Revised: January 16, 2014
Accepted: March 17, 2014
Published online: April 18, 2014
Processing time: 186 Days and 13.2 Hours
Treatment of children with cervical spine disorders requiring fusion is a challenging endeavor for a variety of reasons. The size of the patients, the corresponding abnormal bony anatomy, the inherent ligamentous laxity of children, and the relative rarity of the disorders all play a part in difficulty of treatment. The benefits of modern posterior cervical instrumentation in children, defined as rigid screw-rod systems, have been shown to be many including: improved arthrodesis rates, diminished times in halo-vest immobilization, and improved reduction of deformities. The anatomy of children and the corresponding pathology seen frequently is at the upper cervical spine and craniocervical junction given the relatively large head size of children and the horizontal facets at these regions predisposing them to instability or deformity. Posterior screw fixation, while challenging, allows for a rigid base to allow for fusion in these upper cervical areas which are predisposed to pseudarthrosis with non-rigid fixation. A thorough understanding of the anatomy of the cervical spine, the morphology of the cervical spine, and the available screw options is paramount for placing posterior cervical screws in children. The purpose of this review is to discuss both the anatomical and clinical descriptions related to posterior screw placement in the cervical spine in children.
Core tip: This paper reviews the techniques used for modern posterior screw fixation of the pediatric cervical spine. The preoperative considerations, necessary studies, and surgical techniques are reviewed in order to educate the reader on the use of modern screw fixation in the pediatric cervical spine. Upper cervical fixation techniques as well as lateral mass screw fixation in the subaxial spine are discussed.
- Citation: Hedequist DJ. Modern posterior screw techniques in the pediatric cervical spine. World J Orthop 2014; 5(2): 94-99
- URL: https://www.wjgnet.com/2218-5836/full/v5/i2/94.htm
- DOI: https://dx.doi.org/10.5312/wjo.v5.i2.94
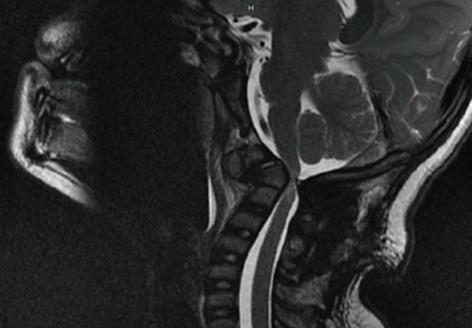
The standard preoperative work-up of any child undergoing surgical treatment for a cervical spine problem will include plain radiographs, magnetic resonance imaging, and computed tomography scanning. Plain radiographs include anterior-posterior and lateral views, as well as flexion-extension lateral views of the cervical spine. The use of magnetic resonance imaging (MRI) is important as it gives detail oriented information regarding the spinal cord, neuroforamen, and position of the vertebral artery. Areas of compression are readily visualized as well as cord signal changes which are important to have as a baseline in patients with instability or neurologic findings (Figure 1).
Computed tomography (CT) scanning with fine cut images is important as it gives concrete information regarding the bony anatomy as well as the course of the vertebral artery. Three-dimensional reconstructions are of paramount importance in cases of upper cervical instrumentation as it gives the surgeon a complete understanding of the course of the vertebral artery which is mandatory with upper cervical screw placement. The standard use of CT angiography or MR angiography is not needed unless either significant congenital bony malformations are present or high grade instability is present with concern regarding the course of the vertebral artery. We have also found in some cases of tumor encasement that angiography is helpful to define the exact location of the vertebral artery as well as the patency of the vertebral artery.
Depending on the reason that cervical surgery is performed fiberoptic techniques may be required for intubation or nasal intubation may be required. Frequently instability is present requiring immobilization during airway placement and having an anesthesiologist present who is experienced in difficult airways is paramount to patient safety. The use of a halo-vest for positioning or Gardner-wells tongs for positioning is of great importance to secure the cranium and allow for adequate fluoroscopic visualization. In the majority of patients I place the halo crown and attach it to a vest and then turn the patient to prone positioning. The posterior aspect of the vest can then be removed for the operation (Figure 2). This is important for a variety of reasons, the first being complete immobilization of the head and neck during positioning and turning which is the safest way to turn when a patient is completely relaxed under anesthesia. Second, placing the patient in a halo crown and vest also allows me to afford reduction of deformities and to place the skull in the appropriate position in order to avoid craniocervical fusions done in misalignment. Finally, if the patient is going to stay in a vest then at the end of the operation the posterior vest can be added and the patient safely turned and then extubated.
The use of neurologic monitoring is required for all pediatric patients undergoing cervical instrumentation and fusion. The standard for all patients is motor-evoked monitoring, sensory monitoring, as well as EMG monitoring of the upper limb. Anesthetic agents should be used which don’t interfere with the ability to obtain stable and reliable monitoring.
Fixation at C1 in the past has traditionally been with sublaminar wiring underneath the arch of the atlas, which is inherently not dangerous or technically difficult given the space available for the cord at this level. However, wiring or cable grafting is problematic both biomechanically and from a pathologic standpoint. C1 wiring is inherently not stable in rotation which is problematic given the articulation of C1 with both the occiput and C2 allows for the majority of cervical rotation. From a clinical standpoint, the posterior ring of C1 frequently requires removal in cases where decompression is required and then wiring is not an option. These factors have led to the anatomical studies of the lateral mass of C1 to determine if screw fixation is feasible, and if so then what are the anatomical constraints[1-3].
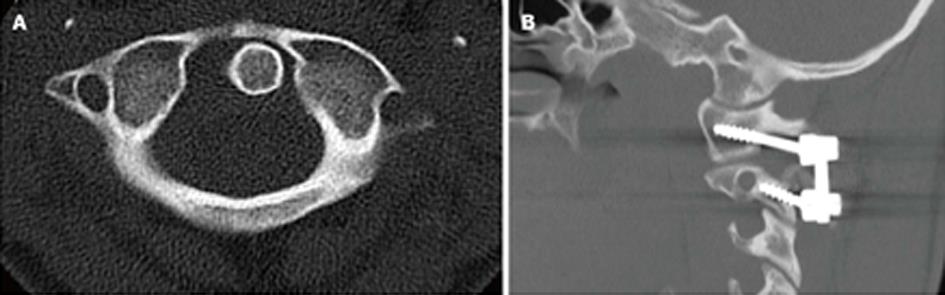
The lateral mass of C1 is a quadrilateral structure of bone lying anterolateral to the spinal cord and in close relationship to the vertebral artery, which lies in the anterolateral confines of the lateral mass. The surgical exposure of the lateral mass entry point is challenging for a variety of reasons. The entry point of the lateral mass screws requires following the posterior arch of C1 surgically down to the entry point into the lateral mass (Figure 3A). This can be done by electrocautery dissection staying on the inferior aspect of the posterior arch of C1 as the vertebral artery lies on the superior aspect of the ring of C1 as it exits from the skull base. Classically the teaching had been the vertebral artery is at risk 1.5 cm from the midline, this has never been validated in children and is not a reliable rule in pathologic cases. Nevertheless, the current recommendation would be to be aware of the position of the vertebral artery laterally on the superior aspect of C1 and if need be a preoperative CT angiography study is helpful, especially with congenital deformities. The ring of C1 gradually turns away and into the lateral mass of C1 and this region needs to be dissected out with meticulous attention to the venous plexus, which is diffuse and engulfs this region. Aggressive bipolar cautery of these venous bleeders prophylactically will make exposure of the entry point easier. The C2 nerve root also is encountered running below the arch of C1 and needs to be identified to find the lateral mass starting point. Variation exists in opinion regarding the need sacrifice the root of C2 for better exposure[4]. I have found this not to be required for adequate exposure or for safe screw placement.
The ideal starting point of C1 screws can be found by studying the preoperative CT scan of the patient, however in all cases the screw starting point remains underneath the arch of C1, although occasionally the undersurface of the arch where it meets the bony lateral mass needs to be burred away (Figure 3B). The starting point is usually in line where the arch meets the lateral mass, it is never lateral to the arch and the medial border is easily identified with a freer. The spinal cord is not at risk with this screw given the entry point is anterolateral and usually lies at the anterior-posterior midpoint of the cord.
The C1 lateral mass usually allows for screw placement even in the youngest of pediatric patients. In a recent series of patients as young as two years of age, CT evaluation revealed that the mean length available for the lateral mass screw was greater than 15 mm and the mean medial-lateral dimensions were greater than 7 mm which would allow for safe placement in all patients of a 3.5 mm screw[2]. The screw trajectory was evaluated in another series of pediatric patients with CT scans and confirmed from an optimal starting point the ideal screw trajectory would be medially angled 16 degrees and could be placed to a depth of 20 mm[1]. In that study, the placement of screws was deemed feasible in 151/152 lateral masses.
Clinically, the anatomic feasibility found in CT studies has been shown to be a reliable indicator of anatomy in children. Two recent series looking specifically at screw placement into C1 in pediatric patients documented successful screw placement with no intraoperative complications and uneventful fusion for a variety of pediatric pathologic conditions[5,6].
The axis plays a significant role in the management of cervical spine problems in children requiring instrumentation and fusion. It can be either the base of a craniocervical fusion; it may be coupled with the atlas in cases of atlanto-axial instability, or may be the top of a mid-level fusion. Many screw options exists for the axis and are preferable to subaxial cabling as the space available for the cord is much less at the axis rendering sub laminar placement of wires dangerous and the inherent biomechanical weakness of cabling. Screw fixation into the axis may be divvied into three separate screw types: pedicle, pars, and intralaminar. The placement of which screw is dependent on a variety of factors which may be seen on the preoperative CT scanning, notably the width of the bony channels and the position of the vertebral artery[7].
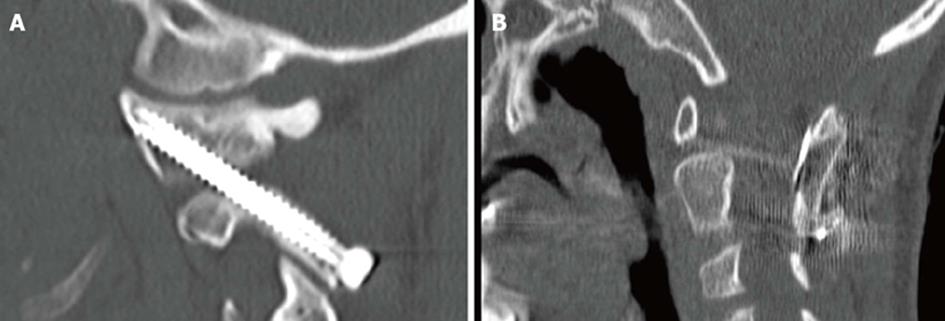
The C2 spinouts process is used as a landmark in the upper cervical spine and can be used as the entry point for intralaminar screws. Intralaminar screws at C2 have been shown to be effective for rigidity of constructs in biomechanical studies[8]. The entry point for C2 laminar screws is on the contralateral side of the spinous process and needs to be placed either caudal or rostral in the spinous process so that crossing screws can be placed (Figure 4A). The dorsal aspect of the lamina is exposed the same for all cervical fusions involving the axis. A starting point on the contralateral side of the spinous process is made using a burr and then the lamina is annulated using an awl. Looking at the dorsal lamina easily sees the rostral-caudal orientation. The avoidance of penetrating the ventral lamina and spinal canal can be done by placing a freer via blunt dissection under the ventral lamina as a landmark to avoid misguided trajectory. Screw length can be estimated by the preoperative studies of the presumed screw tract.
CT analysis of the upper cervical vertebra has shown that the lamina is able to accept 3.5 mm screws in most patients. A recent tomographic study of children revealed screw lengths measured on CT to be around a mean of 20 mm with the majority of lamina having a bony channel able to withstand screw placement[2]. Clinically, the placement of laminar screws has been shown to be safe and efficacious and the decision regarding intralaminar screw placement can be determined with preoperative CT in all patients[7,9,10]. The complication of canal breach has not been reported in multiple clinical studies regarding screw placement in children[5,7].
There is variability in the terminology of C2 screws placed in the pars/isthmus/pedicle. Two separate screw paths exist which have been described, each with different starting points and risks associated with their trajectory. The pars and pedicle are intertwined in a shared mass of bone in the atlas, which needs to be directly visualized during surgical dissection. During dissection as the lamina is followed down laterally the isthmus of C2 can then be followed going superiorly and medially. The dissection of the isthmus is paramount for defining safe screw trajectory as the dorsal and medial part of the isthmus is readily dissected aiding in direct visualization in screw path. The dissection of the isthmus must be done with bipolar cautery to avoid bleeding from the venous plexus, which engulfs the C1-C2 posterior bony complex. The medial aspect of isthmus once dissected can be used to guide screw trajectory and avoid unwanted canal penetration, placing a freer on the medial side will help directly visualize the screw path. Placement of C2 screws can be done with the determination of a pedicle screw or a pars screw. Pars screws are done with a starting point more caudal and just above the C2-C3 facet in the midline. The medial-lateral determination is done by using the medial dissected out isthmus as the landmark and the lateral trajectory is done under fluoroscopic guidance using the dorsal isthmus as a landmark as well. The length if the pars screw is directly determined by the course of the vertebral artery as well as by the C1-C2 articulation (Figure 4B). C2 pedicle screws share the same isthmus of bone but the starting point is more superior and lateral than the pars screws. The screw trajectory is more medially directed and headed into the C2 body, placing the canal at risk unless dissection has identified the medial pars (Figure 4C).
The morphometric studies regarding C2 screws are not entirely clear regarding the variation of pedicle versus pars, but can be interpreted regarding the shared isthmus of bone necessary for screw placement. In a morphometric study of children less than six years of age the mean width of the pedicle measured on CT scan was greater than 3.5 mm and the mean pedicle length was greater than 17 mm[2].
Multiple clinical studies exit regarding the use of pars/pedicle screws in children. While not entirely clear of the separation of pars/pedicle screws it is clear that screws can be place in the vast majority of patients without injury to the vertebral artery or malposition of screws[5-7]. These clinical studies show that rigid screw fixation either through pars/pedicle or intralaminar screws are possible in almost all patients and serves as an excellent and reliable fixation point in pediatric deformity surgery.
Placement of C1-C2 transarticular screws remains a powerful yet challenging technique of fixation. Classically, these screws are placed for C1-C2 instability but may be placed as a base for craniocervical constructs. The challenges of screw placement make dissection of the C2 isthmus as well as C1-C2 joint mandatory for safe screw placement.
The placement of transarticular screws demands a complete understanding of the course of the vertebral artery both in its relationship to the axis and in its relationship to C1. The course of the vertebral artery is anomalous in up to 25% of patients in clinical studies where screw placement would be beneficial[11]. The most common problematic course in relationship to C2 is either a medially deviated course where the ideal trajectory of the screw from the isthmus of C2 into the C1 lateral mass does not exist or in a sagittal plane abnormality where the vertebral artery is high riding and lead to a small isthmus negating any potential screw placement[7]. The position of the vertebral artery in relationship to the C1 lateral mass is also of paramount importance screw placement must end up in the lateral mass after crossing the joint.
Morphometric studies of upper cervical anatomy suggest that a minority of patients less than six have anatomy suitable for transarticular screws given either the size of the C2 isthmus or the course of the vertebral artery[2]. Clinical studies have shown that even in younger patients screws may be safely placed if the preoperative imaging suggests anatomy, which allows for safe screw placement[12,13].
Adequate visualization of the C2 isthmus is paramount to safe screw placement and is done as described above for pars screws. The C1-C2 joint must also be in a reduced position and accessible by direct fell via a freer elevator. We have used a cannulated screw system at our institution and once the guide wire is placed thru C2 into the joint we have made it a step of the procedure then to adequately feel with a freer the guide wire in a good position as well as using confirmatory biplanar fluoroscopy. There is minimal room for error using transarticular screws so guide wire placement in a correct position and must be done by C2 pars visualization, palpation of the guide wire in the C1-C2 joint, and confirmation of correct guide wire placement on AP and lateral fluoroscopy. Once adequate guide wire placement has been done then screws can be placed after measuring, drilling, and tapping (Figure 5A).
Placement of a unilateral C1-C2 transarticular screw is occasionally needed if the anatomy of the vertebral artery on both sides is not symmetrical. Biomechanically his has been shown to be reasonable fixation[13]. We have made it a habit to placed autogenous structural iliac crest graft between C1 and C2 in cases where the ring of C1 is present in order to augment the posterolateral gutter fusion. Typically we have place a horseshoe shaped graft and secured it via cables placed underneath the ring of C1 and through the spinouts process of C2 (Figure 5B).
Clinically, transarticular screws have been safely used in children who have safe anatomy on preoperative CT scans. Brockmeyer reviewed his series of patients treated with transarticular screws and found safe screw placement in children younger than age four[13,14].
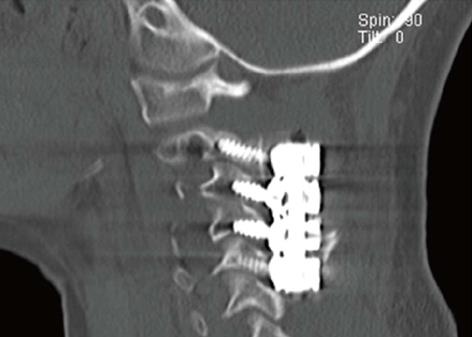
The use of lateral mass screws has been studied in children and shown to be safe and efficacious if the preoperative template on CT scanning is favorable[15,16]. The lateral mass is a quadrangular structure of bone, which has a medial border of the spinal canal and an anterior border the vertebral artery. Multiple techniques exist for placement of screws in the lateral mass with variation in the starting point and variation in both the laterally directed and the cranially directed angle. I have used the modified technique of dividing the lateral mass into a box with the facet above and below being the cranial and caudal borders, the lateral edge of bone being the lateral border and the medial border being where the lamina meets the facet. The starting point for screw placement is 1 mm inferior and 1mm medial to the center of this box. The angulation is approximately 15 degrees laterally and the cranial angulation is dictated by the lateral fluoroscopic views. Fluoroscopy is necessary in children given the small size of the lateral mass does not allow for false drill passage given this will not allow for redirection.
At our institution we have studies the use in lateral mass screws for a variety of pathologic conditions in children. Post-operative computed tomography scanning has shown complete screw containment in all cases and there have been no vertebral artery injuries or post-operative nerve deficits[15,16]. Standard screw diameter is 3.5 mm and we have found it useful to have screws as low as 8 mm in length to avoid anterior penetration into the vertebral artery by a long screw. We have placed subaxial screws in children as young as four years of age, although the indications for this age group are rare given most pathologic conditions in younger children involve the craniocervical junction and the upper cervical spine (Figure 6). We have not used cervical pedicle screws in pediatric patients given the cadaveric anatomical studies showing the size of the pedicle is not adequate for screw placement in the majority of patients[17].
Surgeons taking care of children with cervical spine abnormalities will encounter a wide variety of pathologic conditions requiring fusion. Stability of the spine, reduction of deformities, protection of the spinal cord, and enhanced fusion all are aided by stability obtained with modern instrumentation using screw-rod constructs. These constructs have been shown to be both feasible in morphometric studies as well as safe in clinical studies. Placement of screws demands a complete understanding of the preoperative anatomy which can be done by adequate preoperative studies. Finally, given the small nature of the patients meticulous surgical dissection is paramount to safe screw placement. The modern techniques will lead to an improved rate of arthrodesis while minimizing any time needed in external immobilization which ultimately leads to better patient/family satisfaction.
P- Reviewers: Canavese F, Hyun SJ, Landi A S- Editor: Gou SX L- Editor: A E- Editor: Lu YJ
| 1. | Chamoun RB, Whitehead WE, Curry DJ, Luerssen TG, Jea A. Computed tomography morphometric analysis for C-1 lateral mass screw placement in children. Clinical article. J Neurosurg Pediatr. 2009;3:20-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Geck MJ, Truumees E, Hawthorne D, Singh D, Stokes JK, Flynn A. Feasibility of Rigid Upper Cervical Instrumentation in Children: Tomographic Analysis of Children Aged 2 to 6. J Spinal Disord Tech. 2013;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001;26:2467-2471. [PubMed] |
| 4. | Patel AJ, Gressot LV, Boatey J, Hwang SW, Brayton A, Jea A. Routine sectioning of the C2 nerve root and ganglion for C1 lateral mass screw placement in children: surgical and functional outcomes. Childs Nerv Syst. 2013;29:93-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Haque A, Price AV, Sklar FH, Swift DM, Weprin BE, Sacco DJ. Screw fixation of the upper cervical spine in the pediatric population. Clinical article. J Neurosurg Pediatr. 2009;3:529-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Desai R, Stevenson CB, Crawford AH, Durrani AA, Mangano FT. C-1 lateral mass screw fixation in children with atlantoaxial instability: case series and technical report. J Spinal Disord Tech. 2010;23:474-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Hedequist D, Proctor M. Screw fixation to C2 in children: a case series and technical report. J Pediatr Orthop. 2009;29:21-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Lehman RA, Dmitriev AE, Helgeson MD, Sasso RC, Kuklo TR, Riew KD. Salvage of C2 pedicle and pars screws using the intralaminar technique: a biomechanical analysis. Spine (Phila Pa 1976). 2008;33:960-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 81] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Lehman RA, Sasso RC, Helgeson MD, Dmitriev AE, Gill NW, Rosner MR, Riew KD. Accuracy of intraoperative plain radiographs to detect violations of intralaminar screws placed into the C2 vertebrae: a reliability study. Spine (Phila Pa 1976). 2007;32:3036-3040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Chern JJ, Chamoun RB, Whitehead WE, Curry DJ, Luerssen TG, Jea A. Computed tomography morphometric analysis for axial and subaxial translaminar screw placement in the pediatric cervical spine. J Neurosurg Pediatr. 2009;3:121-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Anderson RC, Ragel BT, Mocco J, Bohman LE, Brockmeyer DL. Selection of a rigid internal fixation construct for stabilization at the craniovertebral junction in pediatric patients. J Neurosurg. 2007;107:36-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Brockmeyer D, Apfelbaum R, Tippets R, Walker M, Carey L. Pediatric cervical spine instrumentation using screw fixation. Pediatr Neurosurg. 1995;22:147-157. [PubMed] |
| 13. | Brockmeyer DL, York JE, Apfelbaum RI. Anatomical suitability of C1-2 transarticular screw placement in pediatric patients. J Neurosurg. 2000;92:7-11. [PubMed] |
| 14. | Gluf WM, Brockmeyer DL. Atlantoaxial transarticular screw fixation: a review of surgical indications, fusion rate, complications, and lessons learned in 67 pediatric patients. J Neurosurg Spine. 2005;2:164-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 123] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 15. | Hedequist D, Proctor M, Hresko T. Lateral mass screw fixation in children. J Child Orthop. 2010;4:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Hedequist D, Hresko T, Proctor M. Modern cervical spine instrumentation in children. Spine (Phila Pa 1976). 2008;33:379-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Vara CS, Thompson GH. A cadaveric examination of pediatric cervical pedicle morphology. Spine (Phila Pa 1976). 2006;31:1107-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |