Revised: May 12, 2012
Accepted: June 5, 2012
Published online: June 18, 2012
The theoretical advantages of metal-on-metal (MOM) bearing couples in total hip arthroplasty (THA) have been recently balanced by concerns regarding adverse local and systemic effects. Higher than anticipated early revision rates have been reported by several joint registries. Failed MOM hips present with a spectrum of symptoms and findings and traditional methods of failure must be considered in addition to the failure modes that appear to be unique to the MOM bearing couple. Metal hypersensitivity and soft tissue immune reactions remain incompletely understood and require careful ongoing study. The tools available to evaluate MOM THAs and the indications for revision surgery remain to be defined. Outcomes following revision of MOM hips appear to depend on appropriate evaluation, early identification, and appropriate surgical management.
- Citation: Griffin JW, D’Apuzzo M, Browne JA. Management of failed metal-on-metal total hip arthroplasty. World J Orthop 2012; 3(6): 70-74
- URL: https://www.wjgnet.com/2218-5836/full/v3/i6/70.htm
- DOI: https://dx.doi.org/10.5312/wjo.v3.i6.70
Total hip replacement has been one of the most performed and predictable surgeries available in the United States for the past decade. In an effort to reduce wear debris and failure related to osteolysis, improved metal-on-metal (MOM) articulations were reintroduced in the 1990s and remain the only option for surface replacement arthroplasty[1]. Following this rebirth, a variety of soft-tissue reactions and periprosthetic lesions were described in patients with MOM arthroplasty[2,3]. This led to concerns regarding potential metal hypersensitivity or immunogenicity and its potential role in catastrophic failure of MOM implants. In addition, increased early rates of revision are being reported by national joint registries. Despite these concerns, outcomes of MOM hip replacements related to performance have been favorable in some studies[4,5].
At the present time, methods to evaluate the patient with a MOM bearing are poorly defined and indications for revision are unclear. Additionally, negative public press regarding MOM bearings has led patients to seek out diagnostic testing in the absence of symptoms[6]. The purpose of this paper is to describe current concepts related to the evaluation and management of MOM total hip arthroplasty (THA).
The first generation of total hip implant with a metal-on-metal articulation is attributed to George McKee of Norwich, England in 1953. The design was primitive but many lasted for more than 7 years. However, a high number of early failures discredited this bearing couple. Concerns regarding “polyethylene disease” with the metal-on-polyethylene articulation advocated by Charnley led to the development of a second generation of MOM implant designs in the early 1980s. Intrigued by the good results of certain metal-on-metal configurations, many thought that this bearing could be an improvement on polyethylene and deserved further evaluation. From the beginning of this second generation of implants, however, serious concerns were raised regarding the risks associated with an increased level of circulating metal ions, and this concern slowed down further development of this bearing couple. The third generation of MOM design encompassed an uncemented version of the second generation implant, which provided a significant number of lessons as it was used in relatively high numbers in clinical practice. The failures associated with these implants appeared to be both mechanical and biological in nature.
The fourth and current generation of MOM design is the result of continued work on the tribology of metal-on-metal. Larger diameters of these implants appeared to improve the lubrication and wear properties of the bearing couple. In addition, the promise of better stability and increased range of motion led to widespread enthusiasm and early clinical adoption of this technology[7].
The diagnostic evaluation of MOM THAs has not been standardized and varies by surgeon experience and patient presentation. A detailed history and physical examination remains a critical first step in developing a differential diagnosis of the painful MOM hip. Failures seem to occur more in females. Initial clinical evaluation should focus on patient symptoms, which commonly include groin pain[8]. Other common symptoms include difficulty with stair climbing, clunking, catching and limited strength[9]. Many patients report never having recovered from the initial operation. Ilipsoas irritation may be present due to the large femoral head size. Symptoms that suggest infection and loosening should also be noted. Physical examination may reveal common problems such as trochanteric bursitis or radiating back pain and exclude the hip itself as the cause of symptoms.
Initial imaging should include high quality radiographs to evaluate for obvious causes of failure that are not unique to MOM THAs. Loosening and lysis may be observed. Iliopsoas impingement has been seen with excessively large femoral head implant size[10]. Component position and should be carefully assessed with anteroposterior and lateral radiographs, acknowledging that many of the modern acetabular components used in MOM THA measure less than a complete hemisphere. Increasing evidence suggests that high inclination angles and excessive anteversion of the acetabular component, small head sizes, and individual prosthesis designs are all contributing factors in the failure of MOM hips[11]. Desy et al[12] performed a retrospective review of 91 patients over 2 years evaluating radiographically the acetabular inclination, version and femoral component alignment of patents with MOM hip replacements and reported that a large acetabular inclination directly correlated with metal ion concentration. Hart et al[13] conducted a prospective trial analyzing blood metal ion levels, computed tomography (CT) scanning and clinical exam in one hundred patient with MOM hip replacements and found that cup inclination, version angles and gender influenced blood cobalt and chromium levels. Additionally, in this study the changes in inclination had the greatest effect on blood metal ion concentration[13]. While studies exist with conflicting results, the general consensus appears to be that poor component positioning appears to play a role in the failure of MOM implants.
There is no generally accepted test for metal hypersensitivity. Patch testing and lymphocyte tests have been used in an attempt to determine sensitivity[1]. Hallab et al[14] reported that the prevalence of dermal sensitivity in patients with failed MOM implants was 50%, which was higher than the general population at 25%. However, based on the current evidence, we are unable to suggest that general patch testing or commercial testing is recommended during assessment the painful MOM hip[15]. Lymphocyte transformation tests as well have shown limited clinical utility in the evaluation of MOM THA.
Routine laboratory data obtained in the evaluation of a painful MOM THA includes the erythrocyte sedimentation rate and c-reactive protein. Ruling out infection as a cause of the painful total hip remains paramount in MOM hip articulations. Infection remains a common cause of early with MOM implants and is likely more common than hypersensitivity responses[9]. Aspiration should be performed in the presence of abnormal inflammatory markers to further evaluation for infection.
Controversy exists regarding serum cobalt and chromium ion levels and the impact of elevated serum ion levels in not understood. Several methods of measuring metal ion levels in the blood are available and variability between different laboratories exists. Elevated metal-ion levels following MOM has been known to exist for some time, although the biological effects of these ions is uncertain. Several studies have suggested a higher rate of revision in the presence of elevated ion levels, although patients with asymptomatic MOM hips and elevated ion levels have been observed. It has been suggested that elevated metal-ion levels correlate to increased wear and pseudotumor formation[16]. Metal-ion levels measuring less than 7 parts per billion appear to be predictive of a well-functioning MOM THA after the initial run-in period[17].
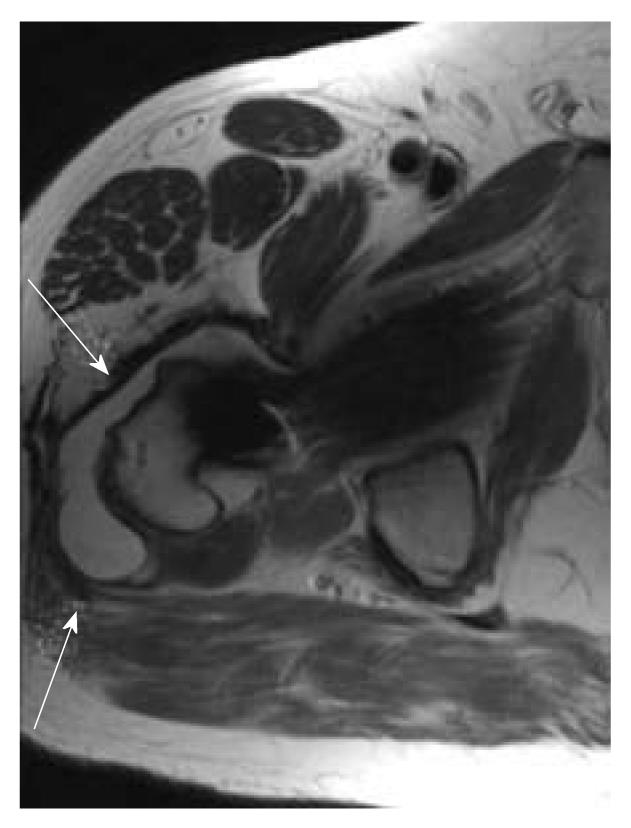
Patients with a painful MOM THA are often evaluated with cross sectional imaging or ultrasound. Standard indications for obtaining further imaging do not exist, although this should be considered in patients with component malpositioning, abductor dysfunction, or clinical concern for pseudotumor. Magnetic resonance imaging protocols to reduce the metal artifact (MARS) have been developed. Revision surgery should be considered in the event that this imaging reveals soft tissue reactions, fluid collections, or tissue masses.
Local adverse soft tissue reactions to MOM bearings have been given a variety of names: aseptic lymphocytic-vasculitis-associated lesions (ALVAL), pseudotumor, necrosis, adverse reaction to metal debris, and adverse local tissue response. The incidence of these reactions appears to be rare with an incidence likely below 1%. Various mechanisms have been proposed to explain these reactions, including patient, technique, and implant factors. The common pathway for this failure mode appears to be increased wear or corrosion with excessive release of metal ions and nanoparticles.
The relative surface area and biological activity usually increase as particle size diminishes. Metal particles are considerably smaller than debris from conventional metal-on-polyethylene bearings. This explains the increased total number of particles released from MOM hips, reported to be more than two orders of magnitude higher than that found with conventional bearings[18,19]. The wear debris is phagocytosed by macrophages and once in the acidic intramedullary environment of the lysosomes, the cobalt-chrome particles are subject to corrosion, producing high intracellular levels of ions, which can cause cell death. It has been shown that, following phagocytosis of metal particles, the osteoblastic activity of the cell is impaired which may contribute to the cellular events that occur during aseptic loosening and soft-tissue destruction[18,20]. Metal wear debris may also cause DNA damage and genomic instability.
A prominent histologic finding associated with MOM bearings is perivascular lymphocytic infiltration[21]. These findings have been termed ALVAL. A delayed-type hypersensitivity response to metal debris has been suggested as a cause of these symptoms, although the clinical significance and underlying cause of this local tissue response remains unclear.
Registries and long-term clinical studies have provided outcomes relating to the survivorship of metal bearing surfaces[22]. Several clinical series have reported good survivorship with certain implant designs. Neumann et al[5] recently provided 10 year follow up data from 100 MOM hip replacements with a 93% overall survivorship. Another 10 year radiographic survivorship study highlighted a 98.3% overall survivorship with pelvic osteolytic lesions in only 2.3% of patients. Engh[23] recently reported 5 year follow up results from a retrospective cohort of modular MOM with a 98% survivorship and a 0.3% rate of local reaction to the MOM bearing surface.
However, several recent studies and international total joint registries have documented increased early failure rates with certain MOM THA designs. Park et al[24] reported osteolysis in over 5% of patients at short term follow-up with MOM hips. Korovossis et al[25] also reported a significant rate of osteolysis with a high early revision rate. The DePuy ASR XL acebular system (Warsaw, Indiana, United States) was recalled in August 2010 after UK joint registry data indicated a 13 percent revision rate within 5 years.
Patient gender may influence MOM implant survival. Amstutz et al[4] conducted a large comparison study of clinical survivorship in men vs women and found that the revision rate was higher in the women’s group; however, this effect did not hold up when component size and surgical technique were equal between groups. Further investigation into this topic is ongoing.
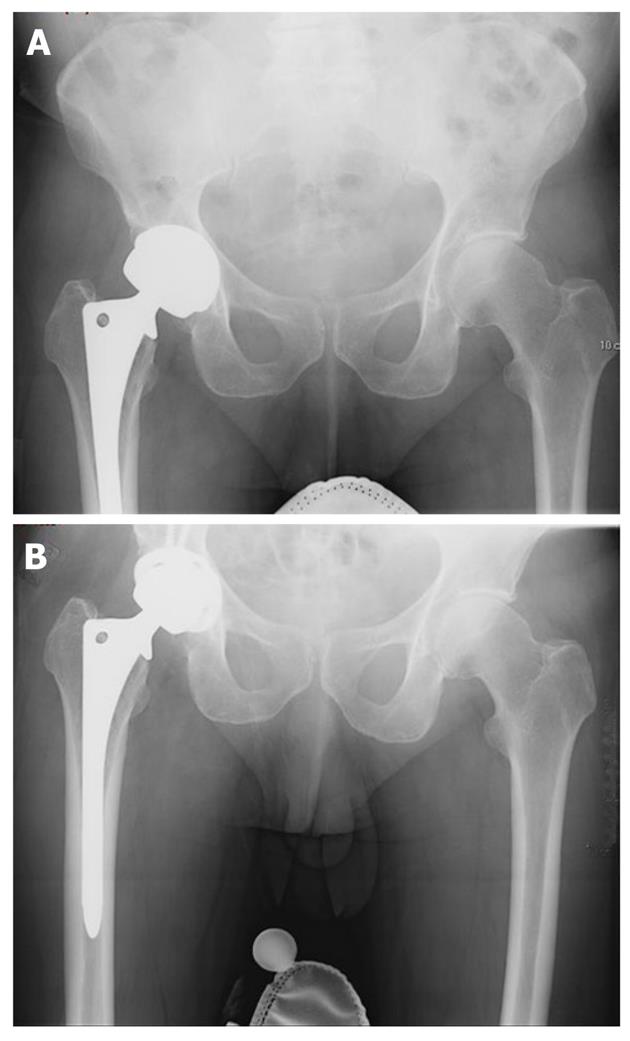
Revision of the failed MOM hip must be individualized to each individual patient and the reason for failure. A common scenario involves revision of the modular femoral head and acetabular component in the presence of a well-fixed femoral stem (Figure 1). An isolated head and liner exchange may be possible if a well-fixed and well-positioned acetabular component will accept a modular polyethylene or ceramic insert. Resection of necrotic tissue and metallosis is recommended. Extensive soft tissue damage can be a concern in the presence of a pseudotumor and a constrained liner should be considered in the event that the abductors are insufficient.
Most published data on outcomes after revision of modern MOM bearings is limited and the results are from small cohorts with limited duration of follow-up. Common preoperative symptoms of groin pain and mechanical symptoms tend to resolve reliably following conversion to an alternative bearing surface[26]. However, revision of MOM bearings has a reported complication of 7%-9% including dislocation[26]. Metal ion levels tend to fall within the first 3 mo after revision surgery but may not fully normalize at short term follow-up (Figure 2).
Metal on metal bearing couples offer the theoretical benefit of low wear rates and increased stability. However, unique failure modes of these implants appear to exist with associated problems making them a poor choice for primary hip arthroplasty at this time. Clinical evaluation of painful MOM bearing surfaces should include a careful history and physical exam in addition to laboratory evaluation and radiographic studies. Outcomes following revision surgery vary and depend on the amount of tissue destruction and bone loss from osteolysis. Early revision when problems are identified seems to offer the best chance at a good outcome.
Peer reviewer: NAS Kemal, Professor, Department of Physical Medicine and Rehabilitation, University of Dicle, Medical School, 21280 Diyarbakır, Turkey
S- Editor Yang XC L- Editor A E- Editor Yang XC
| 1. | Jacobs JJ, Urban RM, Hallab NJ, Skipor AK, Fischer A, Wimmer MA. Metal-on-metal bearing surfaces. J Am Acad Orthop Surg. 2009;17:69-76. [PubMed] |
| 2. | Langton DJ, Joyce TJ, Jameson SS, Lord J, Van Orsouw M, Holland JP, Nargol AV, De Smet KA. Adverse reaction to metal debris following hip resurfacing: the influence of component type, orientation and volumetric wear. J Bone Joint Surg Br. 2011;93:164-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 303] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 3. | Wimmer MA, Fischer A, Büscher R, Pourzal R, Sprecher C, Hauert R, Jacobs JJ. Wear mechanisms in metal-on-metal bearings: the importance of tribochemical reaction layers. J Orthop Res. 2010;28:436-443. [PubMed] |
| 4. | Amstutz HC, Le Duff MJ, Campbell PA, Gruen TA, Wisk LE. Clinical and radiographic results of metal-on-metal hip resurfacing with a minimum ten-year follow-up. J Bone Joint Surg Am. 2010;92:2663-2671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | Neumann DR, Thaler C, Hitzl W, Huber M, Hofstädter T, Dorn U. Long-term results of a contemporary metal-on-metal total hip arthroplasty: a 10-year follow-up study. J Arthroplasty. 2010;25:700-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Donell ST, Darrah C, Nolan JF, Wimhurst J, Toms A, Barker TH, Case CP, Tucker JK. Early failure of the Ultima metal-on-metal total hip replacement in the presence of normal plain radiographs. J Bone Joint Surg Br. 2010;92:1501-1508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Triclot P. Metal-on-metal: history, state of the art (2010). Int Orthop. 2011;35:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Lavigne M, Laffosse JM, Ganapathi M, Girard J, Vendittoli P. Residual groin pain at a minimum of two years after metal-on-metal THA with a twenty-eight-millimeter femoral head, THA with a large-diameter femoral head, and hip resurfacing. J Bone Joint Surg Am. 2011;93 Suppl 2:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Browne JA, Bechtold CD, Berry DJ, Hanssen AD, Lewallen DG. Failed metal-on-metal hip arthroplasties: a spectrum of clinical presentations and operative findings. Clin Orthop Relat Res. 2010;468:2313-2320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 10. | Browne JA, Polga DJ, Sierra RJ, Trousdale RT, Cabanela ME. Failure of larger-diameter metal-on-metal total hip arthroplasty resulting from anterior iliopsoas impingement. J Arthroplasty. 2011;26:978.e5-978.e8. [PubMed] |
| 11. | Haddad FS, Thakrar RR, Hart AJ, Skinner JA, Nargol AV, Nolan JF, Gill HS, Murray DW, Blom AW, Case CP. Metal-on-metal bearings: the evidence so far. J Bone Joint Surg Br. 2011;93:572-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 198] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 12. | Desy NM, Bergeron SG, Petit A, Huk OL, Antoniou J. Surgical variables influence metal ion levels after hip resurfacing. Clin Orthop Relat Res. 2011;469:1635-1641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Hart AJ, Skinner JA, Henckel J, Sampson B, Gordon F. Insufficient acetabular version increases blood metal ion levels after metal-on-metal hip resurfacing. Clin Orthop Relat Res. 2011;469:2590-2597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surg Am. 2001;83-A:428-436. [PubMed] |
| 15. | Granchi D, Ciapetti G, Stea S, Cavedagna D, Bettini N, Bianco T, Fontanesi G, Pizzoferrato A. Evaluation of several immunological parameters in patients with aseptic loosening of hip arthroplasty. Chir Organi Mov. 1995;80:399-408. [PubMed] |
| 16. | Kwon YM, Ostlere SJ, McLardy-Smith P, Athanasou NA, Gill HS, Murray DW. "Asymptomatic" pseudotumors after metal-on-metal hip resurfacing arthroplasty: prevalence and metal ion study. J Arthroplasty. 2011;26:511-518. [PubMed] [DOI] [Full Text] |
| 18. | Doorn PF, Campbell PA, Worrall J, Benya PD, McKellop HA, Amstutz HC. Metal wear particle characterization from metal on metal total hip replacements: transmission electron microscopy study of periprosthetic tissues and isolated particles. J Biomed Mater Res. 1998;42:103-111. [PubMed] |
| 19. | Sieber HP, Rieker CB, Köttig P. Analysis of 118 second-generation metal-on-metal retrieved hip implants. J Bone Joint Surg Br. 1999;81:46-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 168] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 20. | Lohmann CH, Schwartz Z, Köster G, Jahn U, Buchhorn GH, MacDougall MJ, Casasola D, Liu Y, Sylvia VL, Dean DD. Phagocytosis of wear debris by osteoblasts affects differentiation and local factor production in a manner dependent on particle composition. Biomaterials. 2000;21:551-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 118] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 21. | Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Köster G, Lohmann CH. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87:28-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Corten K, MacDonald SJ. Hip resurfacing data from national joint registries: what do they tell us? What do they not tell us? Clin Orthop Relat Res. 2010;468:351-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Engh CA, Ho H, Engh CA. Metal-on-metal hip arthroplasty: does early clinical outcome justify the chance of an adverse local tissue reaction? Clin Orthop Relat Res. 2010;468:406-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Park YS, Moon YW, Lim SJ, Yang JM, Ahn G, Choi YL. Early osteolysis following second-generation metal-on-metal hip replacement. J Bone Joint Surg Am. 2005;87:1515-1521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 145] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 25. | Korovessis P, Petsinis G, Repanti M, Repantis T. Metallosis after contemporary metal-on-metal total hip arthroplasty. Five to nine-year follow-up. J Bone Joint Surg Am. 2006;88:1183-1191. [PubMed] [DOI] [Full Text] |
| 26. | Rajpura A, Porter ML, Gambhir AK, Freemont AJ, Board TN. Clinical experience of revision of metal on metal hip arthroplasty for aseptic lymphocyte dominated vasculitis associated lesions (ALVAL). Hip Int. 2011;21:43-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |