INTRODUCTION
Cervical fractures are potentially devastating injuries due to the potential deleterious neurological sequelae that can result. In general, the more superior the injury, the greater the chance for morbidity and mortality; craniocervical junction injuries can be the deadliest[1]. One of the most vulnerable cervical vertebrae in trauma is the C2 segment. It is estimated that C2 fractures occur in 10%-20% of all cervical injuries[2-5]. The incidence of C2 fractures is on the rise[6], and it is now the most commonly fractured vertebra in the elderly[7,8]. Fractures that involve the odontoid process of C2 are commonly categorized according to the Anderson and D’Alonzo system[4]. Type II odontoid fractures are not infrequently deemed unstable and surgical stabilization is warranted. In contrast, type I odontoid fractures are rarely unstable, and type III odontoid fractures are most often stable enough to be treated with an external orthosis such as halo bracing. Rarely, patients with type III odontoid fractures can present with additional instability in the form of a distractive component with significant vertical displacement and even spinal cord injury[9,10]. In this case report, we present the uncommon case of a transverse C2 body fracture with a distractive and rotational component. We discuss the diagnosis and management of patients with this pathology.
CASE REPORT
A 28-year-old female presented to the emergency department with a catalogue of injuries following a roll-over motor vehicle accident (MVA). She had been riding without seatbelt restraints and was ejected from the vehicle. Most notably, she had significant pain and subjective weakness of her left shoulder. On neurological examination she had full strength throughout her right upper extremity. Examination of her left upper extremity found weakness in the biceps, triceps, wrist flexion, wrist extension, and finger grip: Motor Research Council (MRC) strength score 4+ out of possible 5. Her left deltoid strength was the weakest of all muscle groups, scoring 0 out of 5.
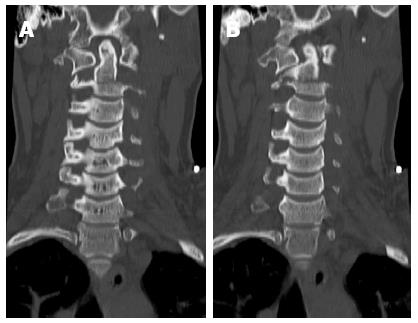
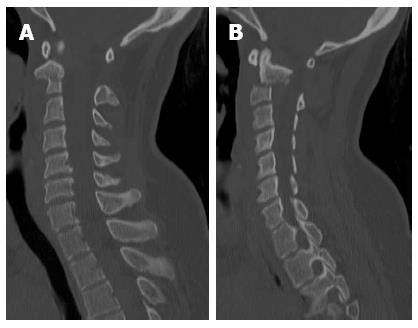
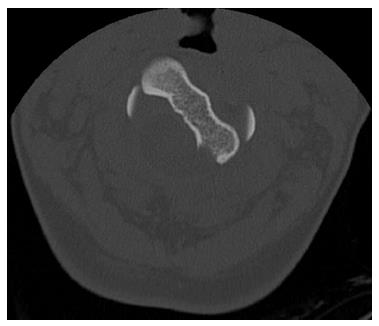
Computer tomography (CT) of the cervical spine revealed an acute comminuted transverse fracture through the body and both transverse processes of the C2 vertebrae, involving the foramina transversaria bilaterally (Figure 1). The C2 body involved a significant rotational component (Figure 2) such that the left portion of the body was within the vertebral canal causing stenosis (Figure 3). Epidural hemorrhage was also noted within the spinal canal at levels C1-C2. As this was deemed a highly unstable fracture, the patient was immediately fixated in a halo and steroids were administered for potential cord injury.
Figure 1 Reformatted coronal computer tomography images showing the transverse body fracture extending through the transverse processes (A, B).
Figure 2 Reformatted sagittal computer tomography images right of midline (A), and left of midline (B).
Figure 3 Axial computer tomography showing left rotational component of upper C2 body.
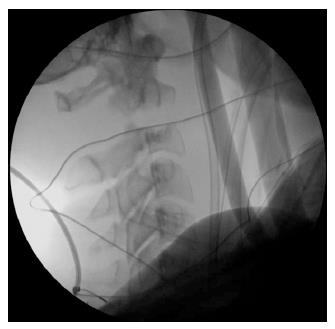
The patient was neurologically stable on post-halo day 1, but on post-halo day 2, her neurological examination began to worsen. She now demonstrated MRC strength of 0 out of 5 in the left deltoid, 0 out of 5 in the left biceps, 3 out of 5 in the left triceps, and 2 out of 5 in left hand grip. MRI did not show significant spinal cord compression. Consequently, the etiology of her weakness was not clear, although a brachial plexus injury was considered. However, surgical stabilization of her C2 fracture was recommended given that the fracture did not appear stable, even with halo bracing (Figure 4). A C1 to C4 posterior spinal fusion with placement of lateral mass screws at C1, C3, and C4 was performed. Significant improvement in the distractive and rotational mal-alignment was achieved. There were no intraoperative complications.
Figure 4 Lateral X-ray image showing persistent distraction in halo brace.
Postoperatively the patient demonstrated MRC strength of 3 out of 5 in left hand grip and left triceps. Left deltoid and biceps strength were still trace out of 5. She remained neurologically stable throughout the rest of her hospital stay and was discharged to a subacute rehabilitation facility. At 2-year follow-up, the patient had made a remarkable recovery of motor function. On examination, she had full strength throughout both her left and right upper extremities (5 out of 5 for deltoids, biceps, triceps, wrist extension, wrist flexion, and finger grip). She did report moderate residual neck pain. Cervical X-ray demonstrated proper placement of instrumentation without evidence of hardware failure and CT confirmed fusion (Figure 5).
Figure 5 Reformatted sagittal computer tomography image obtained at 2-year follow-up showing anatomic alignment and fused segments.
DISCUSSION
Cervical spine injuries can be associated with significant morbidity and even mortality when the spinal cord is injured[11]. One of the most vulnerable cervical levels following trauma is the C2 level[2]. There are a variety of fractures and injuries that can occur at this level. The most common C2 fractures include lateral mass fractures, extension teardrop fractures, traumatic spondylolisthesis (hangman fractures), and odontoid (or dens) fractures[12]. It is estimated that odontoid fractures occur in 10%-20% of all cervical spine injuries[2-5] and its incidence has been reported to be on the rise[6].
Odontoid fractures most commonly occur following trauma after a mechanical fall or motor vehicle collision[13]. The mechanism of injury is a dorsal blow to the head[14]. Its presentation can range from asymptomatic to severe neurological deficits such as quadriparesis. There are also rare reports of patients who present with specific spinal cord syndromes such as Brown-Sequard syndrome[15]. Diagnosis of odontoid fractures relies heavily on imaging, typically plain films (with anteroposterior, lateral, and odontoid views) and cervical CT imaging[16,17]. On initial evaluation for odontoid fractures, plain films have been the first diagnostic test performed. However, CT imaging should be performed when there is suspicion of an odontoid fracture. CT imaging is generally much more sensitive for detecting fractures, defining the extent of pathology, and evaluating the surrounding soft tissue than plain films.
Decisions on the course of treatment for an odontoid fracture depend primarily on two factors: radiologic appearance/characteristics (type of odontoid fracture) and clinical status (presence or absence of neurological deficit)[18,19]. The most widely used classification system currently in practice was described by Anderson and D’Alonzo in which fractures were classified into three main types and can be further subcategorized as displaced or non-displaced[4]. A type 1 odontoid fracture involves an oblique fracture through the odontoid itself and is thought to be a manifestation of an avulsion of the attached alar ligament. This type is the least common of all odontoid fractures and is typically considered a stable fracture with a good rate of successful union because the fracture is located high enough that it does not cause instability[4]. A type II odontoid fracture involves the junction of odontoid process and the vertebral body of C2. These fractures make up the majority of all odontoid fractures. They are generally considered unstable with a high rate of non-union and are the most difficult to treat[4]. A type III odontoid fracture involves a fracture through the cancellous portion of the C2 body. These types of fractures are the second most common of the three odontoid fracture types, and are considered stable enough that external bracing is sufficient to achieve a high rate of union given the presence of large cancellous surfaces[4,18].
Rarely, however, type III odontoid fractures may require surgical attention when deemed unstable. Although displacement and/or dislocation of an odontoid fracture has been described in terms of translation or angulation, vertical displacement (distractive component) or even rotation as a factor in determining stability or adequacy of reduction has received little attention. It is known that the presence of atlantoaxial dislocation in type III odontoid fracture is unstable[20,21], and when there is complete disruption of the anterior atlantoaxial ligament, these injuries appear to be vertically unstable type III odontoid fractures, similar to the injury described in this report[22].
There are only a few reports of isolated unstable type III fractures where a distractive component was present and external traction bracing was deemed inapt warranting surgical management[9,10]. Jea et al[9] described the case of a 73-year-old female with a type III odontoid fracture associated with a significant distractive component following a MVA. On presentation, the patient was quadriplegic and had bilateral cranial nerve XI palsies. This patient underwent a C1-C2 fusion. Despite this treatment, the patient remained quadriplegic and ventilator-dependent. In a case series of three patients reported by Kirkpatrick et al[10], a 65-year-old female, 39-year-old female, and 29-year-old female all sustained type III odontoid fractures associated with unstable distractive components (at least 5 mm of vertical displacement was present) following a MVA. In the 39-year-old female, halo immobilization was attempted but, despite this, motion at the fracture site was noted; the distractive component was severe enough that the C1-C2 facet space oscillated with ventilation when viewed under fluoroscopy. All three patients underwent C1-C2 arthrodesis with transarticular screws and iliac crest bone graft. Two patients had permanent neurological deficits: at 27-mo follow-up, the 65-year-old patient had incomplete C1-C5 level quadriparesis, and at 10 mo, the 39-year-old patient had a C5 tetraplegia. The last patient regained full neurological function at 18 mo post-procedure.
To our knowledge, there are no reports of a C2 body fracture that possess both significant rotational and distractive components as was seen in our patient. These components likely resulted from the atypical fracture pattern seen in this patient; the fracture traversed the C2 vertebral body in a transverse manner. The rotational component in our patient was quite significant, as the left portion of the body caused some degree of narrowing of the spinal canal. Complications from purposely or inadvertently applying traction axially have not been readily described because longitudinal instability associated with odontoid fractures is rare[23]. But in fractures associated with a distractive component, halo traction is not ideal as there is instability secondary to circumferential injury so that traction could cause or worsen neurologic symptoms. Therefore, fractures with distractive and/or rotational components warrant surgical stabilization.
Transverse C2 body fractures with rotational and distractive components are unusual and highly unstable. Surgical stabilization should be considered for these types of fractures.