Published online Jul 18, 2025. doi: 10.5312/wjo.v16.i7.108319
Revised: April 27, 2025
Accepted: June 3, 2025
Published online: July 18, 2025
Processing time: 95 Days and 19.4 Hours
Hereditary multiple exostoses (HME) is an autosomal dominant bone disorder characterized by abnormal bone development. HME mostly involves the forearm, resulting in forearm deformities, limited functional activities, etc. Currently, there are multiple surgical methods including tumor resection with or without ulnar osteotomy and lengthening, simple radial head resection and distal radial hemiepiphysiodesis, but the optimal treatment remains controversial. Ulnar lengthening serves as an effective surgical intervention for forearm deformities in HME patients. This review examines its surgical techniques, complications, and timing of the operation to guide clinical decision-making for improving function and cosmetic outcomes.
Core Tip: This article provides a concise overview of the epidemiology, pathogenesis, and clinical features of hereditary multiple exostoses (HME), focusing on the surgical technique of ulnar lengthening for forearm deformities. It discusses integration with corrective procedures, postoperative complications, and optimal intervention timing. Through a systematic review, the study concludes that ulnar lengthening is a widely recognized and effective treatment for forearm deformities in children with HME.
- Citation: Wang S, Liu HR, Zou KT, Gao F, Wang SY, Mutasa B, Li J, Hong P. Ulnar lengthening in the treatment of forearm deformity caused by hereditary multiple exostoses in children. World J Orthop 2025; 16(7): 108319
- URL: https://www.wjgnet.com/2218-5836/full/v16/i7/108319.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i7.108319
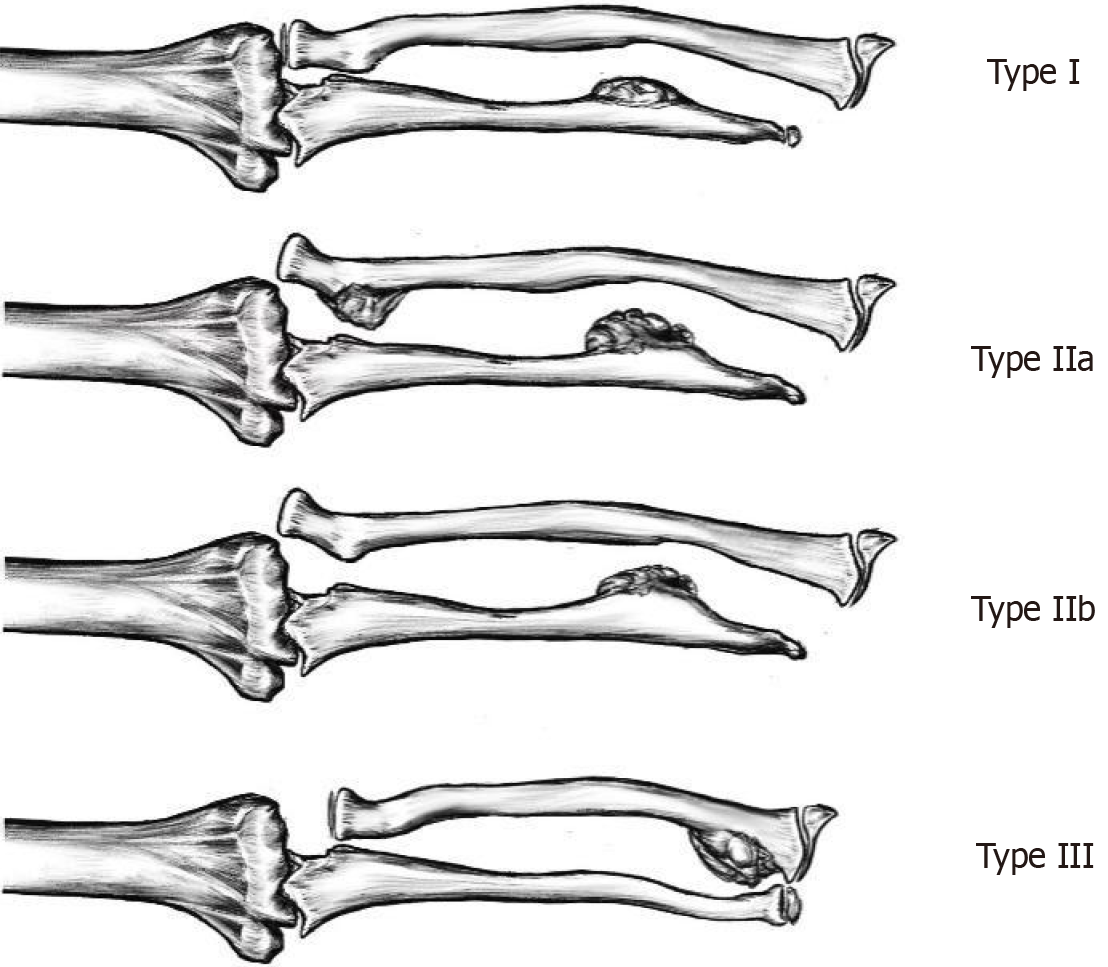
Hereditary multiple exostoses (HME) is an autosomal dominant disorder of the skeletal system with an estimated incidence of approximately 1/50000[1]. HME is mainly associated with mutations in the EXT1 and EXT2 genes[2-4]. Approximately, 30%-60% of HME patients have forearm deformities, including ulnar shortening, ulnar/radial bowing, ulnar deviation of the wrist joint, and radial head dislocation[5-7]. These deformities not only affect the appearances, but also lead to localized pain and limited function of the forearm. For forearm deformities caused by HME, Masada et al[8] proposed a clinical classification in 1989, which has been widely accepted and employed in academic publications (Figure 1). There are numerous surgical options for forearm deformity, including tumor resection with or without ulnar osteotomy and lengthening, simple radial head resection, and distal radial hemiepiphysiodesis, but the optimal option remains controversial[9,10].
The forearm deformity of HME is primarily attributable to the shortening of the ulna, resulting in an imbalance of length ratio between ulna and radius. Since 1970s, scholars have reported the application of one-time ulnar lengthening to correct ulnar shortening deformity[8,11,12]. However, vascular and neurological complications as well as non-union of osteotomy site have been reported in patients receiving one-time lengthening procedures. As the Ilizarov technique became popular, progressive ulnar lengthening is gaining momentum and has been widely reported ever since[12-14]. Surgical intervention restores the normal axis of the forearm by lengthening the shortened ulna, and concomitantly, it can reduce the dislocated radial head and thereby improve the function of forearm[15-17]. This paper presents a review of the application of ulnar lengthening in correcting forearm deformity due to HME.
HME is an autosomal dominant disorder, with approximately 90% of cases stemming from mutations in the EXT1 and EXT2 genes[18,19]. Molecular mechanism studies have shown that EXT gene mutations affect heparan sulfate (HS) synthesis by impairing cell surface HS proteoglycan biosynthesis. It further interferes with fibroblast growth factor and other signaling pathways, and ultimately triggers abnormal chondrocyte proliferation and the formation of exophytic osteochondroma[20]. Exostoses usually grow in the metaphyses of long bones or on the surfaces of flat bones, causing pain by irritating and compressing adjoining structures. Because it grows in the neighbourhood of joints, it often interferes with the movement of the joints[21,22]. Osteochondromas involving the growth plate interfere with normal bone development, and disproportionate bone shortening usually leads to poor joint alignment and limb deformity[23]. In the forearm, the imbalance in growth between the radius and ulna further leads to functional limitations of the forearm and elbow, bowing deformities of the ulnar radius, and dislocation of the radial head.
Currently, there is no unanimous recommendation about the site of ulnar osteotomy. Iba et al[24] based on the analysis of the anatomical structure of the interosseous membrane, concluded that the distance between the osteotomy site and the distal end of the ulna should not be less than 42% of the total length of the ulna, and at the same time, chose the site of the largest bowing arc in order to better correct the ulnar deformity and possibly reduce the dislocated radial head indirectly. Li et al[25] found that the diameter of the ulna at the site of osteotomy was negatively correlated with the time of bone healing at the site of osteotomy, that is, proximal ulna osteotomy was favourable to the healing of the bone. Latest studies[26,27] pointed out that the ulnar osteotomy site should be selected between 1/4 and 1/3 of the proximal ulna for faster healing after osteotomy[28].
One-time ulnar osteotomy lengthening includes transverse, oblique, or stepped osteotomy approach, and bone grafting might be performed and usually plate is used to maintain the length[8]. However, progressive lengthening mostly uses transverse osteotomy.
One-time ulnar osteotomy lengthening is a procedure that is primarily applicable for lengthening less than 20 mm. Excessive lengthening may result in neurological and vascular complications[29].
Progressive ulnar lengthening is widely used in clinical practice, with longer elongation than one-time lengthening without severe neurovascular complications[30]. Chomiak et al[29] recommended ulnar lengthening in combination with internal fixation using a single intramedullary elastic nail, which provided significant benefits in terms of bone elongation, bone healing index, and complication rates. Progressive ulnar lengthening is usually initiated 5-7 days after osteotomy surgery, with a lengthening rate of 1 mm/day[14,27,30,32]. Abe et al[33] stated that in patients of simultaneous lengthening of the radius and ulna, dependent on the age of the patient, lengthening should be initiated 1 or 2 weeks after osteotomy, at a rate of 0.25 mm every 12 hours in ulna and of 0.175 mm every 12 hours in radius.
There is no consensus on the optimal length of ulnar lengthening. Pritchett reported the results of 10 cases of ulnar lengthening, and he recommended over-correction in younger patients prior to skeletal maturity because of a higher tendency for recurrence in younger patients[15]. However, Vogt et al[34] contend that excessive lengthening increases the risk of ulnocarpal impaction syndrome and caution against prophylactic ulnar overlengthening. Recent studies reported that the proportional length of the ulnar radius can be used as a reference index for the amount of ulnar lengthening in children with HME. Huang et al[10] proposed that ulnar lengthening guided by the normal ulnar-to-radial length ratio (approximately 1.1:1) achieved satisfactory postoperative improvements in forearm cosmetic and functional outcomes, with no recurrence of radial head dislocation during follow-up and effective prevention of wrist impingement. During the lengthening process, timely follow-up is critical, complemented by functional assessments to monitor range of motion and wrist stability. Additionally, proactive management of pin-site infections and regular long-term follow-up are essential to minimize complications and facilitate early detection of recurrence.
Ilizarov frame: Ilizarov frame was widely used in the progressive lengthening of the ulna in HME forearm deformity and satisfactory results have been reported[33,35-37]. Its advantages include: (1) Good mechanical stability, ensuring that the osteotomy end remains stable during lengthening; (2) Multiplanar deformity correction; and (3) Effectiveness of radial head reduction[10,38-40]. Huang et al[10] used Ilizarov frame to lengthen the ulna by firstly pulling the radial head down to the level of the ulnar coronoid process through the Kirschner wire at the distal ring, and then restoring the proportional length of the ulna by lengthening the ulna, which resulted in postoperative radial head reduction in over 90% of cases.
The disadvantages of using Ilizarov frame for this condition include: (1) Structural complexity, requiring higher level of skill for the surgeon, and probably prolonging the operative time; (2) Patient comfort: Complex frames may interfere with patients' daily activities, especially in children, which may lead to inconvenience and discomfort; and (3) Difficulty in daily care: Ilizarov frames are bulky in size, which makes it inconvenient for family members to take care of them.
Unilateral external fixation device: Many studies have used unilateral or monolateral external fixation frames for forearm deformity in HME and achieved satisfactory outcomes[7,36,41,42]. It has been widely adopted due to its smaller size, relatively lower price, and easier postoperative care. However, its limited ability to correct ulnar angulation deformity resulted in limited chance of simultaneous radial head reduction[24,34]. Litzelmann et al[43] used ulnar lengthening with unilateral external fixation frame to treat patients with HME forearm deformity associated with radial head dislocation, and in 2 out of 5 cases (40%), the radial head failed to reduce naturally at the end of lengthening process.
According to Ahmed[38], a ring external fixation frame is preferred for patients with HME forearm deformity with radial head dislocation. Both the radius and ulna were fixed with transverse wires in the distal ring. Concurrently, the radius was gradually distracted distally during ulnar lengthening. In patients with HME forearm deformity without radial head dislocation, a unilateral external fixator is preferred for lengthening.
Application of internal fixation: Internal fixation should be used in cases of delayed healing of the osteotomy site after one-time ulnar osteotomy or progressive ulnar osteotomy lengthening. After osteotomy, a plate can be used to stabilize the osteotomy site[8]. Launay et al[44] reported a method of ulna lengthening using a unilateral external fixator combined with elastic stable intramedullary nail (ESIN). Ten children were treated by this method and satisfactory results were achieved. ESIN served as axial guide during the ulnar elongation process, and reduced the risk of delayed union or non-union of the osteotomy site. However, secondary surgery for removing the intramedullary nail could be challenging because it might be buried beneath the bone as healing progresses. In some cases, we could consider leaving the nail in place so it remains for potential future lengthening procedures[44]. If removal is necessary, employing advanced imaging guidance such as computed tomography scan, and longer incision might enhance the success of nail removal. Additional surgery as plating could also be performed if delayed or non-union was observed in patient receiving ulnar lengthening using external fixator alone[16,24].
In addition, correction of forearm deformity can be performed in combination with osteochondroma excision, distal radial hemiepiphysiodesis, and radial osteotomy. Hsu et al[32] suggested that osteochondroma excision is feasible for tumor located near the epiphysis that are palpated as a prominent mass with compression pain. Plenty studies have reported satisfactory outcomes in patients receiving osteochondroma resection combined with progressive ulnar lengthening[32,36,45]. It has been suggested that resection of osteochondroma prior to the correction of ulnar shortening and deformity may reduce the risk of recurrence of ulnar shortening and radial head dislocation[27,46].
Kelly and James[47] reported the results of distal radial hemiepiphysiodesis surgery in 16 children with HME. Follow-up demonstrated significant improvement in the ulnar deviation angle of the distal radius in these children. Hemiepiphysiodesis procedure depends on the growth potential and it is difficult to fine-tune accordingly even with regular postoperative follow-up. Ulnar lengthening combined with corrective radial osteotomy is able to treat radial bowing deformity and improve the appearance and function of the forearm[17,48]. It has been suggested that progressive ulnar lengthening alone helps to correct radial deformity, which is related to bone remodeling in children[7,49]. In a study by Hsu et al[32], improvement in radial deformity was observed in patients (≤ 10 years old) who did not undergo corrective radial osteotomy. They concluded that for children under 10 years of age with HME, progressive ulnar lengthening alone suffices; for children older than 10 years of age, progressive ulnar lengthening combined with corrective radial osteotomy is feasible.
The Sauvé-Kapandji procedure is widely used in the treatment of various distal ulnar-radial joint anomalies. Taleisnik[50] suggested that this procedure minimized the likelihood of some of the complications that can occur after excising the ulna. Shin et al[51] reported that the Sauvé-Kapandji procedure was effective in improving postoperative forearm rotational function. Postoperative measurements showed that patients had a mean improvement of 11.4° in supination and a 21.4° increase in pronation. In cases of combined distal radial/ulnar osteochondroma, tumor resection was performed concurrently in both bone of forearm. Postoperative imaging showed significant improvement in radial articular angle and carpal slip.
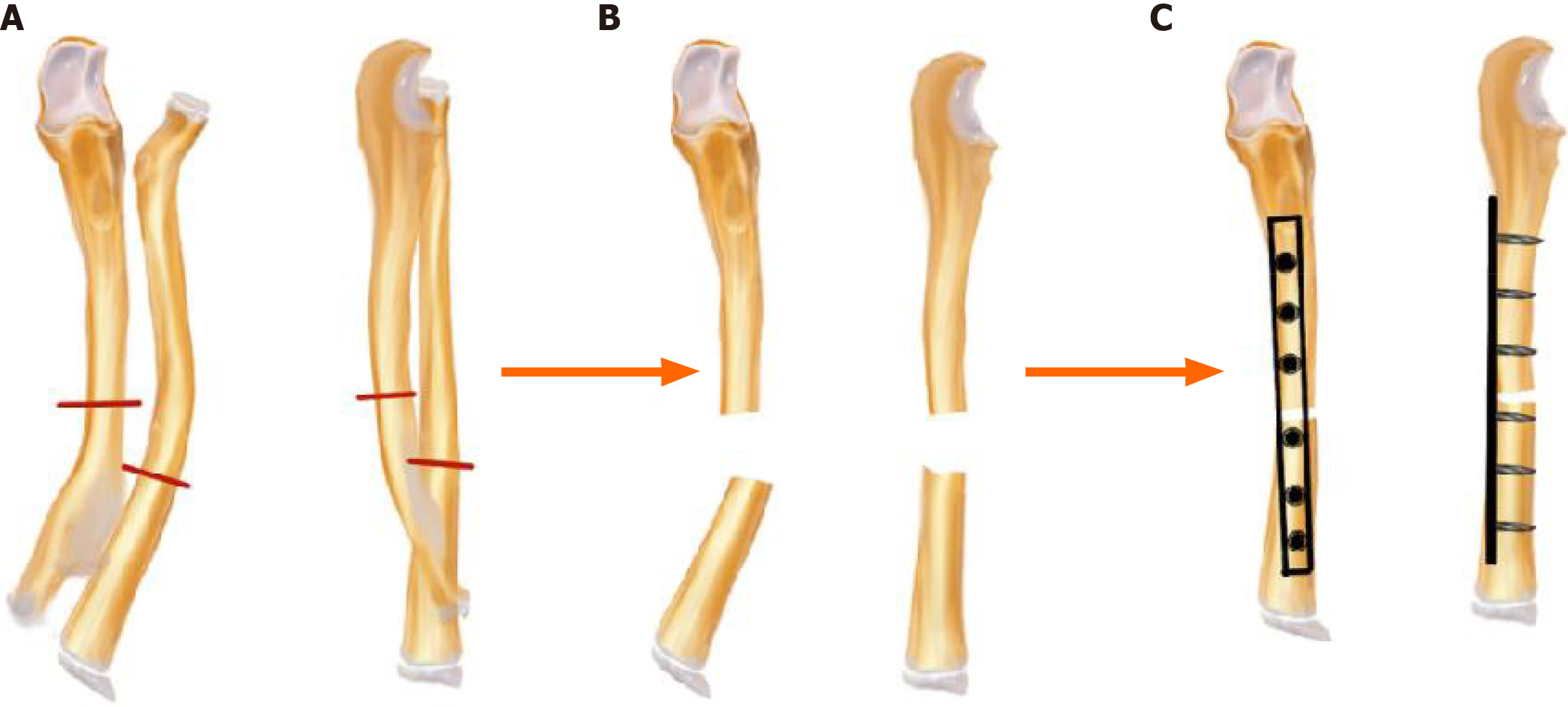
Certain scholars suggested that Masada type II patients with severe deformity of the forearm in skeletal mature patients may be candidate for one-bone forearm (OBF), which consists of resection of the proximal radius and distal ulna, fusion of the proximal ulna to the distal radius, and preservation of the proximal ulnar-humeral and distal radial-wrist joints[52-54]. OBF is a salvage procedure that preserves the critical ulnar-radial bone structures based on achieving a balance between functional reconstruction and morphological restoration[55]. The surgical steps are shown in the Figure 2[53].
Surgical complications mainly include pin tract infection, tumor recurrence, recurrence of ulnar shortening deformity, re-dislocation of the radial head, delayed healing, non-union and deformed union of the osteotomy site.
Pin track infection is a common but minor complication of ulnar lengthening using external fixation devices[14,56]. Standardized postoperative care education with regular dressing changes is important to reduce the infections. If infection is observed, oral antibiotics should be taken promptly.
Regarding tumor recurrence[57,58] the main reason for the recurrence of osteochondroma after surgery is that the cartilage cap is not completely removed. However, extensive resection may damage the physis, and therefore surgeon’s discretion is required during the operation without violating the growth plate[46].
Ulnar shortening recurrence is common in skeletally immature, younger children. This recurrence arises from persistent growth imbalance or insufficient surgical correction, leading to relative shortening of the ulna compared to the radius and associated forearm deformities. Therefore, it can be over-corrected by 5-10 mm in progressive ulnar lengthening[18,29,38] or in a secondary lengthening procedure. In patients with radial head re-dislocation, skeletal maturity should be thoroughly evaluated. In children with skeletal maturity or developmental deformity of the radial head, salvage surgery such as radial head resection, can be performed to alleviate the patient's symptoms. In younger children, secondary lengthening to reduce the radial head may be plausible. Currently, there remains a paucity of large-scale multicenter studies addressing the thresholds for secondary lengthening procedures. Existing criteria are predominantly based on clinicians' empirical judgment, such as persistent relative ulnar shortening, incomplete reduction of radial head dislocation, chronic pain, or restricted joint mobility following primary lengthening. Future prospective studies are imperative to validate the efficacy of these criteria, thereby mitigating risks of overcorrection and unnecessary surgical interventions.
Delayed healing or non-union of the osteotomy site is a serious complication after progressive ulna lengthening, characterized by failure of the osteotomy site to form a continuous callus or complete absence of osseous union. Catagni et al[59] noted that the lengthening rate in the upper extremity may be slower than that in the lower extremity (1 mm per day) when using progressive lengthening. Yasui et al[60] found in animal experiments, that starting lengthening within 2 weeks after the osteotomy was associated with a low risk of bone nonunion, while starting lengthening over 2 weeks after surgery significantly increased the risk of bone nonunion. During the appropriate latency period, the vascular damage within the bone marrow caused by osteotomy can be effectively recovered, thus facilitating the healing of the osteotomy site. In addition, faster lengthening rate is detrimental to the healing of the osteotomy site. During the lengthening process, regular X-rays are required to assess the growth and mineralization of the bone, and adjustments to the distraction rate may be necessary to mitigate this risk. In cases where delayed healing or non-union occurs, treatments include removal of the external fixation device, autologous iliac bone grafting, and replacement of the plate for internal fixation[16,24]. Lu et al[27] showed one case of delayed healing during elongation, and satisfactory outcome achieved after a period of repetitive traction-compression (accordion technique). In addition, intramedullary nail fixation (which can be combined with autologous bone grafting) is also an effective option[61]. Paley[56] concluded that the upper limb lacked stress stimulation during progressive lengthening, and that the mineralization process of the bone is slower than that in the lower limb. Therefore, premature removal of the external fixation frame may lead to deformed healing. Neurovascular injuries may result in localized motor dysfunction in the forearm, sensory paralysis, and delayed healing at the surgical site. Abe et al[33] demonstrated that the neurovascular injuries depend on the type of external fixator, as such injuries are common with the use of ring frames but rare in unilateral fixator.
There is still controversy about the optimal timing of surgical intervention. Several studies have recommended early and aggressive treatment for forearm deformities to avoid progression of the deformity and forearm dysfunction[34,62-64]. Jo et al[65] suggested that when the ulnar-radial length ratio is less than 0.9 or radial curvature (maximum distance of the radial styloid deviation from the long axis of the forearm divided by the percentage of the length of the radius) is greater than 8.1%, the risk of radial head dislocation is high and that early intervention can prevent the progression of radial head dislocation. According to Ahmed[38], early intervention is also important to achieve natural reduction of the radial head. However, surgical intervention does not change the underlying disease[51], and the problem of postoperative recurrence in skeletally immature pediatric patients cannot be ignored. The risk of radial head re-dislocation is higher in younger patients[33,34,66]. Some authors have suggested postponing surgery to avoid recurrence[31,67]. The importance of calculating the optimal time for surgery was noted by Ip et al[48], who suggested that close to skeletal maturity is the best time for surgery. Masada et al[8] recommend early surgery to take the advantage of greater remodeling potential. However, the younger the patient, the greater the risk of recurrence. Multiple risk factors for radial head dislocation in patients with HME have been reported[68,69], and these risk factors include ulnar length ratio (ulnar-radial ratio on radiographs), ulnar curvature, radial curvature, and the number/Location of osteochondromas (tumors of the distal ulna have been associated with the development of radial head dislocation). This has important implications for early surgical intervention to prevent radial head dislocation. An earlier study[30] supports early surgery in patients with radial head dislocation, and surgery before the age of 10 years can better correct the forearm deformity. Patients with non-dislocated radial head can be closely followed up for observation and operated in the neighborhood of skeletal maturity.
In summary, the efficacy of ulnar lengthening in the treatment of forearm deformities in children due to HME is widely accepted. Furthermore, all aspects of the ulnar lengthening process are critical to the success of this procedure. A better understanding of the indications for surgery as well as surgical technique and timing is required. The deformities of radial flexion, ulnar deviation of the wrist and radial head dislocation due to HME can be better corrected by combining with other surgical procedures.
| 1. | Rueda-de-Eusebio A, Gomez-Pena S, Moreno-Casado MJ, Marquina G, Arrazola J, Crespo-Rodríguez AM. Hereditary multiple exostoses: an educational review. Insights Imaging. 2025;16:46. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Wuyts W, Van Hul W, De Boulle K, Hendrickx J, Bakker E, Vanhoenacker F, Mollica F, Lüdecke HJ, Sayli BS, Pazzaglia UE, Mortier G, Hamel B, Conrad EU, Matsushita M, Raskind WH, Willems PJ. Mutations in the EXT1 and EXT2 genes in hereditary multiple exostoses. Am J Hum Genet. 1998;62:346-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 136] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Burgess RC, Cates H. Deformities of the forearm in patients who have multiple cartilaginous exostosis. J Bone Joint Surg Am. 1993;75:13-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 50] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Jones KB, Pacifici M, Hilton MJ. Multiple hereditary exostoses (MHE): elucidating the pathogenesis of a rare skeletal disorder through interdisciplinary research. Connect Tissue Res. 2014;55:80-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Schmale GA, Conrad EU 3rd, Raskind WH. The natural history of hereditary multiple exostoses. J Bone Joint Surg Am. 1994;76:986-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 390] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 6. | Clement ND, Porter DE. Forearm deformity in patients with hereditary multiple exostoses: factors associated with range of motion and radial head dislocation. J Bone Joint Surg Am. 2013;95:1586-1592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | D'Ambrosi R, Barbato A, Caldarini C, Biancardi E, Facchini RM. Gradual ulnar lengthening in children with multiple exostoses and radial head dislocation: results at skeletal maturity. J Child Orthop. 2016;10:127-133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Masada K, Tsuyuguchi Y, Kawai H, Kawabata H, Noguchi K, Ono K. Operations for forearm deformity caused by multiple osteochondromas. J Bone Joint Surg Br. 1989;71:24-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 94] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Zheng C, Han H, Cao Y. Older age and multi-joint external fixator are two risk factors of complications in ulnar lengthening in children with hereditary multiple exostosis. J Orthop Surg Res. 2020;15:555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Huang P, Zhu L, Ning B. Forearm Deformity and Radial Head Dislocation in Pediatric Patients with Hereditary Multiple Exostoses: A Prospective Study Using Proportional Ulnar Length as a Scale to Lengthen the Shortened Ulna. J Bone Joint Surg Am. 2020;102:1066-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Wuyts W, Schmale GA, Chansky HA, Raskind WH. Hereditary Multiple Osteochondromas. 2000 Aug 3. In: GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–. [PubMed] |
| 12. | Baghdadi S, Arabi H, Farhoud A, Moharrami A, Baghdadi T. Clinical and Functional Outcomes of Ulnar Lengthening in the Treatment of Masada Type I Forearm Deformities in Hereditary Multiple Osteochondromas. J Hand Surg Am. 2020;45:876.e1-876.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | El-Sobky TA, Samir S, Atiyya AN, Mahmoud S, Aly AS, Soliman R. Current paediatric orthopaedic practice in hereditary multiple osteochondromas of the forearm: a systematic review. SICOT J. 2018;4:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Hill RA, Ibrahim T, Mann HA, Siapkara A. Forearm lengthening by distraction osteogenesis in children: a report of 22 cases. J Bone Joint Surg Br. 2011;93:1550-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Pritchett JW. Lengthening the ulna in patients with hereditary multiple exostoses. J Bone Joint Surg Br. 1986;68:561-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 68] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Akita S, Murase T, Yonenobu K, Shimada K, Masada K, Yoshikawa H. Long-term results of surgery for forearm deformities in patients with multiple cartilaginous exostoses. J Bone Joint Surg Am. 2007;89:1993-1999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Matsubara H, Tsuchiya H, Sakurakichi K, Yamashiro T, Watanabe K, Tomita K. Correction and lengthening for deformities of the forearm in multiple cartilaginous exostoses. J Orthop Sci. 2006;11:459-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Bukowska-Olech E, Trzebiatowska W, Czech W, Drzymała O, Frąk P, Klarowski F, Kłusek P, Szwajkowska A, Jamsheer A. Hereditary Multiple Exostoses-A Review of the Molecular Background, Diagnostics, and Potential Therapeutic Strategies. Front Genet. 2021;12:759129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 19. | Yuan G, Su Q, Liao W, Hou W, Huang L, Wang P, Wu H. Mutational Analysis of EXT1in a Chinese Family Affected by Hereditary Multiple Osteochondroma. Biomed Res Int. 2021;2021:8888948. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Pacifici M. Hereditary multiple exostoses: are there new plausible treatment strategies? Expert Opin Orphan Drugs. 2018;6:385-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Clement ND, Porter DE. Hereditary multiple exostoses: anatomical distribution and burden of exostoses is dependent upon genotype and gender. Scott Med J. 2014;59:35-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Mundy C, Chung J, Koyama E, Bunting S, Mahimkar R, Pacifici M. Osteochondroma formation is independent of heparanase expression as revealed in a mouse model of hereditary multiple exostoses. J Orthop Res. 2022;40:2391-2401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Beltrami G, Ristori G, Scoccianti G, Tamburini A, Capanna R. Hereditary Multiple Exostoses: a review of clinical appearance and metabolic pattern. Clin Cases Miner Bone Metab. 2016;13:110-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 24. | Iba K, Hanaka M, Ozasa Y, Takahashi N, Kanaya K, Yamashita T. Treatment of forearm deformity with radial head dislocation because of multiple osteochondromas: a series of three cases treated by simple axis correction and distraction osteogenesis of the ulna. J Pediatr Orthop B. 2018;27:315-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Li Y, Han B, Tang J, Chen M, Wang Z. Identification of risk factors affecting bone formation in gradual ulnar lengthening in children with hereditary multiple exostoses: A retrospective study. Medicine (Baltimore). 2019;98:e14280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Yan G, Nan G. Modified osteotomy for treatment of forearm deformities (Masada IIb) in hereditary multiple osteochondromas: a retrospective review. BMC Musculoskelet Disord. 2021;22:943. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 27. | Lu Y, Canavese F, Lin R, Huang Y, Wu X, Lin B, Chen S. Distraction osteogenesis at the proximal third of the ulna for the treatment of Masada type I/IIb deformities in children with hereditary multiple exostoses: a retrospective review of twenty cases. Int Orthop. 2022;46:2877-2885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Khan SN, Cammisa FP Jr, Sandhu HS, Diwan AD, Girardi FP, Lane JM. The biology of bone grafting. J Am Acad Orthop Surg. 2005;13:77-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 496] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 29. | Chomiak J, Ošťádal M, Frydrychová M, Dungl P. Lengthening of the ulna by callotasis in children with multiple hereditary exostoses: comparison of methods with and without internal fixation. J Child Orthop. 2021;15:378-387. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Wang S, Herman B, Wu Y, Lei M, Mutasa B, Hong P, Li J. Ulnar lengthening for children with forearm deformity from hereditary multiple exostoses: a retrospective study from a tertiary medical center. BMC Pediatr. 2024;24:585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 31. | Ham J, Flipsen M, Koolen M, van der Zwan A, Mader K. Multiple osteochondromas (MO) in the forearm: a 12-year single-centre experience. Strategies Trauma Limb Reconstr. 2016;11:169-175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 32. | Hsu PJ, Wu KW, Lee CC, Kuo KN, Chang JF, Wang TM. Less Is More: Ulnar Lengthening Alone without Radial Corrective Osteotomy in Forearm Deformity Secondary to Hereditary Multiple Exostoses. J Clin Med. 2019;8:1765. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Abe M, Shirai H, Okamoto M, Onomura T. Lengthening of the forearm by callus distraction. J Hand Surg Br. 1996;21:151-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 50] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 34. | Vogt B, Tretow HL, Daniilidis K, Wacker S, Buller TC, Henrichs MP, Roedl RW, Schiedel F. Reconstruction of forearm deformity by distraction osteogenesis in children with relative shortening of the ulna due to multiple cartilaginous exostosis. J Pediatr Orthop. 2011;31:393-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 35. | Zhou M, Zhang P, Liu X, Tan M, Shi Z. Ilizarov technique for the treatment of hereditary multiple exostoses: A case report. Asian J Surg. 2024;S1015-9584(24)01646. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 36. | Demir B, Gursu S, Ozturk K, Yildirim T, Konya MN, Er T. Single-stage treatment of complete dislocation of radial head and forearm deformity using distraction osteogenesis in paediatric patients having multiple cartilaginous exostosis. Arch Orthop Trauma Surg. 2011;131:1195-1201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 37. | Cao S, Zeng JF, Xiao S, Dong ZG, Xu ZL, Liu H, Li X, Fang K, Wen J, Zeng M, Tang ZW, Li B, Gong HL, Li FL. Modified ulnar lengthening for correction of the Masada type 2 forearm deformity in hereditary multiple exostosis. Sci Rep. 2023;13:10554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 38. | Ahmed AARY. Gradual ulnar lengthening by an Ilizarov ring fixator for correction of Masada IIb forearm deformity without tumor excision in hereditary multiple exostosis: preliminary results. J Pediatr Orthop B. 2019;28:67-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 39. | Cho YJ, Jung ST. Gradual lengthening of the ulna in patients with multiple hereditary exostoses with a dislocated radial head. Yonsei Med J. 2014;55:178-184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 40. | Shawen SB, McHale KA, Temple HT. Correction of ankle valgus deformity secondary to multiple hereditary osteochondral exostoses with Ilizarov. Foot Ankle Int. 2000;21:1019-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 41. | Zhang R, Wang X, Liu S, Ruan H, Xu J, Kang Q. Hinge positioning method of Ilizarov apparatus in correcting radial head luxation caused by multiple hereditary exostoses. Jt Dis Relat Surg. 2022;33:40-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 42. | Li Y, Wang Z, Chen M, Cai H. Gradual ulnar lengthening in Masada type I/IIb deformity in patients with hereditary multiple osteochondromas: a retrospective study with a mean follow-up of 4.2 years. J Orthop Surg Res. 2020;15:594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 43. | Litzelmann E, Mazda K, Jehanno P, Brasher C, Penneçot GF, Ilharreborde B. Forearm deformities in hereditary multiple exostosis: clinical and functional results at maturity. J Pediatr Orthop. 2012;32:835-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 44. | Launay F, Jouve JL, Viehweger E, Guillaume JM, Jacquemier M, Bollini G. Progressive forearm lengthening with an intramedullary guidewire in children: report of 10 cases. J Pediatr Orthop. 2004;24:21-25. [PubMed] [DOI] [Full Text] |
| 45. | Song SH, Lee H, Youssef H, Oh SM, Park JH, Song HR. Modified Ilizarov technique for the treatment of forearm deformities in multiple cartilaginous exostoses: case series and literature review. J Hand Surg Eur Vol. 2013;38:288-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 46. | Ishikawa J, Kato H, Fujioka F, Iwasaki N, Suenaga N, Minami A. Tumor location affects the results of simple excision for multiple osteochondromas in the forearm. J Bone Joint Surg Am. 2007;89:1238-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 47. | Kelly JP, James MA. Radiographic Outcomes of Hemiepiphyseal Stapling for Distal Radius Deformity Due to Multiple Hereditary Exostoses. J Pediatr Orthop. 2016;36:42-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 48. | Ip D, Li YH, Chow W, Leong JC. Reconstruction of forearm deformities in multiple cartilaginous exostoses. J Pediatr Orthop B. 2003;12:17-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 49. | Nimityongskul P, Anderson LD, Sri P. Plastic deformation of the forearm: a review and case reports. J Trauma. 1991;31:1678-1685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 50. | Taleisnik J. The Sauvé-Kapandji Procedure. Clin Orthop Relat Res. 1992;275:110-123. [DOI] [Full Text] |
| 51. | Shin EK, Jones NF, Lawrence JF. Treatment of multiple hereditary osteochondromas of the forearm in children: a study of surgical procedures. J Bone Joint Surg Br. 2006;88:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 52. | Peterson HA. The ulnius: a one-bone forearm in children. J Pediatr Orthop B. 2008;17:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 53. | Agashe MV, Shah M, Choudhry A, Shah A, Agarwal S, Vaidya S. One-Bone Forearm Procedure for Severe Recalcitrant Forearm Deformities in Masada IIb Hereditary Multiple Exostoses. Indian J Orthop. 2023;57:1777-1784. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 54. | Wang KK, Vuillermin CB, Waters PM. Single-Bone Forearm as a Salvage Procedure in Recalcitrant Pediatric Forearm Pathologies. J Hand Surg Am. 2020;45:947-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 55. | Benameur H, Bensaleh S, Alidrissi N, Jaafar A, Chahbouni M. Modified Technique of Single-Bone Forearm in the Treatment of Deformities. Cureus. 2022;14:e26361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 56. | Paley D. Problems, Obstacles, and Complications of Limb Lengthening by the Ilizarov Technique. Clin Orthop Relat Res. 1990;250:81-104. [RCA] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 279] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 57. | Huser AJ, Nugraha HK, Hariharan AR, Ziegler SE, Feldman DS. Peroneal Nerve Decompression in Patients with Multiple Hereditary Exostoses: Indications, Complications, and Recurrence. J Bone Joint Surg Am. 2024;106:1277-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 58. | Humbert ET, Mehlman C, Crawford AH. Two cases of osteochondroma recurrence after surgical resection. Am J Orthop (Belle Mead NJ). 2001;30:62-64. [PubMed] |
| 59. | Catagni MA, Szabo RM, Cattaneo R. Preliminary experience with Ilizarov method in late reconstruction of radial hemimelia. J Hand Surg Am. 1993;18:316-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 60. | Yasui N, Kojimoto H, Sasaki K, Kitada A, Shimizu H, Shimomura Y. Factors Affecting Callus Distraction in Limb Lengthening. Clin Orthop Relat Res. 1993;293:55-60. [DOI] [Full Text] |
| 61. | De Vitis R, Passiatore M, Cilli V, Maffeis J, Milano G, Taccardo G. Intramedullary nailing for treatment of forearm non-union: Is it useful? - A case series. J Orthop. 2020;20:97-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 62. | Peterson HA. Deformities and problems of the forearm in children with multiple hereditary osteochondromata. J Pediatr Orthop. 1994;14:92-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 63. | Scheider P, Ganger R, Farr S. Age-related Outcomes and Complications of Osteodistraction in the Pediatric Upper Extremity: A Large Retrospective Single-center Study of 61 Cases. J Pediatr Orthop. 2022;42:e181-e187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 64. | Mercier J, Bernasconi R, Steiger C, Kaempfen A, Krieg AH. Conservative and Surgical Treatment of Osteochondromas in Children, Particularly with or without Surgical Lengthening of the Ulna. J Clin Med. 2023;12:4273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 65. | Jo AR, Jung ST, Kim MS, Oh CS, Min BJ. An Evaluation of Forearm Deformities in Hereditary Multiple Exostoses: Factors Associated With Radial Head Dislocation and Comprehensive Classification. J Hand Surg Am. 2017;42:292.e1-292.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 66. | Arms DM, Strecker WB, Manske PR, Schoenecker PL. Management of forearm deformity in multiple hereditary osteochondromatosis. J Pediatr Orthop. 1997;17:450-454. [PubMed] [DOI] [Full Text] |
| 67. | Beutel BG, Klifto CS, Chu A. Timing of forearm deformity correction in a child with multiple hereditary exostosis. Am J Orthop (Belle Mead NJ). 2014;43:422-425. [PubMed] |
| 68. | Gottschalk HP, Kanauchi Y, Bednar MS, Light TR. Effect of osteochondroma location on forearm deformity in patients with multiple hereditary osteochondromatosis. J Hand Surg Am. 2012;37:2286-2293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 69. | Feldman DS, Rand TJ, Deszczynski J, Albrewczynski T, Paley D, Huser AJ. Prediction of Radial Head Subluxation and Dislocation in Patients with Multiple Hereditary Exostoses. J Bone Joint Surg Am. 2021;103:2207-2214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |