Published online Apr 18, 2015. doi: 10.5312/wjo.v6.i3.369
Peer-review started: November 10, 2014
First decision: December 26, 2014
Revised: January 28, 2015
Accepted: February 10, 2015
Article in press: February 12, 2015
Published online: April 18, 2015
Processing time: 151 Days and 10 Hours
Synovial lipomatosis is a benign proliferative disease of the subsynovial adipose which can lead to a variety of presentations. Cases of synovial lipomatosis in children or adolescents are rare. This case report describes an adolescent patient with a rare bilateral presentation of synovial lipomatosis. She had been treated for years prior to her presentation for juvenile idiopathic arthritis. She presented with chronic bilateral knee pain, swelling, and mechanical symptoms. Bilateral MR imaging demonstrated effusions, hypertrophy of the synovium, and polyp-like projections of tissue with the same signal intensity as fat which is pathognomonic for synovial lipomatosis. Arthroscopic synovectomy and extensive debridement of polyp like fat projections of the right knee was performed. Histopathology was consistent with the synovial lipomatosis diagnosis. Postoperatively, the patient was satisfied with her outcome with improved pain relief and function in her right knee.
Core tip: This case demonstrates a unique presentation of bilateral knee synovial lipomatosis occurring in an adolescent. Arthroscopic treatment of this disease can yield a successful outcome. This case presentation will increase the awareness of this condition and decrease the tendency toward delayed diagnoses in the adolescent patient.
- Citation: Miladore N, Childs MA, Sabesan VJ. Synovial lipomatosis: A rare cause of knee pain in an adolescent female. World J Orthop 2015; 6(3): 369-373
- URL: https://www.wjgnet.com/2218-5836/full/v6/i3/369.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i3.369
Synovial lipomatosis, also known as lipoma arborescens or villous lipomatous proliferation of the synovial membrane, is a benign proliferation of subsynovial adipose. Although this process is more likely reactive than neoplastic in origin, it is rare with unknown etiology. There is limited literature on this topic to guide both diagnosis and optimal treatment of this disease[1-11].
Synovial lipomatosis appears to occur at any age, with reports of a patient as young as one year old with protein energy malnutrition to patients well into their eighth decade of life. The most common reported cases are in middle aged males. Patients typically present with pain and swelling of the affected joint. Although it appears to have a predilection for the knee, synovial lipomatosis has also been reported in the wrist and ankle, indicating that it could be a rarer cause of pain in smaller joints[1]. Often times, as seen in our patient, it is missed or undiagnosed for many years.
The recommended treatment is complete synovectomy either arthroscopically or via formal open debridement. The optimal method is debatable but both have good reported results despite limited follow up outcomes data[2]. Although the location of presenting symptoms can be variable, radiologic evaluation and histomorphology appear to be relatively consistent. This case report provides insight into the presentation, keys in diagnosis, and treatment of this rare entity.
Our patient is an 18 years old female [body mass index (BMI): 42 kg/m2], who presented to our clinic with a long standing history of bilateral knee pain, right worse than left. Past medical history was significant for juvenile idiopathic arthritis (JIA) which had been diagnosed clinically nine years prior to presentation and was treated by a Pediatric Rheumatologist. She was placed on a high dose non-steroidal anti-inflammatory drugs and had multiple steroid injections, but was not treated with disease modifying antirheumatic drugs. She initially had improved pain and symptom control with these modalities; however, she eventually became refractory to this treatment and her symptoms worsened.
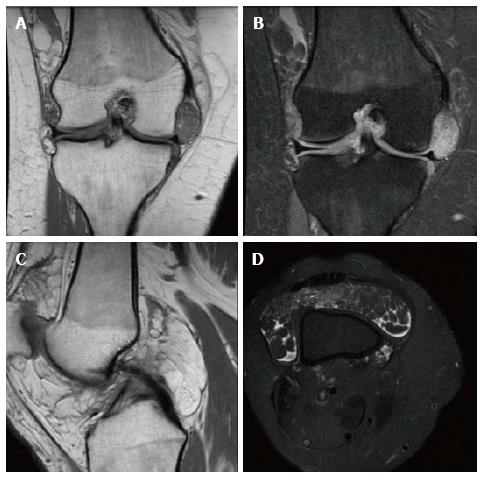
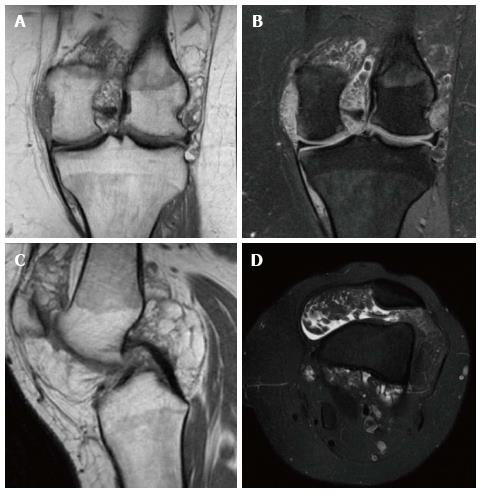
On presentation to our office, the patient’s main complaints were chronic swelling with recent onset of mechanical symptoms, specifically popping, catching, and locking while performing daily activities. She denied any trauma to the area. Examination of her knees revealed bilateral knee effusions with no instability with varus and valgus stress testing. In addition, the patient had a negative posterior and anterior drawer and Lachman’s maneuver. She had normal patellar tracking bilaterally and full active knee range of motion without crepitus or clicking. She had no joint line tenderness and a negative McMurrays and Apley grind test. X-rays and a magnetic resonance imaging (MRI) were obtained. Bilateral knee X-rays revealed no degenerative joint changes, fractures, avascular necrosis or osteochondral lesions. However, the X-rays did demonstrate diffuse soft tissue swelling. Bilateral knee MRIs demonstrated effusion in the suprapatellar bursa and hypertrophic synovium in the right knee worse than left with leaf-like projections of tissue which has the same signal intensity as fat. MRIs were negative for bony, meniscal, or ligament pathology bilaterally. MRI findings were consistent with synovial lipomatosis. Typical MRI findings of this entity include the villous like projections into the joint that are the same signal intensity as fat on both T1 and T2 weighted images (Figures 1 and 2).
Since the patient had clear MRI findings consistent with synovial lipomatosis with continued mechanical symptoms and pain after extensive nonoperative management, a detailed discussion was done regarding surgical treatment options including arthroscopic synovectomy of her right knee.
Patient elected to proceed with arthroscopic synovectomy, extensive debridement and biopsy for suggested synovial lipomatosis. Intraoperative findings demonstrated a significant amount of small lipoma nodules throughout the knee joint. These nodules were identified in the patellofemoral space, in the medial and lateral gutter, and in the medial and anterior joint. There did not appear to be any anterior cruciate ligament, posterior cruciate ligament, medial or lateral meniscal pathology. The articular surface was normal in appearance and no signs chondromalacia evident. The hypertrophic lipomatous nodules were methodically debrided and over 60 cc captured with some sent for pathology examination. Gross description revealed multiple lobulated tan-yellow soft tissue fragments admixed with fibrous tissue. Microscopic description demonstrated benign synovial tissue and fragments of adipose present beneath the synovial surface (Figure 3).
The patient was subsequently discharged home post-operatively. At her two week follow up, her pain was controlled without narcotic medications and swelling was improved. She denied any mechanical symptoms and had regained much of her range of motion. At six weeks follow up she continued to do well and began to discuss options for intervention on the contralateral side. At the patient’s eight month post-operative visit, she had full range of motion of her operative knee, denied return of mechanical symptoms, and continued to be pain free. The patient’s effusion was resolved and her knee was stable on examination.
Synovial lipomatosis is a rare disease which typically presents with symptoms of swelling and joint pain[3]. Synovial lipomatosis can be differentiated from other diagnoses by particular characteristics. When compared to pigmented villonodular synovitis (PVNS), synovial lipomatosis can be differentiated by lack of hemorrhage and hemosiderin on histology[4]. Hoffa disease is limited to the infrapatellar fat pad and is typically post traumatic[12]. Thorough knowledge of the differential is imperative in attaining the correct diagnosis.
In the setting of joint effusion on exam and synovitis on MRI the differential diagnosis includes PVNS, focal adipose tissue accumulation in osteoarthritis, rheumatoid arthritis, and post-traumatic hypertrophy of the infrapatellar fat pad (Hoffa disease)[4]. A clinician should have a heightened awareness and consideration for synovial lipomatosis when the patient has joint pain and swelling, mechanical symptoms, refractory to nonoperative management, no evidence of ligamentous or meniscal pathology, and the appropriate MRI findings. Commonly the laboratory testing is negative in this setting and optimal evaluation to diagnose this rare disease is MR imaging. The MRI findings are diagnostic and help differentiate from a number of other pathologies. Common MRI findings for synovial lipomatosis are villous or “leaf-like” projections into the knee joint diffusely. The signals for the projections will match that of fat on both T1 and T2 weighted images[5]. This is different from PVNS because it lacks hemosiderin deposits which are low signal areas best seen on the fast field echo sequence. Rheumatoid arthritis typically presents with MRI findings of joint space narrowing, synovitis, bony erosion and positive laboratory studies for anti-cyclic citrullinated protein and rheumatoid factor. Hoffa’s disease is post traumatic in origin and will be isolated to hypertrophy of the infrapatellar fat pad.
Our patient had been initially diagnosed with JIA which commonly is a diagnosis of exclusion. Symptoms should last more than six weeks and the patient should be less than sixteen years old[13]. Rheumatoid factor is only positive in about 15% of cases. She was treated with high dose non-steroidal anti-inflammatory medication and injections; however she had continued symptoms of pain and locking, specifically in her knees. In these cases, a clinician may consider utility of MRI imaging especially given the mechanical symptoms to further evaluate intra-articular pathology. MRI findings helped distinguish this patient’s JIA symptoms with more specific intra-articular pathology. Although there is limited literature providing treatment recommendations for synovial lipomatosis, our patient’s clinical improvement and patient satisfaction support surgical treatment recommendations. Success with arthroscopic synovectomy in this case is consistent with previous reported results for both open and arthroscopic treatment. Although long term outcomes and reoccurrence rates have yet to be reported, review of the literature suggests that it is low.
Synovial lipomatosis is a rare diagnosis, but should be considered in the setting of refractory chronic joint effusions and knee pain. The etiology is currently unknown, although it has been hypothesized that trauma, inflammation, rheumatism, developmental, neoplastic, or obesity can be implicated. It has been suggested that perhaps increased BMI may be a risk factor in this disease as was seen in our patient, however there is no evidence supporting this correlation[1,6]. This is often diagnosed in patients with inflammatory diseases. This may be due to higher index of suspicion, a biased diagnostic workup, or it may be a true relationship. Either way, more research is needed to better understand the cause of this disorder, the optimal diagnostic evaluation and treatment.
This case increases awareness of this rare disease. This entity may be missed if the clinician does not have a high index of suspicion, especially in the setting of a young patient with chronic refractory knee pain and an otherwise negative work up. If MRI findings are consistent with diagnosis of synovial lipomatosis, we recommend obtaining a biopsy to verify the diagnosis and to consider arthroscopic debridement. Patients can expect improved pain relief and decreased mechanical symptoms, with good short term results. Our case presentation is limited to one individual; however, it demonstrates the need for further studies as this is an identifiable entity with successful treatment options.
An 18 years old female, with a history of juvenile rheumatoid arthritis, presents with bilateral knee pain.
The patient’s main complaints were chronic swelling with recent onset of mechanical symptoms, specifically popping, catching, and locking while performing daily activities.
Synovial chondromatosis, pigmented villonodular synovitis, synovial hemangiomatosis.
Bilateral knee magnetic resonance imagings demonstrated effusion in the suprapatellar bursa and hypertrophic synovium in the right knee worse than left with leaf-like projections of tissue which has the same signal intensity as fat.
Microscopic description demonstrated benign synovial tissue and fragments of adipose present beneath the synovial surface.
The patient was treated with arthroscopic synovectomy.
Synovial lipomatosis is a rare disease of unknown etiology. Cases in children and adolescents have been infrequently reported.
This case increases awareness of this rare disease. This entity may be missed if the clinician does not have a high index of suspicion, especially in the setting of a young patient with chronic refractory knee pain and an otherwise negative work up.
The authors have performed a good study, the manuscript is interesting.
P- Reviewer: Affatato S, Makishima M, Malik H, Willis-Owen CA S- Editor: Tian YL L- Editor: A E- Editor: Lu YJ
| 1. | Rao S, Rajkumar A, Elizabeth MJ, Ganesan V, Kuruvilla S. Pathology of synovial lipomatosis and its clinical significance. J Lab Physicians. 2011;3:84-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Franco M, Puch JM, Carayon MJ, Bortolotti D, Albano L, Lallemand A. Lipoma arborescens of the knee: report of a case managed by arthroscopic synovectomy. Joint Bone Spine. 2004;71:73-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Hallel T, Lew S, Bansal M. Villous lipomatous proliferation of the synovial membrane (lipoma arborescens). J Bone Joint Surg Am. 1988;70:264-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Horvai AE, Link T. Bone and Soft Tissue Pathology: High-Yield Pathology. Philadelphia: Elsevier Saunders 2012; 186-187. [DOI] [Full Text] |
| 5. | Bejia I, Younes M, Moussa A, Said M, Touzi M, Bergaoui N. Lipoma arborescens affecting multiple joints. Skeletal Radiol. 2005;34:536-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Siva C, Brasington R, Totty W, Sotelo A, Atkinson J. Synovial lipomatosis (lipoma arborescens) affecting multiple joints in a patient with congenital short bowel syndrome. J Rheumatol. 2002;29:1088-1092. [PubMed] |
| 7. | Yildiz C, Deveci MS, Ozcan A, Saraçoğlu HI, Erler K, Basbozkurt M. Lipoma arborescens (diffuse articular lipomatosis). J South Orthop Assoc. 2003;12:163-166. [PubMed] |
| 8. | Bansal M, Changulani M, Shukla R, Sampath J. Synovial lipomatosis of the knee in an adolescent girl. Orthopedics. 2008;31:185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Kakkar N, Vasishta RK, Anand H. Pathological case of the month. Synovial lipomatosis. Arch Pediatr Adolesc Med. 1999;153:203-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Davies AP, Blewitt N. Lipoma arborescens of the knee. Knee. 2005;12:394-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Saddik D, McNally EG, Richardson M. MRI of Hoffa’s fat pad. Skeletal Radiol. 2004;33:433-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 154] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 12. | Al-Shraim MM. Intra-articular lipoma arborescens of the knee joint. Ann Saudi Med. 2011;31:194-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Naz S, Mushtaq A, Rehman S, Bari A, Maqsud A, Khan MZ, Ahmad TM. Juvenile rheumatoid arthritis. J Coll Physicians Surg Pak. 2013;23:409-412. [PubMed] |