Published online Apr 18, 2015. doi: 10.5312/wjo.v6.i3.363
Peer-review started: November 17, 2014
First decision: December 26, 2014
Revised: January 31, 2015
Accepted: February 10, 2015
Article in press: February 12, 2015
Published online: April 18, 2015
Processing time: 151 Days and 10.3 Hours
The management of a combination of fracture and multiligament knee injury (MKI) in traumatic knee injury remains controversial, and there are evolving treatment recommendations. Currently, there are no studies focusing on older adult patients with MKI’s in combination with tibia fractures. As a result, there is no well-established treatment algorithm for older adult patients with these complex injuries. We report two cases of MKI’s with concomitant fractures in patients fifty years of age or older. Both patients were treated surgically for their associated tibial plateau fractures, but were managed with conservative treatment of the multiligamentous knee injuries. We also provide a review of the literature and guidelines for older adult patients with these types of complex traumatic injuries. Early to mid term acceptable outcomes were achieved for both patients through surgical fixation of the tibial plateau fracture and conservative treatment of the ligament injuries. We propose a comprehensive treatment algorithm for management of these complex injuries.
Core tip: Extensive review of the literature illustrates the limited evidence on these types of complex knee injuries. Patients with multiligament knee injury (MKI) and tibial plateau fractures require a complex treatment algorithm optimized to patient specific injuries and expectations. We propose an algorithm for treating MKI with concomitant fracture in middle aged-patients.
- Citation: Sabesan VJ, Danielsky PJ, Childs A, Valikodath T. Multiligament knee injuries with associated tibial plateau fractures: A report of two cases. World J Orthop 2015; 6(3): 363-368
- URL: https://www.wjgnet.com/2218-5836/full/v6/i3/363.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i3.363
Multiligament knee injuries (MKIs) with associated fractures are rare but serious injuries that pose diagnostic and therapeutic challenges. These complex knee injuries usually occur during participation in contact sports or a high energy motor vehicle accident. Several studies have shown a significant delay in the diagnosis of ligamentous injuries in patients presenting with ipsilateral femoral or tibial fractures[1-4]. In addition, there are varying opinions on treatment of these injuries[1,5,6]. Fracture stabilization as well as ligamentous instability must be addressed in surgical planning[7].
The potential morbidity of these knee injuries are significant, with instability and pain being reported many years after the initial injury[5,8-10]. Functional outcomes and pain control remain the standard for determining successful treatment of knee injuries. While consensus in the literature suggests the most effective treatment of tibial plateau fractures is open reduction and internal fixation (ORIF)[11,12], no similar consensus has been reached in regards to restoring ligament function with MKIs[5]. Conservative treatment with immobilization has demonstrated moderate success[13], however, current Level III studies demonstrate improved functional outcomes with surgical repair or ligament reconstruction over nonoperative treatment[8,14]. Because these injuries account for less than 1% of all orthopaedic injuries, there is a lack of high level evidence, especially in the middle-aged patient, on which to base treatment decisions. Our study reviews the treatment and outcomes for two middle aged (≥ fifty years old) patients with both tibial plateau fractures and multi-ligamentous knee injuries. We also provide a review of the literature and define guidelines for treatment for a middle-aged patient population who sustain these complex traumatic injuries.
A 52-year-old male presented to the Emergency Department (ED) status post-MVA with multiple injuries including a left proximal humerus fracture and a severe right knee injury. Radiographs and computed tomography demonstrated a comminuted Schatzker IV tibial plateau fracture dislocation and a femoral condyle fracture (Figure 1). Neurovascular examination was unremarkable and Ankle-Brachial index was 1.0 on the injured leg. The patient initially underwent a closed reduction of knee dislocation in the ED which corrected his alignment in the sagittal plane but there was continued subluxation and displacement in the coronal plane. Given his fracture displacement and instability was subsequently taken to the OR for closed reduction and placement of an external fixator. Examination under anesthesia revealed excessive anteroposterior laxity and medial laxity. Fluoroscopic imaging confirmed increased anterior and posterior laxity with markedly comminuted intra-articular fracture through the lateral tibial plateau and tibial spines and severe depression of the lateral tibial plateau. A post-fixation MRI demonstrated comminuted tibia spine fracture with partial tearing of anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) tibial sided insertions with a complete tear of inferior portion of superficial medial collateral ligament (MCL).
At 2.5 wk post-injury, the external fixator was removed and an open reduction internal fixation of the tibial plateau fractures was performed with medial and lateral peri-articular locking plates as well as a lateral meniscal repair. Intraoperative examination of the knee showed comminution of lateral tibial plateau articular surface and tibial spines with a competent MCL that did not require reconstruction. The lateral femoral condyle fracture was treated nonoperatively, based on intraoperative evaluation. The patient was discharged to a rehabilitation facility with a full extension splint. Potential staged ligament reconstruction was discussed with the patient.
At 8 wk post-injury, the patient’s pain is well controlled. Radiographs demonstrated stable hardware fixation of the comminuted tibial plateau fracture with maintenance of knee joint alignment and fracture reduction (Figure 2). Given the complexity of his injury, the patient remained non-weight bearing for 12 wk but continued with his knee range of motion and brace wear. X-rays demonstrate continued tibial plateau fracture healing with maintenance of plate and screw hardware fixation and increased valgus deformity. The patient progressed to full weight bearing without assisted device by 5 mo post injury, at which time he had been discharged from rehab and remained pain free without narcotic medications.
At 16 mo post injury, patient was ambulating without assisted devices or brace and was pain free. Physical exam demonstrates active right knee range of motion of 15° to 85° and no extensor lag, no joint line tenderness and a 15° valgus deformity, 1+ laxity with Lachmans, anterior and posterior drawer with firm endpoint, symmetric with the contralateral side. There is 3+ laxity at the MCL; however, there is an endpoint, and no laxity with varus stress. Radiographs at that time demonstrated union at the fracture site and stable hardware fixation with no interval articular loss of reduction, valgus deformity of knee with lateral joint space narrowing, and posterior bony calcification, which may represent loose bodies. The patient is able to perform his duties at work without any difficulty, can perform all ADLs, and has minimal knee pain-he was able to play 18 holes of golf. Physical exam showed a moderate knee effusion, 3+ valgus laxity with endpoint, 15 degree valgus deformity, active range of motion 15-85 degrees, and no extensor lag. Knee replacement was discussed with the patient, however, he is happy with his outcome and he is not pursuing further surgery. His International Knee Documentation Committee (IKDC) score was 54.02.
A 59-year-old male presented to the ED after a motorcycle accident with a Schatzker II tibial plateau fracture and an avulsed tibial spine fracture causing rotational subluxation of the medial femoral condyle (Figure 3). While in the ED, he underwent an exam and an attempted reduction, which was unsuccessful due to intra-articular fragments. He was subsequently taken to the OR where left knee arthroscopy demonstrated an ACL injury with a tibial spine fracture button-holed through the MCL, which blocked the previous attempted reduction. The tibial spine was excised which allowed for reduction of the knee dislocation and subsequent ORIF of the left tibial plateau fracture. Intraoperative examination of the knee did not demonstrate valgus laxity and it was determined that the MCL injury did not require treatment. A plan of staged ligament reconstruction was discussed with the patient. He was discharged to an inpatient rehab center and instructed to maintain a non-weight bearing protocol in a hinged knee brace locked in extension for 6-8 wk.
Postoperatively at 1 mo, the patient had a pain level of 6 out of 10 and continued mild knee effusion in the left knee. Radiographs of the left knee showed abnormal widening of the medial compartment and lateral subluxation of the tibia; however, the tibial implants remained intact. On exam he had no definite endpoint when MCL was stressed at 0º and 30º of flexion. The patient was advised to continue non-weight bearing, and use of a brace locked in full extension. The patient was referred to a sports medicine trained orthopaedic surgeon who recommended a plan to stage MCL reconstruction after the tibial plateau fracture healed. The patient elected to proceed with conservative management of his MCL injury.
At two months post-op, he remained non weight bearing with minimal pain, 2/10 and passive ROM of 0°-75° flexion. Radiographic evaluation demonstrated interval healing of the tibial plateau with stable internal fixation, reduction of the tibial spine fracture, and valgus alignment of the knee with lateral subluxation of the tibia (Figure 4). He was instructed to begin passive range of motion exercises and to increase weight bearing with his knee brace locked in full extension.
At three months post-op, patient reported minimal pain with full weight bearing. He demonstrated significant atrophy of the left quadriceps, active flexion of 15-90. Radiographs showed increased callus formation at the fracture site with stable fixation of the hardware. Given the loss of joint space and persistent lateral subluxation of the tibia, the patient was referred to a total joint replacement specialist who recommended implant removal and total knee arthroplasty. The patient elected to delay total knee replacement and continue PT and strengthening. At 1.5 years post injury, the patient is satisfied with his function and stability, and feels they are adequate to perform job related activities and activities of daily living. Consequently, he continues to delay total joint replacement. Overall, he continues to have minimal pain, and demonstrates continued valgus laxity and lateral subluxation. His IKDC evaluation score was 32.2.
MKIs with tibial plateau fractures are severe, potentially life-altering injuries. Current literature describes treatment options for traumatic knee dislocations in younger populations who have isolated multiligamentous knee injuries, but there is no literature that describes treatment algorithms for middle-aged patients with multiligament knee reconstruction combined with tibial plateau fractures. The most pertinent aspect of our case reports is the decision making process that underlies the treatment of combined long bone fractures and multiligamentous knee injuries in an older middle aged patient. The difficulty in development of a treatment algorithm for these complex injuries lies in the low quality evidence (level III or IV studies) that have been published on these injuries. The limited literature examines various treatment methods and surgical techniques with a spectrum of outcome measures that are difficult to compare.
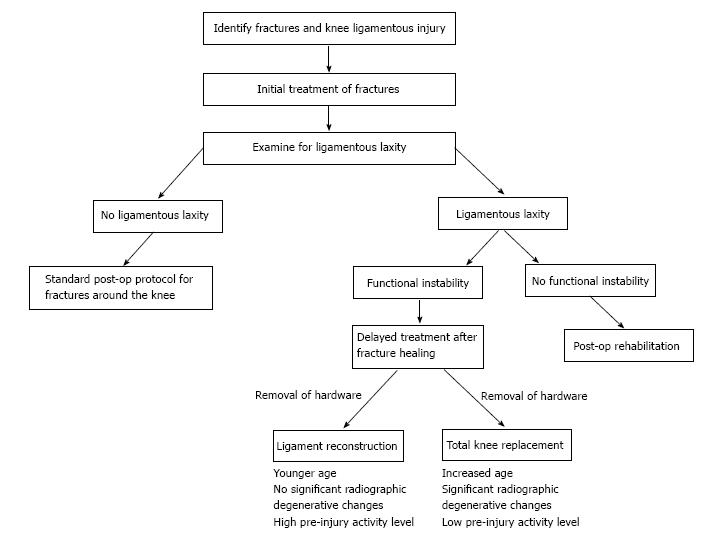
We propose the following algorithm for treating MKI with concomitant fracture in middle aged-patients. At initial presentation, a thorough examination for both bony and soft tissue injuries is performed. If a fracture is identified, treat surgically or non-surgically as appropriate, and re-evaluate ligamentous stability at 6 wk post-injury. As recommended by Stannard et al[15], the fracture should be treated first, and ACL and PCL injuries may be treated after fracture healing. If continued radiographic and clinical signs of instability are observed, a recommendation for staged reconstruction of ligamentous injury should be considered after bony union has been achieved. Surgical intervention is determined on a case by case basis, taking into account a patient’s pre-injury activity level and goals. If radiographic signs of instability are present but patient is asymptomatic for instability, consider nonoperative management of the injuries (Figure 5).
There are a few cases reported in the literature on this particular subset of 50-60 years old with multiligament knee injuries. Subbiah et al[16] reports on a 55 years old patient who underwent ACL and PCL reconstruction, resulting in a satisfactory Lysholm score of 90 and IKDC grading of B at fifteen months. Similarly, Ríos et al[9] performed multiligament reconstructions on two patients in their 60’s, resulting in good Lysholm scores twelve months after surgery, while also reporting on a 61-year-old patient treated conservatively for a PCL, MCL, and LCL injury which resulted in a poor rating[9]. According to results reported by Wasserstein et al[17] the risk of total knee arthroplasty for tibial plateau fractures alone is increased 5.3 times compared to normal age matched population and this risk increases even further when over 48 years of age. Furthermore there is also an increased risk of total knee replacement after isolated ACL reconstructions especially among patients older than 50 year of age[18], therefore it is not unreasonable to consider nonoperative treatment in these older patients for their combined tibial plateau and multiligamentous knee injuries.
Recent literature has shown early operative treatment with ligament reconstruction of MKIs leads to the most effective results in terms of return to prior activity[6]. While the data for nonoperative management has demonstrated poorer results, there is some evidence that these approaches can be successful. As we demonstrate in this case report, nonoperative treatment can provide good patient satisfaction and adequate functional outcomes. We describe two patients with complex knee injuries, involving both ligaments and bone fractures, who were treated nonoperatively for their ligamentous injuries with good final outcomes and patient satisfaction. We also describe a treatment algorithm for these complex injuries.
There is a need for further study in middle-aged to elderly patients, who may achieve successful outcomes and pain control from nonoperative treatment which has lower morbidity as well as requires less dependence on medical resources. We recommend counseling patients that nonoperative management for ligamentous injury is an option, but that knee arthroplasty may be indicated if posttraumatic arthritis develops.
Two patients in their 50’s presenting after high impact motor vehicle collisions with multiple skeletal injuries.
The patient’s main complaints were chronic swelling with recent onset of mechanical symptoms, specifically popping, catching, and locking while performing daily activities.
Radiographic and CT imaging was performed on both patients.
Both patients were treated with open reduction internal fixation.
Current literature describes treatment options for traumatic knee dislocations in younger populations who have isolated multiligamentous knee injuries, but there is no literature that describes treatment algorithms for middle-aged patients with multiligament knee reconstruction combined with tibial plateau fractures.
These cases indicate a need for further study in middle-aged to elderly patients, who may achieve successful outcomes and pain control from nonoperative treatment which has lower morbidity as well as requires less dependence on medical resources.
This is an interesting report on tibia plateau fractures and complex ligament Injury. The paper is written and presented quite well and therefore publication is recommended.
P- Reviewer: Trieb K S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Chahal J, Dhotar HS, Zahrai A, Whelan DB. PCL reconstruction with the tibial inlay technique following intra-medullary nail fixation of an ipsilateral tibial shaft fracture: a treatment algorithm. Knee Surg Sports Traumatol Arthrosc. 2010;18:777-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Thiagarajan P, Ang KC, Das De S, Bose K. Ipsilateral knee ligament injuries and open tibial diaphyseal fractures: incidence and nature of knee ligament injuries sustained. Injury. 1997;28:87-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | van Raay JJ, Raaymakers EL, Dupree HW. Knee ligament injuries combined with ipsilateral tibial and femoral diaphyseal fractures: the “floating knee”. Arch Orthop Trauma Surg. 1991;110:75-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Walker DM, Kennedy JC. Occult knee ligament injuries associated with femoral shaft fractures. Am J Sports Med. 1980;8:172-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 29] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Skendzel JG, Sekiya JK, Wojtys EM. Diagnosis and management of the multiligament-injured knee. J Orthop Sports Phys Ther. 2012;42:234-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Mook WR, Miller MD, Diduch DR, Hertel J, Boachie-Adjei Y, Hart JM. Multiple-ligament knee injuries: a systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am. 2009;91:2946-2957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 142] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 7. | Manske RC, Hosseinzadeh P, Giangarra CE. Multiple ligament knee injury: complications. N Am J Sports Phys Ther. 2008;3:226-233. [PubMed] |
| 8. | Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, Boyd JL, MacDonald PA, Marx RG. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25:430-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 292] [Article Influence: 18.3] [Reference Citation Analysis (1)] |
| 9. | Ríos A, Villa A, Fahandezh H, de José C, Vaquero J. Results after treatment of traumatic knee dislocations: a report of 26 cases. J Trauma. 2003;55:489-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 88] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Wilson SM, Mehta N, Do HT, Ghomrawi H, Lyman S, Marx RG. Epidemiology of multiligament knee reconstruction. Clin Orthop Relat Res. 2014;472:2603-2608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Mills WJ, Nork SE. Open reduction and internal fixation of high-energy tibial plateau fractures. Orthop Clin North Am. 2002;33:177-198, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Ebraheim NA, Sabry FF, Haman SP. Open reduction and internal fixation of 117 tibial plateau fractures. Orthopedics. 2004;27:1281-1287. [PubMed] |
| 13. | Taylor AR, Arden GP, Rainey HA. Traumatic dislocation of the knee. A report of forty-three cases with special reference to conservative treatment. J Bone Joint Surg Br. 1972;54:96-102. [PubMed] |
| 14. | Liow RY, McNicholas MJ, Keating JF, Nutton RW. Ligament repair and reconstruction in traumatic dislocation of the knee. J Bone Joint Surg Br. 2003;85:845-851. [PubMed] |
| 15. | Stannard JP, Schenck RC Jr. Fanelli GP. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia: Lippincott Williams & Wilkins 2009; 1833-1864. |
| 16. | Subbiah M, Pandey V, Rao SK, Rao S. Staged arthroscopic reconstructive surgery for multiple ligament injuries of the knee. J Orthop Surg (Hong Kong). 2011;19:297-302. [PubMed] |
| 17. | Wasserstein D, Henry P, Paterson JM, Kreder HJ, Jenkinson R. Risk of total knee arthroplasty after operatively treated tibial plateau fracture: a matched-population-based cohort study. J Bone Joint Surg Am. 2014;96:144-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 161] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 18. | Leroux T, Ogilvie-Harris D, Dwyer T, Chahal J, Gandhi R, Mahomed N, Wasserstein D. The risk of knee arthroplasty following cruciate ligament reconstruction: a population-based matched cohort study. J Bone Joint Surg Am. 2014;96:2-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |