Published online Jul 18, 2025. doi: 10.5312/wjo.v16.i7.107913
Revised: April 30, 2025
Accepted: June 17, 2025
Published online: July 18, 2025
Processing time: 103 Days and 11.7 Hours
The volar approach with plate fixation is the gold standard for treating distal radius fractures, often requiring incision of the pronator quadratus (PQ) muscle. Preserving the PQ during surgery may facilitate early postoperative recovery. However, conventional minimally invasive plate osteosynthesis (MIPO) tech
To retrospectively analyze distal radius fractures treated using the 3-point positioning-assisted MIPO technique with preservation of the PQ.
The 3-point positioning technique was applied: The Kirschner wire was inserted after fluoroscopy and was correctly adjusted the position of the plate above the PQ. With the aid of Kirschner wires positioning the PQ stripping was performed only once, and the plate then placed in a correct and satisfactory position. Ope
At a mean follow-up of 6.9 ± 0.8 months, the mean scar length was 25.4 ± 1.5 mm, the pain score was 0.7 ± 0.6, the DASH score for the upper limb was 4.7 ± 1.3, and the Gartland-Werley score for wrist function was 4.1 ± 1.1 at the last follow-up. Mean flexion was 97.3%, extension was 97.0%, pronation was 98.9%, supination was 98.9%, and grip strength was 86.6% compared to contralateral values. No unfavorable intraoperative or postoperative complications occurred.
The 3-point positioning technique may reduce the damage to the PQ muscle and is a safe and effective method for MIPO for distal radius fractures.
Core Tip: This study introduces an innovative 3-point positioning technique for distal radius fracture fixation using minimally invasive plate osteosynthesis (MIPO). Under fluoroscopic guidance, Kirschner wires were strategically placed to achieve precise plate positioning above the pronator quadratus (PQ) muscle. This technique reduces PQ dissection to a single surgical maneuver, avoiding the repetitive plate adjustments required in conventional MIPO that may compromise PQ integrity. By optimizing plate placement efficiency, our method demonstrated improved PQ preservation and superior early clinical outcomes compared to traditional approaches.
- Citation: Ye YY, Shen ZQ, Wu CL, Lin YB. Minimally invasive plate osteosynthesis for distal radius fractures using a 3-point positioning technique. World J Orthop 2025; 16(7): 107913
- URL: https://www.wjgnet.com/2218-5836/full/v16/i7/107913.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i7.107913
Distal radius fractures represent the most common orthopedic fractures. While conservative management with casting or bracing remains an option, surgical interventions including open reduction and internal fixation, external fixation, and percutaneous Kirschner wire fixation are frequently employed[1]. The volar Henry approach with plate fixation has emerged as the predominant surgical technique, typically requiring incision of the pronator quadratus (PQ) muscle.
The debate regarding PQ repair during volar plating persists in the literature. However, PQ injury has been associated with several clinically significant consequences: Tendon irritation, compromised vascular supply to the distal radius, destabilization of the distal radioulnar joint, and reduction of forearm pronation strength by up to 21%[2]. These concerns have prompted investigation into PQ-preserving techniques, with several studies demonstrating favorable outcomes[3,4].
Our clinical observations reveal that conventional minimally invasive plate osteosynthesis (MIPO) typically requires 3-4 fluoroscopically-guided plate adjustments to achieve proper positioning. The PQ's anatomical characteristics as a closed compartment without intermuscular septa[5] make it particularly vulnerable during these manipulations. The repeated plate adjustments between radial and ulnar positions inevitably disrupt the PQ's start and end points. Thus, while described as "PQ-preserving", conventional techniques often result in substantial muscular damage.
To address these limitations, we developed a novel 3-point positioning technique designed to optimize PQ preservation. This retrospective study evaluates the clinical outcomes and complications in 30 consecutive patients treated with this innovative approach.
The Human Experimentation and Ethics Committee of our hospital's institutional review board gave its approval to the study's design and data collection (2023101). We reviewed the records of 70 patients who underwent MIPO for distal radius fracture between January 2019 and October 2022. Due to inadequate data, a follow-up of less than six months, concurrent bilateral fractures, or bone and ligament abnormalities in the wrist, 40 cases were excluded. Adults with recent fractures (two weeks), no accompanying lesions, and more than six months of follow-up were included in the study. The series thus consisted of 30 patients, 11 males and 19 females, who were all classified by AO/ASIF. The patients included type A2 (n = 6), type A3 (n = 4), type B1 (n = 7), type B3 (n = 6), type C1 (n = 6), and type C2 (n = 1) individuals. This study did not include patients who had distal radius fractures of types A1, B2, or C3.
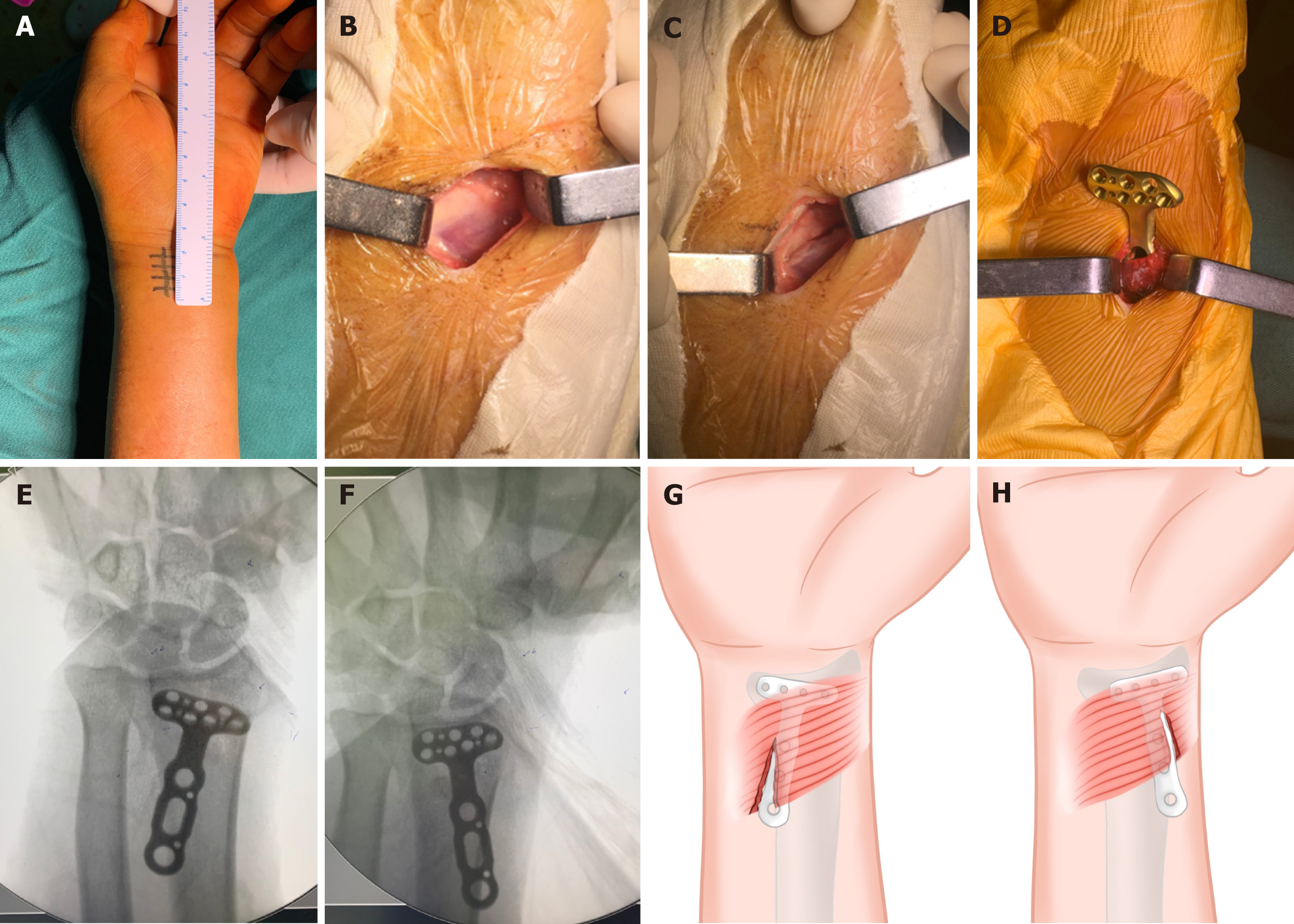
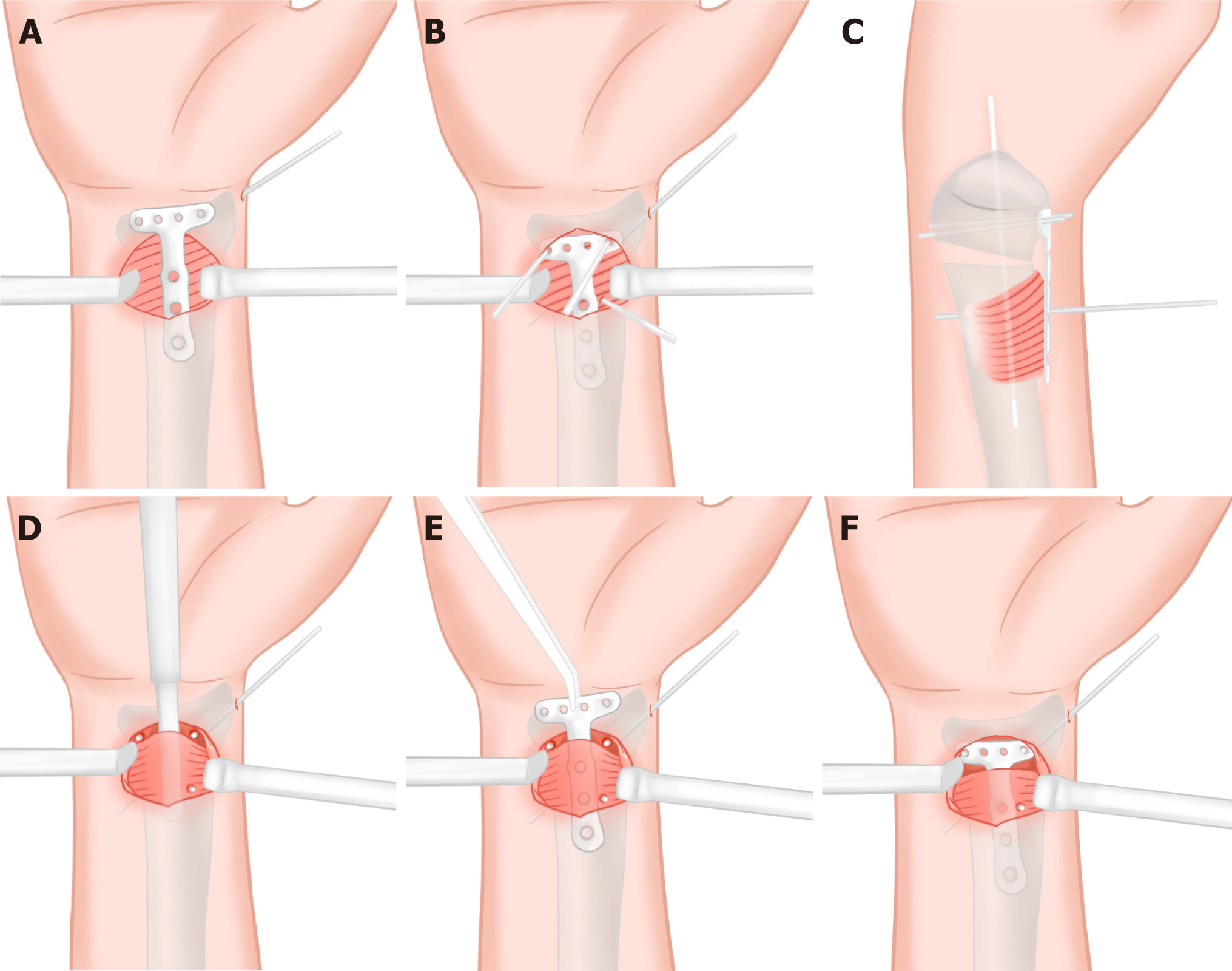
All patients were anesthetized with a brachial plexus block and placed on a radiolucent table. Following the onset of anesthesia, closed manual reduction was performed on all patients. A 15 mm diameter Kirschner wire was inserted from the styloid process of the radius to the ulnar side of the proximal fracture to retain the initial anatomical parameters after preliminary acceptable fracture reduction was confirmed by fluoroscopy (Figure 1). The surgical incision was created with the flexor carpi radialis radial margin being extended under the transverse carpal line to the proximal end 2.5 cm (Figure 2A). After exposing the flexor carpi radialis tendon, it was pulled ulnarally along with the median nerve, the radial artery was pulled radially, and the PQ was exposed (Figure 2B). In distal radius fractures, the distal margin of the PQ is often split by the fracture end. If not, it was cut it transverse and then lifted the distal edge of the PQ from the subperiosteum of the radius and performed fracture reduction (Figure 2C). In the traditional MIPO method, the plate is inserted below the PQ in the next step (Figure 2D). In our clinical practice we have found that it takes an average of 3-4 adjustments to place the plate in the correct position under the PQ, which inevitably leads to the injury of the PQ (Figure 2E-H). We position the volar anatomic locking plate at the distal radius above the PQ in our modified 3-point positioning technology, with the distal end placed at the watershed line of the distal radius (Figure 3A). Two 15mm Kirschner wires were inserted into the radial and ulnar screw holes at the plate’s distal end and passed through the dorsal cortex to temporarily anchor the plate after fluoroscopy confirmed its satisfactory position. To determine the position of the plate on the radial axis, a 15 mm Kirschner wire was positioned close to the ulnar border of the central portion of the plate (Figure 3B and C). The plate was removed after the three Kirschner wires had been trimmed to a length of approximately 0.5 cm and left in place. Between the two Kirschner wires at the distal end and close to the radial border of the Kirschner wire at the proximal end, a subperiosteal dissection of the PQ was performed (Figure 3D). The locking hole of the plate's distal radial and ulnar sides were "guided onto" into the two shorted Kirschner wire posts at the distal end after the plate was inserted into the tunnel from the radial edge of the proximal Kirschner wire (Figure 3E and F). The screw was placed for fixation after fluoroscopy to ensure that the position of the plate was suitable. The 3-point positioning technique was utilized to prevent harm to the PQ muscle from cutting during multiple adjustments and to ensure that the plate could be put in the proper position following a single dissection of the muscle (Figure 3). The remaining screws were inserted to complete the final fixation, and the surgical incision was irrigated and closed layer by layer. No external immobilization was used. Six to eight hours after surgery, early active hand clenching and relaxation exercises were performed. Active and passive wrist flexion and extension and forearm rotation training were started 24 h after surgery. The corresponding training intensity was guided according to the type of fracture and wound healing of patients.
The operation time, incision length, postoperative radial inclination (RI), volar tilt (VT), and ulnar variance (UV) were recorded at the initial follow-up, at 1-, 3-, and 7 days following surgery, at three weeks after surgery, and the last follow-up visit. Wrist pain was assessed using the visual analog scale. At three weeks following surgery and the final follow-up, the upper extremity function score [disabilities of the arm, shoulder and hand (DASH), and hand outcome measure][6] and the Gartland-Werley score[7] of wrist function were evaluated. On the operative and contralateral sides, the range of motion (ROM) (flexion, extension, pronation, and supination) and grip strength measured in kilogram-force with a Jamar® hydraulic dynamometer (per-performance Health, Reims, France) were assessed and compared at the last follow-up visit. Both intraoperative and follow-up complications were recorded.
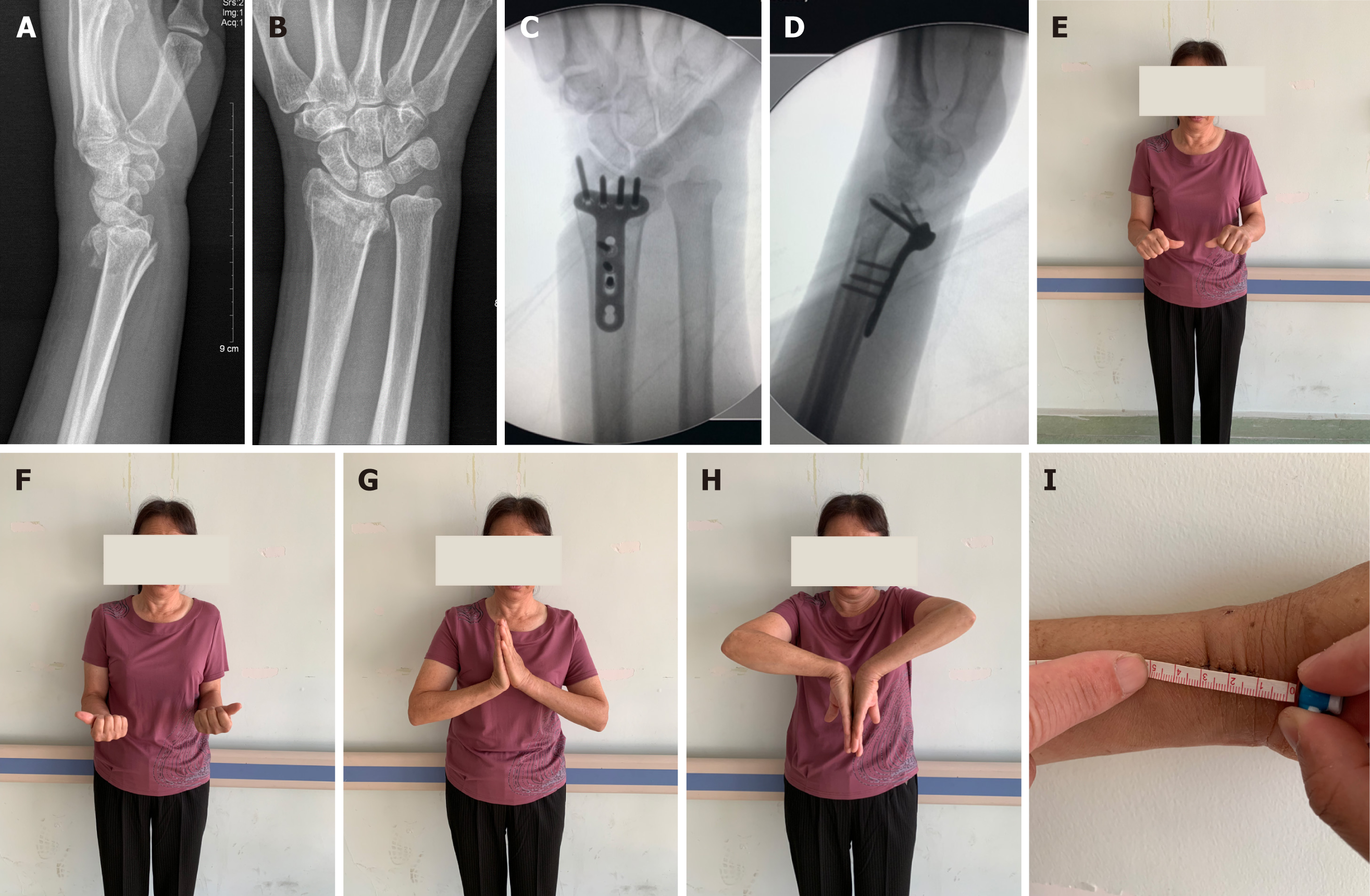
Twenty patients with a mean age of 44.5 ± 12.9 years (range, 22-71 years) were followed up for a mean of 6.9 ± 0.8 months (range, 6-9 months). The average length of an incision was 25.4 ± 1.5 mm (range, 23-28 mm). The mean operative time was 42.1 ± 3.8 minutes (range, 33-50 minutes). The mean RI, VT, and UV were not significantly different from the contralateral side (Table 1). In comparison to the mean pain score three weeks after surgery, the mean pain score at the last follow-up, 0.7± 0.6 (range, 0-2) was significantly different. The DASH score at three weeks following surgery (11.6 ± 2.0) differed considerably from that at the last follow-up (4.7 ± 1.3). The difference between the Gartland-Werley score at the last follow-up (4.1 ± 1.1) and the score at three weeks following surgery (12.0 ± 2.5) was also statistically significant (Table 2). A comparison of ROM and grip strength is shown in Table 3 for both the operational and contralateral sides. Pronation was 98.9%, supination was 98.9%, flexion was 97.3%, extension was 97.0%, and grip strength was 86.6% when compared to the contralateral side (Table 3). These measurements showed a statistically significant reduction in function compared to the contralateral side (P < 0.01). One case (3.3%) developed delayed wound healing within the first postoperative week. Comprehensive evaluation including bacterial culture and inflammatory marker analysis excluded infectious etiology. The wound achieved complete healing following surgical debridement and appropriate local wound care. No complications such as infection, iatrogenic vascular or nerve injury, malunion, or failure of fixation were observed in any of the patients (Figure 4).
The advancement of medical technology and increasing demand for improved cosmetic outcomes have driven the widespread adoption of minimally invasive approaches across surgical specialties. In orthopedic trauma, Imatani et al[8] and Neubauer et al[9] first introduced the concept of minimally invasive management for distal radius fractures. Subsequent technical refinements have enabled some investigators to perform the procedure through incisions as small as 1 cm[10]. However, a minimally invasive strategy for treating distal radius fractures entails more than merely making tiny incisions. The key to minimally invasive treatment of the distal radius fracture is minimum interference with several important surrounding tissues, no damage to the PQ, no dissection of the radial artery or median nerve, and no dissection of the joint capsule or ligament appendages. In particular, the PQ can increase the distal radioulnar joint's stability, supply blood to the distal radius to aid in fracture healing, and provide 21% of the forearm's pronation strength, and an undamaged PQ will also increase the postoperative pronation angle and reduce tendon injury and irritation[2,11].
Sotereanos et al[5] confirmed that the PQ muscle is a closed compartment without a muscle septum by injecting image enhancement agents into cadaveric specimens under fluoroscopy, and its muscle bundle starts from the front and medial side of the lower 1/5 of the ulna and ends on the palmar and anterior edge of the lower 1/5 of the radius. However, conventional minimally invasive treatment of distal radius fractures requires blind penetration of the plate under the PQ muscle at the proximal radius. The plate may be placed on the radial or ulnar side during the procedure, and the position needs to be confirmed and adjusted under fluoroscopy. Our surgical experience demonstrates that conventional minimally invasive plate placement beneath the PQ muscle typically requires 3-4 intraoperative adjustments to achieve optimal positioning. These repeated manipulations invariably result in iatrogenic damage to both the starting and ending points of the PQ at the volar aspect of the lower 1/3 of the radius. This finding challenges the concept of true PQ preservation in standard minimally invasive techniques, as the procedure inherently causes significant muscular disruption. Furthermore, the limited visualization inherent to minimally invasive approaches prevents both intraoperative assessment of PQ injury and subsequent repair under direct vision. Paradoxically, this may result in greater cumulative soft tissue trauma compared to open approaches where direct visualization enables precise anatomical repair. In this study, the "3-point positioning method" is proposed, in which the plate was placed above the PQ muscle in advance, and the exact position of the plate was adjusted by fluoroscopy above it. Three Kirschner wires were used to position the plate, and a unique and relatively accurate dissection and placement of the plate under the periosteum of the PQ muscle was performed between the Kirschner wires at the pile-point to minimize damage to the PQ muscle.
The 3-point positioning method was used to treat patients in this clinical investigation, and it was found to have advantages for early postoperative wrist pain relief, wrist joint activity, and functional recovery. The wrist function of the patients was assessed using the Gartland-Werley scale in this study, with pain serving as the primary predictor. In the palmar approach for distal radius fractures, Itoh et al[12] compared two alternative ways to dispose of the PQ: One method preserved the muscle, while the other incised the muscle and then repaired it with sutures. The outcome demonstrated that the wrist pain scores of the PQ preservation approach were lower at two, three, and four months after surgery. Häberle et al[13] also demonstrated that MIPO used to treat distal radius fractures while protecting the PQ was effective in minimizing postoperative pain within six weeks of surgery. Early postoperative wrist pain scores were lower with our study's 3-point positioning method patients than they were in other published studies[14,15]. Among the reasons may be that the technique causes less damage to the PQ muscle, less swelling of the muscle's soft tissue in the early postoperative period, and less tearing pain in the injured muscle caused by early exercise. The anatomical position and physiological function of the PQ are not impaired, which better isolates the contact of the internal fixation with the tendon and thus avoids irritating it. As a result, patients had lower levels of early pain and were able to achieve better Gartland-Werley scores.
In the early post-operative period, Armangil et al[16] revealed an average loss in forearm pronation strength of about 18.5%, with the forearm pronation durability test indicating a loss of up to 12.9%. Lidocaine was used by McConkey et al[2] to test the contribution of the pronator quadrate to pronation by paralyzing the pronate quadrate. They found that paralysis reduced the pronation of the forearm by 16.7% to 23.2%. If the PQ suture was not completed it was observed that the forearm pronation strength was decreased by 22% at a 1-year follow-up after surgery[17]. Of course, some reports have proposed that the repair of the PQ muscle has no effect on the follow-up results of joint rotation and ROM and believe that the weakening or loss of the PQ muscle function can be compensated for by the pronator teres muscle and the flexor carpi radialis muscle so that the forearm rotation function can be preserved[18,19]. However, we believe that the anatomy of each physiological presence has its distinct meaning. The PQ, if repaired or only slightly damaged, can alleviate pain in the early postoperative period, allowing patients to achieve better postoperative rom and grip strength, and reducing flexor tendon irritation. Fan et al[20] also suggested that in the early stage of recovery, the preserved or repaired PQ muscle has better pronation ability and lower pain scores. The follow-up time of our study was relatively short, only 6.9 ± 0.8 months (range, 6-9 months). We obtained satisfactory ROM and Grip Strength results in a relatively short period when compared with the contralateral side. To achieve similar results, according to previous literature, follow-up is often required for 14.2-22.7 months[21,22]. We think this is related to our protection of the PQ. Of course, if there had been a longer follow-up period, perhaps more positive results would have been presented. In addition, the limitation of this study is the absence of objective quantitative measures to assess PQ muscle integrity, including postoperative imaging modalities (magnetic resonance imaging or ultrasonography) or standardized intraoperative grading systems for muscle preservation.
In terms of surgical indications Naito et al[10] considered that for type C2 and C3 fractures with a comminuted articular surface, the patient should be carefully selected, and wrist arthroscopy should be assisted if necessary. However, for a type C1 distal radius fracture, they believed that a small minimally invasive incision of 1.0 cm could also achieve satisfactory efficacy. The A1 fracture (radial styloid avulsion) was excluded from our study as it can typically be managed conservatively or with minimally invasive percutaneous screw fixation. Type B2 fractures (Barton's fractures) were also excluded due to the technical difficulty of achieving adequate exposure and stable fixation through a minimally invasive approach. Similarly, Type C3 fractures (comminuted intra-articular fractures) were excluded because optimal mana
The 3-point positioning technique has the advantage of requiring only a single dissection of the PQ, thereby preventing injury to the muscle caused by repeatedly adjusting the position of the plate underneath the muscle during the traditional MIPO technique. The plate is tagged with Kirschner wires and prepositioned over the PQ muscle, which is the fundamental originality of this technique. The main innovation of this method is that the plate is placed above the PQ muscle, and the Kirschner wires are inserted as the pile-point after the correct position is confirmed. Finally, the plate was "guided onto" the pile-point. If the fracture is relatively comminuted, 2 to 3 Kirschner wires (1.0 mm and 1.5 mm) can be percutaneously placed from the radial edge of the radius to the ulnar side to maintain the reduction and ensure that the plate placement is not interfered with. When encountering difficulty inserting the most proximal screw, a limited proximal percutaneous incision should be created while maintaining gentle tissue handling. The assistant should optimize exposure by flexing the wrist joint to reduce incision tension and create adequate working space. Prior to final fixation, careful inspection must confirm the absence of tendon, neurovascular, or soft tissue impingement by the plate. Post-fixation assessment should include dynamic testing through the maximal wrist and metacarpophalangeal joint ROM to verify unrestricted tendon gliding. This technique requires particular attention to the learning curve, as optimal outcomes depend on both surgical proficiency and coordinated team execution to achieve consistent results.
The "3-point positioning technique" was used to treat distal radius fractures in this study, which minimizes the damage to the PQ muscle and achieves satisfactory mid-term clinical results. Although it was a retrospective study not involving a large number of cases, this technical innovation is worthy of further refinement, research, and eventual promotion.
I would like to thank Zhang Yan, Zheng Wei for their extraordinary support in this research project.
| 1. | Azad A, Kang HP, Alluri RK, Vakhshori V, Kay HF, Ghiassi A. Epidemiological and Treatment Trends of Distal Radius Fractures across Multiple Age Groups. J Wrist Surg. 2019;8:305-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 84] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 2. | McConkey MO, Schwab TD, Travlos A, Oxland TR, Goetz T. Quantification of pronator quadratus contribution to isometric pronation torque of the forearm. J Hand Surg Am. 2009;34:1612-1617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Neubauer T, Plecko M, Grechenig S, Hartmann A, Ortmaier R, Hitzl W, Feigl G. Minimal invasive plating of distal radius fractures. A safe procedure? Ann Anat. 2019;224:172-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Liechti R, Babst R, Hug U, Link BC, van de Wall BJM, Knobe M, Beeres FJP. The spanning plate as an internal fixator in complex distal radius fractures: a prospective cohort study. Eur J Trauma Emerg Surg. 2022;48:2369-2377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Sotereanos DG, McCarthy DM, Towers JD, Britton CA, Herndon JH. The pronator quadratus: a distinct forearm space? J Hand Surg Am. 1995;20:496-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 43] [Reference Citation Analysis (0)] |
| 7. | GARTLAND JJ Jr, WERLEY CW. Evaluation of healed Colles' fractures. J Bone Joint Surg Am. 1951;33-A:895-907. [PubMed] [DOI] [Full Text] |
| 8. | Imatani J, Noda T, Morito Y, Sato T, Hashizume H, Inoue H. Minimally invasive plate osteosynthesis for comminuted fractures of the metaphysis of the radius. J Hand Surg Br. 2005;30:220-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 9. | Neubauer T, Wagner M. [Minimally invasive plate osteosynthesis: current state. Part 1: General information]. Unfallchirurg. 2009;112:885-94; quiz 895. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Naito K, Zemirline A, Sugiyama Y, Obata H, Liverneaux P, Kaneko K. Possibility of Fixation of a Distal Radius Fracture With a Volar Locking Plate Through a 10 mm Approach. Tech Hand Up Extrem Surg. 2016;20:71-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Walch A, Erhard L, Vogels J, Pozzetto M, Gibert N, Locquet V. Ultrasound Evaluation of the Protector Role of the Pronator Quadratus Suture in Volar Plating. J Ultrasound Med. 2019;38:2785-2791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Itoh S, Yumoto M, Kanai M, Yoshida W, Yoshioka T. Significance of a Pronator Quadratus-Sparing Approach for Volar Locking Plate Fixation of Comminuted Intra-articular Fractures of the Distal Radius. Hand (N Y). 2016;11:83-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Häberle S, Sandmann GH, Deiler S, Kraus TM, Fensky F, Torsiglieri T, Rondak IC, Biberthaler P, Stöckle U, Siebenlist S. Pronator quadratus repair after volar plating of distal radius fractures or not? Results of a prospective randomized trial. Eur J Med Res. 2015;20:93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Fan J, Zhang X, Ji JQ, Yao Y, Li SZ, Yuan F, Cheng LM. Fixation of distal radius fracture with volar locking palmar plates while preserving pronator quadratus through the minimally invasive approach. Technol Health Care. 2021;29:167-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Goorens CK, Debaenst N, Van Royen K, Provyn S, Goubau JF. Minimally Invasive Pronator Quadratus Sparing Approach versus Extended Flexor Carpi Radialis Approach with Pronator Quadratus Repair for Volar Plating in Distal Radial Fractures. J Wrist Surg. 2022;11:41-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Armangil M, Bezirgan U, Başarır K, Bilen G, Demirtaş M, Bilgin SS. The pronator quadratus muscle after plating of distal radius fractures: is the muscle still working? Eur J Orthop Surg Traumatol. 2014;24:335-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Falk SSI, Maksimow A, Mittlmeier T, Gradl G. Does access through the pronator quadratus influence pronation strength in palmar plate fixation of distal radius fractures in elderly patients? Arch Orthop Trauma Surg. 2023;143:5445-5454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 18. | Fang K, Lin X, Liu X, Ke Q, Shi S, Dai Z. Do we need to suture the pronator quadratus muscle when we do open reduction and internal fixation for fracture of the distal radius. BMC Musculoskelet Disord. 2020;21:453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Lo HY, Cheng HY. Clinical study of the pronator quadratus muscle: anatomical features and feasibility of pronator-sparing surgery. BMC Musculoskelet Disord. 2014;15:136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Fan J, Chen K, Zhu H, Jiang B, Yuan F, Zhu X, Mei J, Yu G. Effect of fixing distal radius fracture with volar locking palmar plates while preserving pronator quadratus. Chin Med J (Engl). 2014;127:2929-2933. [PubMed] [DOI] [Full Text] |
| 21. | Asmar G, Bellity J, Falcone MO. Surgical comfort and clinical outcomes of MIPO with an extra-short plate designed for distal radius fractures. Eur J Orthop Surg Traumatol. 2021;31:481-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Zenke Y, Sakai A, Oshige T, Moritani S, Fuse Y, Maehara T, Nakamura T. Clinical results of volar locking plate for distal radius fractures: conventional versus minimally invasive plate osteosynthesis. J Orthop Trauma. 2011;25:425-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |