Published online Jul 18, 2015. doi: 10.5312/wjo.v6.i6.498
Peer-review started: January 31, 2015
First decision: March 6, 2015
Revised: March 13, 2015
Accepted: June 4, 2015
Article in press: June 8, 2015
Published online: July 18, 2015
Processing time: 164 Days and 11.2 Hours
Femoroacetabular impingement is uncommonly associated with a large rim fragment of bone along the superolateral acetabulum. We report an unusual case of femoroacetabular impingement (FAI) with chronic acetabular rim fracture. Radiographic, 3D computed tomography, 3D magnetic resonance imaging and arthroscopy correlation is presented with discussion of relative advantages and disadvantages of various modalities in the context of FAI.
Core tip: Rim fracture is an uncommon finding in the context of femoroacetabular impingement and its management can be aided by bony remodeling and labral-cartilage assessment on pre-operative 3D computed tomography and 3D magnetic resonance imaging.
- Citation: Chhabra A, Nordeck S, Wadhwa V, Madhavapeddi S, Robertson WJ. Femoroacetabular impingement with chronic acetabular rim fracture - 3D computed tomography, 3D magnetic resonance imaging and arthroscopic correlation. World J Orthop 2015; 6(6): 498-504
- URL: https://www.wjgnet.com/2218-5836/full/v6/i6/498.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i6.498
Femoroacetabular impingement is uncommonly associated with a large rim fragment of bone along the superolateral acetabulum. The fragment can put surgeons in a dilemma, whether to excise the fragment or to operatively re-attach it to the acetabulum. Computed tomography (CT) and magnetic resonance imaging (MRI) can be very helpful in pre-operative planning. We report radiographic, 3D CT, 3D MRI and arthroscopy correlation in such a case of chronic acetabular rim fracture and discuss the relative advantages and disadvantages of various imaging modalities.
A 46-year-old man presented to the sports clinic with recalcitrant bilateral hip pain, right worse than left. He was in a motorcycle accident 3 mo before when he landed on his left hip. He noted some pain in the right hip at that time. However, it significantly worsened after playing golf recently, a week before the current presentation. With swinging and rotating movements, he had worsening pain, rated as 9 to 10/10. He had a positive “C sign” and he localized his pain anteriorly in the groin. He also noted that he is limping because of pain and experiences a click and pain getting in and out of a car. He had other prior injuries, namely a motor vehicle accident 14 years ago, which led to right knee injury and meniscus repair; and another injury 7 mo ago when he was running and slipped in a small hole. There, he heard and felt a pop in his left knee and experienced swelling with difficulty in activities over the next several days, which gradually decreased over time. The past medical history was unremarkable, except for type II diabetes mellitus and hypertension. On examination, he walked with a coxalgic gait favoring the right side. The range of motion of the right hip vs left hip was as follows, flexion 95/100, abduction 40/50, internal rotation at 90° of flexion 5/5, external rotation at 90° of flexion 40/40. He had some tenderness anteriorly. No sacroiliac or abductor tenderness was present. He had a positive impingement sign and positive flexion abduction and external rotation (FABER) sign. His motor strength was - 5/5 hip flexion, abduction and adduction; 5/5 tibialis anterior, gastrocnemius and extensor halluces longus (EHL). Straight leg raise was negative. In the left hip, he was slightly tender over the trochanter and had positive impingement on that side as well. FABER was negative and his strength was 5/5 in tibialis anterior, gastrocnemius, EHL and throughout the hip. He had intact sensation and palpable pulses. The clinical diagnosis was femoroacetabular impingement.
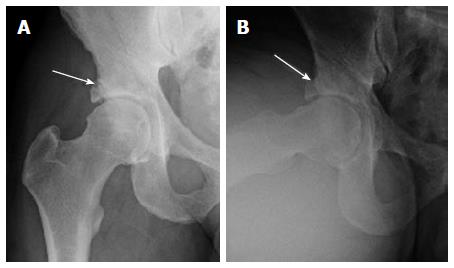
The radiographs of pelvis in anteroposterior standing, and dedicated views of both hips confirmed bilateral femoroacetabular impingement anatomy. The right hip showed a large bony osteophyte, possibly an os acetabulum, resulting a center edge angle of 46°. There was a suggestion of prior rim fracture with a lucent line between the fragment and the underlying bone (Figure 1). The alpha angle was 68° with significantly decreased head and neck offset. Some sclerosis was observed in the acetabulum; however, no substantial joint space narrowing was present. In the left hip, there was some calcification in the area of the labrum as well.
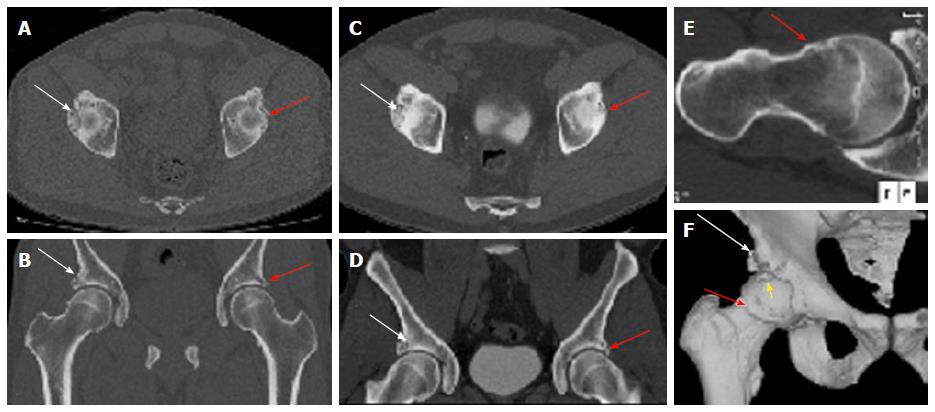
3D CT of the pelvis was obtained on a 64 slice scanner (Aquillion Intuition, Toshiba, Tustin, CA, United States) using 0.625 mm beam collimation for pre-surgical planning purposes. It confirmed bilateral mixed type femoroacetabular impingement (FAI) anatomy and right acetabular rim fracture (Figure 2). The patient also had a CT abdomen and pelvis with contrast 2 years before for other reasons, which showed similar findings in bilateral hips. 3D surface rendered bone reconstructions and thick slab maximum intensity projection obtained on an independent work (Aquarius, Tera Recon, Foster City, CA, United States) nicely showed the volumetric display of the anatomic right hip derangement, rim fracture and a potentially loose anterior superior fragment (Figure 2). The alpha angle was 65°, coronal center edge angle and sagittal center edge angles were 44° and 61°, respectively. The femoral neck shaft angle was 126° and the acetabular version measurements, adjusting for pelvic tilt near zero were 9.4°, 21.3° and 18.1° at 1:00, 2:00 and 3:00 clock positions, respectively. The femoral anteversion was 12.9°.
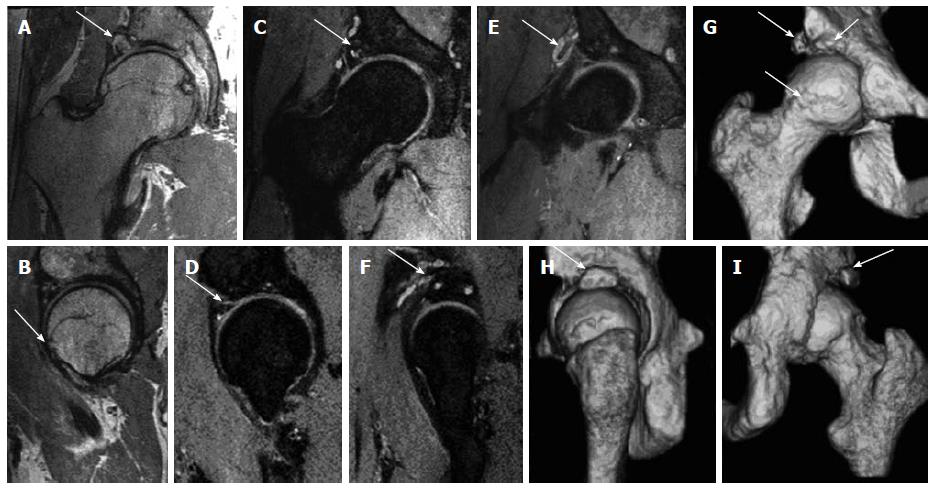
MRI of right hip was obtained for labral and cartilage evaluation. The MRI protocol included both high resolution 2D (3 mm) and isotropic (0.7 mm) 3D proton density weighted and fat suppressed proton density imaging sequences on a 3 Tesla scanner (Achieva, Philips, Best, Netherlands) using a torso coil. The imaging demonstrated again showed the CAM and PINCER anatomy, chronic rim fracture with pseudoarthrosis and cystic changes. There were multifocal labral tears extending from the anterior-superior labrum to the posterior-superior labrum and associated large multiloculated para labral cyst measuring 2.8 cm (AP) × 1.4 cm (Tr) × 2.9 cm (CC), which had undercut and wrapped around the indirect head of the rectus femoris tendon. The femoral cartilage was normal. The acetabular cartilage showed small area of high grade fissuring involving the anterior-superior and superior-lateral acetabulum with underlying subchondral cystic changes (Figure 3). There was low-grade partial tear of the proximal iliofemoral ligament. 3D surface rendered bone reconstructions were obtained from the isotropic 3D imaging on the same work station using semi-automated contour drawing tool that also demonstrated the bony anatomy of FAI and rim fracture. The patient received physical rehabilitation and an ultrasound guided local anesthetic and steroid injection of right hip over the next 4 mo without much relief.
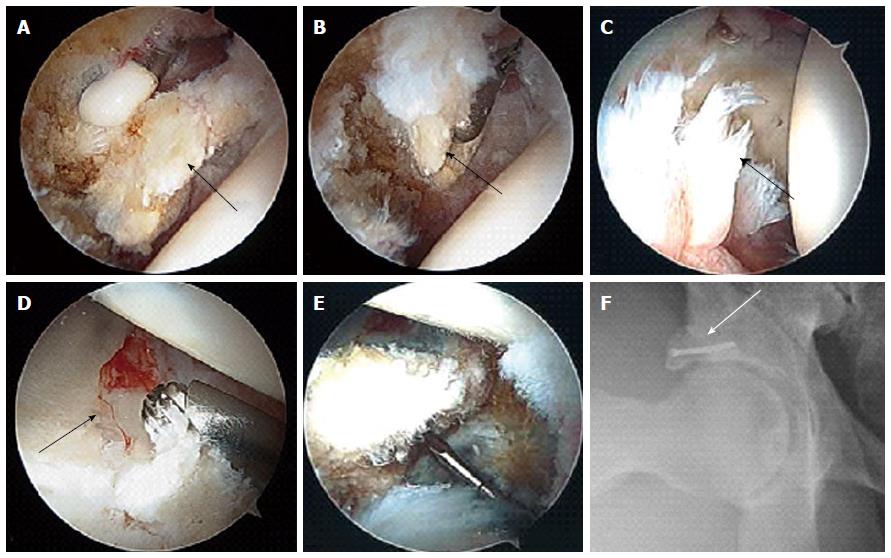
Further 4 mo later, the patient underwent right hip arthroscopy with labral debridement as well as open reduction and internal fixation of acetabular rim fracture with a screw, rim trim and femoroplasty cam decompression. The acetabular labrum was found to be attached to the loose mobile fragment, which disrupted the continuity of the labrum at the 1 to 2 o’clock position as defined with respect to the acetabular notch (Figure 4). This fragment was removed. The remaining anterior labrum was shredded from the 3 o’clock to 6 o’clock position. There was an additional lateral acetubular rim fracture that extended from the 1 o’clock position anteriorly to the 11 o’clock position posteriorly. The rim fragment was mobile, but contained both intact articular cartilage and a labral rim. Femoral head cartilage was intact. The acetabular cartilage was found to be intact anteriorly and posteriorly; however, at the site of the acetabular rim fracture, there was a crack through the acetabular cartilage. The loose body at the calcified acetabulum was somewhat tethered to the soft tissues of the capsule. This was released with radiofrequency and then removed as 1 piece, approximately 1 cm × 1 cm in size. Using an arthroscopic shaver and radiofrequency device, the labrum was debrided back to a stable rim over this area from 3 to 6 o’clock. The labrum also stabilized at its truncation point at 1 o’clock. Acetabular rim trim was then performed using a 4.5 mm shaver along the 1 to 3 o’clock positions. The removal of the acetabular rim fragment would have resulted in a significant loss in lateral acetabular cartilage and labrum. Therefore, it was fixed with a 2.4 mm headless cannulated screw. The screw was inserted arthroscopically and resulted in excellent compression across the fracture site. Finally, femoroplasty and Cam decompression was performed by debriding the femoral head and neck junction over the anterior-superior and anterolateral aspect of the femoral head-neck junction. The patient did well on follow-up obtained over next 6 mo.
Femoroacetabular impingement is a patho-mechanical process due to presence of either a mis-shapen femoral head (CAM lesion) or mal-rotated/deep acetabulum (PINCER lesion) resulting in early and accelerated fibrocartilage and/or hyaline cartilage degeneration[1-5]. For the correction of the altered anatomy, the surgeon pre-operatively needs to know the extent of bony as well as soft tissue lesions or any odd lesions, such as a rim fracture in this case. Our patient showed bilateral FAI anatomy on CT abdomen and pelvis obtained 2 years ago for other reasons but he did not have hip symptoms at that time. It is well reported in the literature that many asymptomatic subjects might show radiographic evidence of altered anatomy suggesting FAI on various imaging modalities and therefore, clinical correlation of symptomatology, positive impingement test, “C sign” and focused hip examination is essential for the FAI diagnosis[6,7].
The association of FAI anatomy with labral tears and hyaline cartilage degeneration is well known. Most common areas of labral tears are in anterosuperior or superolateral quadrants[8]. Higher offset alpha angles are associated with larger labral tears, more cartilage delamination, male sex and decreased range of motion as in this case, where alpha angle was 65°-68°[9]. 3D CT is the current reference standard for demonstration of bony alterations of FAI and is widely used for pre-operative planning[10-12]. It provides exquisite surface rendered reconstructions and affords easy and accurate calculation of various angular and linear measurements intended for prospective surgical bony re-alignment[13,14]. It was difficult to tell on radiographs due to their planar nature, whether the superolateral acetabular rim represented a large os acetabulum with labral ossification or a rim fracture. 3D CT reconstruction confirmed the presence of a rim fracture with pseudoarthrosis and also detected an anterior potentially loose fragment. It has been previously reported that os acetabulum related lucency is parallel to the joint surface unlike the rim fracture, which is more perpendicular in orientation[15]. However, the above differentiation might not be clear cut, and further MR imaging demonstration or surgical inspection of hyaline cartilage extension to the broken fragment might be needed for accurate identification. It has been shown that 3D CT can also moderately predict the internal soft tissue derangement findings of FAI based on altered bony anatomy[16], however, MR imaging is the current reference standard for labrum and hyaline cartilage evaluation for detection of locations of tears, their characterization and determining the extent of secondary osteoarthrosis[4,17].
A high-resolution, non-arthrographic technique at 3 Tesla (T) imaging potentially provides more accurate and reproducible preoperative information regarding the presence and anatomic location of labral and cartilage abnormalities similar to arthrographic technique at 1.5T[18,19]. Soft tissue internal derangement findings nicely correlated with surgical findings. Except for cartilage crack at fracture site, cartilage fissuring was not reported on arthroscopy despite small area being present on MRI with subchondral cystic change. This might be explained by overt sensitivity of MRI. In addition, 3D isotropic spin echo type imaging (0.6-0.75 mm isotropic resolution, TR: 1400-1700 ms, TE: 35-45 ms) on 3T scanner not only allows similar resolution multiplanar reconstructions, but also bone segmentation and surface rendering using the available CT software. MR imaging thereby offers benefits of soft tissue evaluation, bone remodeling, radiation free imaging, and finally convenience for the patient with single stop shop for FAI assessment[20,21]. However, this approach is not free of limitations. These include required availability of 3T scanner, technique optimization, long imaging time of 3D sequence (about 7 min) with potential for patient motion artifacts, and not very crisp bony reconstructions due to the lack of dedicated MR imaging based software at current times. The reconstruction also takes about 20 min for the technologist/reader. Additionally, one is limited in accomplishing pelvic tilt correction similar to whole pelvis CT imaging, which is required for better reproducibility and accuracy of measurements[22,23]. Finally, CT imaging at knee and hip can be used to evaluate the femoral version. Femoral version can either protect (anteversion making CAM deformity less likely to impinge) or make it more susceptible (relative retroversion making it more likely to impinge). Similar technique can be done with MRI but this approach requires more time for acquisition and potential coil movement with some vendors.
Stress injuries of acetabulum, labral ossification, femoral neck stress fractures and rim fracture can occur in the setting of FAI due to altered anatomy[15,24,25]. Rim fracture puts the surgeon in a dilemma whether to remove the bone fragment to mitigate the impingement anatomy, or to re-attach it so as not to the leave the femoral head substantially uncovered and consequently, an unstable hip[26]. Measurement of lateral center edge angle or visual impression on surface rendered 3D CT or 3D MR images can give an indication to the surgeon pre-operatively, as to the amount of resultant undercoverage, if the fractured lateral rim were to be removed. Surgical excision and re-fixation using a cannulated screw by drilling across the fibro-cartilaginous junction helps to promote healing of these fragments or any associated labral tears[26,27], as was also accomplished in our case. Absence of large areas of cartilage abnormality or significant arthritis on MR imaging is good predictor of successful outcome in FAI cases[28,29]. The patient did well on 6 wk and 4 mo follow-up visits. We do not have a long term follow-up on our patient but he did well in the short term.
To conclude, rim fracture is an uncommon finding in the context of FAI and its management can be aided by bony remodeling and labral-cartilage assessment on pre-operative 3D CT and 3D MR imaging.
A 46-year-old man presented with bilateral hip pain, right worse than left.
Femoroacetabular impingement (FAI).
Tumor, infection or inflammatory condition, fracture, and avascular necrosis.
3D computed tomography (CT) and 3D magnetic resonance imaging (MRI) confirmed FAI with chronic acetabular rim fracture.
Right hip arthroscopy with labral debridement as well as open reduction and internal fixation of acetabular rim fracture with a screw, rim trim and femoroplasty cam decompression.
It is well reported in the literature that many asymptomatic subjects might show radiographic evidence of altered anatomy suggesting FAI on various imaging modalities and therefore, clinical correlation of symptomatology, positive impingement test, “C sign” and focused hip examination is essential for the FAI diagnosis.
Femoroacetabular impingement is a patho-mechanical process due to presence of either a mis-shapen femoral head (CAM lesion) or mal-rotated/deep acetabulum (PINCER lesion) resulting in early and accelerated fibrocartilage and/or hyaline cartilage degeneration.
Rim fracture is an uncommon finding in the context of FAI and its management can be aided by bony remodeling and labral-cartilage assessment on pre-operative 3D CT and 3D MR imaging.
The authors present an unusual case of FAI with chronic acetabular rim fracture. Radiographic, 3D CT, 3D MRI and arthroscopy correlation is presented with discussion of their relative advantages and disadvantages in the context of FAI.
P- Reviewer: Cartmell S, Fenichel I, Malik H S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
| 1. | Hofmann S, Tschauner Ch, Graf R. Mechanical causes of osteoarthritis in young adults. Hip Int. 2003;13:3-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;112-120. [PubMed] |
| 3. | Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540-1552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 676] [Cited by in RCA: 681] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 4. | Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 360] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 5. | Cobb J, Logishetty K, Davda K, Iranpour F. Cams and pincer impingement are distinct, not mixed: the acetabular pathomorphology of femoroacetabular impingement. Clin Orthop Relat Res. 2010;468:2143-2151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 73] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Jung KA, Restrepo C, Hellman M, AbdelSalam H, Morrison W, Parvizi J. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg Br. 2011;93:1303-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 115] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 7. | Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436-2444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 371] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 8. | Beall DP, Sweet CF, Martin HD, Lastine CL, Grayson DE, Ly JQ, Fish JR. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005;34:691-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 111] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 9. | Johnston TL, Schenker ML, Briggs KK, Philippon MJ. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24:669-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 209] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 10. | Beaulé PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ. Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res. 2005;23:1286-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Tannast M, Kubiak-Langer M, Langlotz F, Puls M, Murphy SB, Siebenrock KA. Noninvasive three-dimensional assessment of femoroacetabular impingement. J Orthop Res. 2007;25:122-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 193] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 12. | Kang RW, Yanke AB, Espinoza Orias AA, Inoue N, Nho SJ. Emerging ideas: Novel 3-D quantification and classification of cam lesions in patients with femoroacetabular impingement. Clin Orthop Relat Res. 2013;471:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Milone MT, Bedi A, Poultsides L, Magennis E, Byrd JW, Larson CM, Kelly BT. Novel CT-based three-dimensional software improves the characterization of cam morphology. Clin Orthop Relat Res. 2013;471:2484-2491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 14. | Murphy RJ, Subhawong TK, Chhabra A, Carrino JA, Armand M, Hungerford M. A quantitative method to assess focal acetabular overcoverage resulting from pincer deformity using CT data. Clin Orthop Relat Res. 2011;469:2846-2854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Martinez AE, Li SM, Ganz R, Beck M. Os acetabuli in femoro-acetabular impingement: stress fracture or unfused secondary ossification centre of the acetabular rim? Hip Int. 2006;16:281-286. [PubMed] |
| 16. | Heyworth BE, Dolan MM, Nguyen JT, Chen NC, Kelly BT. Preoperative three-dimensional CT predicts intraoperative findings in hip arthroscopy. Clin Orthop Relat Res. 2012;470:1950-1957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 17. | James SL, Ali K, Malara F, Young D, O’Donnell J, Connell DA. MRI findings of femoroacetabular impingement. AJR Am J Roentgenol. 2006;187:1412-1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 88] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 18. | Robinson P. Conventional 3-T MRI and 1.5-T MR arthrography of femoroacetabular impingement. AJR Am J Roentgenol. 2012;199:509-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Park SY, Park JS, Jin W, Rhyu KH, Ryu KN. Diagnosis of acetabular labral tears: comparison of three-dimensional intermediate-weighted fast spin-echo MR arthrography with two-dimensional MR arthrography at 3.0 T. Acta Radiol. 2013;54:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Kang X, Zhang H, Garbuz D, Wilson DR, Hodgson AJ. Preliminary evaluation of an MRI-based technique for displaying and quantifying bony deformities in cam-type femoroacetabular impingement. Int J Comput Assist Radiol Surg. 2013;8:967-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Kavanagh EC, Read P, Carty F, Zoga AC, Parvizi J, Morrison WB. Three-dimensional magnetic resonance imaging analysis of hip morphology in the assessment of femoral acetabular impingement. Clin Radiol. 2011;66:742-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Dandachli W, Ul Islam S, Tippett R, Hall-Craggs MA, Witt JD. Analysis of acetabular version in the native hip: comparison between 2D axial CT and 3D CT measurements. Skeletal Radiol. 2011;40:877-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Lohan DG, Seeger LL, Motamedi K, Hame S, Sayre J. Cam-type femoral-acetabular impingement: is the alpha angle the best MR arthrography has to offer? Skeletal Radiol. 2009;38:855-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 24. | Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423-429. [PubMed] |
| 25. | Epstein NJ, Safran MR. Stress fracture of the acetabular rim: arthroscopic reduction and internal fixation. A case report. J Bone Joint Surg Am. 2009;91:1480-1486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Larson CM, Stone RM. The rarely encountered rim fracture that contributes to both femoroacetabular impingement and hip stability: a report of 2 cases of arthroscopic partial excision and internal fixation. Arthroscopy. 2011;27:1018-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 215] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 28. | Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 311] [Article Influence: 23.9] [Reference Citation Analysis (1)] |
| 29. | Meftah M, Rodriguez JA, Panagopoulos G, Alexiades MM. Long-term results of arthroscopic labral debridement: predictors of outcomes. Orthopedics. 2011;34:e588-e592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |