Published online Aug 18, 2015. doi: 10.5312/wjo.v6.i7.513
Peer-review started: March 3, 2015
First decision: April 10, 2015
Revised: May 12, 2015
Accepted: June 1, 2015
Article in press: June 2, 2015
Published online: August 18, 2015
Processing time: 170 Days and 12.9 Hours
AIM: To evaluate the management, clinical outcome and cost implications of three different treatment regimes for simple elbow dislocations.
METHODS: Following institutional board approval, we performed a retrospective review of all consecutive patients treated for simple elbow dislocations in a Level I trauma centre between January 2008 and December 2010. Based on the length of elbow immobilisation (LOI), patients were divided in three groups (Group I, < 2 wk; Group II, 2-3 wk; and Group III, > 3 wk). Outcome was considered satisfactory when a patient could achieve a pain-free range of motion ≥ 100° (from 30° to 130°). The associated direct medical costs for the treatment of each patient were then calculated and analysed.
RESULTS: We identified 80 patients who met the inclusion criteria. Due to loss to follow up, 13 patients were excluded from further analysis, leaving 67 patients for the final analysis. The mean LOI was 14 d (median 15 d; range 3-43 d) with a mean duration of hospital engagement of 67 d (median 57 d; range 10-351 d). Group III (prolonged immobilisation) had a statistically significant worse outcome in comparison to Group I and II (P = 0.04 and P = 0.01 respectively); however, there was no significant difference in the outcome between groups I and II (P = 0.30). No statistically significant difference in the direct medical costs between the groups was identified.
CONCLUSION: The length of elbow immobilization doesn’t influence the medical cost; however immobilisation longer than three weeks is associated with persistent stiffness and a less satisfactory clinical outcome.
Core tip: Our study demonstrates that prolonged immobilisation following simple elbow dislocations may lead to detrimental effects. We therefore stress the need for increased vigilance to the duration of immobilisation and that every effort should be taken to ensure that without associated fractures, the elbow should not be immobilised for more than three weeks. In addition, our study supports that the direct medical cost from treating these injuries may be substantial regardless of the type of treatment, and this should be known both by commissioners and providers of health care.
- Citation: Panteli M, Pountos I, Kanakaris NK, Tosounidis TH, Giannoudis PV. Cost analysis and outcomes of simple elbow dislocations. World J Orthop 2015; 6(7): 513-520
- URL: https://www.wjgnet.com/2218-5836/full/v6/i7/513.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i7.513
Elbow dislocations represent the second most common dislocation in the adult population following shoulder dislocation, and the most common type of dislocation in the paediatric population[1]. In the United States population alone, the incidence of elbow dislocation has been reported as high as 5.21 per 100000 habitants, with males 10-19 years of age, having the highest risk for dislocation[2]. Seventeen per cent of these dislocations are associated with fractures[3], with nearly half of them occurring in sports[2]. Falls represent the primary mechanism of injury being responsible for 56.5% of elbow dislocations overall[2].
The most commonly used classification system of elbow dislocation is based on the presence of concomitant fractures in the region. Simple dislocations are characterised by the absence of fractures (except from avulsion fractures)[4], whereas complex dislocations are those accompanied by fractures[5,6]. The terrible triad describes a complex posterior dislocation with an intra-articular fracture of the radial head and of the coronoid process[6]. Elbow dislocations are also defined by the direction and topography of the dislocated parts[7].
To date, there is no general consensus regarding the protocol of management of simple elbow dislocations with different protocols being suggested. These include surgical treatment with exploration and repair of the joint ligaments; non-surgical treatment with immobilisation of the elbow joint (varying from few days to more than 3 wk)[5,8-14]; and non-surgical, functional treatment with just a short period of immobilisation of only a few days[5,9-13]. The primary functional outcome has been defined as achieving early active motion within the limits of pain with or without the use of a sling or a hinged brace[5,10].
Numerous complications of simple elbow dislocation have been described including neurovascular injury, joint instability, heterotopic ossification, occult distal radio-ulnar joint disruption and post-traumatic stiffness, most commonly defined as an arc of elbow motion less than 100°[3,5,15-18]. Biomechanical studies have shown that arcs of motion between 30° to 130° are required for most daily activities[19] and that a loss of 50° in the arc of motion, can cause up to an 80% loss of function[18].
Limited information is available with regards to the cost of the management of simple elbow dislocations. To the best of our knowledge, direct medical cost pertaining to National Health Service (NHS) including hospitalisation, imaging, outpatient follow-ups, need for physiotherapy and medication, have not been previously reported.
We hypothesized that prolonged elbow immobilisation (longer than three weeks) yields inferior outcomes. Thereafter, the purpose of this study was to determine the optimal length of elbow immobilisation (LOI) following a simple elbow dislocation. Direct medical costs were also determined.
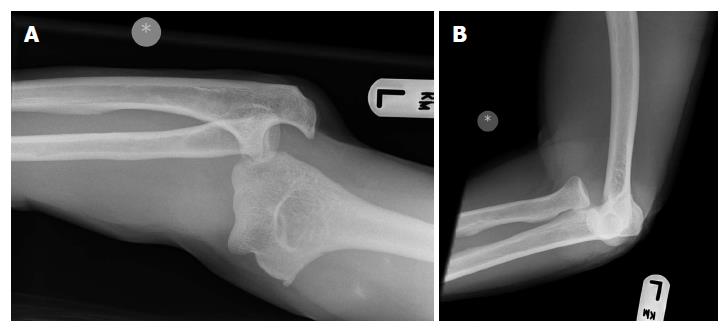
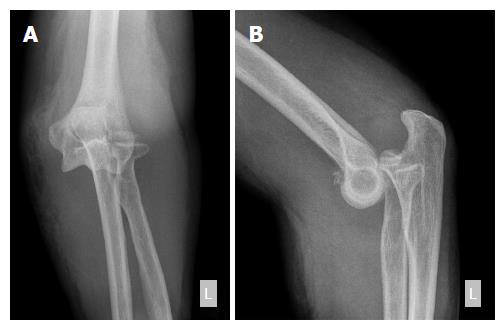
Following institutional board approval (Leeds Teaching Hospitals Institutional Review Board; ID3050; 23/11/ 2010), we performed a retrospective review of all consecutive patients treated for elbow dislocations in a large United Kingdom Level I trauma centre between January 2008 and December 2010. Inclusion criteria comprised of skeletally mature patients with clinically and/or radiologically confirmed acute “simple” elbow dislocations, having at least one year of follow-up. “Simple” dislocation were defined as dislocations that involved soft tissue disruption (Figure 1)[4]. Exclusion criteria included: associated fractures, with the exception of avulsion fractures (“complex” elbow dislocations; Figure 2); open wounds requiring debridement in the operating room; and patients with inadequate follow-up, defined as patients not attending three consecutive appointments at the outpatients clinic, or being followed up by another institution.
All patients were managed at the emergency department according to a standardised protocol. After a careful clinical and radiological evaluation, reduction was attempted under analgesia and conscious sedation or administration of Nitrous Oxide and Oxygen (Entonox®). If the dislocation was obvious and access to radiography was expected to significantly prolong time to reduction, reduction was performed before radiographs were obtained in order to relief the pressure to the soft tissues, thus reducing the risk of neurovascular injury. In case of failed closed reduction, the elbow was reduced in theatres under general anaesthetic. Once reduction was achieved, the stability of the joint and the neurovascular status were checked and documented, and the elbow was immobilised with a backslap and a collar and cuff. Finally, the patients were discharged and a follow-up appointment was arranged, or admitted where indicated. Further imaging [computed tomography (CT) and/or magnetic resonance imaging (MRI)], was performed only in patients with high clinical suspicion of occult fractures and/or complex injury patterns.
Patient demographics including age, gender, mechanism of injury, side and type of dislocation[20], method of treatment, time to mobilisation, clinical outcome, complications, secondary procedures, outpatient reviews, need for physiotherapy and time of discharge from the clinic were recorded.
The decision for the LOI and the need for formal physiotherapy were guided purely by the surgeon’s preference and indirectly by the compliance of patients to attend their allocated appointments. Based on the LOI, patients were divided into three groups (Group I, < 2 wk of immobilisation; Group II, 2-3 wk of immobilisation; and Group III, > 3 wk of immobilisation). The major cause of the prolonged LOI of patients in Group III was the lack of adherence to their scheduled outpatient trauma clinic appointments. The criteria for discharge from physiotherapy were the ability to perform daily living activities, an achievement of satisfactory arc of elbow motion (30° to 130°), or the reach to a plateau in range of motion despite continuing physiotherapy and home exercises. In terms of the clinical outcome, a good/satisfactory result was defined as the achievement of a range of motion ≥ 100° (from 30° to 130°)[19]. If a residual deficit in elbow motion was evident or if the patient reported any significant post-traumatic stiffness, outcome was considered poor/unsatisfactory and the patient was referred back to the treating surgeon.
The associated direct medical costs for the treatment of each patient were calculated and analysed. The costs represent the actual treatment that each patient received, including admission costs where applicable, hospital stay, investigations, outpatient attendances and physiotherapy sessions. The cost of each individual entry was obtained from the appropriate department (Trauma and Orthopaedics finance department and inter-provider tariff list), (Table 1). Costs were given in GPB (£).
| Category | Item | Cost (£) |
| Hospital Services | A and E attendance leading to admission | 95 |
| A and E attendance not leading to admission | 76 | |
| Minor Injuries leading to admission | 34 | |
| Minor Injuries not leading to admission | 42 | |
| Walk in centre leading to admission | 31 | |
| Walk in centre not leading to admission | 34 | |
| Theatre session (including recovery) | 880 | |
| Hospitalisation/day | Acute Care Adult wards admission per day | 269 |
| Follow-up | Outpatient clinic (new) | 116 |
| Outpatient clinic (follow-up) | 93 | |
| Support Services | Physiotherapy/session in clinic | 34 |
| Radiology | X-ray | 59.5 |
| Computed tomography scan | 225 | |
| Magnetic resonance imagingscan | 280 | |
| Radiographer per twenty minutes clinic visit (includes A and E) | 13 |
This was undertaken using IBM SPSS Statistics version 22.0 software (SPSS inc., Chicago, IL). Continuous data were analysed for differences using a two-tailed independent samples t-test, whereas for parametric data a χ2 was used to examine associations between variables. Yates’ correction was applied where appropriate and confidence intervals were calculated when necessary. A P-value < 0.05 was considered significant.
Eighty consecutive patients met the inclusion criteria and were included in the study. The mean age was 36.49 years (median: 32 years; SD 15.68 years). Fifty-one patients in the cohort were male (63.8%), and 33 dislocations (41.3%) involved the right side. The most common mechanism of injury was fall to an outstretched hand from a standing height (30 patients, 37.5%), followed by sport related injuries (26 patients, 32.5%). Common sports associated with the elbow injuries sustained included: rugby (eight patients), football (six patients), skateboarding (three patients), biking and kickboxing (two patients respectively). The rest of the patients were involved in different sports (acrobatics, cricket, rollerblading, rounders and ice-skating). Eighteen patients (22.5%) sustained their injuries following a fall from height, three patients (3.8%) were assaulted and three patients (3.8%) were involved in road traffic accidents.
Posterior or posterior lateral dislocations were the most frequent presentations (63 patients, 78.8%). Medial or posterior medial dislocation was evident in six patients (7.5%), whereas lateral dislocation was diagnosed in three patients (3.8%). In eight patients (10.0%) the direction of dislocation was not documented due to the fact that the reduction of the dislocated joint was performed as an emergency procedure with no pre-reduction radiographic imaging being available.
Thirteen patients had inadequate follow-up (16.3%) and were therefore excluded from the final analysis of the study, leaving 67 patients who formed the study cohort. Group I consisted of 26 patients (median LOI 6 d; range 3-11 d), Group II of 27 patients (median LOI 16 d; range 15-21 d) and Group III of 14 patients (median LOI 23 d; range 22-43 d). The three groups were comparable in terms of age, gender, side, type of dislocation, need for hospital admission and length of follow-up. Table 2 summarises the demographic details and the treatment course according to LOI.
| Group I | Group II | Group III | |
| No. of patients | 26 | 27 | 14 |
| Age (yr) | 34.80 ± 15.04 | 41.36 ± 17.84 | 35.41 ± 12.23 |
| Median: 30 | Median: 37 | Median: 37 | |
| Male/female | 18/8 | 17/10 | 8/6 |
| Right/left | 12/14 | 9/18 | 7/7 |
| No. of patients admitted | 5 (19%) | 3 (11%) | 3 (21%) |
| LOS (h) | 29.59 ± 19.41 | 37.42 ± 36.28 | 33.07 ± 15.03 |
| Range: 19-68 | Range: 15-79 | Range: 17-46 | |
| Patients referred to physiotherapy | 21 | 20 | 11 |
| Patients seen by physiotherapy | 14 | 17 | 5 |
| No. of physiotherapy sessions | 2.43 ± 0.76 | 2.76 ± 1.60 | 2.60 ± 1.34 |
| Median: 2 | Median: 2 | Median: 2 | |
| No. of clinic appointments | 3.31 ± 1.72 | 3.15 ± 1.10 | 3.21 ± 1.48 |
| Median: 3 | Median: 3 | Median: 3 | |
| Time of follow-up (d) | 59.00 ± 38.75 | 67.32 ± 62.62 | 81.66 ± 58.80 |
| Median: 53 | Median: 58 | Median: 62 | |
| Time to mobilisation (d) | 5.82 ± 3.57 | 16.69 ± 4.32 | 24.37 ± 8.97 |
| Median: 6 | Median: 16 | Median: 23 | |
| Good outcome | 21 patients | 23 patients | 6 patients |
Four patients (6.0%) underwent a closed reduction of the dislocation under general anaesthesia (two from Group I and two from Group II). Ten patients (14.9%) were admitted for social reasons. No statistical significant difference was recorded regarding the length of follow-up in the three groups (Table 3). Patients from Group I and Group II had a significantly better outcome compared to Group III, but we did not detect any difference between the first two groups (Table 3). No patient re-attended the emergency department of our institution with a recurrent dislocation within 12 mo from the initial injury.
| Variable | Group I vs Group II | Group I vs Group III | Group IIvs Group III | Test | |||
| P | 95%CI | P | 95%CI | P | 95%CI | ||
| Gender | 0.630 | 0-3.841 | 0.6771 | 0-3.841 | 0.717 | 0-3.841 | χ2 test |
| Age | 0.155 | -15.66-2.56 | 0.898 | -10.09-8.88 | 0.271 | -4.83-16.73 | t-test |
| Side | 0.340 | 0-3.841 | 0.816 | 0-3.841 | 0.300 | 0-3.841 | χ2 test |
| Admission | 0.6591 | 0-3.841 | 0.8681 | 0-3.841 | 0.6741 | 0-3.841 | χ2 test |
| Follow-up | 0.541 | -37.69-20.02 | 0.143 | -54.32-8.17 | 0.485 | -55.13-26.65 | t-test |
| Outcome | 0.669 | 0-3.841 | 0.0371 | 0-3.841 | 0.0141 | 0-3.841 | χ2 test |
| Medical Costs | 0.200 | -98.62-460.17 | 0.401 | -215.08-526.57 | 0.884 | -368.78-318.72 | t-test |
Patients in Group III were more likely not to attend their scheduled physiotherapy appointments compared to Groups I and II (P = 0.23 and P = 0.02 respectively). Though, there was no difference in the number of patients referred to physiotherapy by the treading surgeon, or the number of physiotherapy sessions attended by the patients in all groups.
With regards to the outcome, 17 patients (25.4%) were recorded as having an unsatisfactory outcome (Group I: 5 patients; Group II: 4 patients; Group III: 8 patients). Two patients suffered from post-traumatic neurapraxia (median nerve: one patient in Group II; ulnar nerve: one patient in Group I), which has however improved during the follow-up period.
The direct medical cost per patient according to treatment used was in Group I £1184, in Group II £1005, and in Group III and £1068. The costs were then further broken down to the main components that contributed to the total cost (Tables 4 and 5). Analysis of the total costs per patient failed to indicate any statistically significant difference between the three groups.
| Group I | Group II | Group III | |
| No. of X-rays | 8.38 ± 4.57 | 6.48 ± 2.53 | 7.93 ± 4.58 |
| Median: 7 | Median: 6 | Median: 7 | |
| CT scans | 2 patients | 1 patient | 1 patient |
| MRI scans | 1 patient | - | - |
| Need for theatre reduction | 2 patients | 2 patients | - |
| Treatment description | Group I | Group II | Group III |
| Hospital1 | 219.77 ± 318.27 | 197.62 ± 398.65 | 174.79 ± 204.79 |
| Median: 76.00 | Median: 76.00 | Median: 76.00 | |
| Radiology | 590.12 ± 334.96 | 424.96 ± 156.73 | 539.36 ± 350.21 |
| Median: 528.00 | Median: 396.00 | Median: 429.00 | |
| Outpatients | 330.62 ± 158.96 | 315.78 ± 102.21 | 321.93 ± 137.35 |
| Median: 302.00 | Median: 302.00 | Median: 203.00 | |
| Physiotherapy | 44.46 ± 44.98 | 59.19 ± 62.97 | 31.57 ± 8.97 |
| Median: 68.00 | Median: 68.00 | Median: 0 | |
| Total cost of treatment | 1184.96 ± 534.82 | 1004.19 ± 477.67 | 1067.64 ± 641.91 |
| Median: 1166.50 | Median: 867.00 | Median: 842.00 |
There is insufficient evidence in the current literature from well-designed randomised controlled trials to determine the best method of treatment of simple elbow dislocations in adults. Historically, these were treated with prolonged casting followed up by physiotherapy[5]. It has also been suggested by several studies that the reduction should be followed-up by an up to 2-wk period of immobilisation[5,12]. Recent evidence however, supports the early active mobilisation within two weeks post-injury and as soon as pain allows[1,13,16,21]. The final functional outcomes obtained with early mobilisation are reported to be significantly better when compared to immobilisation[5,16,22,23]. The results of the present study are in agreement with the above findings. In particular, the final outcome of the patients managed with immobilisation not exceeding three weeks, was significantly better compared to the outcome of patients managed with prolonged immobilisation (more than three weeks). Of note is the observation that immobilisation for less that two weeks had the same outcome compared to immobilisation for 2-3 wk.
The characteristics of the patients sustaining simple elbow dislocations were also found to be comparable to the international literature. Taylor et al[4] reported that more than 90% of simple elbow dislocations occur in a posterior or posterior lateral direction, compared to 87.5% in the herein study. Anakwe et al[24] suggested that the epidemiology of simple elbow dislocation is different between men and women, particularly with respect to the mechanism of injury, and that it correlated with patient’s age. We have also found that the predominant gender in this group of injuries is young male patients, who are also more likely to have a sports related injury. Stoneback et al[2] separated sports activities by gender, reporting that males sustained elbow dislocations most often in association with football, wrestling, and basketball and females in gymnastics and skating activities. Even though an association between type of sports and gender was obvious with men being involved in sports such as rugby and football, the relatively small number of patients in our series did not allow us to draw any robust conclusions.
Previous research suggests that patients complete their recovery and return to normal activity by six months after such an injury[24]. We followed-up our patients for a longer period and advised them to contact the treating consultant in case of any concern. We therefore believe that the duration of follow-up in our study allowed us to assess accurately the final outcome in terms of range of motion of the affected elbow joint. The rates of residual pain and stiffness with early elbow motion have been reported to be 62% and 56% respectively, even though the functional outcome and patient reported satisfaction were favourable[23,24]. Residual pain restricting the function of the elbow did not seem to be of significant concern in our cohort, in contrast to significant stiffness limiting daily living activities that was reported as high as 25%[23,24]. Functional instability was less common involving four patients (6%) compared to 8% that was previously reported in the literature[24].
No re-dislocation or late instability was noted in the patients who were treated with early mobilisation. Similar studies in the literature agree with our findings and suggest that early mobilisation does not contribute to residual instability[5,12,13,20]. Other complications seen at the final follow-up included complaints of increasing pain during physical activities, which we believe could be related to the residual joint stiffness and stressing of the joint. None of our patients with a simple elbow dislocation was treated with an early surgical reconstruction. Noteworthy, the existing evidence does not suggest that surgical repair of elbow ligaments for simple elbow dislocation improves long-term function[4,20].
The current literature is limited in terms of the health economics of treating simple elbow dislocations. To the best of our knowledge there is only one study by Yang et al[3] reporting on the direct medical costs of these injuries. More specifically, the authors published a retrospective series of 428 simple and complex elbow dislocations treated in Taiwan, calculating the direct medical cost to be $504 per patient (included inpatient expenditure by admission and ambulatory care expenditure by visit)[3]. This is much lower compared to our estimated costs (average of £1088). We believe what accounts for this divergence are the different costs in a completely different national health care system, as well as the former timing at which these costs were obtained (between 2000 and 2005).
Even though one would expect that the direct medical costs of patients with prolonged immobilisation are higher because of higher incidence of post-traumatic stiffness and associated complications[5,16,22,23], this was not observed in our cohort. Possible explanations of this finding may include: two patients in Group I and two patients in Group II required a reduction in theatre compared to none in Group III, thus increasing the overall costs; patients in Group III were more likely not to attend their physiotherapy sessions, therefore reducing their overall costs. At the same time, the relatively small number of patients included in our study increases the risk of a type II error.
Limitations of this study include its retrospective nature and the small number of subjects, meaning that there is a risk of a type II statistical error. Yet, our findings are in line with the literature, thus providing sufficient evidence to support changes even with comparatively low numbers. Another limitation is the fact that elbow “stiffness” and loss of function was defined as an arc of elbow motion less than 100°[3,5,15-19]. Nevertheless, recent studies report that the functional elbow range of motion that is necessary for activities of daily living may actually be greater than this[25]. We also believe that this study could have been further enhanced by the collection of patient reported outcome measures, which probably reflects better on the loss of function from a patient’s perspective. On the positive side, this study was performed in a level I Trauma Centre, with no attempt for patient selection. Another improvement of the herein study was the inclusion of the associated costs for each group, a parameter that has not been previously adequately reported.
This study clearly underlines the fact that prolonged immobilization adversely affects the clinical outcome following a simple elbow dislocation. Despite the limitations and the retrospective nature of this study, the small number of patients included, and the 16.3% of lost to follow-up, we are confident that this cohort is representative of the actual clinical reality of a large United Kingdom hospital. In addition, this study depicts that the financial cost of treating elbow dislocations to the NHS may be substantial, regardless of the type of treatment. However, for the correct evaluation of each treatment modality a full prospective economic evaluation is desirable. This should include not only the direct medical and non-medical costs, but also the indirect costs associated with the duration of therapy, the final functional outcome, the loss of productivity and any disability payments of each patient[26].
The findings of our study stress the need for increased vigilance to the duration of immobilisation following simple elbow dislocations. Treating physicians (either orthopaedic surgeons or general practitioners) should be aware of the detrimental effects of prolonged immobilisation, and every effort should be taken to ensure that without associated fractures the elbow is not immobilised for more than three weeks. The direct medical cost from treating these injuries is substantial, and this should be known to both commissioners and providers of health care.
The authors would like to recognize and thank Mr Morell D, for his assistance in the collection of data.
Elbow dislocations represent the second most common dislocation in the adult population following shoulder dislocation, and the most common type of dislocation in the paediatric population. To date, there is no general consensus regarding the protocol of management of simple elbow dislocations with different protocols being suggested. In this study the authors determined the optimal length of elbow immobilisation following a simple elbow dislocation, along with their associated direct medical costs.
The duration of immobilisation following simple elbow dislocations is directly associated to the final functional outcome. Treating physicians (either orthopaedic surgeons or general practitioners) should be aware of the optimal immobilisation period required and of the associated direct medical costs for treating these injuries.
This study clearly underlines the fact that immobilization longer than three weeks adversely affects the clinical outcome following a simple elbow dislocation. In addition, the financial cost of treating elbow dislocations to the NHS may be substantial, regardless of the type of treatment.
An increased vigilance to the duration of immobilisation is required when treating these injuries, ensuring that without associated fractures, the elbow should not be immobilised for more than three weeks. Additional prospective studies evaluating the direct medical and non-medical costs, as well as the indirect associated costs could shed more light to the optimal treatment method.
“Simple” elbow dislocations include the dislocations that involve soft tissue disruption without any associated fractures, with the exception of avulsion fractures.
Very well done and useful study, which contributes to existing literature on this subject and clearly tells us that an unnecessary and prolonged immobilization is not only harmful to the patient but the hospital economics.
P- Reviewer: Erickson BJ, Garg B, Sano H, Vaishya R S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Kuhn MA, Ross G. Acute elbow dislocations. Orthop Clin North Am. 2008;39:155-161, v. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Stoneback JW, Owens BD, Sykes J, Athwal GS, Pointer L, Wolf JM. Incidence of elbow dislocations in the United States population. J Bone Joint Surg Am. 2012;94:240-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 148] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 3. | Yang NP, Chen HC, Phan DV, Yu IL, Lee YH, Chan CL, Chou P, Renn JH. Epidemiological survey of orthopedic joint dislocations based on nationwide insurance data in Taiwan, 2000-2005. BMC Musculoskelet Disord. 2011;12:253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Taylor F, Sims M, Theis JC, Herbison GP. Interventions for treating acute elbow dislocations in adults. Cochrane Database Syst Rev. 2012;4:CD007908. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Maripuri SN, Debnath UK, Rao P, Mohanty K. Simple elbow dislocation among adults: a comparative study of two different methods of treatment. Injury. 2007;38:1254-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 6. | Lee DH. Treatment options for complex elbow fracture dislocations. Injury. 2001;32 Suppl 4:SD41-SD69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Rhyou IH, Kim YS. New mechanism of the posterior elbow dislocation. Knee Surg Sports Traumatol Arthrosc. 2012;20:2535-2541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Josefsson PO, Gentz CF, Johnell O, Wendeberg B. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint. A prospective randomized study. J Bone Joint Surg Am. 1987;69:605-608. [PubMed] |
| 9. | Rafai M, Largab A, Cohen D, Trafeh M. [Pure posterior luxation of the elbow in adults: immobilization or early mobilization. A randomized prospective study of 50 cases]. Chir Main. 1999;18:272-278. [PubMed] |
| 10. | Royle SG. Posterior dislocation of the elbow. Clin Orthop Relat Res. 1991;201-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Riel KA, Bernett P. [Simple elbow dislocation. Comparison of long-term results after immobilization and functional treatment]. Unfallchirurg. 1993;96:529-533. [PubMed] |
| 12. | Protzman RR. Dislocation of the elbow joint. J Bone Joint Surg Am. 1978;60:539-541. [PubMed] |
| 13. | Mehlhoff TL, Noble PC, Bennett JB, Tullos HS. Simple dislocation of the elbow in the adult. Results after closed treatment. J Bone Joint Surg Am. 1988;70:244-249. [PubMed] |
| 14. | Schippinger G, Seibert FJ, Steinböck J, Kucharczyk M. Management of simple elbow dislocations. Does the period of immobilization affect the eventual results? Langenbecks Arch Surg. 1999;384:294-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Cohen MS, Hastings H. Acute elbow dislocation: evaluation and management. J Am Acad Orthop Surg. 1998;6:15-23. [PubMed] |
| 16. | Coonrad RW, Roush TF, Major NM, Basamania CJ. The drop sign, a radiographic warning sign of elbow instability. J Shoulder Elbow Surg. 2005;14:312-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Josefsson PO, Johnell O, Gentz CF. Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg Am. 1984;66:927-930. [PubMed] |
| 18. | Charalambous CP, Morrey BF. Posttraumatic elbow stiffness. J Bone Joint Surg Am. 2012;94:1428-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 19. | Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63:872-877. [PubMed] |
| 20. | de Haan J, Schep NW, Tuinebreijer WE, Patka P, den Hartog D. Simple elbow dislocations: a systematic review of the literature. Arch Orthop Trauma Surg. 2010;130:241-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Ross G, McDevitt ER, Chronister R, Ove PN. Treatment of simple elbow dislocation using an immediate motion protocol. Am J Sports Med. 1999;27:308-311. [PubMed] |
| 22. | de Haan J, Schep NW, Zengerink I, van Buijtenen J, Tuinebreijer WE, den Hartog D. Dislocation of the elbow: a retrospective multicentre study of 86 patients. Open Orthop J. 2010;4:76-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Kesmezacar H, Sarıkaya IA. The results of conservatively treated simple elbow dislocations. Acta Orthop Traumatol Turc. 2010;44:199-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Anakwe RE, Middleton SD, Jenkins PJ, McQueen MM, Court-Brown CM. Patient-reported outcomes after simple dislocation of the elbow. J Bone Joint Surg Am. 2011;93:1220-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 25. | Sardelli M, Tashjian RZ, MacWilliams BA. Functional elbow range of motion for contemporary tasks. J Bone Joint Surg Am. 2011;93:471-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 160] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 26. | Bozic KJ, Rosenberg AG, Huckman RS, Herndon JH. Economic evaluation in orthopaedics. J Bone Joint Surg Am. 2003;85-A:129-142. [PubMed] |