Published online Oct 18, 2013. doi: 10.5312/wjo.v4.i4.248
Revised: July 15, 2013
Accepted: September 4, 2013
Published online: October 18, 2013
Processing time: 165 Days and 19.7 Hours
AIM: To investigate the feasibility of a 6-wk progressive strength-training programme commenced shortly after hip fracture surgery in community-dwelling patients.
METHODS: This prospective, single-blinded cohort study evaluated 31 community-dwelling patients from four outpatient geriatric health centres aged 60 years or older, who started a 6-wk programme at a mean of 17.5 ± 5.7 d after hip fracture surgery. The intervention consisted primarily of progressive fractured knee-extension and bilateral leg press strength training (twice weekly), with relative loads commencing at 15 and increasing to 10 repetitions maximum (RM), with three sets in each session. The main measurements included progression in weight loads, hip fracture-related pain during training, maximal isometric knee-extension strength, new mobility score, the timed up and go test, the 6-min walk test and the 10-meter fast speed walk test, assessed before and after the programme.
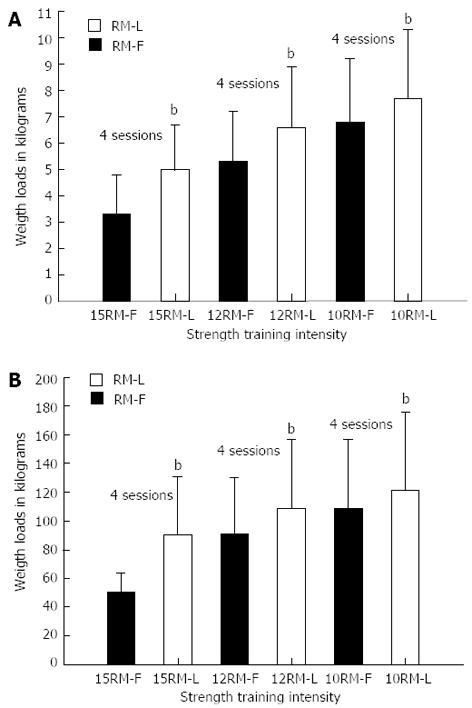
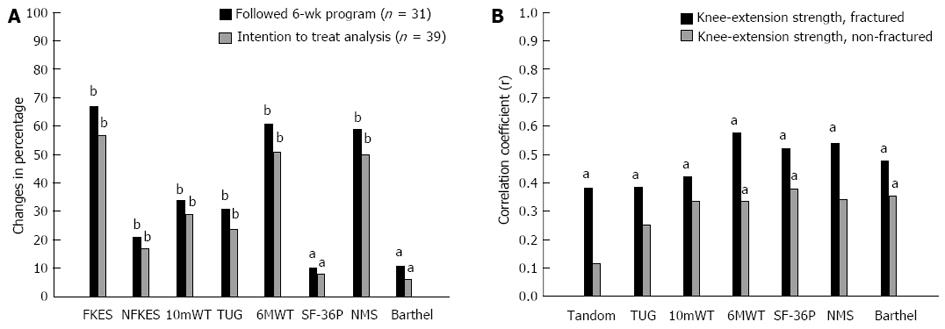
RESULTS: Weight loads in kilograms in the fractured limb knee-extension strength training increased from 3.3 ± 1.5 to 5.7 ± 1.7 and from 6.8 ± 2.4 to 7.7 ± 2.6, respectively, in the first and last 2 wk (P < 0.001). Correspondingly, the weight loads increased from 50.3 ± 1.9 to 90.8 ± 40 kg and from 108.9 ± 47.7 to 121.9 ± 54 kg in the bilateral leg press exercise (P < 0.001). Hip fracture-related pain was reduced, and large improvements were observed in the functional outcome measurements, e.g., the 6-min walk test improved from 200.6 ± 79.5 to 322.8 ± 68.5 m (P < 0.001). The fractured limb knee-extension strength deficit was reduced from 40% to 17%, compared with the non-fractured limb. Ten patients reported knee pain as a minor restricting factor during the last 10 RM knee-extension strength-training sessions, but with no significant influences on performance.
CONCLUSION: Progressive strength training, initiated shortly after hip fracture surgery, seems feasible and does not increase hip fracture-related pain. Progressive strength training resulted in improvement, although a strength deficit of 17% persisted in the fractured limb compared with the non-fractured limb.
Core tip: The recovery of strength and function in patients with hip fractures is an on-going challenge. We aimed to evaluate the feasibility of a 6-wk progressive lower limb strength-training programme. To our knowledge, this was the first study to implement such a program successfully in an outpatient geriatric setting within 2-3 wk after hip fracture surgery. Training loads, muscle strength and functional performances improved without an increase in hip fracture-related pain, which is considered new and important knowledge for all professionals aiming to improve the rehabilitation outcomes of patients with hip fractures.
- Citation: Overgaard J, Kristensen MT. Feasibility of progressive strength training shortly after hip fracture surgery. World J Orthop 2013; 4(4): 248-258
- URL: https://www.wjgnet.com/2218-5836/full/v4/i4/248.htm
- DOI: https://dx.doi.org/10.5312/wjo.v4.i4.248
Hip fractures are associated with poorer survival[1], a greater than 50% loss of fractured lower limb strength within a few week after surgery[2-4] and the return of only poor functional mobility within 4 mo[5]. Knee extensor muscle strength is an independent predictor of falls within 6 mo of hip fracture[6]. Thus, reducing strength deficits should be a high priority in rehabilitation, as the incidence of falls is higher with asymmetrical lower extremity power[7]. Some trials have suggested the benefits of exercise after hip fracture[8], but studies have most often commenced as extended programmes after standard physical therapy has ceased, 6 to 8 wk after fracture at the earliest[9-16]. To our knowledge, only one study has evaluated the effects of early 6-wk (median of 15 d post-surgery) strength training after hip fracture as an in-patient rehabilitation programme[3]. However, no similar studies have been conducted in community-dwelling geriatric patients with hip fractures or have succeeded in promoting the regaining of symmetrical lower limb muscle strength. In addition, most strength intervention studies have based their training intensity on the one repetition maximum (RM) level[3,10-12,15-17], which requires further calculations before use in clinical practice, as well as new one-RM measurements for the subsequent adjustment of training intensity. Such one-RM-based programmes challenge progressive exercise in comparison with, e.g., programmes that start with 12 repetitions and a 12-RM intensity, which in principal, allows physiotherapists to adjust weight loads after each set. That is, weight loads should be increased in the next set for a patient able to perform, e.g., 14 repetitions for such a programme to be called progressive. In summary, there is only limited knowledge regarding the feasibility and effects of a non-one-RM-based progressive strength-training programme commenced within a few wk after hip fracture surgery.
The primary purpose of this prospective cohort study was to evaluate the feasibility of a 15- to 10-RM programme, based on a 6-wk early progressive strength-training programme, after hip fracture. Feasibility was indicated if the absolute strength-training loads increased progressively and if hip fracture-related pain during training remained the same or decreased over time. The secondary purpose was to report functional adaptations, the details of specific weight loads and whether hip fracture-related pain influenced strength and functional testing.
Thirty-nine community-dwelling geriatric patients with hip fractures were included in this study (Table 1) and began the exercise programme at a mean of 17.5 ± 5.7 d after surgery. The types of surgery included hip pins (n = 3), screws (n = 10) and hemiarthroplasty (n = 10) for the 23 patients with intracapsular cervical femoral fractures, whereas the patients with extracapsular intertrochanteric fractures underwent surgery with dynamic hip screws (n = 8) or short intra-medullar hip screws (IMHS, n = 4). Four patients with subtrochanteric fractures all underwent surgery with long IMHS. All of the patients were cleared by the orthopaedic surgeon at the hospital for immediate weight bearing as tolerated on the operated limb, and with the exception of those with hemi-arthroplasty, the patients were under no other restrictions during rehabilitation. Patients with hemiarthroplasty were not allowed to perform > 90° flexion, adduction or internal rotation of the hip. Before inclusion, all of the patients followed a short in-hospital physical therapy programme without strength training, focused on the regaining of basic mobility activities[18,19], before being discharged to their own homes. Patients were recruited from four outpatient geriatric municipality health centres from September 2010 to August 2011. The inclusion criteria were as follows: age greater than or equal to 60 years; intra- or extracapsular hip fracture; no post-surgical restrictions for weight bearing; living in their own homes; and ability to walk independently, according to an indoor new mobility score[20,21] (NMS) ≥ 2 points. The exclusion criterion was as follows: adverse medical conditions, such as neurological impairment (e.g., history of stroke with residual hemiplegia) or uncontrolled cardiac diseases that could potentially influence the patient’s ability to participate in the programme. The ethics committee of the Sealand region (study no. SJ-145) and the Danish data protection agency approved this study. All of the patients provided written informed consent, according to the Declaration of Helsinki II.
| All | Dropout within6 wk, n = 8 | Followed 6-wkprogram, n = 31 | P value | |
| Age (yr) | 77.7 ± 8.7 | 77.2 ± 8.3 | 77.9 ± 9.0 | 0.8 |
| Women | 33 (85) | 7 (21) | 26 (79) | 1.0 |
| Men | 6 (15) | 1 (17) | 5 (83) | |
| Cervical femoral fracture | 23 (59) | 4 (17) | 19 (83) | 0.8 |
| Intertrochanteric fracture | 12 (31) | 3 (25) | 9 (75) | |
| Subtrochanteric fracture | 4 (10) | 1 (25) | 3 (75) | |
| New mobility score (0-9): | ||||
| Pre-fracture functional level | 9 (9-9) | 9 (8.5-9) | 9 (9-9) | 0.8 |
| Baseline functional level | 4 (3-4) | 4 (3-4) | 4 (3-4) | 0.9 |
| Barthel-20 (0-20) | 18 (17-20) | 8 (17-19.5) | 18 (17-20) | 0.9 |
| Balance, tandem test (0-30) | 30 (23-30) | 27 (24-30) | 30 (22-30) | 0.5 |
| Timed up and go test, seconds | 21.0 ± 7.2 | 22.4 ± 10 | 20.2 ± 6.0 | 0.4 |
| Ten-meter fast speed walk, m/s | 0.72 ± 0.22 | 0.65 ± 0.31 | 0.74 ± 0.19 | 0.3 |
| Six min walk test, meters | 198 ± 79 | 189 ± 80 | 201 ± 80 | 0.7 |
| Fractured, knee-extension strength, Nm/kg | 0.47 ± 0.16 | 0.39 ± 0.16 | 0.49 ± 0.16 | 0.1 |
| Non-fractured, knee- extension strength, Nm/kg | 0.79 ± 0.22 | 0.69 ± 0.29 | 0.81 ± 0.28 | 0.2 |
The patients were asked to follow a standardised 6-wk rehabilitation programme with sessions twice weekly (12 sessions in total), which included progressive lower limb strength training. Before the first training session and after the last training session, all of the patients performed the following objective examinations: the timed up-and-go (TUG) test[22]; the 10-m fast speed walk test (10mWT)[23]; the tandem balance test[24]; the 6-min walk test (6MWT)[25]; and the maximal isometric knee-extension strength test for each limb. The pre-fracture functional level was assessed using the questionnaire of the modified[26], functionally validated[27] and reliable[21] NMS (0-9 points, a score of 9 indicating a fully independent pre-fracture walk level)[20] and activities of daily living, using the Barthel-20[28]. Health-related quality of life was assessed using the 36-item short form health survey (SF-36) and was reported as SF-36P (physical) and SF-36M (mental)[29]. The patients were instructed to take their prescribed pain medication before the testing and training.
Physiotherapists involved in the testing of the patients before and after the rehabilitation were blinded to the patients’ participation and progress during the 6-wk rehabilitation programme, and the physiotherapists did not supervise training the sessions.
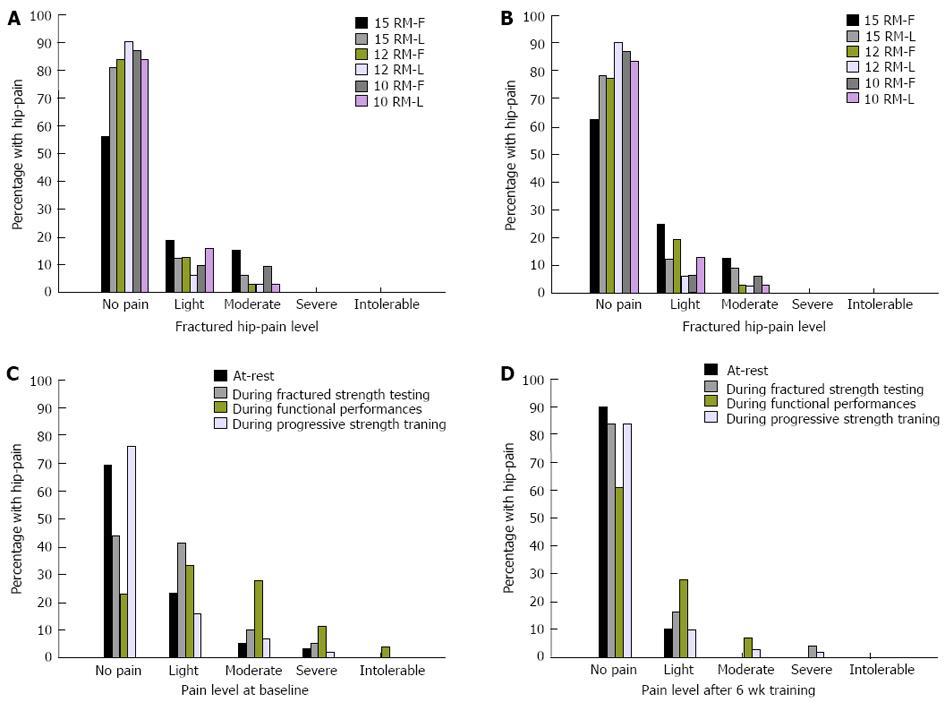
Hip fracture-related pain was measured with a 5-point verbal ranking scale (VRS) (0 = none, 1 = light, 2 = moderate, 3 = severe, 4 = intolerable pain) during all of the strength and performance testing, as well as during all of the strength-training sessions (patients were asked immediately after). The VRS has proved most appropriate for measuring pain in patients with hip fractures[30] and has been used in previous hip fracture studies[2,31,32].
During each strength-training session, the patients were asked about any factors restricting their performance.
The TUG, performed as fast as safely possible, has proved highly reliable in patients with hip fractures[33] when using a standardised four-wheeled rollator[34] and selecting the best of three timed trials[35]. Accordingly, as all of the patients used some kind of walking aid, a standardised four-wheeled rollator was used for all of the walk tests (TUG, 10mWT and 6MWT), both at baseline and at follow-up testing. The best of three timed trials was used for the TUG (performed as previously described)[34], the 10mWT and the tandem balance test (no walking aid used), whereas one timed trial was used for the 6MWT.
Fast speed walking was measured with the 10mWT[23]. Patients were instructed to “walk as fast as safely possible without running” from a standing position, starting behind a line drawn on floor. A stopwatch was started on the command “3-2-1-GO” and was then stopped when the patient’s leading foot crossed a line 10 m away. The results are reported in meters walked per second (m/s).
Static balance was assessed with the tandem test[24] with a score from 0 to 30 points (a score of 30 points indicating no balance problems). The first position was standing with the feet together, the second was placing the feet in semi-tandem, and the last position was setting the feet in a full tandem position. The time was measured with a stopwatch, and up to 10 points (one per second) were assigned for maintaining balance in each of the three positions.
Maximal isometric knee-extension strength was assessed for both limbs with a fixated hand-held dynamometer[36] (Power Track II Commander). The patients were seated on an examination couch with their arms crossed (as in a previous study[37], personnel communication with the first author), their knees at a 90° angle and their upper limb fixed with a strap to the examination couch during testing. The transducer (placed 5 cm above the lateral malleoli) was positioned under a fixation belt that was fastened to the examination couch. After familiarisation with the procedure, the patients performed five voluntary isometric knee extensions for each limb (non-fractured limb first) with strong verbal encouragement, separated by a minimum of a 30-s pause. Maximal isometric strength was expressed in Nm/kg and was derived from the units of force in newtons (N) multiplied by the corresponding lever arm (distance from lateral epicondyle of the femur to the transducer) measured in meters (m), divided by the weight (kg) of the patient[37].
The 6MWT was performed according to recommendations of the American Thoracic Society[25], using a 30-m course with a cone marking each end. The patients were instructed to walk as far as possible, and Borg dyspnoea and fatigue levels[38] were recorded immediately after finishing. No practice trial was conducted, but the patients performed the other objective outcome measurements before the 6MWT.
The patients who entered the programme were of different ages (range, 61-96 years) and pre-fracture functional levels (NMS, 6-9) and therefore exhibited different functional levels at start of the programme. Accordingly, walking and balance exercises were chosen and progressed on an individual level to ensure that each exercise was conducted with the same intensity for all of the patients. The exercises began with warm-up on a stationary bicycle (intensity according to the Borg 10) for 10 min and were followed by functional exercises focused on improving walking forward, backward and sideways and stair climbing with the maximal tolerable weight bearing on the operated limb, with or without the use of walking aids, for 15 min.
The balance training was conducted for approximately 10 min with the patient standing with both legs on the floor and on different surfaces, e.g., an Airex pillow/mattress, an ankle disk or a trampoline, with or without support.
The progressive strength training included unilateral (fractured limb) knee extension (Figure 1A) and bilateral leg presses (Figure 1B). For each exercise, three sets of approximately 15 repetitions with a relative weight load of 15 RM were performed for 2 wk (four sessions). This period was followed by 2 wk with three sets of 12 repetitions (12 RM) and 2 wk with three sets of 10 repetitions (10 RM). To determine the relative weight load, the supervising physiotherapist adjusted the weight load, so the patient reached fatigue at the respective RM level. Accordingly, the weight loads were adjusted after each of the three training sets in each of the 12 sessions if the patient was able to perform more than the planned repetitions, to ensure training at the respective RM level. The reduction in the number of repetitions from 15 to 12 to 10 during the 6-wk strength-training programme was followed by a corresponding increase in intensity from 15 to 12 to 10 RM. The largest difference in kilograms between the starting point and endpoint was used in the final analysis. The total exercise programme lasted approximately 60 min per session.
The fractured limb knee-extension strength training was performed with the patient seated on an examination couch with a 90° hip and knee angle. In the seated position, the patient was instructed to grasp the edge of the examination couch with his or her hands to assure a standardised position. The patient was connected to a weight load system with a strap around the ankle, and a successful single repetition was defined as movement from the 90° knee angle to as close as possible to a maximal knee extension (Figure 1A).
The bilateral leg press strength training was started with maximum allowed flexion in the hip (90° for patients who underwent surgery with hemi- or total arthroplasty) and the knee to a full possible knee extension, and the patients were instructed to press equally with both limbs (Figure 1B).
Strong verbal encouragement was given during all of the strength exercises, and the patients were instructed to continue each set until failure/fatigue. The patients were instructed not to perform additional training during the 6-wk programme.
Descriptive statistics were utilised for baseline characteristics. We used Student’s t test for normally distributed data, the Mann Whitney U test for non-normally distributed data and the χ2 test or Fisher’s exact test for categorical data to evaluate differences between patients and dropouts over the 6-wk programme. We used the paired t test and Wilcoxon’s test to examine changes from baseline to 6 wk, whereas Pearson’s product moment or Spearman’s rho was used for correlation analyses of normally and non-normally distributed data, respectively. Additionally, intention-to-treat analysis was performed, including dropouts with baseline data. The data are presented as mean ± SD when normally distributed and are otherwise presented as medians (25%-75% quartiles) or as numbers with percentages. All of the data analyses were conducted using SPSS, version 19.0. The level of significance was set at P less than 0.05.
Eight of the 39 patients included in this study did not complete the 6-wk programme for the following reasons: back pain (n = 2, already present before study inclusion); second surgeries (n = 2); withdrawal of consent (n = 2); and death (n = 2). Both patients who underwent a second operation exhibited dislocated intracapsular fractures (classified as Garden 3 and 4, respectively). One of these patients did not start the program due to luxation of a hemi-arthroplasty in her own home, whereas the other patient, who underwent surgery with hip pins, participated in three training sessions. Only three out of the eight dropout patients commenced the training programme after baseline testing, of whom one underwent a second surgery (hip pins), one died within the first 2 wk, and one withdrew consent within 4 wk of beginning training due to an acute illness of the spouse. However, those who did not start (n = 5) or complete the training programme exhibited similar demographic and baseline data, compared with the 31 patients who completed the strength-training programme (Table 1), and none of the patients who dropped out cited reasons specific to the programme itself.
Weight loads for the 15, 12 and 10 RM strength training for fractured limb knee extension (Figure 2A) and bilateral leg press (Figure 2B) training increased progressively (P < 0.001) from 12% to 81% (Table 2). At the same time, hip fracture-related pain was reduced (Figure 3 A-B). Adherence to the programme was noteworthy, with 95% of possible sessions completed (352 out of 372 possible).
| Baseline | 6 wk | Percentagechange | P value | |
| New mobility score (0-9) | 3.7 ± 1.1 | 5.9 ± 1.6 | 59 | < 0.001 |
| Barthel (0-20) | 18 (17-20) | 20 (18-20) | 11 | < 0.001 |
| Balance, tandem test (0-30) | 30 (22-30) | 30 (29-30) | 0 | < 0.001 |
| Timed up and go test, seconds | 20.2 ± 6.0 | 13.9 ± 3.2 | -31 | < 0.001 |
| Ten-meter fast speed walk, m/s | 0.74 ± 0.19 | 0.99 ± 0.2 | 34 | < 0.001 |
| Six-min walk, meters | 200.6 ± 79.5 | 322.8 ± 68.5 | 61 | < 0.001 |
| Short-form 36, physical component summary | 33.8 ± 9 | 37.1 ± 8 | 10 | 0.035 |
| Short-form 36, mental component summary | 45.5 ± 11.1 | 46.4 ± 9.6 | 2 | 0.639 |
| Fractured knee-extension strength, Nm/kg | 0.49 ± 0.16 | 0.82 ± 0.32 | 67 | < 0.001 |
| Non-fractured knee-extension strength, Nm/kg | 0.82 ± 0.28 | 0.99 ± 0.34 | 21 | < 0.001 |
| Weight loads in kilograms (kg), fractured knee-extension: | First session | Last session | ||
| 15 RM sessions, n: 34 | 3.3 ± 1.5 | 5 ± 1.7 | 52 | < 0.001 |
| 12 RM sessions, n: 32 | 5.3 ± 1.9 | 6.6 ± 2.3 | 25 | < 0.001 |
| 10 RM sessions, n: 31 | 6.8 ± 2.4 | 7.7 ± 2.6 | 13 | < 0.001 |
| Weight loads (kg), bilateral leg press: | ||||
| 15 RM training sessions | 50.3 ± 13.4 | 90.8 ± 40.0 | 81 | < 0.001 |
| 12 RM training sessions | 91.2 ± 38.8 | 108.9 ± 47.7 | 19 | < 0.001 |
| 10 RM training sessions | 108.9 ± 47.7 | 121.9 ± 54.0 | 12 | < 0.001 |
Of some concern, 10 patients reported knee pain as a minor restricting factor in the last 10 RM session of the fractured limb in the knee extension strength training. Nonetheless, these 10 patients exhibited similar improvements in all strength and functional performances (P > 0.1) and walked a greater distance (P = 0.04) in the 6MWT at follow-up compared with the 21 reporting no knee-pain. The number of patients who expressed knee pain as a minor restricting factor was unchanged (n = 4) during the first and last leg press training session.
Regarding hip pain, only six out of the 39 patients (15%) experienced more than light pain (VRS > 1) in the fractured hip during the baseline knee-extension strength test, but the performances of these patients did not differ from those reporting light or no pain (P = 0.9). Eight patients reported more than light hip pain during the first 15-RM strength-training session (Figure 3C), but their performances did not differ from those reporting none (n = 18) to light pain (n = 6). Hip fracture-related pain was in general very rare in the subsequent strength-training and testing sessions and appeared unrelated to performance (Figure 3D). In contrast, hip fracture-related pain was present in 26% of the TUG, 41% of the 10mWT and 63% of the 6MWT performances at baseline testing (Figure 3C). No significant influence was observed for the TUG or fast speed walking tests (P > 0.1), whereas patients reporting more than light hip fracture-related pain during the baseline 6MWT actually walked a significantly shorter distance of 174 m, compared with 233 m for those with less pain (P = 0.02), and very few reported more than light pain at the 6-wk follow-up testing (Figure 3D).
The patients who completed the 6-wk programme exhibited significant improvements (P < 0.001) in the objective walk measurements, ranging from -31% for the TUG to 61% for the 6MWT (Table 2, Figure 4A). Twenty-six of the 31 patients (84%) exhibited improvements of more than 50 m (range 60-278 m) for the 6MWT, while 81% improved by more than 0.1 m/s for the 10mWT. The maximal isometric knee-extension strength improved (P < 0.001) in both the fractured and non-fractured limbs, by 67% and 21%, respectively. The strength deficit in the fractured limb decreased after rehabilitation, from an average of 40% at baseline to 17% at the study’s conclusion, compared with the non-fractured limb. In addition, the Barthel-20 and the NMS improved (P < 0.001) by 11% and 59%, respectively, whereas the SF-36P improved by 10% (Table 2, Figure 4A). Further analysis of the correlations among all of the different outcome variables after the 6-wk programme revealed that the maximal isometric fractured limb knee-extension strength was significantly correlated with all of the variables (except for the SF-36M) and was superior to that of the non-fractured limb (Figure 4B).
A conservative intention-to-treat analysis for all 39 patients, including baseline data carried forward for the eight dropouts, demonstrated similar 6-wk functional improvements, compared with those patients who completed the programme (Figure 4A).
To our knowledge, this was the first physiotherapy programme including progressive strength training for community-dwelling older patients that commenced within a few wk after hip fracture surgery in an outpatient geriatric health centre. We determined that 6 wk of lower limb strength training in general seems feasible (weight loads increased, and only three patients (9%) who started the programme were not able to complete it), and we observed large improvements in objective and patient-reported outcome measurements, including a conservative intention-to-treat-analysis. Systematic registration of hip fracture-related pain revealed reduced pain levels during strength training, indicating that most of the patients could tolerate the progressive strength-training programme when commenced within 2-3 wk after hip fracture surgery, without hip pain interfering.
Nonetheless, an unexpected and increasing number of patients reported knee pain as a minor restricting factor during the fractured knee-extension strength training. Importantly, no dropouts and improvements similar to those not experiencing this problem were observed. Additionally, knee-extension strength training is recommended nationally for subjects with mild knee osteoarthritis in the study country. In addition, clinicians are provided with the details of specific weight loads used from the start to the end of the 15- to 10-RM sessions for fractured limb knee-extension and bilateral leg press training.
The mean absolute weight load increased by ≥ 52%, 19% and 12% within the 15, 12 and 10 RM knee-extension and leg press sessions, respectively, with an accompanying decrease in hip fracture-related pain. These increases emphasise the importance of adjusting weight loads on a set-to-set basis, as reported in previous studies of patients after knee arthroplasty[37], for the strength training to be progressive, compared to re-evaluation every 2-wk[3] or over a longer interval[15,16], using a one-RM estimation for the training.
Hip fracture-related pain is common and seems to compromise functioning in the short and long terms after hip fracture surgery[31,32,39,40]. Critics might therefore argue that it is not possible to implement our strength programme due to pain problems. We found that up to 25% of patients experienced moderate to severe hip pain during the first 15-RM knee-extension training sessions, but the percentage dropped to only 6% reporting moderate pain at the last 15-RM session and to 0% at the last 10-RM session after 6 wk. Similarly, only 4% of patients reported moderate hip pain as the highest score at the last leg press session. To complete the “pain” picture, up to 63% (6MWT) of patients experienced moderate to intolerable pain during the objective outcome measurements at baseline testing. Nonetheless, hip pain “only” influenced the baseline 6MWT performances and did not compromise performance after 6 wk of training. Thus, it seems possible to increase weight loads progressively; patients might experience a decrease in hip pain within an early 6-wk strength-training programme
Positively, the pre-defined measurement of hip fracture-related pain was of minor influence, but we did find that a number of patients reported knee pain as a minor restricting factor in their fractured knee-extension strength training as intensity increased, which was likely related to patella femoral osteoarthritis. Although no dropouts and similar improvements were observed for these patients, these reports of knee pain should be noted. Unfortunately, we did not monitor whether these patients reduced their pain medications over the 6-wk programme, nor did we assess information about former or present knee problems, e.g., knee osteoarthritis, which could potentially have explained these changes. We therefore recommend the leg press as a more appropriate exercise for patients who report knee pain, as fewer patients reported pain during this exercise, compared with the knee-extension exercise.
The maximal isometric knee-extension strength of the fractured limb increased by a mean of 67%, compared with 21% for the non-fractured limb, but a mean fractured strength deficit of 17% persisted at the 6-wk follow-up. It is possible that initiating a strength-training programme even earlier could have reduced this deficit further, which should be examined in the future. Nonetheless, these results were better than the previously reported leg extensor power deficit of 26% after another early 6-wk strength programme that, in addition, required standard physical therapy on all week days[3]. Furthermore, improvements in our study were much larger than those reported (11%) for fractured knee-extension torque in older patients with hip fractures following a late (mean of 1587 ± 736 d after fracture) 12-wk intensive strength-power programme[41]. In the present study, although not eliminated, the fractured limb strength deficit was reduced by 23% and reached the non-fractured baseline level. Thus, if fractured single-limb leg press training had been chosen, instead of bilateral training, this difference might have been even further diminished. This relationship should be given high priority, as the importance of reducing asymmetric strength deficits after hip fracture is further emphasised; the fractured knee-extension strength was correlated with all of the functional assessments at the follow-up testing and was superior to that of the non-fractured limb. Similar associations have been reported at earlier time points after hip fracture surgery[2].
Performance in the TUG, the 10mWT and the 6MWT improved by a mean of 31%-61%, whereas no improvement was observed for the median tandem balance values. The latter results were probably related to a ceiling effect already present at baseline, which indicates that the tandem test is probably not suitable for measuring progress in balance within this patient group.
Natural recovery and/or less hip pain during follow-up testing probably should be credited to some of the large improvements observed in our study, particularly with regard to knee-extension strength and the 6MWT. Moreover, our patient group walked a mean of 323 m, compared with a mean of 297 m in a Norwegian study that examined patients after ceasing standard rehabilitation and after an additional 3 mo of rehabilitation, including strength training twice weekly plus home training once weekly[15]. In addition, 84% of our patients improved by more than 50 m, which has been considered a meaningful change for the 6MWT in older adults[42] and in patients with hip fractures (> 54 m)[43].
Different opinions exist regarding what should be considered a meaningful improvement in gait speed after hip fracture, ranging from 0.1[44] to 0.26 m/s for a substantial meaningful improvement[45]. We have reported improved gait speed performances, although obtained at the same[3] or at a longer interval post-surgery compared with other studies[11,15], and we have demonstrated an average improvement of 0.25 m/s. More than 80% of the patients improved by more than 0.1 m/s. Nevertheless, the patients did not reach the maximum gait speed level considered “normal” for older people in their 70 s[46]. The improvements in the TUG exceeded the standard error of measurement (2.2 s), but only two patients took less than 10 s at follow-up - a time considered normal for older individuals[33].
The influence of different walking aids on functional performance has been reported for walking velocity[47], the 2-min walk test[48] and for the TUG[34,49]. Thus, the effect of rehabilitation could be overestimated if the same walking aid were not used during pre- and post-rehabilitation testing[34]. All patients with hip fractures use some type of walking aid in the early period after the fracture[50,51], and they commonly change to a less supportive aid, or they eliminate walking aids altogether after rehabilitation[43,50].
Thus, functional improvements beyond natural recovery might more truly be related to the rehabilitation programme in the present study, using a standardised functional walking aid pre- and post-testing.
Large average improvements were observed for the NMS (59%), compared with the Barthel-20 and the SF-36. However, only three patients reached their pre-fracture NMS functional levels. The ceiling effect seen for the Barthel-20 at baseline (median of 18, IQR 17-20) was even more obvious in the follow-up testing, as reported in two earlier studies[3,15]. Thus, as for the tandem balance test, the Barthel-20 index cannot be recommended for measuring progress in similar groups of patients with hip fractures.
Although significant and correlated with measures of knee-extension strength for both limbs upon follow-up, only small improvements (10%) in self-rated health (SF-36P) were reported, whereas no improvement was observed for the SF-36M. These results might be related to the patients, to some extent, basing their self-rated health on their daily lives and function pre-fracture - a level not attained after the 6-wk programme. Similarly, a “later” 3-mo hip fracture intervention programme reported no effect on self-rated health measurements[15].
Functional improvements should be considered in light of the non-randomised design, the level of hip fracture-related pain upon baseline testing and the natural recovery over this early time period after hip fracture surgery. Thus, although we eliminated the potential influence of walking aids on the observed functional improvements, we do not know the exact effect of the progressive strength-training programme. Additionally, the included patients exhibited high pre-fracture functional and cognitive levels, which thus restrict our findings to patients with these characteristics. This limitation is, however, a common problem for research in this patient group, and our expectation is that patients with lower levels of functioning and cognition would also benefit from the programme, which was seen when patients with dementia were provided with an appropriate rehabilitation programme[52]. Another limitation was the consumption of pain medication before testing and training, as well as former knee problems, which were not monitored or recorded.
One strength of the study was the systematic recording of hip fracture-related pain, in addition to other factors that restricted the progressive strength training. Another strength regarding the large improvements seen for both objective and subjective measurements was the blinding of the physiotherapists who conducted all of the baseline and follow-up testing to the progress and participation in the training programme. Finally, although this trial was not randomised, we included a conservative intention-to-treat analysis, which also demonstrated significant improvements for all of the outcome measurements.
In conclusion, this study has demonstrated that progressive strength training, commenced early after hip fracture surgery in community-dwelling older patients, seems feasible; the weight loads increased throughout the study, and hip fracture-related pain during training decreased. Furthermore, the fractured limb strength deficit was reduced, and functional performances improved. That a growing number of patients reported knee pain, although such pain did not influence training or performance, should be considered in clinical practice and in future strength-training studies. Studies focused on the full recovery of function and strength should be conducted using a randomised, controlled design.
We would like to thank the physiotherapists from the Vordingborg, Ringsted, Naestved and Lolland municipalities for their assistance in the data collection. Furthermore, we thank Adrianne E Jones, Emeritus Professor of Human Exercise Metabolism, and Peter RM Jones, Emeritus Professor of Human Functional Anatomy, for their grammatical contributions and Senior Researcher Thomas Bandholm, PhD, for his useful comments on the manuscript.
Patients with hip fracture experience more than 50% knee-extension strength deficits in the fractured limb, compared with the non-fractured limb, shortly after surgery. To the authors’ knowledge, no study has succeeded in eliminating this strength deficit with a rehabilitation programme.
Early intervention after surgery is considered crucial for patients with hip fractures potentially to regain their pre-fracture functional levels.
The major difference of this strength training study, compared with previous studies, was the progressive “on a set-to-set” approach. That is, weight loads were adjusted in the next set in the same session if the patient performed more than the planned number of repetitions, compared with adjustments on a weekly or longer-interval basis.
The strength-training programme seems feasible, as weight loads increased and hip fracture-related pain decreased. The effects of the programme require confirmation in a randomised, controlled trial.
The feasibility of a progressive strength-training programme: If the absolute strength training loads increased progressively and if, at the same time, hip fracture-related pain during training remained the same or if it decreased over time. Progressiveness of the strength-training programme: The reduction in the number of repetitions from 15 to 12 to 10 during the 6-wk strength-training programme is followed by a corresponding increase in the intensity from 15 to 12 to 10 repetitions maximum.
The aim of authors is to investigate the feasibility of a 6-wk progressive strength-training programme commenced shortly after hip fracture.
P- Reviewers Emara KM, Sebestyén A S- Editor Gou SX L- Editor A E- Editor Wu HL
| 1. | Vestergaard P, Rejnmark L, Mosekilde L. Has mortality after a hip fracture increased? J Am Geriatr Soc. 2007;55:1720-1726. [PubMed] |
| 2. | Kristensen MT, Bandholm T, Bencke J, Ekdahl C, Kehlet H. Knee-extension strength, postural control and function are related to fracture type and thigh edema in patients with hip fracture. Clin Biomech (Bristol, Avon). 2009;24:218-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Mitchell SL, Stott DJ, Martin BJ, Grant SJ. Randomized controlled trial of quadriceps training after proximal femoral fracture. Clin Rehabil. 2001;15:282-290. [PubMed] |
| 4. | Sherrington C, Lord SR, Herbert RD. A randomised trial of weight-bearing versus non-weight-bearing exercise for improving physical ability in inpatients after hip fracture. Aust J Physiother. 2003;49:15-22. [PubMed] |
| 5. | Kristensen MT. Factors affecting functional prognosis of patients with hip fracture. Eur J Phys Rehabil Med. 2011;47:257-264. [PubMed] |
| 6. | Yau DT, Chung RC, Pang MY. Knee muscle strength and visual acuity are the most important modifiable predictors of falls in patients after hip fracture surgery: a prospective study. Calcif Tissue Int. 2013;92:287-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Portegijs E, Sipilä S, Rantanen T, Lamb SE. Leg extension power deficit and mobility limitation in women recovering from hip fracture. Am J Phys Med Rehabil. 2008;87:363-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Sherrington C, Tiedemann A, Cameron I. Physical exercise after hip fracture: an evidence overview. Eur J Phys Rehabil Med. 2011;47:297-307. [PubMed] |
| 9. | Sherrington C, Lord SR, Herbert RD. A randomized controlled trial of weight-bearing versus non-weight-bearing exercise for improving physical ability after usual care for hip fracture. Arch Phys Med Rehabil. 2004;85:710-716. [PubMed] |
| 10. | Binder EF, Brown M, Sinacore DR, Steger-May K, Yarasheski KE, Schechtman KB. Effects of extended outpatient rehabilitation after hip fracture: a randomized controlled trial. JAMA. 2004;292:837-846. [PubMed] |
| 11. | Hauer K, Specht N, Schuler M, Bärtsch P, Oster P. Intensive physical training in geriatric patients after severe falls and hip surgery. Age Ageing. 2002;31:49-57. [PubMed] |
| 12. | Host HH, Sinacore DR, Bohnert KL, Steger-May K, Brown M, Binder EF. Training-induced strength and functional adaptations after hip fracture. Phys Ther. 2007;87:292-303. [PubMed] |
| 13. | Mangione KK, Craik RL, Tomlinson SS, Palombaro KM. Can elderly patients who have had a hip fracture perform moderate- to high-intensity exercise at home? Phys Ther. 2005;85:727-739. [PubMed] |
| 14. | Mangione KK, Craik RL, Palombaro KM, Tomlinson SS, Hofmann MT. Home-based leg-strengthening exercise improves function 1 year after hip fracture: a randomized controlled study. J Am Geriatr Soc. 2010;58:1911-1917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 15. | Sylliaas H, Brovold T, Wyller TB, Bergland A. Progressive strength training in older patients after hip fracture: a randomised controlled trial. Age Ageing. 2011;40:221-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 16. | Sylliaas H, Brovold T, Wyller TB, Bergland A. Prolonged strength training in older patients after hip fracture: a randomised controlled trial. Age Ageing. 2012;41:206-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Singh NA, Quine S, Clemson LM, Williams EJ, Williamson DA, Stavrinos TM, Grady JN, Perry TJ, Lloyd BD, Smith EU. Effects of high-intensity progressive resistance training and targeted multidisciplinary treatment of frailty on mortality and nursing home admissions after hip fracture: a randomized controlled trial. J Am Med Dir Assoc. 2012;13:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 221] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 18. | Foss NB, Kristensen MT, Kehlet H. Prediction of postoperative morbidity, mortality and rehabilitation in hip fracture patients: the cumulated ambulation score. Clin Rehabil. 2006;20:701-708. [PubMed] |
| 19. | Kristensen MT, Andersen L, Bech-Jensen R, Moos M, Hovmand B, Ekdahl C, Kehlet H. High intertester reliability of the cumulated ambulation score for the evaluation of basic mobility in patients with hip fracture. Clin Rehabil. 2009;23:1116-1123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Parker MJ, Palmer CR. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br. 1993;75:797-798. [PubMed] |
| 21. | Kristensen MT, Bandholm T, Foss NB, Ekdahl C, Kehlet H. High inter-tester reliability of the new mobility score in patients with hip fracture. J Rehabil Med. 2008;40:589-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 22. | Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142-148. [PubMed] |
| 23. | Watson M. Refining the ten-metre walking test for use with neurologically impaired people. Physiotherap. 2002;88:386-397. |
| 24. | Rossiter-Fornoff JE, Wolf SL, Wolfson LI, Buchner DM. A cross-sectional validation study of the FICSIT common data base static balance measures. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Gerontol A Biol Sci Med Sci. 1995;50:M291-M297. [PubMed] |
| 25. | ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111-117. [PubMed] |
| 26. | Kristensen MT, Kehlet H. Most patients regain prefracture basic mobility after hip fracture surgery in a fast-track programme. Dan Med J. 2012;59:A4447. [PubMed] |
| 27. | Kristensen MT, Foss NB, Ekdahl C, Kehlet H. Prefracture functional level evaluated by the New Mobility Score predicts in-hospital outcome after hip fracture surgery. Acta Orthop. 2010;81:296-302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 121] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 28. | Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud. 1988;10:61-63. [PubMed] |
| 29. | Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-483. [PubMed] |
| 30. | Leino KA, Kuusniemi KS, Lertola KK, Olkkola KT. Comparison of four pain scales in patients with hip fracture or other lower limb trauma. Acta Anaesthesiol Scand. 2011;55:495-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 31. | Kristensen MT. Hip fracture-related pain strongly influences functional performance of patients with an intertrochanteric fracture upon discharge from the hospital. PMR. 2013;5:135-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 32. | Foss NB, Kristensen MT, Palm H, Kehlet H. Postoperative pain after hip fracture is procedure specific. Br J Anaesth. 2009;102:111-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 73] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 33. | Kristensen MT, Henriksen S, Stie SB, Bandholm T. Relative and absolute intertester reliability of the timed up and go test to quantify functional mobility in patients with hip fracture. J Am Geriatr Soc. 2011;59:565-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 34. | Kristensen MT, Bandholm T, Holm B, Ekdahl C, Kehlet H. Timed up & go test score in patients with hip fracture is related to the type of walking aid. Arch Phys Med Rehabil. 2009;90:1760-1765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 35. | Kristensen MT, Ekdahl C, Kehlet H, Bandholm T. How many trials are needed to achieve performance stability of the Timed Up & Go test in patients with hip fracture? Arch Phys Med Rehabil. 2010;91:885-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 36. | Roy MA, Doherty TJ. Reliability of hand-held dynamometry in assessment of knee extensor strength after hip fracture. Am J Phys Med Rehabil. 2004;83:813-818. [PubMed] |
| 37. | Jakobsen TL, Husted H, Kehlet H, Bandholm T. Progressive strength training (10 RM) commenced immediately after fast-track total knee arthroplasty: is it feasible? Disabil Rehabil. 2012;34:1034-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 38. | Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med. 1970;2:92-98. [PubMed] |
| 39. | Lamb SE, Morse RE, Evans JG. Mobility after proximal femoral fracture: the relevance of leg extensor power, postural sway and other factors. Age Ageing. 1995;24:308-314. [PubMed] |
| 40. | Morrison RS, Magaziner J, McLaughlin MA, Orosz G, Silberzweig SB, Koval KJ, Siu AL. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103:303-311. [PubMed] |
| 41. | Portegijs E, Kallinen M, Rantanen T, Heinonen A, Sihvonen S, Alen M, Kiviranta I, Sipilä S. Effects of resistance training on lower-extremity impairments in older people with hip fracture. Arch Phys Med Rehabil. 2008;89:1667-1674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 42. | Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54:743-749. [PubMed] |
| 43. | Latham NK, Mehta V, Nguyen AM, Jette AM, Olarsch S, Papanicolaou D, Chandler J. Performance-based or self-report measures of physical function: which should be used in clinical trials of hip fracture patients? Arch Phys Med Rehabil. 2008;89:2146-2155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 125] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 44. | Palombaro KM, Craik RL, Mangione KK, Tomlinson JD. Determining meaningful changes in gait speed after hip fracture. Phys Ther. 2006;86:809-816. [PubMed] |
| 45. | Alley DE, Hicks GE, Shardell M, Hawkes W, Miller R, Craik RL, Mangione KK, Orwig D, Hochberg M, Resnick B. Meaningful improvement in gait speed in hip fracture recovery. J Am Geriatr Soc. 2011;59:1650-1657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 46. | Bohannon RW. Comfortable and maximum walking speed of adults aged 20-79 years: reference values and determinants. Age Ageing. 1997;26:15-19. [PubMed] |
| 47. | Smidt GL, Mommens MA. System of reporting and comparing influence of ambulatory aids on gait. Phys Ther. 1980;60:551-558. [PubMed] |
| 48. | Foley MP, Prax B, Crowell R, Boone T. Effects of assistive devices on cardiorespiratory demands in older adults. Phys Ther. 1996;76:1313-1319. [PubMed] |
| 49. | Kristensen MT, Foss NB, Kehlet H. Factors with independent influence on the ‘timed up and go’ test in patients with hip fracture. Physiother Res Int. 2009;14:30-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 50. | Ingemarsson AH, Frändin K, Mellström D, Möller M. Walking ability and activity level after hip fracture in the elderly--a follow-up. J Rehabil Med. 2003;35:76-83. [PubMed] |