Published online Dec 18, 2015. doi: 10.5312/wjo.v6.i11.850
Peer-review started: June 1, 2015
First decision: July 10, 2015
Revised: September 4, 2015
Accepted: October 1, 2015
Article in press: October 8, 2015
Published online: December 18, 2015
Processing time: 203 Days and 11.4 Hours
Fractures in sport are a specialised cohort of fracture injuries, occurring in a high functioning population, in which the goals are rapid restoration of function and return to play with the minimal symptom profile possible. While the general principles of fracture management, namely accurate fracture reduction, appropriate immobilisation and timely rehabilitation, guide the treatment of these injuries, management of fractures in athletic populations can differ significantly from those in the general population, due to the need to facilitate a rapid return to high demand activities. However, despite fractures comprising up to 10% of all of sporting injuries, dedicated research into the management and outcome of sport-related fractures is limited. In order to assess the optimal methods of treating such injuries, and so allow optimisation of their outcome, the evidence for the management of each specific sport-related fracture type requires assessment and analysis. We present and review the current evidence directing management of fractures in athletes with an aim to promote valid innovative methods and optimise the outcome of such injuries. From this, key recommendations are provided for the management of the common fracture types seen in the athlete. Six case reports are also presented to illustrate the management planning and application of sport-focussed fracture management in the clinical setting.
Core tip: This is an editorial article, on the topic of optimising the management and outcome of sport-related fractures, providing an informed commentary on the current management of acute fractures in the athlete with an aim to try optimise their outcome. The article begins with a brief overview of the topic, which is followed by a discussion on the management strategies and associated outcomes of the common fracture patterns seen in sporting populations. The published evidence relevant to this is also discussed. The authors then present a series of case reports to illustrate the management of such injuries in the clinical setting.
- Citation: Robertson GA, Wood AM. Fractures in sport: Optimising their management and outcome. World J Orthop 2015; 6(11): 850-863
- URL: https://www.wjgnet.com/2218-5836/full/v6/i11/850.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i11.850
Sports injuries are a major source of morbidity for the athlete[1]. The time required for treatment and recovery can have substantial financial implications both for the individual and for their team[1]. Given the economic revenues associated with professional sport, there has been a major focus in recent years to minimise the impact of sporting injuries, through optimisation of management, acceleration of rehabilitation and promotion of injury prevention[2-4]. Such initiatives have largely focused on acute soft tissue injuries and overuse injuries, such as ligament ruptures and stress fractures, that are commonly associated with sports medicine[2-4]. Little attention, however, has been placed on the management and outcome of acute fractures[5].
Acute fractures comprise 5% to 10% of all sports injuries and account for one of the longest return times to sport post-injury[3,6-16]. Until recently, much of the previous fracture research had focussed on osteoporotic fractures, overlooking cohorts of sporting individuals[17,18]. While fracture management in both cohorts adheres to the general principles of orthopaedic trauma with accurate fracture reduction, appropriate immobilisation and timely rehabilitation, management of fractures in athletes provides a unique challenge, due to the requirement to return to high impact activities as rapidly as able with the optimal symptom profile possible[1,5,18]. Thus in order to properly to assess the optimal management techniques for these injuries, and so maximise their outcome, dedicated research has to be performed focussing specifically on these individual cohorts[5,19-21].
In this editorial we analyse the evidence available for the management of acute sport-related fractures, and discuss the developing methods suggested to optimise management and outcome of these injuries. We will focus on the common fracture locations and types experienced by the athlete[5,22], and, for each of these, we will discuss the standard management of these injuries as well as review the innovative treatment strategies currently being developed to optimise outcomes in the high level athlete. This will be supplemented by a series of case reports which will illustrate the application of these strategies in clinical practice. The topic of sport-related stress fractures is not covered in this editorial as this has been covered previously in various reviews.
When planning the management of acute sport-related fractures, the standard principles of orthopaedic trauma management should always form the basis of decision-making[18]. These are to achieve anatomical fracture reduction, to apply adequate fracture immobilisation, and to perform timely rehabilitation to facilitate the return of normal physiological functioning[18]. However, with fractures in the athlete, particularly high level athletes, there is a requirement to achieve rapid return to high demand activities with lowest symptom profile, in order to restore sporting careers[1,5,18]. As such, specific modifications can be made when treating these injuries to achieve this[1,5,18].
However, it is difficult to provide a unifying set of principles to guide the management of sports-related fractures, as fracture management is often unique to fracture location and fracture pattern[18,19]. And so, in order to establish the optimal modality for treating these injuries, each fracture type has to be assessed individually, with the relevant evidence assessed for each. The four major questions that require defining for each fracture type are: (1) Should management be operative or conservative? (2) Which method of surgical fixation is best to use? (3) Which method of immobilisation is best to use? and (4) How quickly can sporting activities be resumed?
In order to achieve this, we will assess the five most common fracture types for both the upper and lower limb[5,22], and discuss the developing management initiatives that aim to optimise outcome of these injuries in the high level athlete.
Upper limb fractures comprise three quarter of all sports-related fractures, with the five most common types being finger phalanx, distal radius, metacarpal, clavicle and scaphoid[5,22]. In general, around ten percent of upper limb sport-related fractures are treated operatively[20,21]. Both return rates and return times are promising, with rates ranging between 85% and 87% and return times averaging around 9 wk[20,21].
As a whole, the management of finger phalanx fractures varies little between athletic populations and the general population[18,23-25]. The majority of such fractures are undisplaced or minimally displaced and can be treated satisfactorily with an appropriately designed splint for 2 to 3 wk[18,23-27]. For the high level athlete, the exception to this rule is the undisplaced condylar fracture, which has a high rate of displacement in active individuals[24]. Weiss et al[28] noted a displacement rate of 72% with non-operative management of such fractures. As such these often benefit from primary surgical fixation in the athletic population[23,24].
Stable displaced extra-articular fractures are often amendable to conservative management with closed reduction and splinting[18,23-25]. However, displaced intra-articular fractures, displaced proximal base fractures and displaced unstable extra-articular fractures often require surgical stabilisation[18,23-25]. While closed reduction and K-wiring is routinely chosen for stabilisation of such fractures in the general population, there is a developing consensus that internal fixation should be employed in the high level athlete, with interfragmentary screw or plate fixation, as this can facilitate an accelerated return to sporting activity[23-25]. Such decisions can be complex and management is best directed by a specialist hand surgeon with experience in such injuries[23-25].
Methods of immobilisation remain similar to the standard techniques, with Alumafoam, thermoplast, or “finger tip” protectors, regularly employed[23-25]. The challenge with the athlete is designing an orthotic that can allow early return to sport. This is often best achieved in conjunction with a specialist orthotist and should be guided by the rules of the sport, as well as the function of the athlete[23-25].
Regarding the best time to return to sport, guidelines suggest that return within the first week post-injury should be possible with adequate orthotic protection[23-25]. However return to full contact sport should be withheld till there is evidence of radiographic healing, normally around 3 wk, with continued used of protective splinting till 6 wk post fracture[23-25].
Around ninety percent of sport-related distal radius fractures are treated conservatively, being either undisplaced fractures or dorsally displaced extra-articular fractures that can be reduced and splinted into satisfactory anatomical alignment[5,20-22,27,29]. However, for the high level athlete, it is becoming increasingly accepted that such fractures with evidence of radiological instability, such as dorsal comminution, dorsal angulation > 20 degrees, articular radiocarpal fracture, ulnar fracture, and loss of radial length, are best treated with primary surgical intervention, to avoid unsuccessful attempts at conservative management, which delay return to sport[30-32].
Regarding the choice of surgical fixation, the majority of fractures can be adequately managed with locked volar plating[30]. However, clinicians must remain aware of the importance of achieving accurate anatomical reduction in the high level athlete, and occasionally, this is not possible with volar plating alone, particularly with comminuted and intra-articular fractures[30]. Additional plating or bridging external fixation with K-Wire augmentation may be required to provide more accurate reduction[30]. Such decisions should be directed by specialists with experience in the management of sport related distal radial fractures[30].
Immobilisation techniques vary little from standard practice, with a short arm “colles” cast for conservative management and a wrist splint for post-surgical immobilisation[18,30]. Regarding return to sport, it is clear that non-contact, “non-upper-limb” activities can be commenced within 2 to 4 wk of injury with the fracture appropriately immobilised[18,30]. However, both with operative and conservative cases, return to full contact sport should not be performed until there is satisfactory fracture healing, normally around 8 wk post-injury[18,30].
The majority of sport-related metacarpal fracture are undisplaced or minimally displaced and will not require surgery[5,20-22,26,27,33]. These can be treated satisfactorily with an appropriately designed splint and associated buddy strapping[18,24,25,34,35]. For the high level athlete, the exception to this rule is the undisplaced intra-articular metacarpal head fracture and the undisplaced intra-articular thumb metacarpal base fracture, which are unstable, and require primary surgical fixation[18,24,25,34,35].
Most displaced extra-articular fractures can be managed conservatively, with reduction and splinting into satisfactory alignment[18,24,25,34,35]. However, displaced intra-articular fractures and displaced unstable extra-articular fractures often require surgical stabilisation[18,24,25,34,35]. Internal fixation with either interfragmentary screws or plating is the preferred modality in the high level athlete, facilitating an earlier return to rehabilitation and sport[24,25,34]. Rettig et al[33] found that internal fixation of metacarpal fractures resulted in a return time to sport of 14 d while management with closed and K-wiring resulted in a return time of 36 d to sport. When closed reduction and K-wiring is required, K-wires can be cut under the skin and buried to facilitate an accelerated return to sport[35].
A variety of immobilisation methods continue to be used, ranging from short arm “colles” casts to gutter splints, with neither more beneficial than the other[18,24,25,34,35]. The challenge with the athlete, is designing a suitable orthotic that can permit adequate function with appropriate protection on return to sport[24,25,34,35]. This is often best achieved in conjunction with a specialist orthotist and should be guided by the rules of the athlete’s sport, as well as the position of the athlete[24,25,34,35].
Guidelines at present advise return to non-contact, “non-upper-limb” sporting activities within 1 wk post-injury and return to full contact sports within 4 wk post-injury[24,25,34-36]. However, recent studies have suggested that an accelerated return to full contact sport can be achieved with one week of injury[36]. While the authors advise against this, due to the possibility of re-injury, if clinicians decide to attempt this, patients should be thoroughly counselled regarding the risk of re-fracture and strongly advised to maintain protective splinting throughout.
Up to 20% of sport-related clavicle fractures undergo primary surgical intervention[20,21], compared to around 5% in the general population[37]. This is due to the differing management of displaced mid-diaphyseal clavicular fractures for the two populations[38-41]. While displaced mid diaphyseal fractures are regularly managed conservatively in the general population, with acceptable union rates and functional results[37,42], recent research has promoted surgical fixation of such injuries in athletes (particularly contact athletes) when there is complete displacement, shortening greater than 2 cm or comminution[38-41,43,44]. This is directed by the research from the Canadian Orthopaedic Trauma Association[43] and McKee et al[45] who found that operative management of such fractures provides significantly improved shoulder function, symptom profile and union rates in active individuals. Further studies in high level athletes have found that conservative management of such injuries can result in return times of up to two seasons, with refracture rates of over 50%[40], while surgical management results in return times between 68 d and 83 d with no episodes of refracture[39-41]. Nevertheless, given that conservative management remains an acceptable alternative, avoiding the substantial surgical risks, clinicians should involve all patients in a well-informed discussion regarding both sets of management, before proceeding with surgical intervention[18].
Regarding the optimal method of surgical fixation, several studies have found similar return rates and return times to sport for both plate fixation (rates 98% to 100%; times 45 d to 36 wk)[39-41,46,47] and intramedullary nailing (rates 98% to 100%; times 17 d to 3.2 mo)[40,48-50]. However, clinicians should remain aware that the optimal method of fixation is dependent on the location and the nature of the fracture pattern[18,50]. Simple, transverse and oblique, two part mid-diaphyseal fractures are suitable for either form of fixation[18,50], and in such instances, the authors advise that clinicians should use the technique that they are experienced with and feel comfortable performing[40]. Complex comminuted mid-diaphyseal fractures and distal clavicle fractures, however, are not suitable for intra-medullary nailing, with recorded difficulties in achieving and securing accurate reduction[18,46,50]. In such instances, clinicians should employ open reduction internal fixation[18,46,50].
There is little variation for immobilisation techniques in the athlete compared to those of standard practice[18,51,52]. Use of a sling is appropriate for both conservatively and surgically managed fractures, with no clear advantage being shown between this and figure of eight immobilisation[18,51,52].
Return to sport is an important issue with such fractures, due to the risk of refracture[40]. The authors advise that non-contact, “non-upper-limb” activities be commenced within 1 to 2 wk post-injury, for both operative and non-operative cases[18,51,52]. However commencement of contact and “upper-limb” sports should not be commenced till around 8 wk post-injury, with clear evidence of radiographic and clinical healing[18,51,52]. For, the rare cases of conservatively managed displaced mid-diaphyseal fracture, such times may extend to 16 wk[40].
Up to 25% of sport-related scaphoid fractures are treated surgically[21], while only around 5% of those in general population undergo primary surgical intervention[53]. This is because evidence-based recommendations advise primary surgical intervention of undisplaced and minimally displaced waist fractures in the athlete, while such injuries are routinely managed conservatively in the general population[18,54]. Level 1 Evidence from McQueen et al[55] found that primary surgical management of undisplaced scaphoid waist fractures with a percutaneous headless screw results in return times to sport of 6.4 wk while conservative management of such injuries resulted in return times of 15.5 wk. Nevertheless, as conservative management remains an acceptable alternative, the authors advise that clinicians involve patients in a well-informed discussion regarding both sets of management, before proceeding with surgical intervention[18].
Regarding the optimal surgical modality, the Herbert Headless Compression Screw is the most validated method available[54,56,57]. This can be performed percutaneously for minimally displaced fractures, leaving a minimal scar with limited post-operative symptoms, allowing the athlete to return to unimpaired upper limb activities as quickly as possible[54,55].
One of the major benefits of undergoing primary surgical intervention in the athlete, is that no formal post-operative immobilisation is required, allowing rapid commencement of physiotherapy and return to sports[54,55]. Conservative management requires use of a short arm “colles” cast for 8 to 12 wk, delaying commencement of physiotherapy and subsequent return to sport[54-56]. The addition of thumb extension to “colles” casting appears to offer limit benefit in term of time to union and post-treatment function, and so is no longer recommended[57].
Return to sport is clearly accelerated in those athletes who undergo surgical intervention due to the more rapid commencement of upper limb mobilisation exercises[54-56]. Non contact, “non-upper-limb” activities can be commenced within 1 to 2 wk, followed by a graduated return to contact activities, by around 6 to 8 wk post-surgery[54]. With conservative management, non contact activities can be commenced within 1 to 2 wk of injury, however contact sports should not be commenced until removal of cast with clear evidence of radiographic healing[54].
Lower limb fractures comprise one quarter of all sports-related fractures, with the five most common types being ankle, metatarsal, toe phalanx, tibial shaft and fibula[5,22]. Around forty percent of them are treated operatively[20,21]. Return rates are promising at around 86%, however return times can be prolonged, often averaging around 27 wk[20,21].
Until recently, it was recommended that all sport-related ankle fractures be treated surgically, to facilitate an early return to sport[58]. However, emerging evidence shows that surgical intervention is associated with increased rates of persisting symptoms, with similar or prolonged return times to sport compared to conservative management[19]. As such, current recommendations advise that stable undisplaced fractures (i.e., isolated Weber A lateral malleolus, isolated Weber B lateral malleolus and medial malleolus) be treated non-operatively[18,19]. Those that require surgical intervention include displaced unstable fractures (displaced bimalleolar and bimalleolar equivalent fractures), fractures with posterior malleolar fragments greater than a third the articular surface and fractures with sydesmotic disruption[18,19].
The area for debate is the management of undisplaced, radiologically unstable fractures (i.e., undisplaced bimalleolar fractures and undisplaced Weber C fractures), with some advocating primary surgical fixation to facilitate early return to sport and others advocating attempted conservative management to avoid the post-surgical symptom profile[18,19,58]. Robertson et al[19] found that conservative management of undisplaced bimalleolar fracture resulted in return times of 27 wk to sport while surgical management of displaced bimalleolar ankles resulted in return times of 43 wk. Seventy-one percent of the surgically managed patients reported persisting symptoms at follow-up compared to 17% of the conservatively managed patients[19]. As such, current recommendations advise attempted conservative management of these fracture types, with close follow-up and surgical intervention if displacement occurs[18,19].
Regarding the optimal surgical method, open reduction internal fixation with lag screw and tubular plate remains the standard modality[58]. Intra-medullary fixation is an evolving concept though the evidence for use in the athletic population is not available at present[59]. The decision to repair associated soft tissue structures remains debatable, particularly for the high level athlete[60]. Strömsöe et al[61] found that additional deltoid ligament repair resulted in no improvement to sporting function at a mean of 17 mo post-surgery. It is recommended that associated ligament repair only be performed if these structures block intra-operative fracture reduction[18,19,61]. There remains debate over the optimal method of syndemotic stabilisation, with current evidence suggesting that tightrope fixation provides superior results over screw fixation in terms of ankle function, time to return to activities and need for further intervention[60,62]. While it is recommended for use in the elite athlete, long term follow-up of tightrope fixation is limited[57,59]. As such, use of this specialist technique should be restricted to surgeons who are experienced with this procedure[57,59]. For those that undergo screw fixation, there is no functional benefit in screw removal, so this is only recommended if there are adverse symptoms arising from it[63].
Immobilisation of ankle fractures in the elite athlete is now more commonly performed with a moon boot orthosis as this allows for regular removal and earlier commencement of physiotherapy[18]. With stable fractures, weight bearing should be encouraged as early as possible to reduce muscle wastage and deconditioning[18,19]. Times for immobilisation are as per standard ankle fracture management, and should be adhered to properly, to allow for optimal fracture healing before recommencement of sporting activities, limiting the chance of repeat injury[18,19].
Regarding return to sport, the authors recommend commencement of non-contact sporting activities between 6 to 8 wk post-injury, with progression of exercise intensity under the care of the physiotherapists[18,19]. Return to contact sporting activities can then normally be performed around 12 to 16 wk post-injury, though should be guided by radiological evidence of healing[18,19]. The exception to this are those who undergo syndesmotic fixation: in such cases weightbearing should not be commenced till 8 wk post-surgery, so full return to sporting activities is often delayed up to and beyond 20 wk[18,19].
The key difference between the management of metatarsal fractures in the athletic population compared to that in the general population is that, in the elite athlete, primary surgical intervention is recommended for the acute undisplaced or minimally displaced 5th metatarsal proximal meta-diaphyseal (Jones) fracture[18,64]. Level 1 evidence from Mologne et al[65] has found that primary surgical intervention of these injuries resulted in improved return times to sport (surgical 8 wk vs conservative 15 wk), improved rates of union (surgical 95% vs conservative 67%) and improved times to union (surgical 7.5 wk vs conservative 14.5 wk). This has subsequently been confirmed by a systematic review assessing eighteen studies on this subject[64]. Given that conservative management remains an acceptable alternative, the athlete should be thoroughly counselled on the treatment options, detailing both the risks of non-union with conservative management and the risks of infection and nerve damage with surgical management[18,64]. If conservative management is initially attempted, this can be converted to surgical management if a delayed union becomes apparent, normally within two to four months of the initial injury[64,66-68]. This can improve return times to sport in such circumstances[64,66-68].
The preferred surgical technique for the Jones fracture is the intramedullary screw, having the strongest evidence base of all the available methods[18,64]. Reported return to sport times range between 7.5 wk and 12.4 wk and return rates range between 88% to 100%[65,67,69-75]. While there is no evidence-base to recommend a percutaneous technique over an open technique, a percutaneous technique leaves the athlete with a smaller scar which theoretically should reduce the post-operative symptom profile[64].
Immobilisation is an important factor in achieving healing with the Jones fracture, and appropriate adherence to recommended rehabilitation protocols is key to improve the success of both operative and non-operative management[67]. Post-operative immobilisation can be performed with a moon boot to facilitate early range of motion exercises, though conservative management may best be performed in a below knee cast, at least initially, to limit return to activities and allow for optimal fracture healing[18,67,72-74]. Post-operatively, current recommendations advise return to weightbearing 2 wk post-surgery, with commencement of physiotherapy and graduated return to activities by 6 to 8 wk post-surgery[18,67,72-74]. Athletes must be advised not to over accelerate rehabilitation as this significantly increases the chances of treatment failure[67]. For conservative management, immobilisation is required for up to 12 wk, non weightbearing for 6 wk and partial weightbearing for 6 wk[65,75,76]. Compliance is vital, particularly in the restless athlete, as failure to adhere with this results in a high rate of non-union[18,67].
Regarding return to sport for surgically managed Jones fractures, this can normally be achieved around 8 to 12 wk post-surgery, but again, it is important to avoid an over accelerated return as this can damage fixation, impair healing and result in non-union[18,67,72-74]. As such return should only be performed when there is clear evidence of clinical and radiological healing[67]. For conservatively managed Jones fractures, it is similarly important to avoid an over accelerated return, as this results in a high rate of delayed union and non-union[65,67,75,76]. Athletes can expect to wait till up to 16 wk post-injury till return to full level sport, and this again should not be performed till there is clear evidence of clinical and radiological healing[18,64]. For other metatarsal fractures, whether treated conservatively or surgically, these can normally return to sporting activities between 6 to 8 wk post-injury[18].
The majority of sport-related toe phalanx fractures are undisplaced or minimally displaced and so can be treated conservatively, with very satisfactory results[18,21,77]. However, those with gross displacement or significant articular involvement will normally require surgical intervention[18,21,77].
There is little evidence to direct the optimal surgical modality, though, with high level athletes, internal fixation with interfragmentary screw fixation or plate fixation is recommended over closed reduction and K-wiring, as this can facilitate a more rapid return to sporting activities[77].
Immobilisation is best performed with buddy strapping and a forefoot offloading shoe, as this allows the athlete to continue weightbearing during the immobilisation period[18,77]. This is normally for a period of 3 to 4 wk, followed by a graduated return to activities under the care of the physiotherapists[18,77].
Regarding return to sport, while it can tempting for the high level athlete to pursue an accelerated resumption of activities, given the perceived insignificance of such injuries, clinicians must limit return times to a minimum of 4 wk, for both conservative and surgical management, to allow the fracture to heal sufficiently[18,77]. This prevents the risk of re-injury and development of deformity or longstanding pain complications[18,77].
The key difference between the management of tibial shaft fractures in the athletic population compared the general population is that, in the elite athlete, primary surgical intervention is recommended for undisplaced and minimally displaced tibial shaft fractures[18,78]. While such injuries have traditionally been treated non-operatively, with an above knee cast followed by a patellar tendon bearing cast, a recent systematic review has found that, in athletic populations, primary surgical fixation results in improved return rates to sport (surgical 92% vs conservative 67%). with improved return times to sport (surgical 12 to 54 wk vs conservative 28 to 182 wk)[18,78]. Given that conservative management remains an acceptable alternative, avoiding the considerable risks associated with surgery, such decisions require an informed discussion with patient[18]. The risks of surgery should be detailed clearly, including infection, compartment syndrome and neurovascular injury, though patients should also be advised that up to one third of patients managed conservatively require delayed surgical intervention for fracture displacement[18,78-81]. The authors recommend primary surgical intervention for high and middle level athletes with undisplaced or minimally displaced tibial shaft fractures, and attempted conservative management for low level athletes with such injuries. For those managed conservatively, regular follow-up with radiographic review is required to assess for displacement, with appropriate surgical intervention offered accordingly, if this occurs[79-81].
The management of displaced fractures is similar between athletic and non-athletic populations with surgical intervention universally required[18,78]. To note, manipulation and casting of such fractures has been found to result in return times over 2 years, with re-intervention rates over 25%[79]. This is not recommended in the athlete[78].
Intra-medullary nailing remains the preferred technique in the athlete, with the strongest evidence base of all methods[21,82-88]. Return rates range between 70% to 100%[21,82,83,86,87] and return times between 12 to 54 wk[21,82-85,87,88]. Plate fixation often requires a period between 4 to 6 wk non-weightbearing post-operatively, and as such, demonstrates prolonged return times compared to IM nailing[79].
Recommended immobilisation techniques following IM Nailing include use of a moon boot orthotic weightbearing as tolerated for 4 to 6 wk, allowing for range of motion exercises throughout[18]. For conservative management, preferred immobilisation is with an above knee cast for 4 to 6 wk followed by a patellar tendon bearing cast for 4 to 6 wk, with weightbearing guided by radiological evidence of healing[18,79,80].
Rapid return to sport is a key issue with these fractures but it is important to perform this in a time-appropriate manner as over-accelerated return can risk failure of fixation and non-union[18]. Following intra-medullary nailing, progressive immobilisation under the care of the physiotherapist can begin immediately with return to gentle running activities between 6 to 12 wk[18,21,82-88]. Return to full contact sports can normally be performed by 24 wk[18,21,82-88]. There should be clear evidence of radiological union before this is permitted[18]. For conservative management, mobilisation under the care of the physiotherapist cannot be commenced till removal of cast, and as such return to sporting activities is often delayed due to muscle atrophy and deconditioning[18,79,80,89]. Running activities are usually not commenced till between 16 and 20 wk and return to full contact sport can often does occur till over 40 wk post-injury[18,79,80]. Particularly in these cases, this should not be resumed till there is clear evidence of radiological healing, due to a high risk of re-fracture on return to sports[18].
The management of sport-related fibula fractures varies little from that in the general population[18,20,21]. Virtually all these injuries are treated conservatively with favourable return times to sport and limited post-injury symptom profiles[20,21]. The main consideration with the management of these injuries in the high level athlete is to avoid over-accelerated return to full level sport before adequate healing has been achieved, as this may promote development of a non-union[18]. Despite the initial self-limiting nature of such fractures, development of a non-union often requires surgical intervention, which can significantly delay return to sport[18].
Immobilisation of such fractures in the athlete is often best performed with a moon boot weightbearing as tolerated as this allows ongoing physiotherapy exercise to be performed[18].
Regarding return to sport, this should be performed in a graduated fashion between 6 to 8 wk, guided by both radiological and clinical evidence of healing[18]. Clinicians should remain alert for the patient who develops persistent fracture pain on return to sport[18]. Appropriate reduction of activities advised with regular follow-up performed, to exclude the development of a non-union[18].
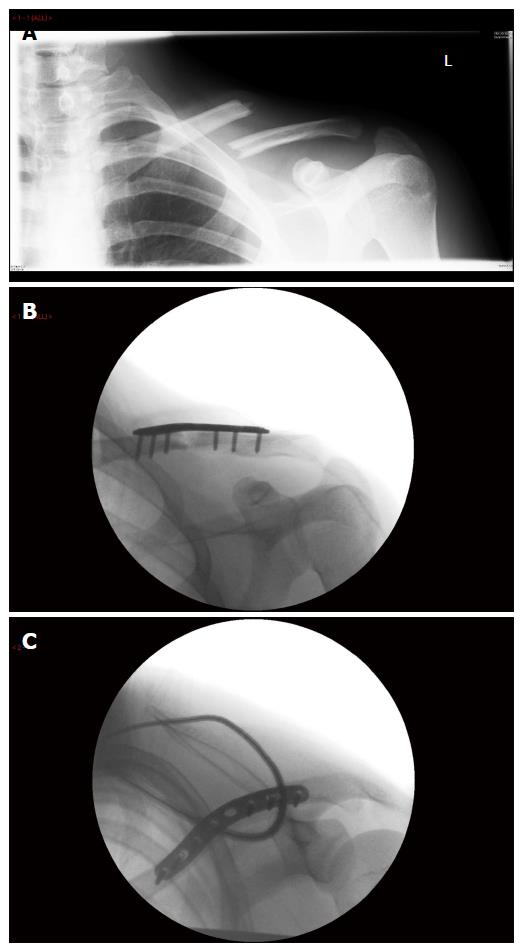
A 20-year-old semi-professional rugby player suffered a fall onto his left shoulder following a tackle during a match. He sustained a mid diaphyseal clavicluar fracture, that was completely displaced on radiographs and clinically shortened greater than 2 cm. It was closed and distally neuro-vascularly intact with no evidence of skin tenting.
Following an informed discussion in clinic, outlining the options of conservative vs surgical management, detailing both the associated risks and predicted outcomes of both treatments, with surgical intervention recommended, the patient opted for surgical management, with a view to be able to return to his sporting career as soon as able.
He underwent open reduction and plate fixation of his clavicle the two days later. There were no complications. Post-operatively, he was immobilised in a sling for 2 wk, then commenced physiotherapy at this stage.
He returned to non-contact training activities 8 wk post-operatively and returned to full level rugby 10 wk post-operatively. At 2-year follow-up, he is occasionally troubled by scar sensitivity, particularly when wearing a rucksack but otherwise reports no other symptoms.
Key message: Primary surgical fixation of displaced mid shaft clavicle fractures can facilitate early return to contact sports with good recovery of shoulder function.
A 24-year-old district level soccer player suffered a forced inversion injury to her left ankle during a tackle. She sustained an undisplaced right bimalleolar ankle fracture. This was closed and distally neuro-vascularly intact. She was placed into a below knee backslab on the day of her injury and this was then converted into a below knee cast one day later in fracture clinic. Radiographs confirmed no displacement of the fracture.
In clinic, her consultant detailed the options of conservative vs surgical management, describing both the associated risks and the predicted outcomes of both treatment, and recommending conservative management. She opted for conservative management with a preference to avoid surgery. She was kept crutch-assisted partial weightbearing in a below knee cast for 6 wk.
Radiographs at one, 2 and 6 wk demonstrated no displacement of the fracture, and the cast was removed at 6 wk. She commenced physiotherapy at this stage, with a progressive weightbearing programme.
She returned to training activities 14 wk post-injury and returned to full level soccer 20 wk post-injury. At 2-year follow-up, she reports no adverse symptoms.
Key message: Successful conservative management of undisplaced, radiologically unstable, ankle fractures can result in rapid return to sport with the avoidance of the surgical intervention and an improved outcome symptom profile.
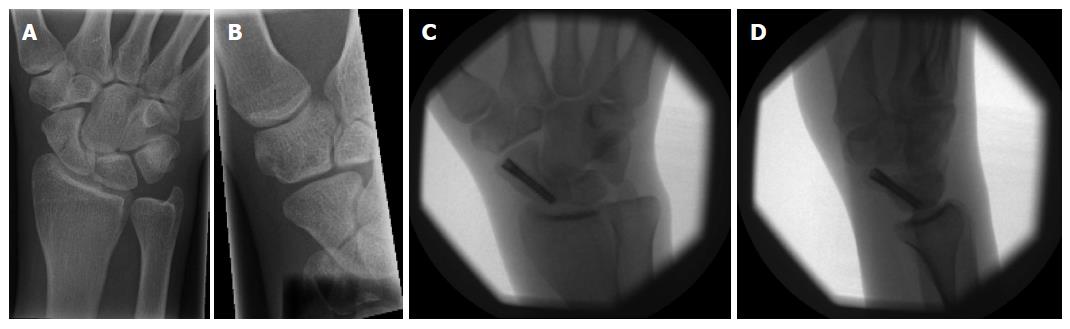
A 26-year-old right hand dominant professional cyclist suffered a fall from his bike during a race onto his right outstretched hand. He sustained an undisplaced scaphoid waist fracture. The injury was closed and distally neuro-vascularly intact.
Following extensive discussion in clinic, outlining the options of conservative vs surgical management, detailing the associated risks of treatment and the predicted outcomes, with surgical intervention recommended, the patient opted for surgical fixation, with the aim to be able to return to his sporting career as soon as able. He underwent retrograde percutaneous screw fixation of his scaphoid fracture three days later. There were no complications.
Post-operatively, he required no immobilisation and commenced physiotherapy within 1 wk of his surgery. He returned to non-contact, “non-upper limb” training activities 3 wk post-operatively and returned to cycling 7 wk post-operatively. At 2-year follow-up, he reports occasional pains around his scaphoid region following prolonged cycles, particularly in the cold, though is otherwise functionally well.
Key message: Primary surgical fixation of undisplaced scaphoid waist fractures can facilitate early return to upper limb sports with good recovery of wrist function.
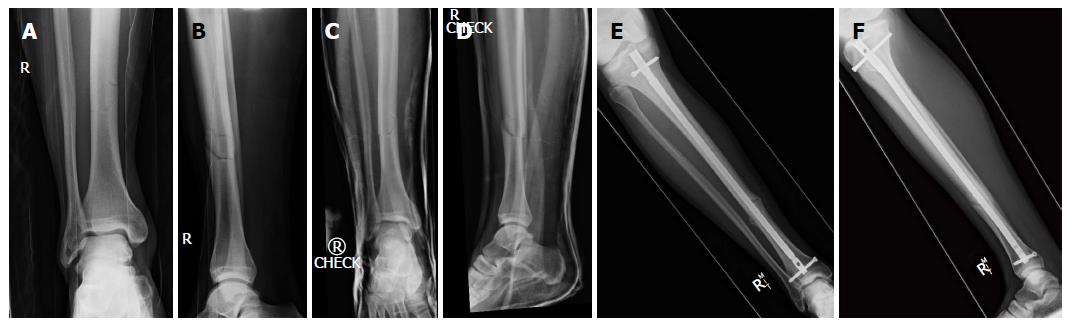
A 23-year-old professional soccer player suffered a twisting injury to his right lower leg, as his studs got caught in the turf, during a tackle. He sustained an undisplaced tibial shaft fracture, which was closed and distally neurovascularly intact. In the Emergency Department, he was placed into an above knee cast, and further radiographs demonstrated minimal fracture displacement with acceptable alignment to consider non-operative management. He was admitted as an inpatient to monitor for post-injury compartment syndrome.
On the ward round the following morning, there was an extensive discussion between the patient and his consultant, regarding the options of conservative vs surgical management. The risks associated with each form of treatment and the predicted outcomes from both were detailed clearly, with surgical intervention recommended. The patient opted for surgical intervention, with the aim to return to his sporting career as soon as able. He underwent intra-medually nailing of his tibia that day. There were no complications.
Post-operatively, he was weightbearing as tolerated in a moon boot and commenced physiotherapy day 1 post-surgery. He commenced training activities at 16 wk post-surgery and returned to full level soccer at 35 wk post-surgery. At 2-year follow-up, he reports mild anterior knee pain on prolonged kneeling but is otherwise functioning well.
Key message: Primary surgical fixation of undisplaced and minimally displaced tibial shaft fractures can facilitate early return to sport with good recovery of lower limb function.
A 27-year-old amateur level soccer player suffered a twisting injury to his left foot after turning rapidly to avoid a tackling opponent. He sustained a left 5th metatarsal Jones fracture, which was undisplaced on radiographs. The injury was closed and distally neurovascularly intact.
He was seen in fracture clinic the next day and following an extensive discussion, regarding the options of conservative vs surgical management, detailing the associated risks and predicted outcomes of both, with surgical intervention recommended, the patient chose to persist with conservative management, with an aim to avoid surgery. He was placed into a below knee cast and kept non-weightbearing with crutches for 6 wk. He was then converted to a moon boot orthotic, partial weightbearing with crutches for a further 6 wk.
At his 9 wk follow-up appointment, he reported having returned to gentle running activities and suffering a lot of pain from the fracture site during this. Radiographs at that time showed he was progressing to a delayed union. His consultant then explained the current status of his fracture, detailing the likelihood and timeframe to union with both surgical and conservative management, discussing the associated risks and predicted outcomes of each treatment method, and recommending surgical intervention. The patient then opted for surgical management with an aim to return to sport as soon as able with minimum persisting pain. He underwent percutaneous screw fixation of his fracture two days later. There were no complications.
Post-operatively, he was mobilised partial weightbearing with crutches in a moon boot for 2 wk, and then was progressed to full weightbearing over the next 4 wk under the care of the physiotherapists. Repeat radiographs at his 6 wk appointment confirmed progressive union of his fracture. He commenced training activities 8 wk post-surgery and returned to full level soccer 12 wk post-surgery. At his 2-year follow-up, he reports no symptoms from his fracture.
Key message: Primary surgical fixation of undisplaced fifth metatarsal Jones fractures can result in more rapid return to sport and improved union rates than conservative management. If delayed union develops with conservative management, operative intervention still remains a valid option to promote fracture union and facilitate an early return to sport.
A 26-year-old right hand dominant amateur team cyclist suffered a fall from his bike whilst racing, landing on an outstretched right hand. He sustained a right distal radius fracture that was dorsally displaced and angulated, with associated dorsal comminution. It was a closed injury and was distally neuro-vascularly intact. He underwent closed reduction and below elbow “colles” backslab application under “Bier’s Block” Regional Anaesthesia in the Emergency Department. Post-Manipulation radiographs confirmed satisfactory reduction of the fracture.
He was seen in Fracture Clinic the following day, where his consultant had an extensive discussion with him regarding the options of conservative vs surgical management, detailing the associated risks and the predicted outcomes for both, and recommending surgical intervention. The patient opted for conservative management with the desire to avoid surgery. He was then reviewed 1 and 2 wk post-injury, with radiographic follow-up and conversion to a below elbow “colles” cast at the 2 wk appointment. Check radiographs at that stage showed the fracture had lost reduction.
His consultant then explained the current status of his fracture, describing the predicted function and outcome with conservative management vs surgical management, detailing the associated risks and the predicted outcomes for both, and recommending surgical intervention. He opted for surgical management due to the concerns raised about his resultant hand and wrist function if he developed a malunion of the fracture. The following day he underwent operative fixation of the fracture. Intra-operatively, satisfactory reduction of the fracture was achieved with a volar locking plate alone, although a combined volar and dorsal approach was required, with intra-operative K-wire stabilisation of fracture fragments to achieve this. There were no intra-operative complications.
Post-operatively, he was kept in a futura wrist splint for 3 wk, mobilising as able, and commencing formal physiotherapy within the first post-operative week. He was advised to avoid heavy lifting for 6 wk post-surgery. He commenced non-contact “non-upper-limb” training activities at 4 wk post-surgery and returned to cycling at 10 wk post-surgery. At 2-year follow-up, he reports pain in the wrist during prolonged cycles, especially in the cold, though he does not wish to have further procedure to correct this. He reports no other symptoms or functional limitations.
Key message: Primary surgical fixation of radiologically unstable, undisplaced or reduced, distal radius fractures can avoid the likely risk of loss of fracture reduction seen with conservative management, and so facilitate early return to sport.
The optimal management of sport-related fractures is key in order to allow athletes to return to sport as quickly as able with the lowest side effect possible. The management principles for these injuries are largely comparable to those the general population; however there remains key examples where management between the athlete and general population differ[19,23-25,30,33-35,39-41,43,45,55,60,64,65,77,78]. It is vital for clinicians to be aware of such examples, and to appropriately inform both the athlete and the sports team of the available management options, as choice of the incorrect treatment can result in reduced return rates to sport and delayed return times to sport[19,23-25,30,33-35,39-41,43,45,55,60,64,65,77,78]. Given the importance of high level sport in modern society, both financially and socially, such decision can have significant consequences.
Ongoing research is required to assess for further optimisation of fracture management within athletic populations, to improve the return rates, return times and symptom profiles following these injuries. Clinicians should keep records of management of these injuries and publish findings accordingly. Similarly, well-organised prospective epidemiological studies should be performed to detect variations in management, and the influence this has on the outcomes following these injuries. Finally, future well-conducted randomised trials assessing the management of these injuries should be actively encouraged and funded, as these will form the key stone to establish the optimal treatment of sport-related fractures.
Despite an ongoing drive to optimise outcomes with these injuries, clinicians treating such athletes should always adhere to robust orthopaedic principles, and should never compromise appropriate periods of immobilisation for accelerated return to sport. Severe consequences can arise from over-accelerated rehabilitation, however the outcome of these injuries shows much promise when managed appropriately. It is recommended that experienced specialists should take charge of the orthopaedic care of high level athletes, as the management of their injuries is a specialised area, with unique treatment strategies and differing goals compared to the standard population.
P- Reviewer: Barbero M, Elgafy H S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Brukner P, Khan K. Brukner and Khan’s Clinical Sports Medicine 4th ed. Australia: McGraw-Hill Medical 2012; 1268. |
| 2. | Woods C, Hawkins RD, Maltby S, Hulse M, Thomas A, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football--analysis of hamstring injuries. Br J Sports Med. 2004;38:36-41. [PubMed] |
| 3. | Woods C, Hawkins R, Hulse M, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football-analysis of preseason injuries. Br J Sports Med. 2002;36:436-441; discussion 441. [PubMed] |
| 4. | Woods C, Hawkins R, Hulse M, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football: an analysis of ankle sprains. Br J Sports Med. 2003;37:233-238. [PubMed] |
| 5. | Court-Brown CM, Wood AM, Aitken S. The epidemiology of acute sports-related fractures in adults. Injury. 2008;39:1365-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Bathgate A, Best JP, Craig G, Jamieson M. A prospective study of injuries to elite Australian rugby union players. Br J Sports Med. 2002;36:265-269; discussion 269. [PubMed] |
| 7. | Bird YN, Waller AE, Marshall SW, Alsop JC, Chalmers DJ, Gerrard DF. The New Zealand Rugby Injury and Performance Project: V. Epidemiology of a season of rugby injury. Br J Sports Med. 1998;32:319-325. [PubMed] |
| 8. | Brooks JH, Fuller CW, Kemp SP, Reddin DB. Epidemiology of injuries in English professional rugby union: part 1 match injuries. Br J Sports Med. 2005;39:757-766. [PubMed] |
| 9. | Brooks JH, Fuller CW, Kemp SP, Reddin DB. Epidemiology of injuries in English professional rugby union: part 2 training Injuries. Br J Sports Med. 2005;39:767-775. [PubMed] |
| 10. | Brooks JH, Fuller CW, Kemp SP, Reddin DB. A prospective study of injuries and training amongst the England 2003 Rugby World Cup squad. Br J Sports Med. 2005;39:288-293. [PubMed] |
| 11. | Fridman L, Fraser-Thomas JL, McFaull SR, Macpherson AK. Epidemiology of sports-related injuries in children and youth presenting to Canadian emergency departments from 2007-2010. BMC Sports Sci Med Rehabil. 2013;5:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Garraway M, Macleod D. Epidemiology of rugby football injuries. Lancet. 1995;345:1485-1487. [PubMed] |
| 13. | Junge A, Dvorak J, Graf-Baumann T, Peterson L. Football injuries during FIFA tournaments and the Olympic Games, 1998-2001: development and implementation of an injury-reporting system. Am J Sports Med. 2004;32:80S-89S. [PubMed] |
| 14. | Nicol A, Pollock A, Kirkwood G, Parekh N, Robson J. Rugby union injuries in Scottish schools. J Public Health (Oxf). 2011;33:256-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Swenson DM, Henke NM, Collins CL, Fields SK, Comstock RD. Epidemiology of United States high school sports-related fractures, 2008-09 to 2010-11. Am J Sports Med. 2012;40:2078-2084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Swenson DM, Yard EE, Collins CL, Fields SK, Comstock RD. Epidemiology of US high school sports-related fractures, 2005-2009. Clin J Sport Med. 2010;20:293-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691-697. [PubMed] |
| 18. | Court-Brown CM, McQueen MM, Tornetta PI. Trauma. Orthopaedic Surgery Essentials Series. Vol. 1st ed. Philadelphia: Lippincott Williams & Wilkins 2006; . |
| 19. | Robertson GA, Wood AM, Aitken SA, Court Brown C. Epidemiology, management, and outcome of sport-related ankle fractures in a standard UK population. Foot Ankle Int. 2014;35:1143-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Robertson GA, Wood AM, Heil K, Aitken SA, Court-Brown CM. The epidemiology, morbidity and outcome of fractures in rugby union from a standard population. Injury. 2014;45:677-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Robertson GA, Wood AM, Bakker-Dyos J, Aitken SA, Keenan AC, Court-Brown CM. The epidemiology, morbidity, and outcome of soccer-related fractures in a standard population. Am J Sports Med. 2012;40:1851-1857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Aitken SA, Watson BS, Wood AM, Court-Brown CM. Sports-related fractures in South East Scotland: an analysis of 990 fractures. J Orthop Surg (Hong Kong). 2014;22:313-317. [PubMed] |
| 23. | Gaston RG, Chadderdon C. Phalangeal fractures: displaced/nondisplaced. Hand Clin. 2012;28:395-401, x. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 24. | Geissler WB. Operative fixation of metacarpal and phalangeal fractures in athletes. Hand Clin. 2009;25:409-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Shaftel ND, Capo JT. Fractures of the digits and metacarpals: when to splint and when to repair? Sports Med Arthrosc. 2014;22:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Aitken S, Court-Brown CM. The epidemiology of sports-related fractures of the hand. Injury. 2008;39:1377-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 27. | Aitken SA. The epidemiology of upper limb, lower limb and pelvic fractures in adults. University of Edinburgh, 2013. . |
| 28. | Weiss AP, Hastings H. Distal unicondylar fractures of the proximal phalanx. J Hand Surg Am. 1993;18:594-599. [PubMed] |
| 29. | Lawson GM, Hajducka C, McQueen MM. Sports fractures of the distal radius--epidemiology and outcome. Injury. 1995;26:33-36. [PubMed] |
| 30. | Henn CM, Wolfe SW. Distal radius fractures in athletes: approaches and treatment considerations. Sports Med Arthrosc. 2014;22:29-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 31. | Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989;20:208-210. [PubMed] |
| 32. | Mackenney PJ, McQueen MM, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88:1944-1951. [PubMed] |
| 33. | Rettig AC, Ryan R, Shelbourne KD, McCarroll JR, Johnson F, Ahlfeld SK. Metacarpal fractures in the athlete. Am J Sports Med. 1989;17:567-572. [PubMed] |
| 34. | Fufa DT, Goldfarb CA. Fractures of the thumb and finger metacarpals in athletes. Hand Clin. 2012;28:379-388, x. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 35. | Singletary S, Freeland AE, Jarrett CA. Metacarpal fractures in athletes: treatment, rehabilitation, and safe early return to play. J Hand Ther. 2003;16:171-179. [PubMed] |
| 36. | Etier B, Scillia AJ, Tessier DD, Aune K, Emblom BA, Dugas JR, Cain EL. Return to Play Following Metacarpal Fractures in Football Players. Orthop J Sports Med. 2014;7:1. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 37. | Singh R, Rambani R, Kanakaris N, Giannoudis PV. A 2-year experience, management and outcome of 200 clavicle fractures. Injury. 2012;43:159-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 38. | Jones GL, Bishop JY, Lewis B, Pedroza AD. Intraobserver and interobserver agreement in the classification and treatment of midshaft clavicle fractures. Am J Sports Med. 2014;42:1176-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 39. | Meisterling SW, Cain EL, Fleisig GS, Hartzell JL, Dugas JR. Return to athletic activity after plate fixation of displaced midshaft clavicle fractures. Am J Sports Med. 2013;41:2632-2636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 40. | Morgan RJ, Bankston LS, Hoenig MP, Connor PM. Evolving management of middle-third clavicle fractures in the National Football League. Am J Sports Med. 2010;38:2092-2096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 41. | Ranalletta M, Rossi LA, Piuzzi NS, Bertona A, Bongiovanni SL, Maignon G. Return to sports after plate fixation of displaced midshaft clavicular fractures in athletes. Am J Sports Med. 2015;43:565-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 42. | Robinson CM, Goudie EB, Murray IR, Jenkins PJ, Ahktar MA, Read EO, Foster CJ, Clark K, Brooksbank AJ, Arthur A. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am. 2013;95:1576-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 287] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 43. | Altamimi SA, McKee MD. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. J Bone Joint Surg Am. 2008;90 Suppl 2 Pt 1:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 111] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 44. | Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79:537-539. [PubMed] |
| 45. | McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94:675-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 275] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 46. | Fleming MA, Dachs R, Maqungo S, du Plessis JP, Vrettos BC, Roche SJ. Angular stable fixation of displaced distal-third clavicle fractures with superior precontoured locking plates. J Shoulder Elbow Surg. 2015;24:700-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 47. | Verborgt O, Pittoors K, Van Glabbeek F, Declercq G, Nuyts R, Somville J. Plate fixation of middle-third fractures of the clavicle in the semi-professional athlete. Acta Orthop Belg. 2005;71:17-21. [PubMed] |
| 48. | Grassi FA, Tajana MS, D’Angelo F. Management of midclavicular fractures: comparison between nonoperative treatment and open intramedullary fixation in 80 patients. J Trauma. 2001;50:1096-1100. [PubMed] |
| 49. | Jubel A, Andemahr J, Bergmann H, Prokop A, Rehm KE. Elastic stable intramedullary nailing of midclavicular fractures in athletes. Br J Sports Med. 2003;37:480-483; discussion 484. [PubMed] |
| 50. | Meier C, Grueninger P, Platz A. Elastic stable intramedullary nailing for midclavicular fractures in athletes: indications, technical pitfalls and early results. Acta Orthop Belg. 2006;72:269-275. [PubMed] |
| 51. | Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92:1851-1857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 152] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 52. | Pujalte GG, Housner JA. Management of clavicle fractures. Curr Sports Med Rep. 2008;7:275-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 53. | Valen B. Treatment of scaphoid fractures in a local hospital. Tidsskr Nor Laegeforen. 2013;133:1079-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 54. | Garcia RM, Ruch DS. Management of scaphoid fractures in the athlete: open and percutaneous fixation. Sports Med Arthrosc. 2014;22:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 55. | McQueen MM, Gelbke MK, Wakefield A, Will EM, Gaebler C. Percutaneous screw fixation versus conservative treatment for fractures of the waist of the scaphoid: a prospective randomised study. J Bone Joint Surg Br. 2008;90:66-71. [PubMed] |
| 56. | Modi CS, Nancoo T, Powers D, Ho K, Boer R, Turner SM. Operative versus nonoperative treatment of acute undisplaced and minimally displaced scaphoid waist fractures--a systematic review. Injury. 2009;40:268-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 57. | Yin ZG, Zhang JB, Kan SL, Wang P. Treatment of acute scaphoid fractures: systematic review and meta-analysis. Clin Orthop Relat Res. 2007;460:142-151. [PubMed] |
| 58. | Del Buono A, Smith R, Coco M, Woolley L, Denaro V, Maffulli N. Return to sports after ankle fractures: a systematic review. Br Med Bull. 2013;106:179-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 59. | Bugler KE, Watson CD, Hardie AR, Appleton P, McQueen MM, Court-Brown CM, White TO. The treatment of unstable fractures of the ankle using the Acumed fibular nail: development of a technique. J Bone Joint Surg Br. 2012;94:1107-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 60. | Porter DA, Jaggers RR, Barnes AF, Rund AM. Optimal management of ankle syndesmosis injuries. Open Access J Sports Med. 2014;5:173-182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 61. | Strömsöe K, Höqevold HE, Skjeldal S, Alho A. The repair of a ruptured deltoid ligament is not necessary in ankle fractures. J Bone Joint Surg Br. 1995;77:920-921. [PubMed] |
| 62. | Schepers T. Acute distal tibiofibular syndesmosis injury: a systematic review of suture-button versus syndesmotic screw repair. Int Orthop. 2012;36:1199-1206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 134] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 63. | Schepers T. To retain or remove the syndesmotic screw: a review of literature. Arch Orthop Trauma Surg. 2011;131:879-883. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 64. | Roche AJ, Calder JD. Treatment and return to sport following a Jones fracture of the fifth metatarsal: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:1307-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 92] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 65. | Mologne TS, Lundeen JM, Clapper MF, O’Brien TJ. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 2005;33:970-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 136] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 66. | Hens J, Martens M. Surgical treatment of Jones fractures. Arch Orthop Trauma Surg. 1990;109:277-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 67. | Larson CM, Almekinders LC, Taft TN, Garrett WE. Intramedullary screw fixation of Jones fractures. Analysis of failure. Am J Sports Med. 2002;30:55-60. [PubMed] |
| 68. | Sarimo J, Rantanen J, Orava S, Alanen J. Tension-band wiring for fractures of the fifth metatarsal located in the junction of the proximal metaphysis and diaphysis. Am J Sports Med. 2006;34:476-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 69. | Mindrebo N, Shelbourne KD, Van Meter CD, Rettig AC. Outpatient percutaneous screw fixation of the acute Jones fracture. Am J Sports Med. 1993;21:720-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 68] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 70. | Murawski CD, Kennedy JG. Percutaneous internal fixation of proximal fifth metatarsal jones fractures (Zones II and III) with Charlotte Carolina screw and bone marrow aspirate concentrate: an outcome study in athletes. Am J Sports Med. 2011;39:1295-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 71. | Nagao M, Saita Y, Kameda S, Seto H, Sadatsuki R, Takazawa Y, Yoshimura M, Aoba Y, Ikeda H, Kaneko K. Headless compression screw fixation of jones fractures: an outcomes study in Japanese athletes. Am J Sports Med. 2012;40:2578-2582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 72. | Porter DA, Rund AM, Dobslaw R, Duncan M. Comparison of 4.5- and 5.5-mm cannulated stainless steel screws for fifth metatarsal Jones fracture fixation. Foot Ankle Int. 2009;30:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 73. | Porter DA, Duncan M, Meyer SJ. Fifth metatarsal Jones fracture fixation with a 4.5-mm cannulated stainless steel screw in the competitive and recreational athlete: a clinical and radiographic evaluation. Am J Sports Med. 2005;33:726-733. [PubMed] |
| 74. | Portland G, Kelikian A, Kodros S. Acute surgical management of Jones’ fractures. Foot Ankle Int. 2003;24:829-833. [PubMed] |
| 75. | Raikin SM, Slenker N, Ratigan B. The association of a varus hindfoot and fracture of the fifth metatarsal metaphyseal-diaphyseal junction: the Jones fracture. Am J Sports Med. 2008;36:1367-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 76. | Fernández Fairen M, Guillen J, Busto JM, Roura J. Fractures of the fifth metatarsal in basketball players. Knee Surg Sports Traumatol Arthrosc. 1999;7:373-377. [PubMed] |
| 77. | Laird RC. Acute forefoot and midfoot injuries. Clin Podiatr Med Surg. 2015;32:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 78. | Robertson GA, Wood AM. Return to sport following tibial shaft fractures: a systematic review. Sports Health, 2015: Published online before print. . [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 79. | Abdel-Salam A, Eyres KS, Cleary J. Internal fixation of closed tibial fractures for the management of sports injuries. Br J Sports Med. 1991;25:213-217. [PubMed] |
| 80. | Chang WR, Kapasi Z, Daisley S, Leach WJ. Tibial shaft fractures in football players. J Orthop Surg Res. 2007;2:11. [PubMed] |
| 81. | Peter RE, Bachelin P, Fritschy D. Skiers’ lower leg shaft fracture. Outcome in 91 cases treated conservatively with Sarmiento’s brace. Am J Sports Med. 1988;16:486-491. [PubMed] |
| 82. | Fankhauser F, Seibert FJ, Boldin C, Schatz B, Lamm B. The unreamed intramedullary tibial nail in tibial shaft fractures of soccer players: a prospective study. Knee Surg Sports Traumatol Arthrosc. 2004;12:254-258. [PubMed] |
| 83. | Gaebler C, McQueen MM, Vécsei V, Court-Brown CM. Reamed versus minimally reamed nailing: a prospectively randomised study of 100 patients with closed fractures of the tibia. Injury. 2011;42 Suppl 4:S17-S21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 84. | Gaston P, Will E, Elton RA, McQueen MM, Court-Brown CM. Fractures of the tibia. Can their outcome be predicted? J Bone Joint Surg Br. 1999;81:71-76. [PubMed] |
| 85. | Habernek H. Percutaneous cerclage wiring and interlocking nailing for treatment of torsional fractures of the tibia. Clin Orthop Relat Res. 1991;164-168. [PubMed] |
| 86. | Keating JF, O’Brien PJ, Blachut PA, Meek RN, Broekhuyse HM. Locking intramedullary nailing with and without reaming for open fractures of the tibial shaft. A prospective, randomized study. J Bone Joint Surg Am. 1997;79:334-341. [PubMed] |
| 87. | Salai M, Blankstein A, Israeli A, Chechik A, Amit Y, Horoszowski H. Closed intramedullary nailing of tibial fractures in sportsmen. Br J Sports Med. 1988;22:82. [PubMed] |
| 88. | Shaw AD, Gustilo T, Court-Brown CM. Epidemiology and outcome of tibial diaphyseal fractures in footballers. Injury. 1997;28:365-367. [PubMed] |
| 89. | Khalid M, Brannigan A, Burke T. Calf muscle wasting after tibial shaft fracture. Br J Sports Med. 2006;40:552-553. [PubMed] |