Published online Oct 18, 2016. doi: 10.5312/wjo.v7.i10.657
Peer-review started: May 19, 2016
First decision: July 5, 2016
Revised: July 15, 2016
Accepted: July 29, 2016
Article in press: August 1, 2016
Published online: October 18, 2016
Processing time: 147 Days and 6.2 Hours
Posterior ankle impingement syndrome (PAIS) is a common injury in athletes engaging in repetitive plantarflexion, particularly ballet dancers and soccer players. Despite the increase in popularity of the posterior two-portal hindfoot approach, concerns with the technique remain, including; the technical difficulty, relatively steep learning curve, and difficulty performing simultaneous anterior ankle arthroscopy. The purpose of the current literature review is to provide comprehensive knowledge about PAIS, and to describe a systematic four-stage approach of the posterior two-portal arthroscopy. The etiology, clinical presentation, diagnostic strategies are first introduced followed by options in conservative and surgical management. A detailed systematic approach to posterior hindfoot arthroscopy is then described. This technique allows for systematic review of the anatomic structures and treatment of the bony and/or soft tissue lesions in four regions of interest in the hindfoot (superolateral, superomedial, inferomedial, and inferolateral). The review then discusses biological adjuncts and postoperative rehabilitation and ends with a discussion on the most recent clinical outcomes after posterior hindfoot arthroscopy for PAIS. Although clinical evidence suggests high success rates following posterior hindfoot arthroscopy in the short- and mid-term it may be limited in the pathology that can be addressed due to the technical skills required, but the systematic four-stage approach of the posterior two-portal arthroscopy may improve upon this problem.
Core tip: A systematic four-stage approach was developed to standardize technical variety of posterior two-portal hindfoot arthroscopy for the treatment of posterior ankle impingement syndrome (PAIS). After making two-portals using the “nick and spread” technique, hindfoot strictures are divided into 4 regions of interest (superolateral, superomedial, inferomedial, and inferolateral) based on the intermalleolar ligament. In each region, anatomical structures are systematically reviewed and treated in regards to the presence of mechanical impingement and inflammation. Clinical evidence suggests high success rates following arthroscopic approach in short- and mid- term follow-up. This technique can help the surgeons optimize the outcomes following two-portal hindfoot arthroscopy for PAIS.
- Citation: Yasui Y, Hannon CP, Hurley E, Kennedy JG. Posterior ankle impingement syndrome: A systematic four-stage approach. World J Orthop 2016; 7(10): 657-663
- URL: https://www.wjgnet.com/2218-5836/full/v7/i10/657.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i10.657
Posterior ankle impingement syndrome (PAIS) is a spectrum of clinical disorders characterized by posterior ankle pain during plantar flexion or hyper flexion[1]. PAIS has become more commonly recognized, particularly in athletes because of heightened awareness[2-4] and more advanced imaging[5-7]. Conservative treatment may be indicated in the early stage of PAIS, however; approximately 40% patients eventually require surgical intervention due to intractable hindfoot pain.
The traditional open surgical treatment of PAIS through a lateral or medial approach has had good results, however complication rates are high[8]. Since its introduction in 2000[1], the posterior two portal hindfoot approach has been adopted by many surgeons for treatment of PAIS. Recently, a systematic review by Zwiers et al[9] highlighted the advantages of the endoscopic approach over the open approach including lower complication rates, shorter recovery time, less blood loss, less postoperative pain, and comparable functional outcomes. However, concerns with the technique remain; including the technical difficulty, relatively steep learning curve, and difficulty performing simultaneous anterior ankle arthroscopy[3].
This review discusses the etiology of PAIS, the spectrum of clinical disorders it encompasses, its clinical presentation and management. The review provides an up-to date assessment of the clinical evidence for the treatment of PAIS and describes a systematic four-stage approach of the posterior two-portal hindfoot arthroscopy.
PAIS pathology can be due to both osseous and/or soft tissue lesions and anatomic variants (Table 1)[10]. Osseous lesions include a Stieda process (elongated protuberance)[10], pathological os trigonum (non-fused ossicle found in up to 25% of the normal adult population)[11], osteophytes, osteochondral lesion (OCL), loose bodies, chondromatosis, and subtalar coalition. In soft tissue lesions, flexor hallux longus (FHL) tenosynovitis, synovitis, impingement of the joint capsule, and impingement of the anomalous muscles[12] are described.
| Osseus lesions | Soft tissue lesions |
| Stieda process | Flexor hallux longus tenosynovitis |
| Os trigonum | Synovitis |
| Osteophytes | Impingement of the joint capsule |
| Osteochondral lesion | Impingement of the anomalous muscles |
| Loose bodies | |
| Chondromatosis | |
| Subtalar coalition |
PAIS is characterized by deep posterior ankle pain caused by plantar flexion of the ankle joint[13]. Pain is described as consistent, sharp, dull and radiating, however, it is usually hard for patients to indicate the exact location of the pain in the hindfoot. It is most commonly seen in athletes who participate in sports that require repetitive plantar flexion such as ballet dancers, soccer players, and downhill runners[14]. In these athletes PAIS may present acutely after a forced plantar flexion injury or chronically due to overuse. After an acute injury, patients have a robust inflammatory response leading to pain and swelling that manifests in the hindfoot 3-4 wk after the injury. More commonly, PAIS develops over time in these athletes because repetitive flexion causes increased compression and forces on the anatomic structures between the calcaneus and the posterior part of the distal tibia. In these athletes who present with chronic hindfoot pain, the clinician must have a heightened suspicion for PAIS as these symptoms may mimic posterior capsulitis and rheumatoid arthritis. Clinically, it is less common to see PAIS in the non-athletic population or athletes who perform plantar flexion of ankle joint less frequently. In patients who present with chronic hindfoot pain and do not engage in activities with repetitive flexion, anatomic variants may be implicated in the development of PAIS.
A full history and physical examination is critical in the diagnosis of PAIS. Physical examination should include a complete neurovascular examination as well strength and range of motion assessment. Hindfoot pain aggravated by plantar flexion of the ankle indicates a positive plantar flexion test. A negative plantar flexion test makes a diagnosis of PAIS significantly less likely, but no studies have reported on the specificity or sensitivity of the plantar flexion test in the diagnosis of PAIS. Patients may also be tender over the posteromedial (PM) aspect of the ankle joint. The clinician must pay special attention to the exact location of tenderness, as pain over the posterior tibial tendon may indicate posterior tibial tendon tenosynovitis or dysfunction and not PAIS. To further clarify the location of the pain, the clinician may passively flex and extend the great toe. If the patient is tender during passive or active ROM, it may indicate pathology involving the FHL tendon. A neurologic examination should be performed to exclude tarsal tunnel syndrome, as the pain may be caused by Valleix’s sign[15].
Standard plain X-rays[6], computed tomography (CT), and magnetic resonance imaging (MRI) are useful for diagnosis and preoperative planning[7]. In standard plain X-rays, anteroposterior (AP), mortise, and lateral views of ankle joint are commonly used. The lateral view is the most useful view to observe osseous lesions of hindfoot (e.g., Stieda process, os trigonum, osteophytes, loose bodies, chondromatosis, subtalar coalition). Recently, the posterior impingement (PIM) view has been recommended instead of a conventional lateral view for symptomatic hindfoot pain. The PIM view is a lateral, 25-degree external rotation, oblique view of the ankle, which has shown significant superior diagnostic accuracy compared with the lateral view in the detection of os trigonum[16].
Compared with radiographs, multi-slice helical CT is more useful to evaluate osseous pathologies. CT provides fine detail regarding the size, location, and number of anatomical bony abnormalities[17]. Many surgeons prefer CT to examine the osteophyte of the tibia that sometimes co-exists with PAIS[18] and thus often use it to determine whether the anterior or posterior scope would be performed[18].
MRI is more useful to evaluate soft tissue lesions of the ankle. Of note, the presence and location of anomalous muscles should be evaluated. These anomalous muscles cause PAIS, but also increase the difficulty of operative treatment[12]. The peroneus quartus is the most commonly reported anomalous muscle, with between 7% and 22% of the population having them, other anomalous muscles such as flexor digitorum accessorius longus only occur in between 1% and 8% of the population[12].
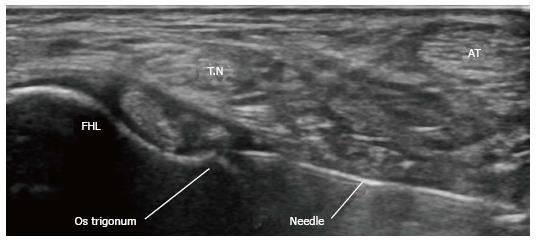
After the positive plantar flexion test is elicited, the authors prefer to evaluate the condition of the hindfoot structures using standard plain X-ray and MRI. Then, we perform an ultrasound diagnostic injection using a local anesthetic to confirm the diagnosis (Figure 1).
Conservative treatment includes rest, modification of activity, physiotherapy, anti-inflammatory drugs, and ultrasound-guided injections[19]. Ultrasound-guided injections may be useful in high-level athletes to allow them to finish the season[20]. Although no substantial evidence has published the success rate with conservative treatment[19], a small cohort study reported approximately 60% success rates following conservative treatment in PAIS[21].
Surgical management is indicated for patients following failure to address symptoms after 3 mo of conservative treatment. However, if athletic patients want to return to athletic activity promptly, then surgical intervention can be recommended early in the treatment process. Options include open treatment or arthroscopic intervention[3,22,23]. The advantages of arthroscopic procedures for PAIS are that they are less invasive, have a lower risk of postoperative complications, and shorter recovery time for returning to full activity. However, the technical difficulty and relatively steep learning curve are disadvantages[3]. Additionally, it is difficult to perform simultaneous treatments for anterior ankle pathologies using a posterior two-portal approach, while subtalar arthroscopy or conventional ankle arthroscopy with posterolateral (PL) portal are more available[24].
For patients who have isolated PAIS, the authors utilize posterior hindfoot arthroscopy. For patients who require operative intervention for both PAIS and ankle anterior pathologies (e.g., anterior impingement syndrome, anterior OCL, degenerative ankle arthritis), the authors prefer to treat anterior pathologies in the supine position with traditional anterior arthroscopic portals, then, switch to the prone position for posterior hindfoot arthroscopy.
The senior author (John G Kennedy) uses the original posterior two-portal technique, similar to the 21-point systematic surgical approach in anterior ankle arthroscopic surgery[25]. The senior author utilizes a systematic four-stage approach for posterior hindfoot arthroscopy beginning with a systematic evaluation of the anatomical structures and subsequent operative treatment for pathological abnormalities.
Typical arthroscopy equipment used in anterior ankle arthroscopy is required for posterior hindfoot arthroscopy. A 2.7/4.0 mm arthroscope with 30/70 degree viewing angle, a 3.5/4.5 mm shaver for soft tissue debridement, a 4.0 mm aggressive shaver or burr for bony resection, osteotomy, and fluoroscopy (optional) are used. Sizes of arthroscopes can be selected depending on the surgeon’s
preference. A thigh tourniquet is necessary to obtain good visualization of hindfoot anatomical structures. Additionally, an irrigation system is useful. The fluid pressure is usually set to 50-60 mmHg, and fluid flow is 0.5 L/min. Although dorsiflexion of hindfoot is usually applied for providing good visualization of the ankle and subtalar joints, a non-invasive distractor is may be applied to assist with visualization.
The patient should be positioned in the prone or sloppy lateral position. The senior authors have found that general or spinal anesthesias with a regional block are most effective. The operative foot should be elevated using a support or cushion placed underneath the lower leg, so that the leg is raised approximately 15 cm above the contralateral leg. This position can prevent contact of the arthroscope or instruments with the contralateral side in the operative procedure.
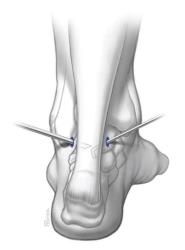
Marking anatomical landmarks and portal sites: In posterior hindfoot arthroscopy, a PL and PM portal are most commonly utilized. Prior to incision, landmarks including lateral malleoli (LM), medial malleoli (MM) and Achilles tendon should be marked using a sterile surgical marker. Portal sites should then be marked out. The portal sites are 1.0 mm anterior to the borders of Achilles tendon and at the level between the horizontal lines running from the inferior poles of MM and tip of LM (Figure 2). The sural nerve can be palpated and its course marked to avoid iatrogenic nerve injury.
Establishing portals: After all anatomic landmarks and portal sites have been identified and marked, a #11 blade should be used to make 1 cm vertical incisions at the labeled portal sites for the PM and PL portals. Then, subcutaneous blunt dissection using a mosquito clamp is performed via both portals. At this time, care must be taken to avoid damage to the sural nerve. The “nick and spread” technique is important to avoid sural neurovascular damages. A 2.7-mm arthroscope sleeve with trocar is carefully advanced via a PL portal to touch the posterior aspect of the talus by directing it towards the first interdigital web space. All instruments should be directed towards first interdigital web space to prevent iatrogenic neurovascular bundle injury in the hindfoot. Once the bone can be palpated with the trocar, it is switched out for a 2.7-mm arthroscope.
Creating working space: Initial visualization is poor because of the fat tissue located behind the posterior aspect of talus. After the shaver blade is confirmed in arthroscopic view, soft tissue is debrided to expose the intermalleolar (IM) ligament using a 3.5 or 4.0 mm aggressive shaver. The shaver blade must always be maneuvered very gently under arthroscopic visualization to avoid iatrogenic injury to healthy tissue.
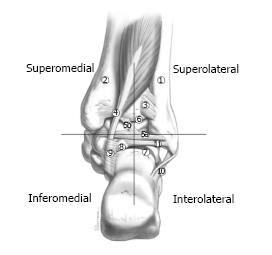
Systematic four-stage approach to visualization of the hindfoot: The systematic approach in posterior ankle arthroscopy allows for a full assessment of all structures at the posterior ankle and subtalar joint (Figure 3). The anatomic landmark for defining the quadrants is the IM ligament that has been well described previously[26,27] based on the IM ligament, the hindfoot structures are divided into 4 regions of interest (superolateral, superomedial, inferomedial, and inferolateral). The authors prefer to start the inspection from the superolateral quadrant and then proceed to the other regions in a counterclockwise fashion for right ankles and a clockwise fashion for left ankles.
This quadrant contains the posterior inferior tibiofibular ligament, transverse ligament, and IM ligament. The IM ligament may be associated with PIM[8,27]. During inspection of the superolateral quadrant, the ankle should be passively plantarflexed to see if any of these ligaments are impinged under direct visualization[26]. If impingement is present, the related structures should be debrided using a shaver or punch.
The FHL tendon and its associated fibro-osseous tunnel are found in this quadrant. Of note, the neurovascular bundle lies just medial to FHL tendon. It is therefore essential that any instruments should be maneuvered in the area lateral to FHL tendon. Additionally, surgeons should evaluate if the anomalous muscles particularly the peroneous qaurtus are present[13]. It is sometime difficult to expose the FHL tendon because of soft tissue cicatrization. In these cases, moving (passive flexion/extension) the great toe may help surgeons identify the FHL tendon.
Tenosynovitis around FHL tendon is a typical finding in patients with hindfoot pain (63% to 85%)[8,28]. By moving the great toe, impingement of the tendon in its sheath can be identified and resected using a 4.5-mm shaver. A low-lying muscle of FHL can be found, which may cause impingement between the associated bony or soft tissues. Any tenosynovitis or identified impingement should be debrided.
A Stieda process or separate os trigonum can be observed in this region. These bony structures are removed using osteotomes or shaver, with care taken to avoid causing iatrogenic cartilage lesions in the subtalar joint. The scope and shaver are switched in order to gain optimal access to achieve adequate debridement. The posterior talofibular ligament (PTFL) that attaches to these structures may need to be released, however the authors prefer to preserve as much as possible of the posterior talofibular ligament.
Once those osseous structures are removed, the arthroscope is advanced into the fibro-osseous tunnel, which allows full visualization of the FHL tendon. Any pathology restricting smooth passive movement of the FHL tendon in the fibro-osseous tunnel such as vincula, nodules, or cicatrization should be debrided and removed.
The PTFL and the calcaneofibular ligament (CFL) are found in this region. The PTFL may be thickened and hypertrophied, requiring debridement. In the case of an ankle history of chronic lateral ankle instability, attenuation or scarring of the CFL may be found. Any tenosynovitis or identified impingement should be debrided.
Intra-articular inspection of the talocrural and subtalar joints: The talocrural joint and subtalar joint are inspected following visualization of all four quadrants of the hindfoot. Both joints can be visualized using same standard portals. Ankle dorsiflexion can allow full visualization of joint surfaces, however, soft tissue distractors are sometimes used to obtain better visualization[29]. Any pathology detected including OCLs, synovitis, osteophytes, and hypertrophic capsule should be addressed. For OCLs, the authors recommend bone marrow stimulation using a microfracture pic or drilling to produce fibrocartilage repair tissue.
Biologics including platelet-rich plasma (PRP) and concentrated bone marrow aspirate (CBMA) may be used at the time of the surgery. These biologic augments are becoming recognized as promising adjuvants that may improve the quality of regenerative tissue and decrease inflammatory responses[30]. For PAIS, PRP and CBMA are injected into the degenerative tendon or bed of the lesion after irrigation water is stopped. The authors also recommend injecting these biological adjuvants into the joint after the wound is closed to limit the inflammatory response.
A compression bandage is applied after surgery and patients are allowed to be weightbearing as tolerated immediately after surgery. Patients may also begin ranging their ankle as tolerated. The goal of early ROM and weightbearing is to prevent post-operative stiffness and hopefully limit the delay in return to sport[13,30]. Typically, ankle immobilization is not necessary, unless patients had more significant osseous injury, which may require modifications of the above protocol.
Several clinical studies have reported good short-term clinical results following posterior two-portal hindfoot arthroscopy for PAIS (Table 2)[28,29,31-41]. A majority of studies have reported post-operative American Orthopaedic Foot and Ankle Society (AOFAS) Scores greater than 85[28,29,31-34,36,37,39,41] at short-term follow-up. A recent systematic review by Zwiers et al[9] demonstrated that the mean time to return to full activity was on average 11.3 wk (5.9-12.9 wk) following arthroscopic treatment. Complication rates after posterior hindfoot arthroscopy were also low with 1.8% of patients suffering a major complication and 5.4% of patients suffering a minor complication[9]. However, the current literature is limited by long-term follow-up studies evaluating the outcomes after posterior hindfoot arthroscopy for PAIS.
| Ref. | Year | No. of cases (n) | LoE | Follow-up (mo) | Primary outcome measure | Pre-operative score | Post-operative score | Return to sport (wk) |
| Jerosch et al[32] | 2006 | 10 | IV | 28 (6-61) | AOFAS | 43 | 87 | 12 |
| Tey et al[33] | 2007 | 15 | IV | 3 (15-63) | AOFAS | 84.4 | 98.5 | 14.1 |
| Horibe et al[34] | 2008 | 11 | IV | 33.8 (12-58) | AOFAS | 71 | 99 | 12 |
| Scholten et al[28] | 2008 | 55 | IV | 38 (24-54) | AOFAS | 71.1 | 90 | 18.9 |
| Willits et al[31] | 2008 | 16 | IV | 3 (6-74) | AOFAS | N/A | 91 | 63 |
| Calder et al[35] | 2010 | 27 | IV | 23 (15-49) | N/A | N/A | N/A | 5.9 |
| Noguchi et al[36] | 2010 | 12 | IV | 9.7 (6-14) | AOFAS | 68 | 98.3 | 5.9 |
| Galla et al[37] | 2011 | 30 | IV | 9.7 (6-14) | AOFAS | 60 | 90 | N/A |
| Ogut et al[38] | 2011 | 14 | IV | 31.6 (8-75) | AOFAS | 53.6 | 84.2 | 30.6 |
| Nikisch et al[39] | 2012 | 80 | IV | 15.4 (5-59) | N/A | N/A | N/A | N/A |
| van Dijk et al[29] | 2009 | 55 | IV | 90 (24-480) | AOFAS | 75 | 90 | N/A |
| Lopez-Valerio et al[40] | 2015 | 20 | IV | 78.6 (24-120) | VAS | 7.5 | 0.8 | 6.7 |
| Dinato et al[41] | 2015 | 17 | III | N/A | AOFAS | 62.9 | 92.3 | 15.6 |
| 15 | 67.9 | 94 | 16.3 |
PAIS is a clinical spectrum of both soft tissue and osseous pathology that is common in athletes who repetitively plantar flex their ankle. Patients who do not respond to conservative management may require operative intervention. While open treatments have showed good success in the short-term for PAIS, posterior hindfoot arthroscopy may lead to equivalent outcomes with less morbidity. Performing two-portal hindfoot arthroscopy in the described systematic four-stage approach allows for standardized evaluation of the anatomic structures of the hindfoot and ultimately to address any pathology that may be present. Clinical outcomes after posterior hindfoot arthroscopy for PAIS are very good in the short-term with low complication rates, however future long-term studies are warranted.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Anand A, Fernandez-Fairen M S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 462] [Cited by in RCA: 335] [Article Influence: 13.4] [Reference Citation Analysis (1)] |
| 2. | van Dijk CN, van Bergen CJ. Advancements in ankle arthroscopy. J Am Acad Orthop Surg. 2008;16:635-646. [PubMed] |
| 3. | Coetzee JC, Seybold JD, Moser BR, Stone RM. Management of Posterior Impingement in the Ankle in Athletes and Dancers. Foot Ankle Int. 2015;36:988-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Nault ML, Kocher MS, Micheli LJ. Os trigonum syndrome. J Am Acad Orthop Surg. 2014;22:545-553. [PubMed] |
| 5. | Sofka CM. Posterior ankle impingement: clarification and confirmation of the pathoanatomy. HSS J. 2010;6:99-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Wiegerinck JI, Vroemen JC, van Dongen TH, Sierevelt IN, Maas M, van Dijk CN. The posterior impingement view: an alternative conventional projection to detect bony posterior ankle impingement. Arthroscopy. 2014;30:1311-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Hayashi D, Roemer FW, D’Hooghe P, Guermazi A. Posterior ankle impingement in athletes: Pathogenesis, imaging features and differential diagnoses. Eur J Radiol. 2015;84:2231-2241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Hamilton WG, Geppert MJ, Thompson FM. Pain in the posterior aspect of the ankle in dancers. Differential diagnosis and operative treatment. J Bone Joint Surg Am. 1996;78:1491-1500. [PubMed] |
| 9. | Zwiers R, Wiegerinck JI, Murawski CD, Smyth NA, Kennedy JG, van Dijk CN. Surgical treatment for posterior ankle impingement. Arthroscopy. 2013;29:1263-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Maquirriain J. Posterior ankle impingement syndrome. J Am Acad Orthop Surg. 2005;13:365-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 81] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Lawson JP. Symptomatic radiographic variants in extremities. Radiology. 1985;157:625-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 46] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Best A, Giza E, Linklater J, Sullivan M. Posterior impingement of the ankle caused by anomalous muscles. A report of four cases. J Bone Joint Surg Am. 2005;87:2075-2079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Smyth NA, Murawski CD, Levine DS, Kennedy JG. Hindfoot arthroscopic surgery for posterior ankle impingement: a systematic surgical approach and case series. Am J Sports Med. 2013;41:1869-1876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Smyth NA, Zwiers R, Wiegerinck JI, Hannon CP, Murawski CD, van Dijk CN, Kennedy JG. Posterior hindfoot arthroscopy: a review. Am J Sports Med. 2014;42:225-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 15. | Umans H. Ankle impingement syndromes. Semin Musculoskelet Radiol. 2002;6:133-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Wiegnerinck JI, Kerkhoffs GMM, Struijs PAA, van Dijk CN. The posterior impingement-view: An alternative conventional projection to detect bony posterior ankle impingement. Arthroscopy. 2014;30:1311-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Burghardt AJ, Link TM, Majumdar S. High-resolution computed tomography for clinical imaging of bone microarchitecture. Clin Orthop Relat Res. 2011;469:2179-2193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 184] [Cited by in RCA: 186] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 18. | Niek van Dijk C. Anterior and posterior ankle impingement. Foot Ankle Clin. 2006;11:663-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Ribbans WJ, Ribbans HA, Cruickshank JA, Wood EV. The management of posterior ankle impingement syndrome in sport: a review. Foot Ankle Surg. 2015;21:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 20. | Roche AJ, Calder JD, Lloyd Williams R. Posterior ankle impingement in dancers and athletes. Foot Ankle Clin. 2013;18:301-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Hedrick MR, McBryde AM. Posterior ankle impingement. Foot Ankle Int. 1994;15:2-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 101] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Marumoto JM, Ferkel RD. Arthroscopic excision of the os trigonum: a new technique with preliminary clinical results. Foot Ankle Int. 1997;18:777-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 67] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Allegra F, Maffulli N, Cerza F, Delianni E. Postero-medial approach procedure in the supine position for one-step anterior and posterior ankle arthroscopy. Sports Med Arthrosc. 2009;17:185-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Ferkel RD. In which position do we perform arthroscopy of the hindfoot--supine or prone? Commentary on an article by Florian Nickisch, MD, et al.: “Postoperative complications of posterior ankle and hindfoot arthroscopy”. J Bone Joint Surg Am. 2012;94:e33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Ferkel RD, Fischer SP. Progress in ankle arthroscopy. Clin Orthop Relat Res. 1989;240:210-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 37] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Golanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, van Dijk CN. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010;18:557-569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 212] [Cited by in RCA: 229] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 27. | Oh CS, Won HS, Hur MS, Chung IH, Kim S, Suh JS, Sung KS. Anatomic variations and MRI of the intermalleolar ligament. AJR Am J Roentgenol. 2006;186:943-947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 28. | Scholten PE, Sierevelt IN, van Dijk CN. Hindfoot endoscopy for posterior ankle impingement. J Bone Joint Surg Am. 2008;90:2665-2672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 92] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 29. | van Dijk CN, de Leeuw PA, Scholten PE. Hindfoot endoscopy for posterior ankle impingement. Surgical technique. J Bone Joint Surg Am. 2009;91 Suppl 2:287-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 30. | Cassano JM, Kennedy JG, Ross KA, Fraser EJ, Goodale MB, Fortier LA. Bone marrow concentrate and platelet-rich plasma differ in cell distribution and interleukin 1 receptor antagonist protein concentration. Knee Surg Sports Traumatol Arthrosc. 2016; Feb 1; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 207] [Article Influence: 29.6] [Reference Citation Analysis (1)] |
| 31. | Willits K, Sonneveld H, Amendola A, Giffin JR, Griffin S, Fowler PJ. Outcome of posterior ankle arthroscopy for hindfoot impingement. Arthroscopy. 2008;24:196-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 32. | Jerosch J, Fadel M. Endoscopic resection of a symptomatic os trigonum. Knee Surg Sports Traumatol Arthrosc. 2006;14:1188-1193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Tey M, Monllau JC, Centenera JM, Pelfort X. Benefits of arthroscopic tuberculoplasty in posterior ankle impingement syndrome. Knee Surg Sports Traumatol Arthrosc. 2007;15:1235-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 34. | Horibe S, Kita K, Natsu-ume T, Hamada M, Mae T, Shino K. A novel technique of arthroscopic excision of a symptomatic os trigonum. Arthroscopy. 2008;24:121.e1-121.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 35. | Calder JD, Sexton SA, Pearce CJ. Return to training and playing after posterior ankle arthroscopy for posterior impingement in elite professional soccer. Am J Sports Med. 2010;38:120-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 70] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 36. | Noguchi H, Ishii Y, Takeda M, Hasegawa A, Monden S, Takagishi K. Arthroscopic excision of posterior ankle bony impingement for early return to the field: short-term results. Foot Ankle Int. 2010;31:398-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 37. | Galla M, Lobenhoffer P. Technique and results of arthroscopic treatment of posterior ankle impingement. Foot Ankle Surg. 2011;17:79-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 38. | Ogut T, Ayhan E, Irgit K, Sarikaya AI. Endoscopic treatment of posterior ankle pain. Knee Surg Sports Traumatol Arthrosc. 2011;19:1355-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 39. | Nickisch F, Barg A, Saltzman CL, Beals TC, Bonasia DE, Phisitkul P, Femino JE, Amendola A. Postoperative complications of posterior ankle and hindfoot arthroscopy. J Bone Joint Surg Am. 2012;94:439-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 104] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 40. | López Valerio V, Seijas R, Alvarez P, Ares O, Steinbacher G, Sallent A, Cugat R. Endoscopic repair of posterior ankle impingement syndrome due to os trigonum in soccer players. Foot Ankle Int. 2015;36:70-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 41. | Dinato MC, Luques IU, Freitas Mde F, Pereira Filho MV, Ninomiya AF, Pagnano RG, Etchebehere M. Endoscopic treatment of the posterior ankle impingement syndrome on amateur and professional athletes. Knee Surg Sports Traumatol Arthrosc. 2016;24:1396-1401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |