26 of 36 (72.2%) | -1 | 2 of 2 (100.0%) | 28 of 32 (87.5%) | 1 of 2 (50.0%) |
| Wright et al[29] | -1 | 25 of 39 (64.1%) | -1 | -1 | -1 |
| The present report | 1 of 6 (16.7%) | 4 of 5 (80.0%) | 2 of 5 (40.0%) | 3 of 5 (60.0%) | 1 of 3 (33.3%) |
Morphological similarities, particularly in 3D reconstruction, between certain tear types exist. As evident from the reconstructions, the primary similarities are observed in the parrot beak and radial configurations, and the complex and cleavage tear configurations. Interestingly, when combining each into a single category, the sensitivities rivaled those of the normal and bucket handle tear configurations.
Observer 1: Accuracy when combining parrot beak and radial tears (7 of 11, 63.6%), and complex and cleavage tears (6 of 8, 75%).
Observer 2: Accuracy when combining parrot beak and radial tears (7 of 11, 63.6%), and complex and cleavage tears (7 of 8, 87.5%).
The MR diagnosis of a meniscal tear relies both on signal contrast and morphology. In un- or minimally displaced tears, the fluid entering the tear provides the contrasting signal with the surrounding normal meniscus, enabling the diagnosis. In severely displaced tears, the abnormal morphology of the meniscus is the key factor, indicating a tear is present. With 3D reconstruction from the MRI, these signal contrasts are utilised to provide distinct borders during the segmentation process to highlight out the meniscus, leaving only the morphology to interpret. Theoretically then, if the increased signal is seen on the 2D images, it should be reflected in the 3D reconstruction, enabling simpler diagnosis of tear presence and morphology.
In identifying meniscal tear presence or absence, the accuracies, sensitivities and specificities, as well as positive and negative predicative values in this study were equal to those obtained from 2D MRI[18-20]. Advantages of the 3D reconstruction however include presenting the MRI data in a visuospatially simple format and enabling object viewing in any plane to aid pathological identification. Further, it does not rely on radiologic skill or significant experience for interpretation.
Investigating by meniscal tear configuration, 3D reconstruction appeared useful in identifying normal menisci (Observer 1: Accuracy = 90.9%; Observer 2: Accuracy = 81.8%), and the complex configuration of bucket handle tears (Observer 1: Accuracy = 80.0%; Observer 2: Accuracy = 80.0%). However it had a lower accuracy in determining the remaining meniscal tear configurations.
Currently the achievement of adequate fine detail in 3D reconstruction enabling differentiation between morphologically similar tears is not possible using the present standard scan protocols. As can be seen when combining the morphologically similar tears above, the accuracy rivaled that achieved for the bucket handle tear configuration. Obscurations of meniscal tear border definition arise due to inaccuracies in the MRI, and in segmentation. MRI inaccuracies may be attributed to inherent magnetic field inhomogeneities, volume averaging and limited contrast dependent on the signal-to-noise ratio (SNR) maintainable across the FOV. Presently segmentation remains user dependent, time consuming and MRI quality reliant. Accurate tear and meniscal edge definition is still user defined, despite some semi-automated functions facilitating simpler and more efficient segmentation. While these inaccuracies are present, it is not possible to accurately determine meniscal tear extension to the periphery, this having clinical implication on prediction of healing whether or not the tear extends to the white-red zone or not.
Minimising these inaccuracies will increase the MRI quality, and hence the meniscal tear definition in 3D reconstruction. The greatest inaccuracy minimisation would be achieved by eliminating the volume averaging occurring due to the interslice gaps in current clinical knee MRI sequences. Current clinical MRI knee scan protocols leads to three separate image series, only one of which may be imported and 3D reconstructed at a time. This leads to uni-planar reconstruction, as the interpolated images in the remaining two imaging planes are very pixelated and of poor quality.
Adopting an isotropic volume scan protocol for clinical knee MRI scanning eliminates the interslice gaps, as the whole volume is scanned simultaneously, producing true 3D MRI. Recently this has been investigated as an alternative to conventional knee scanning protocols, with comparable results[21-25] obtained in a shorter scanning time[26]. This has a great impact on 3D reconstruction, as the whole data volume is imported, resulting in equivalent contrast in all three-image window planes, allowing tri-planar 3D reconstructions. This tri-planar reconstruction is anticipated to have finer meniscal tear and border definition, increasing the accuracy in differentiating between the morphologically similar tears.
There are some limitations, both of the study and the practical applicability of the reconstructions, that merit discussion. The time consuming nature of the reconstructions mean that only a low number could be generated and this limits the robustness of the conclusions drawn. It also means that the real time clinical use of being able to present the 3D model on screen to the patient, however much it might aid understanding and appreciation of their pathology, is not presently possible.
The time between the MRI and arthroscopy was significant, and the potential for tear propagation or alteration of configuration exists. All patients however had arthroscopic corroboration of their MRI findings, so, for this patient cohort, there were no alterations in tear configurations, inaccurate tear assessment or false positive or negative diagnoses. Further, no differentiation between traumatic and degenerative tears was made. Although the pathophysiological processes that underpin these two tear types are distinct, as their diagnosis still relies on the separation of the tissue planes at the joint surface with synovial fluid entering the gap and altering the MR signal, this was deemed insignificant.
Lastly, longitudinal undisplaced tears were not included as one of the configurations for assessment, as the postulate was that being undisplaced, there would be too narrow a signal change for the 3D reconstruction to be able to accurately pick up the tear.
In conclusion, uni-planar 3D meniscal tear reconstruction is useful in identifying normal menisci and menisci with bucket handle tears. It however is unable to accurately report the remaining meniscal tear configurations. Significant technological advances need to be made in both MRI and 3D reconstruction, to rival 2D MRI diagnostic accuracy in defining meniscal tear configurations.
Three-dimensional (3D) imaging and reconstruction technology is becoming more prevalent as an accepted imaging technique and, with respect to the knee meniscus, is attractive in presenting the whole meniscus on a single screen, with simple user functions enabling multiplanar visualization thereof. This technology has predominantly been applied to normal menisci in evaluation of knee kinematics and contact pressures during the gait cycle. However, meniscal tears adopt several different configurations and this abnormal morphology and signal generated on the magnetic resonance imaging (MRI) may complicate the reconstructions, thereby reducing the accuracy. This study aims to investigate whether 3D reconstruction from 2D MR images may presently be used to determine both the meniscal tear presence, and configuration.
Presently the research emphasis on knee meniscus 3D reconstruction has been focused on generating models of the whole meniscus and its movement with respect to the tibial plateau during the gait cycle. This technology is being used extensively by the Osteoarthritis Initiative in the investigation of meniscal extrusion and its potential causation of osteoarthritis. No application to meniscal tear reconstruction is presently being undertaken.
To the authors’ knowledge this is the first study to determine that 3D reconstruction from 2D MRI at present standard meniscal scan sequences is useful in determining normal menisci and menisci with bucket handle tears. It cautions the application to the remaining meniscal tear configurations.
Present application of the technology to practical diagnosis of a meniscal tear presence or absence appears possible and comparable to MRI. Similarly so in applying it bucket-handle tears, but not in the remaining meniscal tear configurations. Further technological development is needed in both the MRI and 3D reconstruction technology domains in order to improve the signal and contrast ratios, and the automation in tissue border definition to create the complete model respectively. Application of an isotropic voxel scan sequence and transition from 2D to 3D MRI in clinical imaging protocols to detect knee meniscal tears will go some way to improving this. Having the 3D reconstructed images of the meniscus at hand when consulting a patient also greatly aids understanding of their anatomy and hopefully soon, their pathology also.
The authors demonstrated the accuracy for meniscal tears on 3D reconstructed MRI. Uni-planar 3D meniscal tear reconstruction is useful in identifying normal menisci and menisci with bucket handle tears. It however is unable to accurately report the remaining meniscal tear configurations. The authors present an innovative technique in order to improve 3D reconstructed magnetic resonance scans: By adopting an isotropic volume scan protocol, the whole volume is scanned simultaneously enabling true tri-planar reconstruction. This is anticipated to have finer meniscal tear and border definition, increasing the accuracy in differentiating between the morphologically similar tears.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: South Africa
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Fernandez-Fairen M, Ohishi T, Papachristou GC S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Masouros SD, McDermott ID, Amis AA, Bull AM. Biomechanics of the meniscus-meniscal ligament construct of the knee. Knee Surg Sports Traumatol Arthrosc. 2008;16:1121-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 115] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 2. | Lee JM, Allen CR, Fu , FH . Natural history of the post-meniscectomy knee. Sports Med Arthroscopy Rev. 2002;10:236-243. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Ding C, Martel-Pelletier J, Pelletier JP, Abram F, Raynauld JP, Cicuttini F, Jones G. Meniscal tear as an osteoarthritis risk factor in a largely non-osteoarthritic cohort: a cross-sectional study. J Rheumatol. 2007;34:776-784. [PubMed] |
| 4. | Englund M, Roos EM, Roos HP, Lohmander LS. Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology (Oxford). 2001;40:631-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 181] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 5. | Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum. 2003;48:2178-2187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 427] [Cited by in RCA: 468] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 6. | Hede A, Jensen DB, Blyme P, Sonne-Holm S. Epidemiology of meniscal lesions in the knee. 1,215 open operations in Copenhagen 1982-84. Acta Orthop Scand. 1990;61:435-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 94] [Article Influence: 2.7] [Reference Citation Analysis (2)] |
| 7. | Newman AP, Daniels AU, Burks RT. Principles and decision making in meniscal surgery. Arthroscopy. 1993;9:33-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 125] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Hough AJ, Webber RJ. Pathology of the meniscus. Clin Orthop Relat Res. 1990;32-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Boks SS, Vroegindeweij D, Koes BW, Hunink MM, Bierma-Zeinstra SM. Magnetic resonance imaging abnormalities in symptomatic and contralateral knees: prevalence and associations with traumatic history in general practice. Am J Sports Med. 2006;34:1984-1991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 49] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Stoller DW, Martin C, Crues JV, Kaplan L, Mink JH. Meniscal tears: pathologic correlation with MR imaging. Radiology. 1987;163:731-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 261] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 11. | Jerosch J, Castro WH, Assheuer J. Age-related magnetic resonance imaging morphology of the menisci in asymptomatic individuals. Arch Orthop Trauma Surg. 1996;115:199-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Thompson WO, Thaete FL, Fu FH, Dye SF. Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med. 1991;19:210-215; discussion 215-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 243] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 13. | Disler DG, Kattapuram SV, Chew FS, Rosenthal DI, Patel D. Meniscal tears of the knee: preliminary comparison of three-dimensional MR reconstruction with two-dimensional MR imaging and arthroscopy. AJR Am J Roentgenol. 1993;160:343-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Hao Z, Jin D, Zhang Y, Zhang J. A finite element 3D model of in vivo human knee joint based on MRI for the tibiofemoral joint contact analysis. ICDHM’07 Proceedings of the First International Conference on Digital Human Modeling. 2007;Springer, 2007: 616-622. |
| 15. | Zielinska B, Donahue TL. 3D finite element model of meniscectomy: changes in joint contact behavior. J Biomech Eng. 2006;128:115-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 113] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 16. | DeFrate LE, Sun H, Gill TJ, Rubash HE, Li G. In vivo tibiofemoral contact analysis using 3D MRI-based knee models. J Biomech. 2004;37:1499-1504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 134] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 17. | Bowers ME, Tung GA, Fleming BC, Crisco JJ, Rey J. Quantification of meniscal volume by segmentation of 3T magnetic resonance images. J Biomech. 2007;40:2811-2815. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Quinn SF, Brown TR, Szumowski J. Menisci of the knee: radial MR imaging correlated with arthroscopy in 259 patients. Radiology. 1992;185:577-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Kojima KY, Demlow TA, Szumowski J, Quinn SF. Coronal fat suppression fast spin echo images of the knee: evaluation of 202 patients with arthroscopic correlation. Magn Reson Imaging. 1996;14:1017-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Cheung LP, Li KC, Hollett MD, Bergman AG, Herfkens RJ. Meniscal tears of the knee: accuracy of detection with fast spin-echo MR imaging and arthroscopic correlation in 293 patients. Radiology. 1997;203:508-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 80] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Kijowski R, Davis KW, Woods MA, Lindstrom MJ, De Smet AA, Gold GE, Busse RF. Knee joint: comprehensive assessment with 3D isotropic resolution fast spin-echo MR imaging--diagnostic performance compared with that of conventional MR imaging at 3.0 T. Radiology. 2009;252:486-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 207] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 22. | Jung JY, Yoon YC, Kwon JW, Ahn JH, Choe BK. Diagnosis of internal derangement of the knee at 3.0-T MR imaging: 3D isotropic intermediate-weighted versus 2D sequences. Radiology. 2009;253:780-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 97] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 23. | Gold GE, Busse RF, Beehler C, Han E, Brau AC, Beatty PJ, Beaulieu CF. Isotropic MRI of the knee with 3D fast spin-echo extended echo-train acquisition (XETA): initial experience. AJR Am J Roentgenol. 2007;188:1287-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 154] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 24. | Notohamiprodjo M, Horng A, Pietschmann MF, Müller PE, Horger W, Park J, Crispin A, del Olmo JR, Weckbach S, Herrmann KA. MRI of the knee at 3T: first clinical results with an isotropic PDfs-weighted 3D-TSE-sequence. Invest Radiol. 2009;44:585-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 84] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 25. | Yao L, Pitts JT, Thomasson D. Isotropic 3D fast spin-echo with proton-density-like contrast: a comprehensive approach to musculoskeletal MRI. AJR Am J Roentgenol. 2007;188:W199-W201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Yoon YC, Kim SS, Chung HW, Choe BK, Ahn JH. Diagnostic efficacy in knee MRI comparing conventional technique and multiplanar reconstruction with one-millimeter FSE PDW images. Acta Radiol. 2007;48:869-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Jee WH, McCauley TR, Kim JM, Jun DJ, Lee YJ, Choi BG, Choi KH. Meniscal tear configurations: categorization with MR imaging. AJR Am J Roentgenol. 2003;180:93-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 28. | Jung JY, Jee WH, Park MY, Lee SY, Kim JM. Meniscal tear configurations: categorization with 3D isotropic turbo spin-echo MRI compared with conventional MRI at 3 T. AJR Am J Roentgenol. 2012;198:W173-W180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 29. | Wright DH, De Smet AA, Norris M. Bucket-handle tears of the medial and lateral menisci of the knee: value of MR imaging in detecting displaced fragments. AJR Am J Roentgenol. 1995;165:621-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 95] [Article Influence: 3.2] [Reference Citation Analysis (0)] |