Published online Oct 18, 2012. doi: 10.5312/wjo.v3.i10.162
Revised: August 25, 2012
Accepted: October 10, 2012
Published online: October 18, 2012
AIM: To develop new fixation techniques for the treatment of periprosthetic fractures using intraprosthetic screw fixation with inserted threaded liners.
METHODS: A Vancouver B1 periprosthetic fracture was simulated in femur prosthesis constructs using sawbones and cemented regular straight hip stems. Fixation was then performed with either unicortical locked-screw plating using the less invasive stabilization system-plate or with intraprosthetic screw fixation using inserted liners. Two experimental groups were formed using either prostheses made of titanium alloy or prostheses made of cobalt chrome alloy. Fixation stability was compared in an axial load-to-failure model. Drilling was performed using a specially invented prosthesis drill with constantly applied internal cooling.
RESULTS: The intraprosthetic fixation model with titanium prostheses was superior to the unicortical locked-screw fixation in all tested devices. The intraprosthetic fixation model required 10 456 N ± 1892 N for failure and the unicortical locked-screw plating required 7649 N ± 653 N (P < 0.05). There was no significant difference between the second experimental group and the control group.
CONCLUSION: Intraprosthetic screw anchorage with special threaded liners enhances the primary stability in treating periprosthetic fractures by internal fixation.
- Citation: Brand S, Klotz J, Hassel T, Petri M, Haasper C, Bach FW, Krettek C, Goesling T. Intraprosthetic fixation techniques in the treatment of periprosthetic fractures-A biomechanical study. World J Orthop 2012; 3(10): 162-166
- URL: https://www.wjgnet.com/2218-5836/full/v3/i10/162.htm
- DOI: https://dx.doi.org/10.5312/wjo.v3.i10.162
The number of implanted hip prosthesis is still increasing all over the world[1]. This increase and the growth in life expectancy will higher the incidence of periprosthetic fractures[2,3]. Today, the risk of a periprosthetic fracture is about 0.3-2.0 percent in the first years after implantation[3-7].
Operative treatment is the first choice and non-operative treatment is reserved only for special situations. The best method of operative treatment is still controversial and depends on different factors[8]. The Vancouver-classification is very useful in choosing the right treatment of these fractures. No doubt, fractures with unstable stems (B2)[9-12] should be treated by revision arthroplasty[13-15]. Fractures with a stable stem can be treated by osteosynthesis. However, the best way of stabilization is still controversial. Plate fixation[16-21], cerclages[22-24], and even external fixation[25,26] are described in the literature. Several studies have emphasized the advantage of locking screws. But the screw anchorage in the proximal fragment might be limited due to a mismatch between a big stem and thin cortical shell.
The strongest part in the proximal part is the prosthesis itself. Thus, the idea of an intraprosthetic screw fixation arises to enhance stability in the proximal part. The presented biomechanical study compares the stability of intraprosthetic screw fixation using glued liners inserted in either hip prostheses made of titanium alloy or cobalt chrome prostheses and locked plating in a simulated fracture model (Vancouver B1). We hypothesized significant higher fixation strength to axial loading in the intraprosthetic fixation groups.
The developing process of the intraprosthetic drill-machine has already been part of another publication[27]. High-performance cutting (HPC)-drills were used in this study that are strong and stable enough to provide optimal intraprosthetic drilling and connectivity to commonly used manual drilling machines in trauma surgery. Temperature control to tissue preserving levels during the drilling process was performed with the use of a custom made constantly applied internal cooling solution with a special transportation channel for removing the produced chips. The used liners were thread cut before inserting into prosthesis. To achieve optimal screw fitting thread cutting was performed using a regular thread cutter. They were then glued into the borehole after drilling the prosthesis using regularly used fibrin glue.
A total of twelve synthetic femurs (Sawbone Composite medium third generation, Pacific Research Labs Vashon Island, Washington, United States) were used instead of donor bones because of their availability and their equal shape and mechanical characteristics. A conventional straight stem prosthesis (Ecofit, Fa. Implantcast, Buxtehude, Germany) was implanted in each femur using bone cement for implantation to provide equal primary stability of the stems among all femurs. Titanium stems were used in eight femurs; prostheses made from chrome-molybdenum were implanted in four femurs.
The femurs were osteotomized 15 mm below the tip of the stem to create a Vancouver type C periprosthetic fracture. The screw fixation in the proximal part of the femur was our point of interest. The distal femur was abandoned and not involved in the study. We chose a commercial titanium locking plate (9-hole Less Invasive Stabilization System, Synthes, West Chester, United States) for the fixation. This locking plate is recommended for periprosthetic fractures of the femur and was tested in different studies[17,28,29]. Specially designed periprosthetic screws (ø 4 and 5 mm Periprosthetic Locking Screws, Synthes, West Chester, United States) are available to increase the number of threads within the unicortical fixation.
The company provided us with screw blanks, which had the threaded locking head but a non-manufactured shaft. We customised threads that fitted to the threads of the liners within the prosthesis.
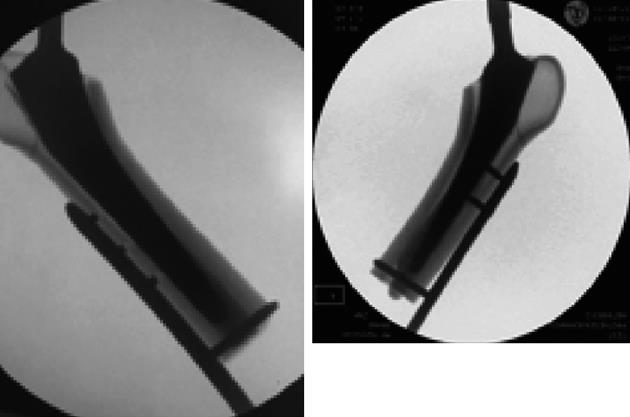
In the control group the locking plate was fixed with three unicortical locking screws implanted at the level of the prosthesis made from titanium alloy and one solid bicortical locking screw below the tip of the cemented stem (Figure 1).
In the experimental group with implanted titanium prostheses the locking plate was fixed with the same bicortical screw configuration beneath the tip of the prosthesis. At the level of the prosthesis only two intraprosthetic screws were implanted instead of the three unicortical screws (Figure 1). After drilling two holes at the level of the prosthesis (insertion depth 10 mm), the liners were inserted using fibrin glue. The internal thread was made for the reception of 4 mm locking screws. Due to the insertion of the screw the liners spread and clamped the bore channel. In the third group with cobalt chrome prostheses the fixation technique was similar to the one described in the first experimental group. The screws were inserted with the commercial torque wrench.
The distal plate end was fixed in a specially designed cup with locking screws to provide maximum stability during testing (Figure 2). An insertion angle of 6 degrees valgus was chosen following the mechanical axis of the femur of the leg.
Tests were performed with the prepared specimens mounted in a universal testing machine using a custom made locking screw device for the less invasive stabilization system (LISS)-plate fixation (Zwick Z250, Zwick, Ulm, Germany) (Figure 2). A standard commercially available metal head (32 mm) was placed at the top of the implanted prosthesis. A constantly increasing load was applied to the metal head in the anatomical axis of the femur with a starting force of 0 nm. The applied force was continuously measured and recorded. Reversible (elastic) and irreversible (plastic) deformation was expected. Elastic during the continuously load increase and plastic at the primary endpoint with either plastic deformity of the LISS plate or an irreversible loss of integrity of the whole locking plate fixation with avulsion of the locking screws.
The loads to failure values were evaluated using a student’s t-test. The following null-hypothesis was set: Equality of all tested fixation techniques regarding maximum axial load forces and failure of the locking screws. A value of P < 0.05 was chosen.
RESULT
The intraprosthetic group with straight stems made of titanium and inserted threaded liners failed at an average of 10 456 N ± 1892 N, the group with cobalt chrome stems and liners failed at an average of 9781 N ± 2323 N. The control group failed at an average of 7649 N ± 653 N. There was a significant difference found between the control group and the experimental group with liners and hip stems made of titanium alloy (P < 0.05). There was no significant difference between the control group and the other experimental group with the cobalt chrome stems (P > 0.05).
All drillings were successfully done without any problems in tapping, insertion or locking. No hardware failure occurred during implantation. In all tested devices in the control group a loss of fixation integrity at the level of the implanted prosthesis was observed. A total blow out of all unicortical screws was seen in 3 of 4 tested devices in this group.
There was no such hardware failure in the first experimental group; increase of axial loading lead to a bowing in the plate device in these cases rather than to a blow out of the liner-screw construct at the level of the prostheses. Differently, in the second experimental group with the cobalt chrome prostheses a loss of integrity at implant level was observed in two constructs at maximum axial loading.
This study was performed to compare different fixation techniques for the treatment of Vancouver type B1 periprosthetic fractures of the proximal femur. The most important finding of our study was that intraprosthetic screw fixation provided significantly higher failure loads compared to unicortical locked-screw plating in the titanium alloy fixation group. There were no significant differences between the control group and the second experimental group using cobalt chrome stems. Reasons for the different axial loads between the two experimental groups are plausibly caused by the differences between the materials used. Both, drilling the channel and inserting the liner with its clip function do work better in hip stems made of titanium alloy. Those implants are easier to process, drilling is easier to control and to perform, and caused by the lower level of stiffness and rigidity gluing and clipping the liner is more stable.
Intraprosthetic fixation leads to a significant increase in primary stability without weakening the implant-cement-femur-model that could lead to an early weight-bearing patient mobilization. Furthermore, we observed high standard deviations in both experimental groups compared to the control group. This seems to be caused by different positioning of the intraprosthetic screw. Although drilled with the use of fluoroscopy, there were still different results in screw fitting distance. This could explain the high standard deviation. Additionally, it shows the superiority of the intraprosthetic construct with reaching higher loading forces even with eccentric drilling and a reduced intraprosthetic screw fitting distance.
Limitations of the presented experimental biomechanical testing are the small number of cases in each group. Because of the study design and the comparability between both groups the number of cases seems to be large enough to produce useful results. The use of identical synthetic composites secures a high level of comparability between both groups. Additionally, compared to the thinner cortical strength of older osteoporotic bone the thicker cortical strength with the composite femurs is likely to be an advantage for the control group. Furthermore, the use of cement favors the control group by increasing the anchoring screws. With these tests the focus was only on the proximal fixation as weak point of locking screw fixation.
This new idea of intraprosthetic fixation in the treatment of periprosthetic fractures has not been published before. Presently, a variety of different operative treatments exist depending on the fracture location and stability of the stem[30]. Comparable extension forces have not been published before.
Dennis et al[30] presented a biomechanical review of five different fixation techniques. In axial loading tests plate constructs with proximal unicortical screws and distal bicortical screws were more stable than constructs with cables or plates and cables. In axial compression displacement in the most stable groups started at a maximum compression load of 4977 N. Other authors described satisfactory results with the use of simple conventional plating[2,31], angular stable internal fixation[17] or indirect reduction without grafting[19,20].
Especially with thinner, osteoporotic bone stock, intraprosthetic fixation could lead to an increase in primary stability. This technique might be even more superior in very osteoporotic femurs with a very small cortical shell. During testing even eccentric drilled screws in the prosthetic stem achieved significantly higher primary stability than the control group. A weakening of the implanted prosthesis actually appears implausible but not impossible. A main problem with intraprosthetic drilling might be the control of the heat development during drilling procedure and the transportation of the metal chips. With the use of custom-made continuously internally cooled HPC-drills with a special transportation channel, these problems might have been resolved.
The actual presented study has to been seen as a preliminary load to failure evaluation. Further studies are necessary to prove the mechanical integrity of the prosthesis and the bony anchorage of the prosthesis as well as the avoided temperature increase and the evacuation of the metal debris. Additionally, further testing should also focus on securing the optimal screw position for intraprosthetic anchorage to achieve the highest level of anchorage strength without weakening the prosthesis. Furthermore, one of the next steps will be the testing of the dynamic stability of the intraprosthetic screw fixation technique.
Intraprosthetic screw anchorage in titanium prostheses with special threaded liners enhances the primary stability in treating periprosthetic fractures by internal fixation.
The number of implanted hip prostheses is still increasing and so is the number of proximal femur fractures after total hip replacement. Fractures with an unstable hip stem are generally treated with revision arthroplasty and the use of a longer hip stem. For the treatment of fractures with a stable stem various techniques have been described, e.g., unicortical plate fixation, cerclages, struts, but none of them seems to be superior to the others. To improve the primary stability different intraprosthetic fixation techniques were tested for axial loading forces in this presented study.
Intraprostheitc screw fixation represents a new idea and technique to improve the primary stability in the treatment of periprosthetic fractures. Intraprosthetic fixation was achieved with the use of thread cut liners that were inserted into the drilling hole. The liners were then used like dowels.
New techniques of intraprosthetic screw fixation were described. Compared to the commonly used unicortical plate fixation the axial loading forces achieved were significantly higher in the experimental group using hip stems made of titanium alloy. There was no significant difference between the second experimental group using cobalt chrome prostheses. All drillings were done successfully without problems in drilling, inserting or locking. Although an experimental biomechanical study, the results could lead to a future change in the treatment of periprosthetic fractures to a significant increase in primary stability.
Intraprosthetic screw anchorage in titanium prostheses with special threaded liners enhances the primary stability in treating periprosthetic fractures by internal fixation. This could lead to a change in the treatment algorithm of periprosthetic fractures to allow early weight bearing and reduce the in-hospital morbidity with older patients.
Periprosthetic fracture describes a fracture of for example the proximal femur after the patient underwent total hip replacement. The treatment is depending on the stability of the implanted hip stem. Intraprosthetic screw anchorage describes a new technique of screw fixation were the bore hole is drilled into the prosthesis using a specially developed drill. Plate fixation and cerclages are different techniques in fracture treatment.
The authors present an interesting report of a novel fixation technique for periprosthetic fractures of the femur. With static loading, they show that the new technique is more stable than conventional plating in the titanium constructs. Because of its novelty, it might be interesting to readers.
Peer reviewers: Christiaan JA van Bergen, MD, Orthopaedic Research Center Amsterdam, Department of Orthopaedic Surgery, Academic Medical Center, Meibergdreef 9, 1105 AZ, Amsterdam, Netherlands; Hassan Serhan, PhD, Prestige Adjunct Professor, 325 Paramount Drive, Raynham, MA 02767, United States
S- Editor Huang XZ L- Editor Roemmele A E- Editor Lu YJ
| 1. | Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury. 2007;38:651-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 302] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 2. | Lewallen DG, Berry DJ. Periprosthetic fracture of the femur after total hip arthroplasty: treatment and results to date. Instr Course Lect. 1998;47:243-249. [PubMed] |
| 3. | Rayan F, Haddad F. Periprosthetic femoral fractures in total hip arthroplasty - a review. Hip Int. 2010;20:418-426. [PubMed] |
| 4. | Kavanagh BF. Femoral fractures associated with total hip arthroplasty. Orthop Clin North Am. 1992;23:249-257. [PubMed] |
| 5. | Della Rocca GJ, Leung KS, Pape HC. Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma. 2011;25 Suppl 2:S66-S70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 205] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 6. | Bhattacharyya T, Chang D, Meigs JB, Estok DM, Malchau H. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am. 2007;89:2658-2662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 293] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 7. | Franklin J, Malchau H. Risk factors for periprosthetic femoral fracture. Injury. 2007;38:655-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 160] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 8. | Ricci WM, Haidukewych GJ. Periprosthetic femoral fractures. Instr Course Lect. 2009;58:105-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Klein GR, Parvizi J, Rapuri V, Wolf CF, Hozack WJ, Sharkey PF, Purtill JJ. Proximal femoral replacement for the treatment of periprosthetic fractures. J Bone Joint Surg Am. 2005;87:1777-1781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Kolstad K. Revision THR after periprosthetic femoral fractures. An analysis of 23 cases. Acta Orthop Scand. 1994;65:505-508. [PubMed] |
| 11. | Ogawa H, Ito Y, Takigami I, Shimizu K. Revision total hip arthroplasty for a Vancouver type B3 periprosthetic fracture using an allograft-cemented stem composite by the telescoping technique. J Arthroplasty. 2011;26:665.e625-e665.e628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Rayan F, Konan S, Haddad FS. Uncemented revision hip arthroplasty in B2 and B3 periprosthetic femoral fractures - A prospective analysis. Hip Int. 2010;20:38-42. [PubMed] |
| 13. | Ries MD. Intraoperative modular stem lengthening to treat periprosthetic femur fracture. J Arthroplasty. 1996;11:204-205. |
| 14. | Springer BD, Berry DJ, Lewallen DG. Treatment of periprosthetic femoral fractures following total hip arthroplasty with femoral component revision. J Bone Joint Surg Am. 2003;85-A:2156-2162. [PubMed] |
| 15. | Tsiridis E, Narvani AA, Haddad FS, Timperley JA, Gie GA. Impaction femoral allografting and cemented revision for periprosthetic femoral fractures. J Bone Joint Surg Br. 2004;86:1124-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Frankie L, Xiang Z. [Locking compression plate fixation for periprosthetic femoral fracture]. Zhongguo Xiu Fu Chong Jian Wai Ke Zazhi. 2002;16:123-125. [PubMed] |
| 17. | Kääb MJ, Stöckle U, Schütz M, Stefansky J, Perka C, Haas NP. Stabilisation of periprosthetic fractures with angular stable internal fixation: a report of 13 cases. Arch Orthop Trauma Surg. 2006;126:105-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 49] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Radcliffe SN, Smith DN. The Mennen plate in periprosthetic hip fractures. Injury. 1996;27:27-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Ricci WM, Bolhofner BR, Loftus T, Cox C, Mitchell S, Borrelli J. Indirect reduction and plate fixation, without grafting, for periprosthetic femoral shaft fractures about a stable intramedullary implant. Surgical Technique. J Bone Joint Surg Am. 2006;88 Suppl 1 Pt 2:275-282. [PubMed] |
| 20. | Ricci WM, Loftus T, Cox C, Borrelli J. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma. 2006;20:190-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 157] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 21. | Tarnowski JR, Holck K. Osteosynthesis of a periprosthetic fracture of the proximal femur with the distal femur LISS system. Acta Orthop Belg. 2008;74:125-127. [PubMed] |
| 22. | Haddad FS, Marston RA, Muirhead-Allwood SK. The Dall-Miles cable and plate system for periprosthetic femoral fractures. Injury. 1997;28:445-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 47] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Tadross TS, Nanu AM, Buchanan MJ, Checketts RG. Dall-Miles plating for periprosthetic B1 fractures of the femur. J Arthroplasty. 2000;15:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 69] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Venu KM, Koka R, Garikipati R, Shenava Y, Madhu TS. Dall-Miles cable and plate fixation for the treatment of peri-prosthetic femoral fractures-analysis of results in 13 cases. Injury. 2001;32:395-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Pafilas D, Kourtzis N. Hybrid external fixation as a new treatment method for periprosthetic femoral fracture. A case report. J Bone Joint Surg Am. 2006;88:188-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Sakai T, Ohzono K, Nakase T, Lee SB, Manaka T, Nishihara S. Treatment of periprosthetic femoral fracture after cementless total hip arthroplasty with Ilizarov external fixation. J Arthroplasty. 2007;22:617-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Klotz J. Developing a special drill for intraprosthetic screw fixation. Hannover: Leibniz University Hannover 2011; . |
| 28. | Müller M, Kääb M, Tohtz S, Haas NP, Perka C. Periprosthetic femoral fractures: outcome after treatment with LISS internal fixation or stem replacement in 36 patients. Acta Orthop Belg. 2009;75:776-783. [PubMed] |
| 29. | Krettek C, Schandelmaier P, Richter M, Tscherne H. [Distal femoral fractures]. Swiss Surg. 1998;263-278. [PubMed] |
| 30. | Dennis MG, Simon JA, Kummer FJ, Koval KJ, DiCesare PE. Fixation of periprosthetic femoral shaft fractures occurring at the tip of the stem: a biomechanical study of 5 techniques. J Arthroplasty. 2000;15:523-528. [PubMed] |
| 31. | Siegmeth A, Menth-Chiari W, Wozasek GE, Vécsei V. [Periprosthetic femur shaft fracture. Indications and outcome in 51 patients]. Unfallchirurg. 1998;101:901-906. [PubMed] |