Published online Aug 18, 2012. doi: 10.5312/wjo.v3.i8.122
Revised: July 1, 2012
Accepted: August 7, 2012
Published online: August 18, 2012
Instability following total hip arthroplasty (THA) is an unfortunately frequent and serious problem that requires thorough evaluation and preoperative planning before surgical intervention. Prevention through optimal index surgery is of great importance, as the management of an unstable THA is challenging even for an experienced joints surgeon. However, even after well-planned surgery, a significant incidence of recurrent instability still exists. Non-operative management is often successful if the components are well-fixed and correctly positioned in the absence of neurocognitive disorders. If conservative management fails, surgical options include revision of malpositioned components; exchange of modular components such as the femoral head and acetabular liner; bipolar arthroplasty; tripolar arthroplasty; use of a larger femoral head; use of a constrained liner; soft tissue reinforcement and advancement of the greater trochanter.
- Citation: Werner BC, Brown TE. Instability after total hip arthroplasty. World J Orthop 2012; 3(8): 122-130
- URL: https://www.wjgnet.com/2218-5836/full/v3/i8/122.htm
- DOI: https://dx.doi.org/10.5312/wjo.v3.i8.122
Dislocation following total hip arthroplasty (THA) is a significant and unfortunately common complication. A landmark review in 1982 by Woo and Morrey of over 10 000 primary THAs reported a dislocation rate of 3.2%[1]. Other studies have reported dislocation rates of 0.3% to 10% for primary THAs and up to 28% for revision THAs[2-14]. The risk of dislocation is influenced by patient factors such as age, sex, previous surgery, and cognitive or neurologic disorders as well as surgical factors, including surgical approach, choice of implant, soft tissue and surgeon experience[13-15]. Although most dislocations after THA are isolated events and can be managed non-operatively, some patients will require surgical intervention to manage or prevent recurrent instability[7,16,17]. A thorough understanding of the etiology of dislocations, evaluation of an unstable THA, and appropriate management of such instability is necessary to ensure optimum outcomes for patients.
Instability is one of the most common complications of THA[1,7,16]. Determining the true incidence and prevalence of postoperative dislocation is challenging, as there are a variety of patient, surgical and implant factors, which compound the fact that most published reports on the topic are from high volume medical centers, which excludes community practices[14]. Most dislocations occur within the first 3 mo following surgery. The literature suggests that 50%-70% of dislocations occur within the first 5 wk to 3 mo postoperatively, and more than three fourths of dislocations within the first year following surgery[1,8,9,17-19]. Accordingly, the cumulative risk of dislocation does not remain constant following THA, increasing with time due to trauma, polyethylene wear, increased pseudocapsule laxity and deteriorating muscle strength[20-22]. Improved understanding of the etiology of instability following THA and concordant improvements in surgical techniques have led to a documented decrease in the dislocation rate over time[23-27].
Patient-related risk factors must be evaluated and considered preoperatively, intra-operatively and post-operatively although they are out of surgeon’s direct control (Table 1). The independent correlation of height and weight with the risk of dislocation has not been clearly demonstrated in the literature[13,28]. Several other important patient risk factors for dislocation, however, have been identified. Two large series on gender differences report that women dislocate following THA approximately twice as frequently as do men[1,9,13,18,29,30]. This apparent gender disparity is postulated to be attributed to muscle mass and strength differences, as well as differences in the compliance and elasticity of the soft tissues as a result of genetic and hormonal differences between the sexes.
| Patient factors | Surgical factors |
| Female gender | Surgical approach |
| Age > 80 yr | Capsular repair |
| Neuromuscular disorders | Soft tissue tension |
| Cognitive disorders | Component malpositioning |
| Alcoholism | Femoral head size |
| Abductor weakness | Impingement |
| Prior hip surgery | Surgeon experience |
Evidence that age is an independent risk factor for dislocation is at best inconclusive and still controversial[13,28]. Larger series of patients have not found age to be an independent predictor of instability, yet reports do exist in the literature which find statistical trends or evidence to the contrary[14,31,32]. Advanced age (greater than 80 years old) brings increased frailty, decline in muscular tone, inability to follow postoperative protocols and higher incidences of cognitive problems, all of which have been linked to increased dislocation rates, and likely confound literature reports of age as an independent risk factor.
Patients with neuromuscular and cognitive disorders, including cerebral palsy, muscular dystrophies, psychoses, dementia and alcoholism have also been consistently demonstrated to be at a higher risk for postoperative dislocation[13,14,30,33-38]. Muscle weakness, muscle or general imbalance and inability to comply with with activity restrictions all are considered to be the likely causative factors[32]. Diseases such as muscular dystrophy and myasthenia gravis are inherent to the musculature and directly cause muscle weakness, which can increase dislocation incidence, particularly with abductor weakness. Other neurologic conditions, such as Parkinson’s disease, cerebral palsy and multiple sclerosis can lead to similar muscle, particularly abductor, weakness. Cognitive dysfunction has likewise been shown to be an independent risk factor for hip instability following THA[32,39]. For these patients, noncompliance or inability to follow post-operative activity restrictions were implicated as the likely cause for dislocation.
A history of prior hip surgery is also considered to be an independent risk factor for dislocation[14,17,36,38,40]. Woo and Morrey found the incidence of instability to double in hips that had undergone any previous open surgical procedure[1]. This is likely due to scarring, laxity and other soft tissue issues directly resulting from the previous operative procedure.
Patient-related risk factors, although out of the surgeon’s control, are important to consider when evaluating a potential THA candidate preoperatively. Patients with one or more of these risk factors should be appropriately counseled preoperatively about their increased risk of postoperative instability.
Several elements of the surgical process and technique may contribute to postoperative instability, including surgical approach, implant-related factors, soft tissue repair and tensioning, impingement and surgeon experience.
The incidence of instability as it relates to surgical approach has been extensively investigated and reviewed in the literature. Historically, higher dislocations rates have been reported for the posterior approach (5.8%) vs the anterolateral approach (2.3%)[1,36]. A recent meta-analysis involving 13 203 primary THAs found dislocation rates of 1.27% for trans-trochanteric, 3.23% for posterior (2.03% with capsular repair), 2.18% for anterolateral and 0.55% for the direct lateral approach[36,41]. Furthermore, the literature demonstrates that 75% to 90% of dislocations are in the posterior direction, thus surgical approaches that compromise posterior soft tissues theoretically could contribute to posterior instability[7,13]. Therefore, when risk of dislocation is of particular concern, the posterior approach historically has been the least favored. Other investigators have shown, however, that a meticulous posterior capsular repair decreases dislocation rates to comparable levels to other approaches. White et al[42] demonstrated a reduction from 2.8% to 0.6% in 1000 patients; Goldstein et al[43] reported a decrease from 4.8% to 0.7% in 1515 patients; and Pellicci et al[44] reported a reduction from 4.1% to 0.0% in 395 patients with posterior capsular repair[36].
Soft tissue tension, influenced by the joint capsule, short external rotators and gluteal muscles, has been meticulously evaluated as a factor in dislocation[13]. Even appropriately placed components may become unstable if the appropriate length and offset are not restored. As discussed before, reconstruction of the posterior capsule and short external rotators after a posterior approach has been shown to significantly reduce dislocation rate[42-44]. The surgeon can also greatly affect soft tissue tension with femoral offset. Patients who dislocate have a notable loss of offset compared to patients with stable hips[33,35]. If the soft tissues are lax, and the offset has already been maximized, a lateralized liner can increase soft tissue tension.
Implant-related risk factors are also an important consideration, as malpositioning of components is the most common cause of instability[41]. Intrinsic implant related factors, such as implant type, design and size, are important to consider both preoperatively and intraoperatively. Femoral head component sizing is of particular interest. The larger the femoral head, the further it must sublux before it can dislocate, a distance referred to as the jump distance. Berry et al[29] in a study of 21 047 THAs, found a significantly decreased rate of dislocation with the use of larger femoral heads in all surgical approaches. Additional studies have also found decreased rates of dislocation with larger head sizes, although a large head has not always been found to be necessary to achieve low early dislocation rates[7,44,45]. When determining the appropriate head size, the surgeon must also consider the appropriate combination of socket type, orientation and approach to optimize the implant and minimize the dislocation rate. Increasing femoral offset has been described to have a positive effect on decreasing the incidence of dislocation by optimizing soft tissue tensioning[7,33,45]. Likewise, neck design and geometry have been demonstrated by numerous authors as important to the stability of the THA[46,47].
Component malposition is the most common cause of instability following THA[11,41,48]. Excessive anteversion of the acetabulum may result in anterior dislocation; excessive retroversion may result in posterior dislocation; similarly, excessive abduction may result in lateral dislocation. Ali Khan et al[18] found that the most common surgical error was placement of the acetabular component in excessive anteversion and abduction, a finding reinforced by numerous other authors[19,49]. A recent study by Callanan et al[50] found increased risk of acetabular cup malposition for minimally invasive approaches, low volume surgeons, and obese patients. Daly and Morrey[24] found that 86% of patients who underwent revision surgery without correction of acetabular component malposition continued to have instability. Furthermore, the largest number of successful revision surgeries occurred in patients who underwent repositioning of the acetabular component. Based on several studies, cup anteversion should be 20°± 5° (measured from the axis of the cup) and 40°± 10° of cup abduction to be considered in the safe zone of lower dislocation risk[13,51-53]. Forward rotation of the pelvis must be taken into account, or excessive retroversion of the cup can result[39]. Positioning of the femoral component is not as simple to evaluate due to lack of standardization regarding rotation. Many imaging modalities have been evaluated in an attempt to determine optimal femoral component orientation, but significance with regards to determining hip stability has not been definitely established[5,54].
Impingement, including prosthetic, cement or bony, is another surgical factor involved in dislocation. Whether caused by osteophytes that were not resected at the time of the primary surgical procedure, or capsular scar tissue or heterotopic ossification that developed postoperatively, impingement can directly be linked to instability, and should be addressed at the time of revision surgery. Daly and Morrey[7] found impingement as the primary cause of instability in 9 hips in a series of 95 recurrent dislocations. Surgical correction of this, however, had a success rate of only 56%.
Surgeon experience is the final surgical risk factor for THA instability. The rate of dislocation has an inverse relationship to the experience of the surgeon[55]. For every ten primary arthroplasties performed yearly, there is a 50% reduction in the postoperative dislocation rate[55]. There is also a high dislocation rate amongst surgeons who perform less than thirty THAs yearly[7].
The evaluation of an unstable THA should follow a standardized and methodical approach to allow formulation of the ideal treatment plan. Even with optimum component orientation, adequate soft-tissue balancing and the appropriate components, dislocation after THA can still occur in the hands of the most experienced joint surgeons.
The history is vital to understanding how the dislocation occurred. Elucidating how the current dislocation occurred, or the activity that was being performed in relation to the position of the affected limb, as well as an inquiry into other potential previous episodes of instability or dislocation is of paramount importance. Questions regarding the presence of infectious symptoms such as fevers, chills, antecedent pain or night sweats are also important. A review of previous documentation, including operative notes documenting what approach was used, types and positioning of implants, as well as any noted intra- or post-operative complications is vital.
Physical examination should include assessment of both lower extremities, carefully noting gait, range of motion, strength (paying close attention to the abductor musculature), neurovascular status, leg length, location of previous incisions and leg position on presentation. Additionally, if clinically indicated, diagnostic tests including white blood cell count, erythrocyte sedimentation rate, C-reactive protein level, aspiration and cultures should be considered, as infection may be a contributing factor to the instability[13].
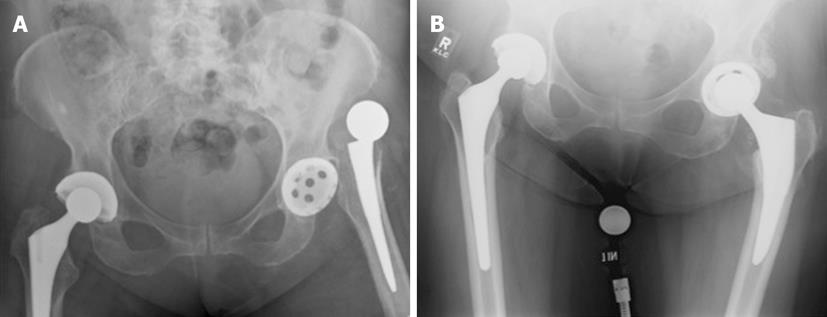
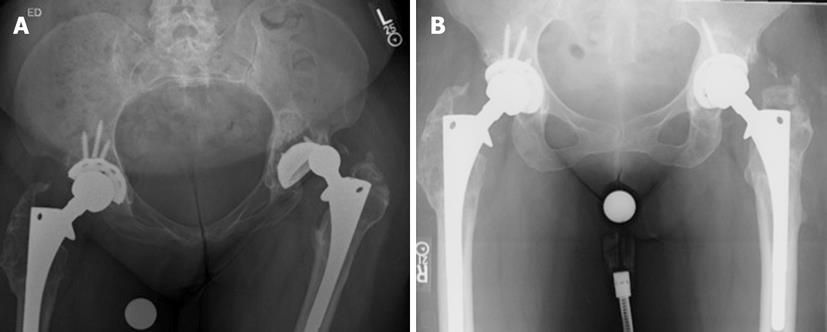
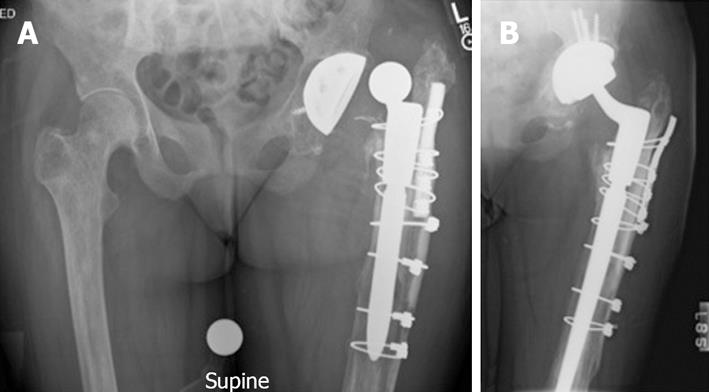
Radiographic assessment begins with an anteroposterior pelvis and true lateral radiograph of the affected hip (Figures 1-3). The femoral component should be assessed for head-to-neck ratio, loosening, neck length and offset, angulation and any evidence of subsidence. An attempt to determine the version of the femoral component should also be undertaken, although this can be challenging to measure radiographically. There is a high incidence of femoral malposition in hips with instability when femoral version is measured fluoroscopically[33]. Similarly, assessment of the acetabular orientation is difficult to ascertain from plain radiographs of the hip as well. Various methods have been described to measure acetabular anteversion using both plain radiographs and computed tomography scans[51,56].
The initial management of an unstable or dislocated THA is closed reduction. Once this has been completed, it is vital to assess the stable range of motion of the hip. Both non-operative and operative options exist, the choice of which depends on the patient’s inherent risk factors for future dislocations, reason for the dislocation, acuity of dislocation, stable range of motion, treatment goals and many other factors. It should be emphasized that instability is an extremely complex problem often better handled by an arthroplasty specialist[24].
If the patient has instability or presents after a first dislocation, has an acceptable stable range of motion (> 90 degrees of flexion and at least 45 degrees of internal rotation), and post-reduction radiographs demonstrate acceptable alignment and position of components, then treatment with external bracing often results in good outcomes[19,53]. However, the use of braces is extremely patient-dependent, as the braces are inconvenient and cumbersome. Even the most compliant patients will have difficulty using braces effectively, making them challenging to study in large numbers or to implement effectively on a regular basis. Despite these challenges, it is estimated that two-thirds of patients can be successfully managed with closed reduction followed by bracing[57].
In patients who have a secondary dislocation, who have failed conservative management, or obvious component malalignment is noted on plain radiographs, surgical revision should be a strong consideration. Of paramount importance is identifying the cause(s) of instability, and addressing all of the possible causes for the instability at the index revision operation[24]. Surgical options for the treatment of instability or recurrent dislocation include revision of components; exchange of modular components such as the femoral head and acetabular liner; bipolar arthroplasty; tripolar arthroplasty; use of a larger femoral head; use of a constrained liner; soft tissue reinforcement and advancement of the greater trochanter[16].
The first consideration once surgical management of the unstable THA has been chosen is the surgical approach. Although convenient, the previous surgical approach need not always be used, especially if the revision surgeon is more familiar with a different approach. Whenever possible, however, previous incisions should be incorporated into the new approach, as parallel incisions may lead to vascular compromise of the bridging skin[58,59].
The more challenging preoperative decision in revision surgery is whether to retain well-fixed components. In general, when well-fixed components are malpositioned, they should be replaced[16,40]. Daly and Morrey[24] found that 6/7 patients with retained, well-fixed but mal-aligned components continued to have instability. In the case of infection, usually components will need to be exchanged following incision and debridement, in either a one or two stage procedure. When the components are well-positioned, retention with exchange of modular components is reasonable, although the revision surgeon must still be acutely aware that even subtle component malposition can result in clinically significant instability[40].
Modular component exchange is typically reserved for patients who do not have gross malpositioning of any components or significant abductor weakness[14]. This surgical treatment involves exchanging and elevating the polyethylene acetabular liner and upsizing the femoral head[16,60]. At the time of revision, the surgeon may take advantage of numerous modular options, including increasing femoral head size, increasing neck length, or various liner options. Several studies have demonstrated reasonable success (69%-96%) with modular component exchange[61-65].
Bipolar and tripolar arthroplasty have also been successfully utilized in treating recurrent instability following THA[23,66-71]. The bipolar arthroplasty component consists of a small femoral head located inside a polyethylene shell that is then covered by a larger femoral head. This theoretically allows motion between the small femoral head and the liner as well as the larger femoral head and the acetabulum[16]. Placement of a bipolar prosthesis inside an acetabular component with a liner is known as a tripolar arthroplasty[16]. Parvizi et al[66] described the outcome of 27 patients who were treated for instability using this technique. In their study, 81% of patients gained hip stability, 7% experienced a single episode of instability, and the remaining 11% had recurrent instability requiring further surgery[14]. Nadaud et al[67] described a series of 23 revisions that were fixed cups switched to bipolar for instability. All patients in their series who underwent revision to a bipolar prosthesis had no further instability, leading them to conclude that acetabular revision to a bipolar prosthesis provides reliable stability in recurrent prosthetic hip instability.
Grigoris et al[72] first described the use of the the tripolar arthroplasty for the treatment of recurrent dislocation. In their series, 0/8 patients had recurrent dislocation at a mean of 4.2 years. Guyen et al[68] published a series of 167 primary THAs using tripolar arthroplasty at the index operation for patients with at least 2 risk factors for dislocation. At an average follow up of close to 2 years, no dislocations had been noted. Levine et al[71] reported a series of 31 hips revised with a tripolar articular construct for instability. 93% of the patients undergoing revision did not require further revision surgery.
There is clearly evidence in the literature supporting the use of bipolar and tripolar arthroplasty as salvage procedures in the management of recurrent dislocation. However, these do not come without problems, the most important of which is the potential for medial or superior migration of the prosthesis with time. Groin pain is also a frequently reported issue for these patients. Thus, the majority of authors do not recommend routine use of bipolar or tripolar arthropasty as main-stay treatment of recurrent dislocation[16,66,68,69].
Large femoral heads represent another option to address hip instability. Femoral head sizes greater than 36 mm have been designed to provide increased stability through a rather simple theory: the larger the femoral head, the greater the volume of the head that needs to be displaced from the acetabulum for dislocation to occur. This is accomplished through an improved head-neck ratio and by increasing the jump distance (distance the femoral head must travel to dislocate)[9,73]. Kung et al[74] evaluated 230 patients for the effect of femoral head size (28 mm vs 36 mm) on postoperative stability. At a mean follow up of 27 mo, they found that the use of the larger femoral head brought the dislocation rate from 12.7% down to 0%. However, if the abductor mechanism was absent, there was no statistically significant reduction in dislocation rate. Smith et al[75] found similar success in 377 hips treated with 38 mm metal-on-metal arthroplasties, with no dislocations in the critical early follow-up period, however recent literature has questioned the use of metal-on-metal arthroplasties for other reasons. Peters et al[76] found similar success with the use of large femoral heads (38 mm), with a reduction of dislocation rate from 2.5% to 0%. Amstutz et al[77] investigated the use of large femoral heads for patients with recurrent dislocations (29 hips) and in primary surgeries (57 hips). The prevalence of dislocation was 13.7% for the recurrent dislocation group and 3.5 for the primary surgery group. The authors also noted that the use of large femoral heads necessitates simultaneous insertion of a thin polyethylene liner, the longevity of which has not been determined.
Constrained liners are designed to physically resist dislocation of the femoral head by locking the head into the acetabular cup, and are an invaluable tool in the surgical management of recurrent dislocations[9]. This device is particularly useful for the surgical management of recurrent dislocation in the setting of abductor deficiency, recurrent dislocation of undetermined etiology and in patients with multiple dislocations due to neurological impairment[16]. The success of constrained liners for instability in these specific situations has been well-documented in the literature[4,5,12,78-81]. Additionally, constrained liners offer the ability provide enhanced stability to a hip without the need to revise well-fixed, well-positioned acetabular components[16]. Anderson et al[5] first reported the use of constrained liners as a salvage procedure in patients with recurrent dislocations. 71% of the 21 patients in their report experienced no further dislocations at a minimum of 2-year follow-up. Callaghan et al[25] reported a series of 31 hips with constrained liners implanted into well-fixed acetabular components, and found that 94% of patients were failure-free at an average follow up of nearly 4 years. Significant improvements in dislocation rates with the use of constrained liners in previously unstable THAs were also noted in more recent series[80,81]. Constrained liners offer a valuable option for the management of recurrent dislocations when no obvious cause for dislocation can be identified or if the dislocation is due to soft-tissue deficit that is not otherwise repairable. The surgeon must, however, be careful to ensure that the components are well-positioned prior to proceeding with constrained liner placement, as even subtle component malpositioning can be the cause of such instability[16,40].
The use of additional static restraint to augment the deficient posterior capsule or enhance a deficient abductor mechanism have been described by many authors, although with notable variability in outcome. Lavigne et al[2] were the first to report the use of an Achilles tendon allograft placed between the greater trochanter and the ischium to reduce the range of internal rotation and enhance stability. In their series of 10 patients, 6 had complete elimination of instability at 3-year follow up. Recently Van Warmerdam et al[82] described the use of an Achilles autograft sling to improve hip stability. In their series of 8 patients, 7 patients had no recurrent instability with maintenance of good postoperative range of motion at an average of 5 years’ follow-up. The authors concluded that allograft slings can be used to improve hip stability without significant limitation of postoperative hip range of motion.
Barbosa et al[27] described the successful use of a synthetic ligament prosthesis to treat 4 patients with recurrent posterior dislocation of THA without ascertainable cause. At an average follow-up of over 2 years, none of the patients experienced further dislocation. Stromsoe et al[83] described the use of fascia lata to augment deficient abductors. In their series of 18 patients with posterior THA dislocations, 16 achieved stability with the procedure.
Soft-tissue procedures provide an additional approach to achieving THA stability in patients who are poor candidates for other options such as constrained liners. These procedures can be technically demanding and are likely to fail in patients with any component malpositioning.
Trochanteric advancement, although now somewhat historic, has been used to increase abductor tension and stability with good results[14]. The technique is designed and has been proven to improve the resting length and functioning of the abductor mechanism, which consequently affords increased hip stability in 81%-90% of cases[14,84-87]. The advent of modular implants allows the surgeon to increase femoral neck length to accomplish the same goals without the potential morbidity of greater trochanteric nonunion. Thus, it continues to be used only as an option when there is proximal migration of an un-united trochanter after a trochanteric osteotomy[14].
Instability following THA is an unfortunately frequent and serious problem that requires thorough evaluation and preoperative planning before surgical intervention. Prevention through optimal index surgery is of great importance, as the management of an unstable THA is challenging even for an experienced joints surgeon. However, even after well-planned surgery, a significant incidence of recurrent instability still exists. Non-operative management is often successful if the components are well-fixed and correctly positioned in the absence of neurocognitive disorders. If conservative management fails, surgical options include revision of malpositioned components; exchange of modular components such as the femoral head and acetabular liner; bipolar arthroplasty; tripolar arthroplasty; use of a larger femoral head; use of a constrained liner; soft tissue reinforcement and advancement of the greater trochanter. In cases of recurrent instability after appropriate revision surgery, salvage procedures may become necessary. Patients who fail to respond to any measures may be candidates for end stage revision to a resection arthroplasty.
Peer reviewer: Madana Vallem, MD, Mohawk Valley Orthopedics,1903 Sunset Ave # 3, Utica, NY 13502, United States
S- Editor Huang XZ L- Editor A E- Editor Zheng XM
| 1. | Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295-1306. [PubMed] |
| 2. | Lavigne MJ, Sanchez AA, Coutts RD. Recurrent dislocation after total hip arthroplasty: treatment with an Achilles tendon allograft. J Arthroplasty. 2001;16:13-18. [PubMed] |
| 3. | Hedlundh U, Ahnfelt L, Hybbinette CH, Wallinder L, Weckström J, Fredin H. Dislocations and the femoral head size in primary total hip arthroplasty. Clin Orthop Relat Res. 1996;333:226-233. [PubMed] |
| 4. | Goetz DD, Bremner BR, Callaghan JJ, Capello WN, Johnston RC. Salvage of a recurrently dislocating total hip prosthesis with use of a constrained acetabular component. A concise follow-up of a previous report. J Bone Joint Surg Am. 2004;86-A:2419-2423. [PubMed] |
| 5. | Anderson MJ, Murray WR, Skinner HB. Constrained acetabular components. J Arthroplasty. 1994;9:17-23. [PubMed] |
| 6. | Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty : an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84-A:1788-1792. [PubMed] |
| 7. | Morrey BF. Instability after total hip arthroplasty. Orthop Clin North Am. 1992;23:237-248. [PubMed] |
| 8. | Fricka KB, Marshall A, Paprosky WG. Constrained liners in revision total hip arthroplasty: an overuse syndrome: in the affirmative. J Arthroplasty. 2006;21:121-125. [PubMed] [DOI] [Full Text] |
| 9. | Sikes CV, Lai LP, Schreiber M, Mont MA, Jinnah RH, Seyler TM. Instability after total hip arthroplasty: treatment with large femoral heads vs constrained liners. J Arthroplasty. 2008;23:59-63. [PubMed] [DOI] [Full Text] |
| 10. | Kotwal RS, Ganapathi M, John A, Maheson M, Jones SA. Outcome of treatment for dislocation after primary total hip replacement. J Bone Joint Surg Br. 2009;91:321-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Krenzel BA, Berend ME, Malinzak RA, Faris PM, Keating EM, Meding JB, Ritter MA. High preoperative range of motion is a significant risk factor for dislocation in primary total hip arthroplasty. J Arthroplasty. 2010;25:31-35. [PubMed] [DOI] [Full Text] |
| 12. | Williams JT, Ragland PS, Clarke S. Constrained components for the unstable hip following total hip arthroplasty: a literature review. Int Orthop. 2007;31:273-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Soong M, Rubash HE, Macaulay W. Dislocation after total hip arthroplasty. J Am Acad Orthop Surg. 2004;12:314-321. [PubMed] |
| 14. | Bourne RB, Mehin R. The dislocating hip: what to do, what to do. J Arthroplasty. 2004;19:111-114. [PubMed] |
| 15. | Berry DJ, von Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86-A:9-14. [PubMed] |
| 16. | Parvizi J, Picinic E, Sharkey PF. Revision total hip arthroplasty for instability: surgical techniques and principles. J Bone Joint Surg Am. 2008;90:1134-1142. [PubMed] |
| 17. | Padgett DE, Warashina H. The unstable total hip replacement. Clin Orthop Relat Res. 2004;420:72-79. [PubMed] |
| 18. | Ali Khan MA, Brakenbury PH, Reynolds IS. Dislocation following total hip replacement. J Bone Joint Surg Br. 1981;63-B:214-218. [PubMed] |
| 19. | Williams JF, Gottesman MJ, Mallory TH. Dislocation after total hip arthroplasty. Treatment with an above-knee hip spica cast. Clin Orthop Relat Res. 1982;53-58. [PubMed] |
| 20. | Mallory TH, Lombardi AV, Fada RA, Herrington SM, Eberle RW. Dislocation after total hip arthroplasty using the anterolateral abductor split approach. Clin Orthop Relat Res. 1999;358:166-172. [PubMed] |
| 21. | Berend KR, Lombardi AV, Mallory TH, Adams JB, Russell JH, Groseth KL. The long-term outcome of 755 consecutive constrained acetabular components in total hip arthroplasty examining the successes and failures. J Arthroplasty. 2005;20:93-102. [PubMed] [DOI] [Full Text] |
| 22. | Berry DJ. Unstable total hip arthroplasty: detailed overview. Instr Course Lect. 2001;50:265-274. [PubMed] |
| 23. | Callaghan JJ, O'Rourke MR, Goetz DD, Lewallen DG, Johnston RC, Capello WN. Use of a constrained tripolar acetabular liner to treat intraoperative instability and postoperative dislocation after total hip arthroplasty: a review of our experience. Clin Orthop Relat Res. 2004;429:117-123. [PubMed] |
| 24. | Daly PJ, Morrey BF. Operative correction of an unstable total hip arthroplasty. J Bone Joint Surg Am. 1992;74:1334-1343. [PubMed] |
| 25. | Callaghan JJ, Parvizi J, Novak CC, Bremner B, Shrader W, Lewallen DG, Johnston RC, Goetz DD. A constrained liner cemented into a secure cementless acetabular shell. J Bone Joint Surg Am. 2004;86-A:2206-2211. [PubMed] |
| 26. | Bremner BR, Goetz DD, Callaghan JJ, Capello WN, Johnston RC. Use of constrained acetabular components for hip instability: an average 10-year follow-up study. J Arthroplasty. 2003;18:131-137. [PubMed] |
| 27. | Barbosa JK, Khan AM, Andrew JG. Treatment of recurrent dislocation of total hip arthroplasty using a ligament prosthesis. J Arthroplasty. 2004;19:318-321. [PubMed] |
| 28. | Sanchez-Sotelo J, Berry DJ. Epidemiology of instability after total hip replacement. Orthop Clin North Am. 2001;32:543-52, vii. [PubMed] |
| 29. | Berry DJ, von Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456-2463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 30. | Pulido L, Restrepo C, Parvizi J. Late instability following total hip arthroplasty. Clin Med Res. 2007;5:139-142. [PubMed] [DOI] [Full Text] |
| 31. | Newington DP, Bannister GC, Fordyce M. Primary total hip replacement in patients over 80 years of age. J Bone Joint Surg Br. 1990;72:450-452. [PubMed] |
| 32. | Woolson ST, Rahimtoola ZO. Risk factors for dislocation during the first 3 months after primary total hip replacement. J Arthroplasty. 1999;14:662-668. [PubMed] |
| 33. | Fackler CD, Poss R. Dislocation in total hip arthroplasties. Clin Orthop Relat Res. 1980;151:169-178. [PubMed] |
| 34. | Carter AH, Sheehan EC, Mortazavi SM, Purtill JJ, Sharkey PF, Parvizi J. Revision for recurrent instability: what are the predictors of failure. J Arthroplasty. 2011;26:46-52. [PubMed] [DOI] [Full Text] |
| 35. | D'Angelo F, Murena L, Zatti G, Cherubino P. The unstable total hip replacement. Indian J Orthop. 2008;42:252-259. [PubMed] [DOI] [Full Text] |
| 36. | Patel PD, Potts A, Froimson MI. The dislocating hip arthroplasty: prevention and treatment. J Arthroplasty. 2007;22:86-90. [PubMed] [DOI] [Full Text] |
| 37. | Dobzyniak M, Fehring TK, Odum S. Early failure in total hip arthroplasty. Clin Orthop Relat Res. 2006;447:76-78. [PubMed] [DOI] [Full Text] |
| 38. | Zhao F, Ma C, Xiong C. [Treatments of dislocation after total hip replacement]. Zhongguo Xiu Fu Chong Jian Wai Ke Zazhi. 2007;21:12-14. [PubMed] |
| 39. | Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202-1210. [PubMed] |
| 40. | Parvizi J, Kim KI, Goldberg G, Mallo G, Hozack WJ. Recurrent instability after total hip arthroplasty: beware of subtle component malpositioning. Clin Orthop Relat Res. 2006;447:60-65. [PubMed] [DOI] [Full Text] |
| 41. | Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res. 2002;405:46-53. [PubMed] |
| 42. | White RE, Forness TJ, Allman JK, Junick DW. Effect of posterior capsular repair on early dislocation in primary total hip replacement. Clin Orthop Relat Res. 2001;393:163-167. [PubMed] |
| 43. | Goldstein WM, Gleason TF, Kopplin M, Branson JJ. Prevalence of dislocation after total hip arthroplasty through a posterolateral approach with partial capsulotomy and capsulorrhaphy. J Bone Joint Surg Am. 2001;83-A Suppl 2:2-7. [PubMed] |
| 44. | Pellicci PM, Bostrom M, Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop Relat Res. 1998;355:224-228. [PubMed] |
| 45. | Barrack RL. Dislocation after total hip arthroplasty: implant design and orientation. J Am Acad Orthop Surg. 2003;11:89-99. [PubMed] |
| 46. | Bader R, Scholz R, Steinhauser E, Zimmermann S, Busch R, Mittelmeier W. The influence of head and neck geometry on stability of total hip replacement: a mechanical test study. Acta Orthop Scand. 2004;75:415-421. [PubMed] |
| 47. | Barrack RL, Butler RA, Laster DR, Andrews P. Stem design and dislocation after revision total hip arthroplasty: clinical results and computer modeling. J Arthroplasty. 2001;16:8-12. [PubMed] |
| 48. | Rogers M, Blom AW, Barnett A, Karantana A, Bannister GC. Revision for recurrent dislocation of total hip replacement. Hip Int. 2009;19:109-113. [PubMed] |
| 49. | Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530-534. [PubMed] |
| 50. | Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, Malchau H. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469:319-329. [PubMed] [DOI] [Full Text] |
| 51. | Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217-220. [PubMed] |
| 52. | Harris WH. Advances in surgical technique for total hip replacement: without and with osteotomy of the greater trochanter. Clin Orthop Relat Res. 1980;146:188-204. [PubMed] |
| 53. | Kummer FJ, Shah S, Iyer S, DiCesare PE. The effect of acetabular cup orientations on limiting hip rotation. J Arthroplasty. 1999;14:509-513. [PubMed] |
| 54. | Eftekhar NS. Dislocation and instability complicating low friction arthroplasty of the hip joint. 1976. Clin Orthop Relat Res. 2006;453:1-5. [PubMed] |
| 55. | Hedlundh U, Ahnfelt L, Hybbinette CH, Weckstrom J, Fredin H. Surgical experience related to dislocations after total hip arthroplasty. J Bone Joint Surg Br. 1996;78:206-209. [PubMed] |
| 56. | Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228-232. [PubMed] |
| 57. | Fraser GA, Wroblewski BM. Revision of the Charnley low-friction arthroplasty for recurrent or irreducible dislocation. J Bone Joint Surg Br. 1981;63B:552-555. [PubMed] |
| 58. | Barrack RL, Burnett SJ. Preoperative planning for revision total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2800-2811. [PubMed] |
| 59. | Barrack RL, Burnett RS. Preoperative planning for revision total hip arthroplasty. Instr Course Lect. 2006;55:233-244. [PubMed] |
| 60. | Parvizi J, Wade FA, Rapuri V, Springer BD, Berry DJ, Hozack WJ. Revision hip arthroplasty for late instability secondary to polyethylene wear. Clin Orthop Relat Res. 2006;447:66-69. [PubMed] [DOI] [Full Text] |
| 61. | Biviji AA, Ezzet KA, Pulido P, Colwell CW. Modular femoral head and liner exchange for the unstable total hip arthroplasty. J Arthroplasty. 2009;24:625-630. [PubMed] [DOI] [Full Text] |
| 62. | Lombardi AV, Berend KR. Isolated acetabular liner exchange. J Am Acad Orthop Surg. 2008;16:243-248. [PubMed] |
| 63. | Toomey SD, Hopper RH, McAuley JP, Engh CA. Modular component exchange for treatment of recurrent dislocation of a total hip replacement in selected patients. J Bone Joint Surg Am. 2001;83-A:1529-1533. [PubMed] |
| 64. | McGann WA, Welch RB. Treatment of the unstable total hip arthroplasty using modularity, soft tissue, and allograft reconstruction. J Arthroplasty. 2001;16:19-23. [PubMed] |
| 65. | Earll MD, Fehring TK, Griffin WL, Mason JB, McCoy T, Odum S. Success rate of modular component exchange for the treatment of an unstable total hip arthroplasty. J Arthroplasty. 2002;17:864-869. [PubMed] |
| 66. | Parvizi J, Morrey BF. Bipolar hip arthroplasty as a salvage treatment for instability of the hip. J Bone Joint Surg Am. 2000;82-A:1132-1139. [PubMed] |
| 67. | Nadaud MC, Fehring TK, Odum S, Mason JB, Griffin WL, McCoy TH. Bipolar reconstruction for recurrent instability of the hip. Orthopedics. 2004;27:746-751. [PubMed] |
| 68. | Guyen O, Pibarot V, Vaz G, Chevillotte C, Carret JP, Bejui-Hugues J. Unconstrained tripolar implants for primary total hip arthroplasty in patients at risk for dislocation. J Arthroplasty. 2007;22:849-858. [PubMed] [DOI] [Full Text] |
| 69. | Cooke CC, Hozack W, Lavernia C, Sharkey P, Shastri S, Rothman RH. Early failure mechanisms of constrained tripolar acetabular sockets used in revision total hip arthroplasty. J Arthroplasty. 2003;18:827-833. [PubMed] |
| 70. | Guyen O, Chen QS, Bejui-Hugues J, Berry DJ, An KN. Unconstrained tripolar hip implants: effect on hip stability. Clin Orthop Relat Res. 2007;455:202-208. [PubMed] [DOI] [Full Text] |
| 71. | Levine BR, Della Valle CJ, Deirmengian CA, Breien KM, Weeden SH, Sporer SM, Paprosky WG. The use of a tripolar articulation in revision total hip arthroplasty: a minimum of 24 months' follow-up. J Arthroplasty. 2008;23:1182-1188. [PubMed] [DOI] [Full Text] |
| 72. | Grigoris P, Grecula MJ, Amstutz HC. Tripolar hip replacement for recurrent prosthetic dislocation. Clin Orthop Relat Res. 1994;304:148-155. [PubMed] |
| 73. | Beaulé PE, Schmalzried TP, Udomkiat P, Amstutz HC. Jumbo femoral head for the treatment of recurrent dislocation following total hip replacement. J Bone Joint Surg Am. 2002;84-A:256-263. [PubMed] |
| 74. | Kung PL, Ries MD. Effect of femoral head size and abductors on dislocation after revision THA. Clin Orthop Relat Res. 2007;465:170-174. [PubMed] [DOI] [Full Text] |
| 75. | Smith TM, Berend KR, Lombardi AV, Emerson RH, Mallory TH. Metal-on-metal total hip arthroplasty with large heads may prevent early dislocation. Clin Orthop Relat Res. 2005;441:137-142. [PubMed] |
| 76. | Peters CL, McPherson E, Jackson JD, Erickson JA. Reduction in early dislocation rate with large-diameter femoral heads in primary total hip arthroplasty. J Arthroplasty. 2007;22:140-144. [PubMed] [DOI] [Full Text] |
| 77. | Amstutz HC, Le Duff MJ, Beaulé PE. Prevention and treatment of dislocation after total hip replacement using large diameter balls. Clin Orthop Relat Res. 2004;429:108-116. [PubMed] |
| 78. | Shapiro GS, Weiland DE, Markel DC, Padgett DE, Sculco TP, Pellicci PM. The use of a constrained acetabular component for recurrent dislocation. J Arthroplasty. 2003;18:250-258. [PubMed] [DOI] [Full Text] |
| 79. | Yang C, Goodman SB. Outcome and complications of constrained acetabular components. Orthopedics. 2009;32:115. [PubMed] |
| 80. | Hernigou P, Filippini P, Flouzat-Lachaniette CH, Batista SU, Poignard A. Constrained liner in neurologic or cognitively impaired patients undergoing primary THA. Clin Orthop Relat Res. 2010;468:3255-3262. [PubMed] [DOI] [Full Text] |
| 81. | Rady AE, Asal MK, Bassiony AA. The use of a constrained cementless acetabular component for instability in total hip replacement. Hip Int. 2010;20:434-439. [PubMed] |
| 82. | Van Warmerdam JM, McGann WA, Donnelly JR, Kim J, Welch RB. Achilles allograft reconstruction for recurrent dislocation in total hip arthroplasty. J Arthroplasty. 2011;26:941-948. [PubMed] [DOI] [Full Text] |
| 83. | Strømsøe K, Eikvar K. Fascia lata plasty in recurrent posterior dislocation after total hip arthroplasty. Arch Orthop Trauma Surg. 1995;114:292-294. [PubMed] |
| 84. | Ekelund A. Trochanteric osteotomy for recurrent dislocation of total hip arthroplasty. J Arthroplasty. 1993;8:629-632. [PubMed] |
| 85. | Kaplan SJ, Thomas WH, Poss R. Trochanteric advancement for recurrent dislocation after total hip arthroplasty. J Arthroplasty. 1987;2:119-124. [PubMed] |
| 86. | Dennis DA, Lynch CB. Trochanteric osteotomy and advancement: a technique for abductor related hip instability. Orthopedics. 2004;27:959-961. [PubMed] |
| 87. | DeWal H, Su E, DiCesare PE. Instability following total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2003;32:377-382. [PubMed] |