INTRODUCTION
Shoulder dislocations account for about 50% of all major joint dislocations presenting to emergency departments, and the most common type (95%-98%) of this frequent injury is the anterior shoulder dislocation[1-9]. Acute anterior shoulder dislocations usually represent impressing orthopaedic emergency cases, and reduction should be performed as soon as possible, as reduction is the most effective pain relief therapy.
More than 2500 years ago Hippocrates (460-377 B.C.) described in detail various methods for reducing shoulder dislocations, and reduction with the heel has become the most famous one (Figure 1). Hippocrates stated, that “reduction is to be effected, if possible, immediately while still warm, otherwise as quickly as it can be done for reduction will be a much quicker and easier process for the operator and a much less painful one to the patient if effected before swelling comes on”[10-14].
Figure 1 The most famous Hippocrates method for reducing anterior shoulder dislocations using the operator´s heel in the patient´s axilla for counter-traction.
The operator can use his whole body weight to perform traction on the injured arm.
Since that time, at least 34 different methods for reducing shoulder dislocations have been reported in the literature and are used, often not evidence based and with little scientific theory behind their use[2,8,10-13,15-34]. And in spite of the fact that the Hippocrates method hardly has been evaluated in a scientific manner and numerous associated iatrogenic complications have been reported, this method remains to be one of the most common techniques for reducing anterior shoulder dislocations, especially in European countries[8,25,26,35-40].
We report the case of a 69-year-old farmer under coumarin anticoagulant therapy who sustained acute first time anterior dislocation of his dominant right shoulder. By using the Hippocrates method with the patient under general anaesthesia, the brachial vein was injured and an increasing hematoma subsequently caused brachial plexus paresis by pressure.
CASE REPORT
A 69-year-old famer fell off his tractor and thereby sustained a traumatic first-time anterior dislocation of his dominant right shoulder. Due to cardiac arrhythmia he has been under coumarin anticoagulant therapy since 15 years. On admission at a foreign clinic in a rural area more than six hours after the occupational accident the neurovascular status of the right arm was documented as regular. The right shoulder region revealed the typical clinical signs of an anterior shoulder dislocation, but there were absolutely no signs of soft tissue swelling or hematoma. Radiological evaluation of the right shoulder (true anteroposterior and outlet views) confirmed a subcoracoidal anterior shoulder dislocation with a classical Hill-Sachs lesion. Closed reduction was performed subsequently under general anaesthesia using the Hippocrates method. Post-reduction X-rays showed successful relocation of the right shoulder and the already known Hill-Sachs lesion, but additional fractures could be excluded.
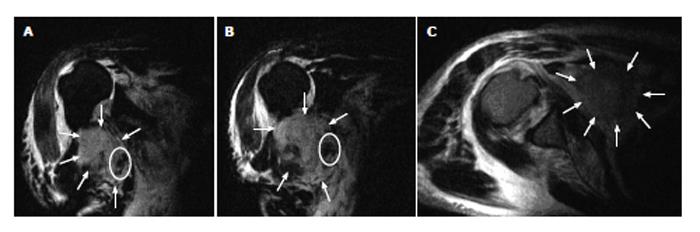
Twelve hours after reduction the patient complained about an increasing swelling in the right axillary region combined with paresthesia of the whole right hand. Clinical examination revealed a right drop hand, and active flexion of the right elbow was not possible anymore. Coumarin medication had already been stopped at admission, but the current international normalised ratio value was still 3.1. Open magnetic resonance imaging (MRI) examination showed ruptures of the rotator cuff and of the short tendon of the biceps muscle as well as a massive retropectoral hematoma (5.0 cm × 7.5 cm × 8.5 cm) compressing the axillary neurovascular bundle (Figure 2). Thereupon the patient was transferred to our level one trauma centre for surgical treatment.
Figure 2 Open magnetic resonance imaging coronar STIR T2 (A and B) and axial TSE T2 (C) sequences representing a large retropectoral hematoma (arrows) compressing the neurovascular bundle (ellipse).
Note striking raised position of the humeral head due to massive rotator cuff tears (A and B).
Immediate surgical exploration of the right axillary region was performed under medical promotion of coagulation by prothrombin complex concentrate (PPSB) and showed extensive soft tissue trauma with disruption of the short tendon of the biceps muscle, rupture of the coracobrachial muscle and 300 mL retropectoral hematoma which was evacuated. The whole neurovascular bundle was surrounded by hematoma and there was severe soft tissue edema especially at the course of the radial nerve near to the outflow of the deep brachial artery. After meticulous exposure of the neurovascular bundle we finally found a small tear of the proximal brachial vein which had to be sutured microsurgically. The radial, median and ulnar nerves as well as the deep brachial artery were found to be intact.
After recovery from general anaesthesia motor function of the right arm increased rapidly, but neurological examination three days after surgery still revealed incomplete brachial plexus palsy without sensory deficits. Therefore the patient performed prolonged physiotherapy, and six months after trauma motor function of the right hand had fully recovered. Activities of daily living were nearly not restricted and working as a farmer was possible again, but due to the rotator cuff tears the patient still had problems performing overhead activities like combing hair, for example.
DISCUSSION
The presented case report shows that the Hippocrates method for reducing anterior shoulder dislocations can-at least in inexperienced hands and feet-lead to severe iatrogenic complications. In this case we have the rare advantage of an extensive and accurate documentation of the initial treatment in the foreign clinic, as a standardized documentation is mandatory when treating an occupational accident. Documented lapse of symptoms as well as intraoperative findings confirm the strong suspicion that the described neurovascular complications were iatrogenically caused by the use of the Hippocrates method under general anaesthesia and not by the primary trauma, as the first symptoms of neurovascular damage occurred twelve hours after reduction and as the whole neurovascular bundle was surrounded by hematoma and there was a severe soft tissue edema at the course of the radial nerve near to the outflow of the deep brachial artery, and this is exactly where the operator’s heel has been positioned while performing the reduction.
Of course it is not always possible to decide if a vascular injury had been caused by the dislocation trauma itself or iatrogenically by the reduction maneuvre. A lesion of a vein or a smaller artery caused by the initial trauma might primarily be occluded by the dislocated humeral head and might start bleeding not before a successful reduction has diminished the occluding pressure on the injured vessel. But in our case the patient was under coumarin anticoagulant therapy and the first clinical examination was performed more than six hours after trauma, so that it is very unlikely that the tear of the proximal brachial vein was caused by the initial trauma without development of a significant axillary haematoma within six hours.
Allie reported that 19 out of 27 patients with primary axillary artery injuries after shoulder dislocation showed a striking axillary mass already at the time of initial presentation[37].
Regarding the Hippocrates method for reducing anterior shoulder dislocations numerous iatrogenic complications have been reported in the literature[35,36,38-40]. Schmal reported a tear of the subscapular artery, for example, and Cyffka recognized an iatrogenically caused displaced humeral head fracture after performing the Hippocrates method[35,36].
Several pathogenic mechanisms can be proposed in order to explain neurovascular damage caused by performing the Hippocrates method. On the one hand, the dislocated humeral head can act as a fulcrum over which the neurovascular bundle is bent while performing traction on the injured arm, and the operator’s heel can push the vessels against the tight inferior rim of the pectoralis minor muscle and thus cause a pincer-like shear stress on the vessels as well as severe direct local damage (Figure 3). On the other hand, simple tethering of the axillary vessels by their subscapular and circumflex branches can lead to disruption by performing traction on the arm and counter-traction by use of the heel, whereupon excessive forces are possible by use of the whole body weight (Figure 1).
Figure 3 Topographic relations between the axillary neurovascular bundle and the humeral head in normal (A) and anteriorly dislocated (B) position.
The humeral head, acting as a fulcrum, and the tight caudal rim of the pectoralis minor muscle can lead to pincer-like forces on the neurovascular bundle during performing the Hippocrates method for reducing anterior shoulder dislocations.
Predisposing factors for vascular injuries during shoulder reduction are old age with associated atherosclerotic changes of the vessels and recurrent shoulder dislocations, as repeated trauma can cause periscapular fibrosis and adhesions with fixation of the axillary artery and vein branches, which may lead to tearing of the vessels during a subsequent reduction maneuvre[39].
Another relevant risk factor for iatrogenic damage by performing shoulder reductions might be the primary use of general anaesthesia, as the physician can not get any feedback from the patient during as well as a certain period after reduction until the patient is conscious again. In our case, the patient might have recognized the ongoing development of neurovascular damage some hours earlier without the use of general anaesthesia. And in our long-time experience more than 90% of anterior shoulder dislocations can successfully be reduced without the use of general anaesthesia (unpublished data).
According to the original description of the Hippocrates reduction method by use of the heel “the patient must lie supine, usually on the floor. The doctor must stand on the side of the injured shoulder. He holds the upper extremity with both hands, pulls it toward his side, and by using, for example, his right heel in the right axilla, he counterpushes the head of the humerus, which is thus easily reduced.” Hippocrates additionally stated that “it is wise to put a small hard cotton ball in the axilla before starting to push to minimize trauma and maximize the surfaces where pressure is applied”[12]. But this ancient advice is usually not considered anymore today.
There are at least 33 alternative reduction techniques for anterior shoulder dislocations reported in the literature, among which the Kocher method, the Milch technique and the Scapular Manipulation technique have been evaluated scientifically in several studies each[2,8,10-13,15-34].
Like the Hippocrates method, also the Kocher method is associated with iatrogenic complications and thus should not be used as a first choice in our opinion[12,33]. The Milch technique and the Scapular Manipulation technique, however, have proved to be safe as well as successful[10,16,27-32]. According to these data we are primary using a modified Scapular Manipulation technique for reducing anterior shoulder dislocations at our department[33].
In conclusion, the hazardousness of using the Hippocrates method can be explained by traction on the outstretched arm with force of the operator’s whole body weight, direct trauma to the axillary region by the physician’s heel, and the topographic relations of neurovascular structures and the dislocated humeral head. As there is a variety of alternative reduction techniques which have been evaluated scientifically and proofed to be safe, we strongly caution against the use of the Hippocrates method as a first line technique for reducing anterior shoulder dislocations, especially in elder patients with fragile vessels or under anticoagulant therapy, and recommend the Scapular Manipulation technique or the Milch technique, for example, as a first choice.