Published online Dec 18, 2015. doi: 10.5312/wjo.v6.i11.996
Peer-review started: February 27, 2015
First decision: April 28, 2015
Revised: July 21, 2015
Accepted: August 4, 2015
Article in press: August 7, 2015
Published online: December 18, 2015
Processing time: 293 Days and 7 Hours
AIM: To compare minimally invasive (MIS) and open techniques for MIS lumbar laminectomy, direct lateral and transforaminal lumbar interbody fusion (TLIF) surgeries with respect to length of surgery, estimated blood loss (EBL), neurologic complications, perioperative transfusion, postoperative pain, postoperative narcotic use, and length of stay (LOS).
METHODS: A systematic review of previously published studies accessible through PubMed was performed. Only articles in English journals or published with English language translations were included. Level of evidence of the selected articles was assessed. Statistical data was calculated with analysis of variance with P < 0.05 considered statistically significant.
RESULTS: A total of 11 pertinent laminectomy studies, 20 direct lateral studies, and 27 TLIF studies were found. For laminectomy, MIS techniques resulted in a significantly longer length of surgery (177.5 min vs 129.0 min, P = 0.04), shorter LOS (4.3 d vs 5.3 d, P = 0.01) and less perioperative pain (visual analog scale: 16 ± 17 vs 34 ± 31, P = 0.04). There is evidence of decreased narcotic use for MIS patients (postoperative intravenous morphine use: 9.3 mg vs 42.8 mg), however this difference is of unknown significance. Direct lateral approaches have insufficient comparative data to establish relative perioperative outcomes. MIS TLIF had superior EBL (352 mL vs 580 mL, P < 0.0001) and LOS (7.7 d vs 10.4 d, P < 0.0001) and limited data to suggest lower perioperative pain.
CONCLUSION: Based on perioperative outcomes data, MIS approach is superior to open approach for TLIF. For laminectomy, MIS and open approaches can be chosen based on surgeon preference. For lateral approaches, there is insufficient evidence to find non-inferior perioperative outcomes at this time.
Core tip: Perioperative outcomes in minimally invasive (MIS) approaches to the lumbar spine have not been specifically examined in systematic reviews of MIS lumbar laminectomy, direct lateral and transforaminal lumbar interbody fusion (TLIF) surgeries. Based on perioperative outcomes data, MIS approach is superior to open approach for TLIF. For laminectomy, MIS and open approaches can be chosen based on surgeon preference. For lateral approaches, there is insufficient evidence to find non-inferior perioperative outcomes at this time.
- Citation: Skovrlj B, Belton P, Zarzour H, Qureshi SA. Perioperative outcomes in minimally invasive lumbar spine surgery: A systematic review. World J Orthop 2015; 6(11): 996-1005
- URL: https://www.wjgnet.com/2218-5836/full/v6/i11/996.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i11.996
Minimally invasive surgical (MIS) approaches to lumbar spinal surgery have been an area of increasing clinical interest for over 50 years. Percutaneous approaches to lumbar disk herniation began with chemonucleolysis treatment for sciatica by Smith[1] in 1964. In 1997, Smith[1] and Foley et al[2] introduced the tubular distraction system for a microendoscopic approach to microdiscectomy. This system allowed direct visualization of the surgical field while minimizing dissection and distraction of the paraspinal muscles and thoracolumbar fascia. By reducing the size of the operative field and reducing the number of damaged blood vessels, muscles and fascial structures, blood loss and post-operative pain would be reduced, leading to a shorter hospital stay, faster time to mobilization, and reduced post-operative analgesia needs.
After the development of the microendoscopic microdiscectomy, there were a series of rapid advances, applying the technology to other surgeries. In 1998, McAfee et al[3] described the direct lateral interbody fusion (DLIF) as an alternative to anterior lumbar interbody fusion (ALIF). Foley et al[4] described the MIS transforaminal lumbar interbody fusion (TLIF) in 2003, followed by Mummaneni et al[5] detailing the Mini-Open TLIF. In 2006, Ozgur et al[6] described the extreme lateral interbody fusion (XLIF) as another minimally invasive alternative to the ALIF. In 2010, a new, purely percutaneous approach for laminotomy and decompression, the Minimally Invasive Lumbar Decompression (mild®), was described by Chopko et al[7].
The initial hope that MIS approaches to the lumbar spine would lead to long-term reductions in patient-reported pain relative to open approaches has not yet been substantiated. Most studies of long-term results have reported similar outcomes between MIS and traditional open surgeries[8-10]. This leaves short-term measures, specifically perioperative outcomes, as the main possible distinguishing clinical feature between MIS lumbar spinal surgery and open surgical technique. There have not been any systematic reviews specifically focusing on perioperative outcomes across minimally invasive lumbar spinal surgical modalities, nor have there been systematic reviews of either minimally invasive laminectomy or far lateral fusion approaches.
This systematic review examines perioperative outcomes in minimally invasive lumbar spinal surgeries across several surgery types for adult degenerative spine disease: (1) MIS laminectomy vs open laminectomy; (2) MIS TLIF vs open TLIF; and (3) MIS XLIF and DLIF vs ALIF.
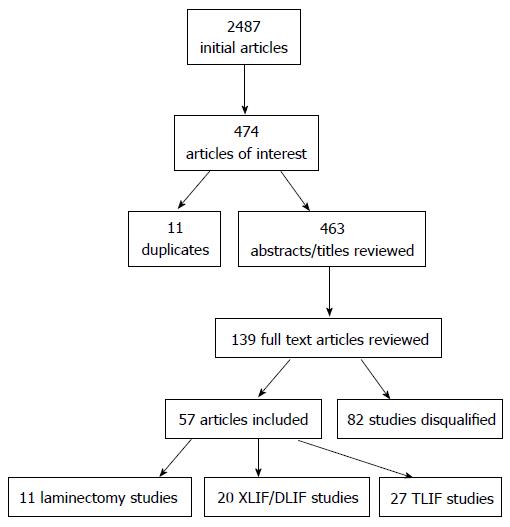
A series of searches using the PubMed-National Library of Medicine/National Institutes of health (http://www.ncbi.nlm.nih.gov) database were performed. Only articles in English journals or published with English abstracts were included. Level of evidence of the selected articles was assessed. Search keywords included: “minimally invasive”, “spine surgery”, “laminectomy”, “TLIF”, “DLIF”, “XLIF”, and “ALIF”. Abstracts were reviewed for clinical studies that reported perioperative outcomes in relevant surgical intervention categories (Figure 1).
Studies were only included if they categorically used “laminectomy” for all subjects. Kinoshita et al[11] performed laminotomies for single level decompression, and sometimes performed laminectomies for multiple level decompression. It can be argued that laminotomy vs laminectomy is a distinction without a difference, but including laminotomies would then bring a number of microdiscectomy techniques into the range of covered studies. As this would introduce significant heterogeneity into the category, only studies describing laminectomy as part of the decompression surgery were included in the laminectomy category.
TLIF studies were included regardless of whether bilateral or unilateral instrumentation was used. Only studies with both an open TLIF and an MIS TLIF arm were included. Studies that compared MIS TLIF with posterior lumbar interbody fusion (PLIF) or did not report TLIF and PLIF results separately were excluded.
Axial lumbar interbody fusion (AxiaLIF) studies were not included. Studies with large portions of the study population receiving dual fixation (XLIF plus PLIF) were excluded.
Perioperative outcomes of interest examined in this systematic review include the following: (1) Length of surgery; (2) Estimated blood loss (EBL); (3) Neurologic complications; (4) Perioperative transfusion; (5) Postoperative pain; (6) Postoperative narcotic use; and (7) Length of stay (LOS).
Results were tabulated by intervention, indication for intervention, data by study arm, and relevant qualifications (bias, observer status, etc.) gathered. Multiple reports of the data from the same patient population were disregarded. Data from similar studies was pooled and calculated with analysis of variance (ANOVA). Numerical data that was reported stratified into subgroups other than MIS/non-MIS, were re-pooled and calculated with ANOVA. Numerical data only reported in graph form were incorporated using graphical methods. Durotomy and cerebrospinal fluid leak were included as reportable neurologic complications. Incorporation of isolated additional neurologic complications resulted in some study groups having complication rates above 100%. In order to summarize data across studies, joint statistics were calculated using ANOVA. The statistical review of this study was performed by a biomedical statistician.
No studies found used independent observers for EBL or neurologic complications. At least two studies reported change in hemoglobin, presumably independently measured, but did not separately report patient fluid balance[12,13]. No studies used defined criteria for or an independent or blinded observer to decide the following study parameters: (1) Hospital discharge eligibility (i.e., LOS); (2) Opiate prescription or availability; and (3) Need for perioperative transfusion.
Identified pertinent studies are shown in Table 1, including three randomized controlled trials (RCTs) (Cho et al[14], Usman et al[15] and Watanabe et al[16]), one incompletely randomized trial (Mobbs et al[17]; randomized by consecutive, odd/even patient order[18]), and one cohort comparison study[12]. In Table 2, results for length of surgery, EBL, rate of neurologic complications, and LOS are shown. Pooling across RCTs/incomplete-RCTs with published standard deviations, length of surgery was significantly longer for MIS surgeries than open surgeries (177.5 min vs 129.0 min, P = 0.004), EBL was non-significantly less in MIS surgeries (115.0 mL vs 102.1 mL, P = 0.580), and LOS was significantly shorter following MIS surgeries than open surgeries (4.3 d vs 5.3 d, P = 0.010). Pooled rates of neurological complications in the two RCTs specifically reporting complications by group showed non-significantly higher rates of complications in open procedures (2.0% MIS vs 4.3% open, P = 0.52).
| Ref. | Year | Surgery | Population | MIS patients | Open patients |
| RCTs/IRCTs | |||||
| Cho et al[14] | 2007 | Split process laminectomy: Marmot operation | LSS | 40 | 30 |
| Usman et al[15] | 2013 | Unilateral laminectomy | LSS, no spondylolisthesis | 30 | 30 |
| Mobbs et al[17] | 2014 | Laminectomy: Unilateral laminectomy for bilateral decompression | LSS, max 2 levels, no spondylolisthesis | 27 | 27 |
| Watanabe et al[16] | 2011 | Lumbar spinous process-splitting laminectomy | Neurogenic claudication | 22 | 19 |
| Clinical case series | |||||
| Rahman et al[18] | 2008 | Laminectomy | LSS, no discectomy | 38 | 88 |
| Nomura et al[19] | 2014 | Laminectomy: Spinous process-splitting laminectomy | Spondylolisthesis, LSS due to herniation | 124 | - |
| Parikh et al[20] | 2008 | Laminectomy | Degenerative disease | 75 | - |
| Komp et al[21] | 2011 | Laminectomy: Unilateral laminectomy for bilateral decompression | LSS, no spondylolisthesis > 1 | 74 | - |
| Nomura et al[22] | 2012 | Laminectomy: Unilateral laminectomy for bilateral decompression: Paramedian approach | LSS, no discectomy | 70 | - |
| Tomasino et al[23] | 2009 | Laminectomy: Unilateral laminectomy for bilateral decompression | LSS, herniation in obese | 28 | - |
| Wada et al[24] | 2010 | Laminectomy | LSS, elderly patients | 15 | - |
| Length of surgery (min) ± SD | Estimated blood loss (cc) ± SD | Neurologic complications | Length of stay (d) ± SD | |||||
| MIS | Open | MIS | Open | MIS | Open | MIS | Open | |
| RCTs/IRCTs | ||||||||
| Cho et al[14] | 259 ± 122 | 193 ± 68 | 154 ± 135 | 132 ± 128 | - | - | 4.0 ± 2.9 | 7.2 ± 1.6 |
| Usman et al[15] | 69 ± 0.1 | 65 ± 0.1 | - | - | - | - | 4.7 ± 0.5 | 3.5 ± 0.5 |
| Mobbs et al[17] | - | - | 40 | 110 | 4% | 7% | 2.3 | 4.2 |
| Watanabe et al[16] | 69 ± 29 | 82 ± 36 | 44 ± 75 | 55 ± 48 | 0% | 0% | - | - |
| Clinical case series | ||||||||
| Rahman et al[18] | 110 ± 10 | 157 ± 7 | 52 ± 14 | 246 ± 32 | 5% | 8% | 2.1 ± 0.7 | 4.1 ± 0.4 |
| Nomura et al[19] | 187 ± 68 | - | 90 ± 94 | - | 2% | - | - | - |
| Parikh et al[20] | 118 ± 40 | - | 41 ± 90 | - | 11% | - | 1.2 | 1.3 |
| Komp et al[21] | 44 | - | 01 | - | 14% | - | - | - |
| Nomura et al[22] | 772 | - | 15.02 | - | 0% | - | - | - |
| Tomasino et al[23] | 102 ± 44 | - | 35 ± 76 | - | 11% | - | 2.1 | 2.2 |
| Wada et al[24] | 144 | - | 60 | - | 7% | - | - | - |
Three studies specifically examined rates of post-operative pain in these patient groups. Watanabe et al[16] examined the visual analog scale (VAS) score for post-operative wound pain on post-operative day 7 and found a VAS of 16 (± 17) for MIS patients and a VAS of 34 (± 31) for open laminectomies, a statistically significant difference (P = 0.04). Mobbs et al[17] examined post-operative narcotic use during hospital stay and found an intravenous morphine equivalent of 9.3 mg in MIS patients and 42.8 mg in open patients, a difference of unknown statistical significance (P value not stated). Komp et al[21] reported that “no operation-related pain medication was required” in their MIS case series.
No studies reported a need for transfusions following either MIS or open laminectomy.
No randomized trials using an ALIF control arm were identified in the literature search. One RCT had XLIF as part of the intervention in both the study arm and control arm groups[25]. Two studies mixed traumatic and/or post-infectious patients in the study population; as these indications were in the minority in each of these studies, the studies were included[13,26].
Identified pertinent studies are shown in Table 3, including four cohort control studies and 15 case series. In Table 4, results for length of surgery, EBL, rate of neurologic complications, and LOS are shown. In the authors’ opinion, the current non-randomized data does not justify pooling or a meta-analysis due to heterogeneity and potential bias. Only one study (Huang et al[29]) was a prospectively designed and enrolled study; and, it used an approach (minimal access ALIF) that has not been repeated in any other study.
| Ref. | Year | Surgery | Type of study | Population | MIS patients | Open patients |
| Cohort studies | ||||||
| Hrabalek et al[27] | 2014 | XLIF | Retrospective cohort, XLIF vs ALIF | DDD, FBSS, spondylolisthesis | 88 | 120 |
| Smith et al[28] | 2012 | XLIF | Retrospective cohort, XLIF vs ALIF | DDD, LSS, FBSS, spondylolisthesis, herniation | 115 | 87 |
| 1Rodgers et al[12] | 2010 | XLIF | Retrospective cohort, XLIF vs PLIF | > 80 yr, LSS, FBSS spondylolisthesis, scoliosis, fracture | 40 | 20 |
| Huang et al[29] | 2010 | MIS-ALIF2 | Prospective cohort, MIS-ALIF vs ALIF | Not defined | 10 | 13 |
| Case series | ||||||
| 3Rodgers et al[13] | 2011 | XLIF | PCS | LSS, DDD, FBSS, spondylolisthesis, scoliosis | 600 | - |
| Ruetten et al[30] | 2005 | XLIF | RCS | Lumbar disc prolapse | 463 | - |
| Lykissas et al[31] | 2014 | XLIF | RCS | Degenerative spinal conditions | 144 | - |
| Grimm et al[32] | 2014 | XLIF | RCS | DDD, LSS, FBSS, scoliosis, spondylolisthesis, herniation | 108 | - |
| Tohmeh et al[33] | 2011 | XLIF | PCS | LSS, DDD, spondylolisthesis, spondylosis, scoliosis, recurrent herniation, ASD | 102 | - |
| Berjano et al[34] | 2012 | XLIF | RCS | DDD, LSS, spondylolisthesis | 97 | - |
| Lee et al[26] | 2014 | DLIF | RCS | LSS, spondylolisthesis, scoliosis, post-infectious | 90 | - |
| Marchi et al[35] | 2012 | XLIF | PCS | Spondylolisthesis | 52 | - |
| Sharma et al[36] | 2011 | XLIF | RCS | Spondylosis ± listhesis, scoliosis | 43 | - |
| Pimenta et al[25] | 2011 | XLIF | PCS | DDD | 36 | - |
| Ahmadian et al[37] | 2013 | XLIF | RCS | L4/L5 spondylolisthesis | 31 | - |
| Caputo et al[38] | 2012 | XLIF | PCS | Scoliosis | 30 | - |
| Malham et al[39] | 2012 | XLIF | PCS | DDD, spondylolisthesis, scoliosis | 30 | - |
| 4Pimenta et al[40] | 2013 | XLIF | RCT | L4/L5 DDD | 30 | - |
| Elowitz et al[41] | 2011 | XLIF | PCS | LSS | 25 | - |
| Oliveira et al[42] | 2010 | XLIF | PCS | Degenerative spinal conditions | 21 | - |
| Ref. | Length of surgery (min) ± SD | Estimated blood loss (cc) ± SD | Neurologic complications | Length of stay (d) ± SD | ||||
| MIS | Open | MIS | Open | MIS | Open | MIS | Open | |
| Cohort studies | ||||||||
| Hrabalek et al[27] | - | - | - | - | 28% | 24% | - | - |
| Smith et al[28] | 112 ± 31 | 173 ± 31 | 90 ± 74 | 311 ± 370 | 3% | 6% | 1.7 ± 1.3 | 3.6 ± 0.9 |
| Rodgers et al[12] | - | - | 1.4 g Hb | 2.7 g Hb | - | - | 1.3 | 5.3 |
| Huang et al[29] | 176 ± 8 | 202 ± 15 | 572 ± 93 | 970 ± 209 | - | - | 11.6 ± 1.3 | 12.5 ± 1.3 |
| Case series | ||||||||
| Rodgers et al[13] | - | - | 1.38 g Hb | - | 1% | - | 1.2 | - |
| Ruetten et al[30] | 27 | - | 01 | - | 0% | - | - | - |
| Lykissas et al[31] | 295 ± 180 | - | - | - | 135% | - | - | - |
| Grimm et al[32] | 122 | - | 181 | - | 20% | - | 3.0 | - |
| Tohmeh et al[33] | - | - | - | - | 48% | - | - | - |
| Berjano et al[34] | - | - | - | - | 16% | - | - | - |
| Lee et al[26] | 52 ± 19 | - | 01 | - | 19% | - | - | - |
| Marchi et al[35] | 73 ± 31 | - | < 50 | - | 29% | - | - | - |
| Sharma et al[36] | - | - | - | - | 70% | - | - | - |
| Pimenta et al[25] | 130 | - | - | - | 28% | - | 1.4 | - |
| Ahmadian et al[37] | - | - | 94 | - | - | - | 3.5 | - |
| Caputo et al[38] | - | - | - | - | 2 | - | - | - |
| Malham et al[39] | 84 | - | 70 | - | 20% | - | - | - |
| Pimenta et al[40] | 69 ± 11 | - | < 50 | - | 13% | - | - | - |
| Elowitz et al[41] | - | - | - | - | 20%3 | - | - | - |
| Oliveira et al[42] | 86 | - | 44 | - | 14% | - | 1.2 | - |
Within the reported data for MIS anterior fusion approaches, average length of surgery varied from 27 min to 295 min, average EBL from “not measureable” to 572 mL, and neurologic complication rates varied from 0% to 130%.
Two studies reported on perioperative transfusion use in this patient population. Hrabalek et al[27] reported a 0% transfusion use in the MIS XLIF and open ALIF cohorts. Rodgers’s 2010 study, focusing on patients 80 years of age and older, reported no use of perioperative transfusion in MIS XLIF patients, but a 70% rate of transfusion in PLIF patients[12]. Regarding non-controlled studies, Rodgers et al[13] reported a 0.2% rate of transfusion in XLIF patients, while Berjano et al[34] reported a 1% transfusion rate.
Three non-controlled studies reported on perioperative pain and narcotic use in patients treated with lateral interbody fusion. Ruetten et al[30] reported a mean VAS back of 4 (out of 100) and a VAS leg of 14 (out of 100) on post-operative day 1, stating that no post-operative pain medication was required in their 463 patient series. Marchi et al[35] reported mean VAS back of 45 and VAS leg of 31 one week following surgery, while Pimenta et al[40] reported a combined VAS Back/Leg value of 50 at the same time point.
Virtually all of the data gathered involved application of the XLIF (NuVasive, San Diego, California, United States) system; there is at this point limited data on other systems.
Identified pertinent studies are shown in Table 5, including 1 RCT (Wang et al[43]) and 2 incompletely randomized controlled trials (Shunwu et al[44]: Randomized by admission date; Wang et al[45]: randomized by consecutive, odd/even patient order). In Table 6, results for length of surgery, EBL, rate of neurologic complications, and LOS are shown. Pooling across RCTs and incompletely-RCTs with published standard deviations, length of surgery was non-significantly longer for MIS surgeries than open surgeries (150 min vs 143 min, P = 0.09), EBL was significantly less in MIS surgeries (352 mL vs 580.9 mL, P < 0.0001), and LOS was significantly shorter following MIS surgeries than open surgeries (7.7 d vs 10.4 d, P < 0.0001). Pooled rates of neurological complications in the two RCTs specifically reporting complications by group showed non-significantly higher rates of complications in open procedures (4.1% MIS vs 5.3% open, P = 0.697).
| Ref. | Year | Surgery | Population | MIS patients | Open patients |
| RCTs/IRCTs | |||||
| Wang et al[43] | 2011 | TLIF | LSS, herniation, spondylolisthesis | 41 | 38 |
| Shunwu et al[44] | 2010 | TLIF | Degenerative lumbar disease | 32 | 30 |
| Wang et al[45] | 2011 | TLIF | Failed discectomy and decompression | 25 | 27 |
| Cohort studies | |||||
| Wong et al[46] | 2014 | TLIF | FBSS, DDD, spondylolisthesis | 144 | 54 |
| Zhang et al[47] | 2013 | TLIF | DDD | 82 | 76 |
| Villavicencio et al[48] | 2010 | TLIF | LSS, DDD ± herniation, spondylolisthesis | 76 | 63 |
| Lee et al[49] | 2012 | TLIF | LSS, DDD, herniation, spondylolisthesis | 72 | 72 |
| Terman et al[50] | 2014 | TLIF | DDD, LSS, spondylolisthesis, herniation | 53 | 21 |
| Cheng et al[51] | 2013 | TLIF | Spondylosis/listhesis, foraminal stenosis | 50 | 25 |
| Liang et al[52] | 2011 | TLIF | Degenerative lumbar instability | 45 | 42 |
| Yang et al[53] | 2013 | TLIF | Lumbar degenerative diseases | 43 | 104 |
| Gu et al[54] | 2014 | TLIF | Degenerative conditions | 43 | 38 |
| Wang et al[55] | 2010 | TLIF | Spondylolisthesis | 42 | 43 |
| Zairi et al[56] | 2013 | Mini open TLIF | DDD, spondylolisthesis | 40 | 60 |
| Seng et al[57] | 2013 | TLIF | DDD, spondylolisthesis | 40 | 40 |
| Pelton et al[58] | 2012 | TLIF | DDD, spondylolisthesis | 33 | 33 |
| Singh et al[59] | 2014 | TLIF | DDD, spondylolisthesis | 33 | 33 |
| Brodano et al[60] | 2013 | Mini open TLIF | DDD, spondylolisthesis | 30 | 34 |
| Zou et al[61] | 2013 | TLIF | LSS, spondylolisthesis, herniation | 30 | 30 |
| 1Peng et al[62] | 2009 | TLIF | DDD, spondylolisthesis | 29 | 29 |
| Archavlis et al[63] | 2013 | TLIF | SDS and severe FJO | 24 | 25 |
| Dhall et al[64] | 2008 | Mini open TLIF | DDD, spondylolisthesis | 21 | 21 |
| Schizas et al[65] | 2009 | TLIF | DDD, spondylolisthesis | 18 | 18 |
| Adogwa et al[66] | 2011 | TLIF | Grade I spondylolithesis | 15 | 15 |
| Niesche et al[67] | 2014 | TLIF | Recurrent lumbar disc herniation | 14 | 19 |
| Lau et al[68] | 2011 | TLIF | Spondylosis/listhesis/lysis | 10 | 12 |
| Ref. | Length of surgery (min) ± SD | Estimated blood loss (cc) ± SD | Neurologic complications | Length of stay (d) ± SD | ||||
| MIS | Open | MIS | Open | MIS | Open | MIS | Open | |
| RCTs/IRCTs | ||||||||
| Wang et al[43] | 168.7 ± 36.4 | 145.0 ± 26.8 | 207.7 ± 57.6 | 258.9 ± 122.2 | 2% | 0% | 6.4 ± 2.5 | 8.7 ± 2.1 |
| Shunwu et al[44] | 159.2 ± 21.7 | 142.8 ± 22.5 | 399.8 ± 125.8 | 517.0 ± 147.8 | 0% | 0% | 9.3 ± 2.6 | 12.5 ± 1.8 |
| Wang et al[45] | 139.0 ± 27.0 | 143.0 ± 35.0 | 291.0 ± 86.0 | 652.0 ± 150.0 | 12% | 19% | - | - |
| Cohort studies | ||||||||
| Wong et al[46] | 173 | 309 | 115 | 485 | 12% | 13% | 2.8 | 4.4 |
| Zhang et al[47] | 120 ± 35 | 115 ± 28 | 250 ± 75 | 650 ± 150 | 0% | 3% | - | - |
| Villavicencio et al[48] | 223 ± 68 | 215 ± 60 | 163 ± 131 | 367 ± 298 | 11% | 13% | 3.0 ± 2.3 | 4.2 ± 3.5 |
| Lee et al[49] | 166 ± 52 | 182 ± 45 | 161 ± 51 | 447 ± 519 | 1% | 0% | 3.2 ± 2.9 | 6.8 ± 3.4 |
| Terman et al[50] | - | - | 100 | 450 | - | - | 2.0 | 3.0 |
| Cheng et al[51] | 245 ± 73 | 279 ± 15 | 393 ± 284 | 536 ± 324 | 0% | 12% | 4.8 ± 1.8 | 6.1 ± 1.8 |
| Liang et al[52] | 127 ± 60 | 96 ± 46 | 194 ± 86 | 357 ± 116 | - | - | - | - |
| Yang et al[53] | 175 ± 35 | 177 ± 30 | 362 ± 177 | 720 ± 171 | 7% | 2% | 4.0 ± 1.3 | 7.1 ± 1.0 |
| Gu et al[54] | 196 ± 28 | 187 ± 23 | 248 ± 94 | 576 ± 176 | 5% | 3% | 9.3 ± 3.7 | 12.1 ± 3.6 |
| Wang et al[55] | 145 ± 27 | 156 ± 32 | 264 ± 89 | 673 ± 145 | 10% | 7% | 10.6 ± 2.5 | 14.6 ± 3.8 |
| Zairi et al[56] | 170 | 186 | 148 | 486 | 3% | 3% | 4.5 | 5.5 |
| Seng et al[57] | 185 ± 9 | 166 ± 7 | 127 ± 46 | 405 ± 80 | - | - | - | - |
| Pelton et al[58] | 112 ± 33 | 185 ± 34 | 125 ± 76 | 275 ± 99 | - | - | 2.0 ± 0.7 | 3.0 ± 1.1 |
| Singh et al[59] | 116 ± 28 | 186 ± 31 | 124 ± 92 | 380 ± 191 | - | - | 2.3 ± 1.2 | 2.9 ± 1.1 |
| Brodano et al[60] | 144 | 102 | 230 | 620 | 3% | 9% | 4.1 | 7.4 |
| Zou et al[61] | 150 ± 41 | 175 ± 37 | 131 ± 74 | 318 ± 177 | 0% | 0% | 7.5 ± 2.7 | 9.3 ± 4.2 |
| Peng et al[62] | 216 | 171 | 150 | 681 | - | - | 4.0 | 6.7 |
| Archavlis et al[63] | 220 ± 48 | 190 ± 65 | 185 ± 140 | 255 ± 468 | 13% | 4% | 7.0 | 11.0 |
| Dhall et al[64] | 199 | 237 | 194 | 505 | 0% | 5% | 3.0 | 5.5 |
| Schizas et al[65] | - | - | 456 | 961 | 17% | 6% | 6.1 | 8.2 |
| Adogwa et al[66] | 300 | 210 | 200 | 295 | 0% | 0% | 3.0 | 5.0 |
| Niesche et al[67] | 140 | 130 | 150 | 380 | 0% | 11% | 5.0 | 10.0 |
| Lau et al[68] | 390 | 365 | 467 | 566 | 0% | 0% | 5.0 | 6.2 |
Regarding post-operative pain, Wang et al[45] polled patients on post-operative day 2, finding a VAS back of 2.2 ± 0.6 in MIS patients and 4.3 ± 0.5, a statistically significant difference (P < 0.05). Investigating the need for perioperative blood transfusions, Shunwu et al[44] found that 0 of 32 of the MIS patients needed transfusion, while the 30 open patients needed an average of 0.40 units of blood (SD: 0.97), a significant difference (P = 0.017).
The current growing trends in the use of MIS approaches in lumbar spine surgery have led to a concerted effort to compare outcomes between MIS and open techniques. Previous studies on long-term outcomes between MIS and open approaches in lumbar spine surgery have not revealed a significant difference between the two approaches[8-10]. This is the first systematic review of perioperative outcomes in lumbar MIS lumbar spine surgery aiming to reveal differences between MIS and open techniques in terms of lengths of surgery, EBL, neurologic complications, perioperative transfusion, postoperative pain, postoperative narcotic use and LOS.
To facilitate the interpretation of the currently existing data, lumbar spine procedures were divided into different types including decompressive laminectomy and interbody fusions. Interbody fusions were further subdivided into TLIF and lateral vs anterior interbody fusions.
In decompressive laminectomy, this study found the muscle-sparing MIS approach to result in significantly longer operative times compared to the open approach (177.5 min vs 129.0 min, P = 0.004). Although decompressive lumbar laminectomy is a relatively straightforward spinal operation, there exists a steep learning curve associated with microscope-assisted tubular spinal surgery[68], which could be one important factor accounting for the differences in operative times between the two techniques. With the growing popularity of minimally invasive approaches and the growing number of younger surgeons performing minimally invasive approaches, over time, as younger surgeons become more proficient with MIS techniques, operative times will likely decrease and we could see a decrease in the difference in operative times between MIS and open lumbar decompressions.
This study also found that patients undergoing MIS decompression were found to have less postoperative pain, lower perioperative transfusion rates and decreased LOS compared to those who underwent open decompression. These findings are not surprising given that the MIS technique results in significantly smaller surgical incisions, is muscle sparing and bypasses the need for extensive paraspinal and soft tissue stripping.
In terms of perioperative outcomes following lumbar decompressive laminectomy, there is a state of equipoise between MIS and open approaches, with neither technique clearly superior. At this time, individual patient and surgeon preferences are appropriate to guide decision making until further evidence becomes available.
Lumbar interbody fusion has become a popular surgical tool in the treatment of a wide variety of lumbar pathology including degenerative disc disease, recurrent lumbar herniation, spondylolisthesis and complex lumbar stenosis[69]. Currently popular approaches for achieving lumbar interbody fusion include the open anterior (ALIF) and MIS lateral (DLIF and XLIF) retroperitoneal approaches and the open and MIS posterior transforaminal (TLIF) approaches. While each one of these approaches utilizes a different anatomic corridor, they all have a common end goal of achieving interbody fusion. However, approach specific limitations and direct and indirect complications make each one of these approaches unique and worthy of comparison.
There are currently no randomized trials comparing ALIF and DLIF/XLIF in the literature. There is a wide variation in the reported outcomes data between MIS and open approaches for ALIF and DLIF/XLIF and this heterogeneity does not allow for meta-analysis of the current literature due to the high risk of potential bias. Furthermore, all of the currently available literature on lateral approaches involves the use of a single commercial system (XLIF, NuVasive, San Diego, California, United States) while there are currently many different commercial systems in use across the country.
There is currently a dearth of high quality literature on MIS alternatives (DLIF, XLIF) to ALIF. Although there appears to be no evidence of inferiority, these approaches should be considered investigational by surgeons and patients until better quality studies justify evidence-based statements of non-inferiority.
There have been several high quality studies in the literature comparing MIS TLIF and open TLIF surgeries. In terms of EBL, LOS, transfusion need and perioperative pain, the current data all favor MIS TLIF.
Although EBL differences across randomized studies did not reach clinically meaningful levels of ≥ 750 mL, one of the randomized studies did find a significantly reduced transfusion need between MIS and open TLIF[44].
LOS was found to be significantly reduced in MIS TLIF by almost three days, however all of the studies originated from Chinese hospitals. LOS effect estimates, however, may not be applicable across countries, as different health systems use different discharge qualifications and have appreciably different LOS for similar procedures.
There are no outcome categories reported that identify MIS approaches to be significantly worse. Based on current data for perioperative outcomes, it appears that MIS approaches are superior to open approaches in TLIF.
Currently, there exists a wide variation in reported perioperative outcomes in both open and MIS lumbar spine surgery in the literature. Although multiple different outcomes are being reported there exists a lack of defined criteria for many of the reported outcomes such as hospital LOS, postoperative narcotic utilization and need for perioperative transfusion. Furthermore, none of the currently published literature used independent observers when reporting outcomes such as EBL and neurologic complication, leading to the risk of complication under-reporting due to the self-reporting nature of the outcomes data collection.
The current evidence does not clearly support superior perioperative outcomes for patients receiving minimally invasive spine surgery across all modalities. Based on perioperative outcomes data, we recommend a MIS approach to TLIF surgeries. MIS and open approaches can be chosen based on patient and surgeon preference when performing a laminectomy. Regarding lateral approach surgeries, there is insufficient evidence to find non-inferior perioperative outcomes at this time.
The advents of the surgical microscope and advances in technology have led to an increase in popularity in minimally invasive spine surgery. While prior studies have compared minimally invasive spine surgery to the traditional open spine surgery in terms of long-term outcomes, no study has compared the two techniques in terms of perioperative outcomes.
Outcomes research in spine surgery has become a very important and highly prioritized area of research with the primary focus of minimizing cost while maximizing outcome.
This is the first study evaluating perioperative outcomes, comparing minimally invasive approaches and techniques vs open surgery in the treatment of degenerative lumbar spine disease.
While minimally invasive spine surgery has shown to have similar long-term outcomes to open spine surgery, it is important to evaluate perioperative outcomes of minimally invasive techniques to the standard open surgery in order to fully determine the advantages or disadvantages of the new technology compared to the gold standard.
The authors present us a comprehensive systematic review regarding short term outcomes following minimally invasive lumbar spine surgery. This topic is of interest and of novelty.
P- Reviewer: Huang W, Jelinek F, Wang SJ S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 2. | Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997;3:301-307. |
| 3. | McAfee PC, Regan JJ, Geis WP, Fedder IL. Minimally invasive anterior retroperitoneal approach to the lumbar spine. Emphasis on the lateral BAK. Spine (Phila Pa 1976). 1998;23:1476-1484. [PubMed] |
| 4. | Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976). 2003;28:S26-S35. [PubMed] |
| 5. | Mummaneni PV, Rodts GE. The mini-open transforaminal lumbar interbody fusion. Neurosurgery. 2005;57:256-261; discussion 256-261. [PubMed] |
| 6. | Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006;6:435-443. [PubMed] |
| 7. | Chopko B, Caraway DL. MiDAS I (mild Decompression Alternative to Open Surgery): a preliminary report of a prospective, multi-center clinical study. Pain Physician. 2010;13:369-378. [PubMed] |
| 8. | Nellensteijn J, Ostelo R, Bartels R, Peul W, van Royen B, van Tulder M. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: a systematic review of the literature. Eur Spine J. 2010;19:181-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 139] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 9. | Goldstein CL, Macwan K, Sundararajan K, Rampersaud YR. Comparative outcomes of minimally invasive surgery for posterior lumbar fusion: a systematic review. Clin Orthop Relat Res. 2014;472:1727-1737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 105] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 10. | Jacobs WC, Arts MP, van Tulder MW, Rubinstein SM, van Middelkoop M, Ostelo RW, Verhagen AP, Koes BW, Peul WC. Surgical techniques for sciatica due to herniated disc, a systematic review. Eur Spine J. 2012;21:2232-2251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Kinoshita T, Ohki I, Roth KR, Amano K, Moriya H. Results of degenerative spondylolisthesis treated with posterior decompression alone via a new surgical approach. J Neurosurg. 2001;95:11-16. [PubMed] |
| 12. | Rodgers WB, Gerber EJ, Rodgers JA. Lumbar fusion in octogenarians: the promise of minimally invasive surgery. Spine (Phila Pa 1976). 2010;35:S355-S360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 13. | Rodgers WB, Gerber EJ, Patterson J. Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine (Phila Pa 1976). 2011;36:26-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 348] [Cited by in RCA: 328] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 14. | Cho DY, Lin HL, Lee WY, Lee HC. Split-spinous process laminotomy and discectomy for degenerative lumbar spinal stenosis: a preliminary report. J Neurosurg Spine. 2007;6:229-239. [PubMed] |
| 15. | Usman M, Ali M, Khanzada K, Ishaq M, Naeem-ul-Haq R, Ali M. Unilateral approach for bilateral decompression of lumbar spinal stenosis: a minimal invasive surgery. J Coll Physicians Surg Pak. 2013;23:852-856. [PubMed] |
| 16. | Watanabe K, Matsumoto M, Ikegami T, Nishiwaki Y, Tsuji T, Ishii K, Ogawa Y, Takaishi H, Nakamura M, Toyama Y. Reduced postoperative wound pain after lumbar spinous process-splitting laminectomy for lumbar canal stenosis: a randomized controlled study. J Neurosurg Spine. 2011;14:51-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 85] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 17. | Mobbs RJ, Li J, Sivabalan P, Raley D, Rao PJ. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine. 2014;21:179-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 187] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 18. | Rahman M, Summers LE, Richter B, Mimran RI, Jacob RP. Comparison of techniques for decompressive lumbar laminectomy: the minimally invasive versus the „classic“ open approach. Minim Invasive Neurosurg. 2008;51:100-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 135] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 19. | Nomura H, Yanagisawa Y, Arima J, Oga M. Clinical outcome of microscopic lumbar spinous process-splitting laminectomy: clinical article. J Neurosurg Spine. 2014;21:187-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Parikh K, Tomasino A, Knopman J. Operative results and learning curve: microscope-assisted tubular microsurgery for 1- and 2-level discectomies and laminectomies. Neurosurg Focus. 2008;25:E14. [RCA] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Komp M, Hahn P, Merk H, Godolias G, Ruetten S. Bilateral operation of lumbar degenerative central spinal stenosis in full-endoscopic interlaminar technique with unilateral approach: prospective 2-year results of 74 patients. J Spinal Disord Tech. 2011;24:281-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 22. | Nomura K, Yoshida M. Microendoscopic Decompression Surgery for Lumbar Spinal Canal Stenosis via the Paramedian Approach: Preliminary Results. Global Spine J. 2012;2:87-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Tomasino A, Parikh K, Steinberger J, Knopman J, Boockvar J, Härtl R. Tubular microsurgery for lumbar discectomies and laminectomies in obese patients: operative results and outcome. Spine (Phila Pa 1976). 2009;34:E664-E672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Wada K, Sairyo K, Sakai T, Yasui N. Minimally invasive endoscopic bilateral decompression with a unilateral approach (endo-BiDUA) for elderly patients with lumbar spinal canal stenosis. Minim Invasive Neurosurg. 2010;53:65-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Pimenta L, Oliveira L, Schaffa T, Coutinho E, Marchi L. Lumbar total disc replacement from an extreme lateral approach: clinical experience with a minimum of 2 years’ follow-up. J Neurosurg Spine. 2011;14:38-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 26. | Lee YS, Park SW, Kim YB. Direct lateral lumbar interbody fusion: clinical and radiological outcomes. J Korean Neurosurg Soc. 2014;55:248-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Hrabalek L, Adamus M, Gryga A, Wanek T, Tucek P. A comparison of complication rate between anterior and lateral approaches to the lumbar spine. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158:127-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Smith WD, Christian G, Serrano S, Malone KT. A comparison of perioperative charges and outcome between open and mini-open approaches for anterior lumbar discectomy and fusion. J Clin Neurosci. 2012;19:673-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 29. | Huang TJ, Weng YJ, Li YY, Cheng CC, Hsu RW. Actin-free Gc-globulin after minimal access and conventional anterior lumbar surgery. J Surg Res. 2010;164:105-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Ruetten S, Komp M, Godolias G. An extreme lateral access for the surgery of lumbar disc herniations inside the spinal canal using the full-endoscopic uniportal transforaminal approach-technique and prospective results of 463 patients. Spine (Phila Pa 1976). 2005;30:2570-2578. [PubMed] |
| 31. | Lykissas MG, Aichmair A, Sama AA, Hughes AP, Lebl DR, Cammisa FP, Girardi FP. Nerve injury and recovery after lateral lumbar interbody fusion with and without bone morphogenetic protein-2 augmentation: a cohort-controlled study. Spine J. 2014;14:217-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Grimm BD, Leas DP, Poletti SC, Johnson DR 2nd. Postoperative Complications Within the First Year After Extreme Lateral Interbody Fusion: Experience of the First 108 Patients. J Spinal Disord Tech. 2014;Epub ahead of print. [PubMed] |
| 33. | Tohmeh AG, Rodgers WB, Peterson MD. Dynamically evoked, discrete-threshold electromyography in the extreme lateral interbody fusion approach. J Neurosurg Spine. 2011;14:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 137] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 34. | Berjano P, Balsano M, Buric J, Petruzzi M, Lamartina C. Direct lateral access lumbar and thoracolumbar fusion: preliminary results. Eur Spine J. 2012;21 Suppl 1:S37-S42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 35. | Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Stand-alone lateral interbody fusion for the treatment of low-grade degenerative spondylolisthesis. ScientificWorldJournal. 2012;2012:456346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 122] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 36. | Sharma AK, Kepler CK, Girardi FP, Cammisa FP, Huang RC, Sama AA. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech. 2011;24:242-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 172] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 37. | Ahmadian A, Verma S, Mundis GM, Oskouian RJ, Smith DA, Uribe JS. Minimally invasive lateral retroperitoneal transpsoas interbody fusion for L4-5 spondylolisthesis: clinical outcomes. J Neurosurg Spine. 2013;19:314-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 38. | Caputo AM, Michael KW, Chapman TM, Massey GM, Howes CR, Isaacs RE, Brown CR. Clinical outcomes of extreme lateral interbody fusion in the treatment of adult degenerative scoliosis. ScientificWorldJournal. 2012;2012:680643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 39. | Malham GM, Ellis NJ, Parker RM, Seex KA. Clinical outcome and fusion rates after the first 30 extreme lateral interbody fusions. ScientificWorldJournal. 2012;2012:246989. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 95] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 40. | Pimenta L, Marchi L, Oliveira L, Coutinho E, Amaral R. A prospective, randomized, controlled trial comparing radiographic and clinical outcomes between stand-alone lateral interbody lumbar fusion with either silicate calcium phosphate or rh-BMP2. J Neurol Surg A Cent Eur Neurosurg. 2013;74:343-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 41. | Elowitz EH, Yanni DS, Chwajol M, Starke RM, Perin NI. Evaluation of indirect decompression of the lumbar spinal canal following minimally invasive lateral transpsoas interbody fusion: radiographic and outcome analysis. Minim Invasive Neurosurg. 2011;54:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 119] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 42. | Oliveira L, Marchi L, Coutinho E, Pimenta L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976). 2010;35:S331-S337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 320] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 43. | Wang HL, Lü FZ, Jiang JY, Ma X, Xia XL, Wang LX. Minimally invasive lumbar interbody fusion via MAST Quadrant retractor versus open surgery: a prospective randomized clinical trial. Chin Med J (Engl). 2011;124:3868-3874. [PubMed] |
| 44. | Shunwu F, Xing Z, Fengdong Z, Xiangqian F. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976). 2010;35:1615-1620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 192] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 45. | Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Minimally invasive or open transforaminal lumbar interbody fusion as revision surgery for patients previously treated by open discectomy and decompression of the lumbar spine. Eur Spine J. 2011;20:623-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 46. | Wong AP, Smith ZA, Stadler JA, Hu XY, Yan JZ, Li XF, Lee JH, Khoo LT. Minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): surgical technique, long-term 4-year prospective outcomes, and complications compared with an open TLIF cohort. Neurosurg Clin N Am. 2014;25:279-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 105] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 47. | Zhang W, Duan L, Shang X, Xu X, Hu Y, He R. [Effectiveness of minimally invasive transforaminal lumbar interbody fusion assisted with microscope in treatment of lumbar degenerative disease]. Zhongguo Xiufu Chongjian Waike Zazhi. 2013;27:268-273. [PubMed] |
| 48. | Villavicencio AT, Burneikiene S, Roeca CM, Nelson EL, Mason A. Minimally invasive versus open transforaminal lumbar interbody fusion. Surg Neurol Int. 2010;1:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 120] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 49. | Lee KH, Yue WM, Yeo W, Soeharno H, Tan SB. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2012;21:2265-2270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 201] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 50. | Terman SW, Yee TJ, Lau D, Khan AA, La Marca F, Park P. Minimally invasive versus open transforaminal lumbar interbody fusion: comparison of clinical outcomes among obese patients. J Neurosurg Spine. 2014;20:644-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 51. | Cheng JS, Park P, Le H, Reisner L, Chou D, Mummaneni PV. Short-term and long-term outcomes of minimally invasive and open transforaminal lumbar interbody fusions: is there a difference? Neurosurg Focus. 2013;35:E6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 52. | Liang B, Yin G, Zhao J, Li N, Hu Z. [Surgical treatment of degenerative lumbar instability by minimally invasive transforaminal lumbar interbody fusion]. Zhongguo Xiufu Chongjian Waike Zazhi. 2011;25:1449-1454. [PubMed] |
| 53. | Yang J, Kong Q, Song Y, Liu H, Zeng J. [Comparison of short-term effectiveness between minimally invasive surgery- and open-transforaminal lumbar interbody fusion for single-level lumbar degenerative disease]. Zhongguo Xiufu Chongjian Waike Zazhi. 2013;27:262-267. [PubMed] |
| 54. | Gu G, Zhang H, Fan G, He S, Cai X, Shen X, Guan X, Zhou X. Comparison of minimally invasive versus open transforaminal lumbar interbody fusion in two-level degenerative lumbar disease. Int Orthop. 2014;38:817-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 55. | Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J. 2010;19:1780-1784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 194] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 56. | Zairi F, Arikat A, Allaoui M, Assaker R. Transforaminal lumbar interbody fusion: comparison between open and mini-open approaches with two years follow-up. J Neurol Surg A Cent Eur Neurosurg. 2013;74:131-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 57. | Seng C, Siddiqui MA, Wong KP, Zhang K, Yeo W, Tan SB, Yue WM. Five-year outcomes of minimally invasive versus open transforaminal lumbar interbody fusion: a matched-pair comparison study. Spine (Phila Pa 1976). 2013;38:2049-2055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 172] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 58. | Pelton MA, Phillips FM, Singh K. A comparison of perioperative costs and outcomes in patients with and without workers’ compensation claims treated with minimally invasive or open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976). 2012;37:1914-1919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 59. | Singh K, Nandyala SV, Marquez-Lara A, Fineberg SJ, Oglesby M, Pelton MA, Andersson GB, Isayeva D, Jegier BJ, Phillips FM. A perioperative cost analysis comparing single-level minimally invasive and open transforaminal lumbar interbody fusion. Spine J. 2014;14:1694-1701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 107] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 60. | Brodano GB, Martikos K, Lolli F, Gasbarrini A, Cioni A, Bandiera S, Di Silvestre M, Boriani S, Greggi T. Transforaminal Lumbar Interbody Fusion in Degenerative Disc Disease and Spondylolisthesis Grade I: Minimally Invasive Versus Open Surgery. J Spinal Disord Tech. 2013;Epub ahead of print. [PubMed] |
| 61. | Zou S, Wang J, Pan W, Zheng Y, Huang B. [Comparison of traumatic related index in serum between minimally invasive and open transforaminal lumbar interbody fusion for tissue injury]. Zhongguo Xiufu Chongjian Waike Zazhi. 2013;27:960-964. [PubMed] |
| 62. | Peng CW, Yue WM, Poh SY, Yeo W, Tan SB. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976). 2009;34:1385-1389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 324] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 63. | Archavlis E, Carvi y Nievas M. Comparison of minimally invasive fusion and instrumentation versus open surgery for severe stenotic spondylolisthesis with high-grade facet joint osteoarthritis. Eur Spine J. 2013;22:1731-1740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 64. | Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine. 2008;9:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 252] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 65. | Schizas C, Tzinieris N, Tsiridis E, Kosmopoulos V. Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop. 2009;33:1683-1688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 183] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 66. | Adogwa O, Parker SL, Bydon A, Cheng J, McGirt MJ. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech. 2011;24:479-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 156] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 67. | Niesche M, Juratli TA, Sitoci KH, Neidel J, Daubner D, Schackert G, Leimert M. Percutaneous pedicle screw and rod fixation with TLIF in a series of 14 patients with recurrent lumbar disc herniation. Clin Neurol Neurosurg. 2014;124:25-31. [PubMed] |
| 68. | Lau D, Lee JG, Han SJ. Complications and perioperative factors associated with learning the technique of minimally invasive transforaminal lumbar interbody fusion (TLIF). J Clin Neurosci. 2011;18:624-627. [RCA] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 69. | Gologorsky Y, Skovrlj B, Steinberger J, Moore M, Arginteanu M, Moore F, Steinberger A. Increased incidence of pseudarthrosis after unilateral instrumented transforaminal lumbar interbody fusion in patients with lumbar spondylosis: Clinical article. J Neurosurg Spine. 2014;21:601-607. [PubMed] |