Published online Jul 18, 2025. doi: 10.5312/wjo.v16.i7.107869
Revised: April 29, 2025
Accepted: June 20, 2025
Published online: July 18, 2025
Processing time: 109 Days and 10.1 Hours
Sagittal spinopelvic alignment (SSA) is essential for preserving a stable and effective upright posture and locomotion. Although alterations in the SSA are recognised to induce compensatory modifications in the pelvis, hips, and knees, the inverse relationship concerning knee pathology undergoing total knee arthroplasty (TKA) has been examined by a limited number of studies, yielding inconclusive results.
To generate evidence of the effect of TKA on the SSA from existing literature.
Databases like PubMed, EMBASE, and Scopus were used to identify articles related to the “knee spine syndrome” phenomenon using a combination of subject terms and keywords such as “spinopelvic parameters”, “sagittal spinal balance”, and “total knee arthroplasty” were used with appropriate Boolean operators. Studies measuring the SSA following TKA were included, and research was conducted as per preferred reporting items for systematic review and meta-analysis guidelines.
A total of 475 participants had undergone TKA, and six studies measuring SSA were analysed. Following TKA, pelvic tilt was the only parameter that showed significant changes, while lumbar lordosis (LL), pelvic incidence, and sacral slope were non-significant, as evident from the forest plots.
The body's sagittal alignment is a complex balance between pelvic, spine, and lower extremity parameters. TKA, while having the potential to correct the flexion contracture, can also correct it. Still, the primary SSA for spinal pathology, i.e., LL, may not be corrected in patients with co-existent spinal degenerative disease.
Core Tip: Sagittal spinopelvic alignment (SSA) plays a critical role in maintaining upright posture and mobility. While spinal alignment changes are known to cause compensatory shifts in the pelvis, hips, and knees, few studies have explored the reverse relationship, particularly in patients undergoing total knee arthroplasty (TKA), with inconclusive findings. SSA represents a complex interaction among pelvic, spinal, and lower limb structures. Although TKA can improve knee flexion contractures, it may not fully address lumbar lordosis, especially in individuals with concurrent spinal degenerative conditions, limiting overall sagittal correction.
- Citation: Jain M, Pal DK, Narayan Sahu R, Meher BR, Patro BK, Tripathy SK. Effect of total knee arthroplasty on the spinopelvic parameters: A systemic review and metanalysis. World J Orthop 2025; 16(7): 107869
- URL: https://www.wjgnet.com/2218-5836/full/v16/i7/107869.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i7.107869
Osteoarthritis (OA) is a disease in which cartilage and underlying bone degenerate within a joint. In the late stages of knee OA, patients develop fixed flexion deformity as well as varus or valgus coronal deformity. Total knee arthroplasty (TKA) is a safe and efficacious treatment modality for these patients[1]. It mitigates pain, rectifies deformities, reinstates function, and improves the patient's quality of life[2]. Sagittal spinopelvic alignment (SSA) is essential for the body's stability and efficiency in posture and ambulation[3-5]. Any imbalance in the SSA can induce compensatory adjustments in the pelvis, hips, and knees to sustain a level of static horizontal gaze with minimal energy expenditure. Hambrecht et al[6] found that altered SSA was the principal cause for low back pain. Fontalis et al[7] defined the "knee spine syndrome" as lumbar spine symptoms resulting from degenerative alterations in the knee. Few researchers attempted to determine the changes in the SSA following TKA. However, the evidence is insufficient to draw strong conclusions because few studies document changes in SSA[8,9], while others do not[10-13]. With this background, we intend to conduct a meta-analysis to generate results from the available studies and potentially solve this enigma.
The protocol was registered on the International Prospective Register of Systematic Review (CRD42024556689), and the institute's ethical committee granted us a waiver (T/IM-NF/Ortho/24/51). The meta-analysis was conducted and reported by preferred reporting items for systematic review and meta-analysis[14].
We searched PubMed, EMBASE, and Scopus to identify articles related to “knee spine syndrome” phenomenon. A combination of subject terms and keywords such as “spinopelvic parameters”, “sagittal spinal balance”, and “total knee arthroplasty” were used with appropriate Boolean operators. The search strategy used both Medical Subject Headings and keyword variants of all relevant terms. We also adjusted for vocabulary and grammar between different databases using the Population, Intervention, Comparison, Outcome method. The reference lists of published reviews and retrieved articles were manually checked for additional studies. The detailed search strategy for individual databases is provided in supplementary data (Supplementary Table 1).
Studies measuring the SSA following the TKA and published in the English language till 15th April 2025 were included. Articles including SSA parameters, namely the pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), lumbar lordosis (LL), and sagittal vertical axis (SVA) pre and post-total knee replacement (TKR) of one or both knees were included in our study. We only included pre-TKA and post-TKA studies in the meta-analysis with mean and standard deviation available for SSA parameters. Studies measuring the SSA following uni-compartmental replacement, those having prior spinal fusion, or patients with TKA whose data was missing were excluded from our study. Conference abstracts were tried to extract data and failed to, leading to the exclusion of the study.
Two reviewers independently screened the articles with title and abstract, followed by full-text screening using the eligibility criteria. In case of any conflict, adjudication was done by one senior researcher. The full text was tried for retrieval along with retrieval of appropriate parameters by contacting the corresponding author. Microsoft Excel entered the data related to the first author, publication year, study design, and follow-up time. The SSA, which included the PI, PT, SS, LL, and SVA pre-TKA and post-TKA, were recorded in an Excel sheet.
This meta-analysis was performed utilising STATA software[15]. This meta-analysis focused on changes in sacropelvic parameters, specifically PI, PT, SS, and LL, all of which are continuous variables. The mean difference with a 95%CI was computed for continuous variables to evaluate the effect size and examine the differences in outcome measures before and after TKR. The random-effects model was employed for comprehensive between-group analyses when heterogeneity among individual studies exceeded 50%. We performed meta-regression to determine the impact of the follow-up duration on the variation in SSA.
We used the Risk of Bias in Non-randomised Studies-of Interventions to assess the risk of bias in individual studies for the primary outcome[16]. Two reviewers independently evaluated and documented their evaluations and rationales in each domain for each included study. The differences between them were resolved in consultation with the third reviewer.
The number of included studies was found to be less than ten. This fact will lead to misinterpretation of publication bias using statistical methods due to less power[17].
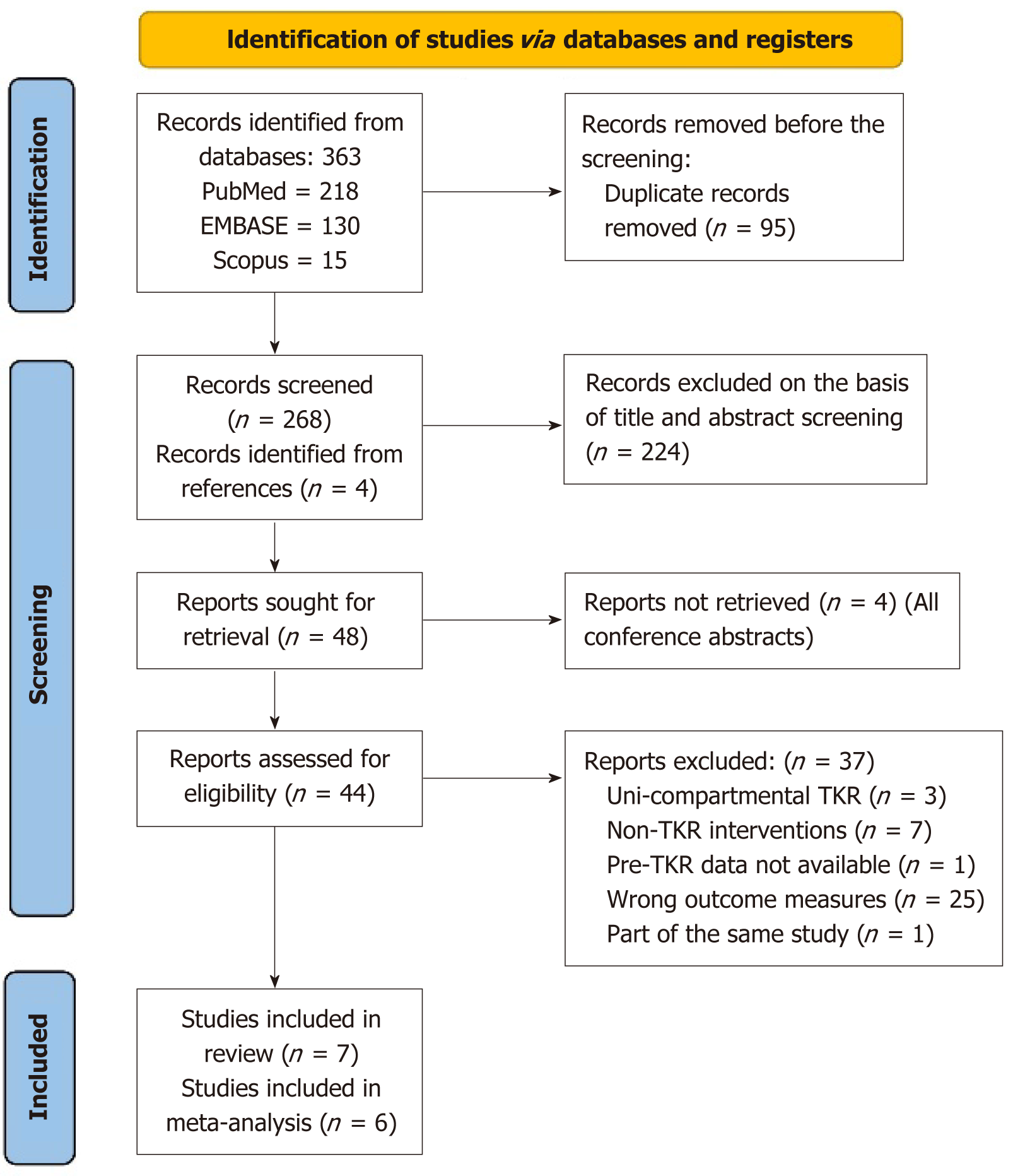
We identified a total of 363 records from three databases, and 48 records were finally sought for full text. We finally identified seven studies eligible, with one of them not having mean ± SD available for spinal parameters[8-13,18]. The details of the screening of articles and details of the exclusion of articles during full-text screening are provided herewith (Figure 1). All of the included studies had a moderate risk of bias ( Supplementary Table 2)[8-13].
The studies included a total of 475 participants who had undergone TKR, with studies conducted in South Korea, Japan, Turkey, the United States, and India. The postoperative follow-up period ranged from two weeks to 63 months. All of the studies were published from 2020 to 2022. All of the studies reported three spinal parameters (LL, PT, and SS), whereas only four studies reported pre-TKR and post-TKR PI values (Table 1)[8-13].
| Ref. | Year of publication | Sample size | Outcomes measured | Country | Any comorbidity | Post-op follow-up period | Level of evidence | Risk of bias |
| Kim et al[13] | 2020 | 101 | LL, PT, SS | South Korea | Knee FC in all patients | 3 months, 12 months | Pre and post study design | Moderate |
| Kitagawa et al[10] | 2021 | 110 | LL, PT, SS, PI | Japan | Maximum had knee FC | 1 month | Pre and post study design | Moderate |
| Batibay et al[8] | 2020 | 83 | LL, PT, SS, PI | Turkey | - | 12-63 months, mean 37 months | Pre and post study design | Moderate |
| Han et al[12] | 2021 | 36 | LL, PT, SS, PI | South Korea | Knee FC in all patients | 2 weeks, 6 weeks, 6 months, 1 year, 2 years | Pre and post study design | Moderate |
| Shichman et al[9] | 2023 | 113 | LL, PT, SS | United States | Knee FC in 20 patients | 3 months | Pre and post study design | Moderate |
| Puthiyapura et al[11] | 2022 | 32 | LL, PT, SS, PI | India | Knee FC (> 100) correction in 15/32 patients | 3 months | Pre and post study design | Moderate |
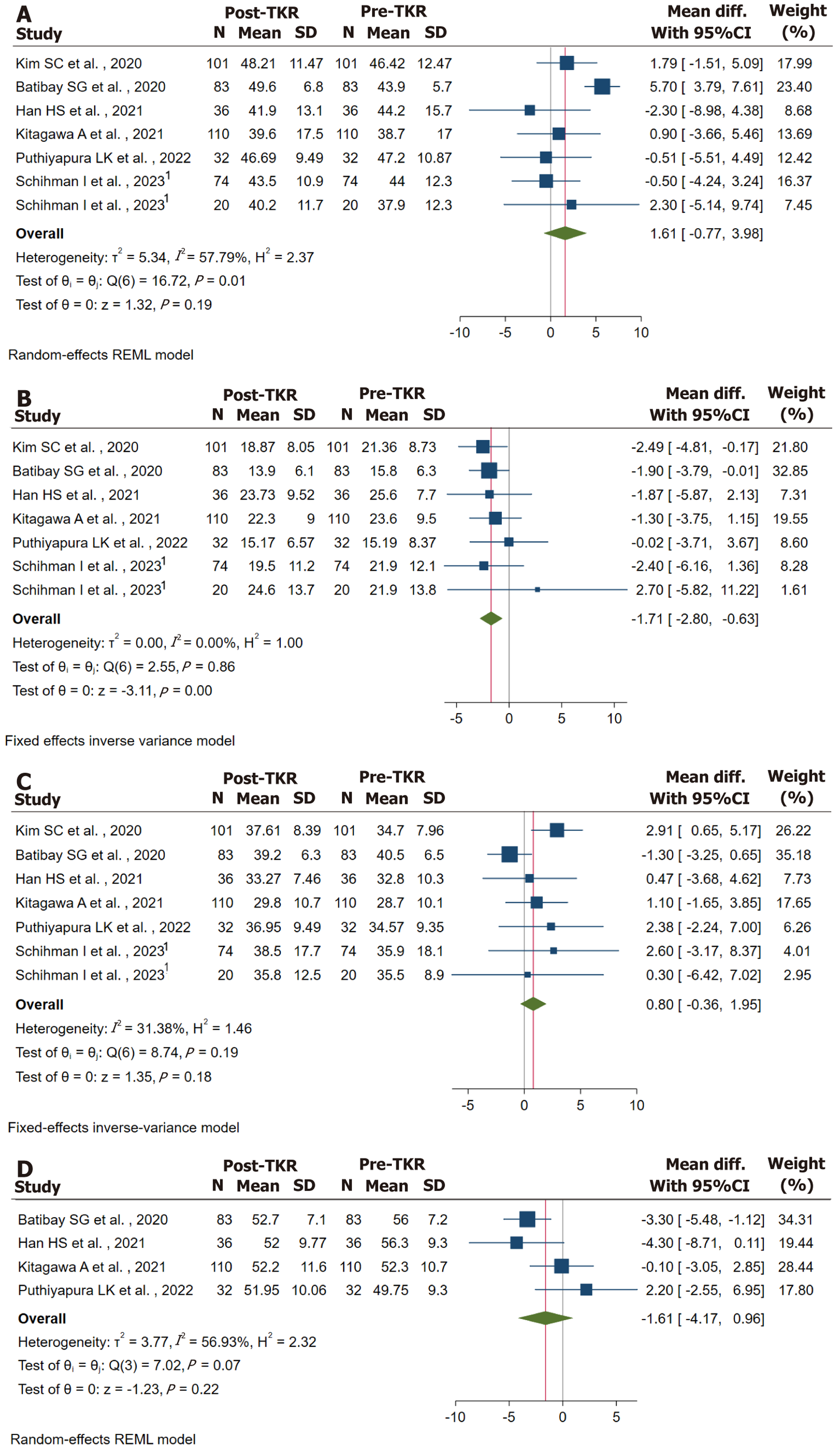
There is significant heterogeneity within the studies incorporated in the meta-analysis (I2 = 57.79%, P = 0.01). There is an increase of 1.361 of LL (95%CI: -0.77 to 3.98), but it was not statistically significant (Figure 2A)[8-13]. The meta-regression analysis estimated a significant association between time of follow-up and change in LL (coefficient 0.56, P value < 0.001).
There is no significant heterogeneity among the studies included in study (I2 = 0.0%, P = 0.86). There is a decrease of 1.71 of PT (95%CI: -2.80 to -0.63), and it was statistically significant (Figure 2B)[8-13]. The meta-regression analysis estimated no significant association between follow-up time and change in PT (co-efficient -0.20, P = 0.866).
There is no substantial heterogeneity among the studies incorporated in our analysis (I2 = 31.38%, P = 0.19). There is an increase of 0.80 of SS (95%CI: -0.36 to 1.95), but it was not statistically significant (Figure 2C)[8-13]. The meta-regression analysis estimated a significant association between follow-up time and change in SS (co-efficient -0.28, P = 0.048).
There is considerable heterogeneity among the studies included in the meta-analysis (I2 = 56.93%, P = 0.07). There is a decrease of 1.61o of PI (95%CI: -4.17 to 0.96), but it was not statistically significant (Figure 2D)[8,10-12]. The meta-regression analysis estimated no considerable association between follow-up time and change in PI (co-efficient -0.17, P = 0.500).
Bipedalism is a stable, ergonomic posture that necessitates the coordination of the alignment of the lower limbs, pelvis, and spine[19]. The sagittal alignment from the cervical spine to the lower extremities functions as an integrated system, where pathology in any segment can disrupt the overall sagittal balance, resulting in compensatory adjustments in other segments. The human body initiates compensatory mechanisms to sustain an upright posture, align the head over the pelvis, and preserve a horizontal gaze[20]. The pelvis adjusts for alterations in the spine within the sagittal plane during the initial phase. The pelvis remains unable to compensate for additional sagittal plane imbalance, potentially resulting in knee flexion[21]. Additional studies have corroborated the association between spinal deformities and compensatory mechanisms in the lower limbs, as well as pelvic translation[20-22].
Our primary finding was that SSA, namely the PT, was corrected by TKA. This finding was observed as early as three months in our study. Patients with OA knees undergoing TKA can have knee deformities, which may activate the compensation mechanism in the pelvis. This can lead to an increase in retroversion, which explains our improvement of PT post-TKA. Kitagawa et al[10] observed a minor decrease and increase in postoperative values of PT and SS due to a slight anteversion of the posterior tilted pelvis, without affecting the intrinsic pelvic morphology. On the other hand, Batibay et al[8] and Han et al[12] found only significant changes in PT but non-significant changes in SS. These studies with a larger number of patients gave a pooled effect of change in PT in our analysis. Lee et al[23] found in their study that patients in which flexion contracture (FC) was corrected to > 10 had improvement in PT though SS did not change. The authors assert that alterations in the knee joint angle significantly influenced the adjacent and more mobile segments, such as the hip and pelvis, more than the rigid degenerative spine. Patients with OA knee can have a FC and TKA is likely to remove the FC. But, often, patients with old age have coexistent spinal and knee degenerative changes. FC of the knee could also be due to an existing spinal problem where the compensatory mechanism has recruited the knees to cause deformity. Here, it seems logical that the FC will improve after TKR. Still, the SSA, being primarily due to spinal disorder, will not alter, and there is a possibility of the FC to return after sometime of surgery if the spinal problems are not addressed. Patients therefore tend to stand with knee flexion without knee FC when evaluated clinically[13]. Therefore, surgeons need a proper understanding of the etiopathogenesis of knee FC and correct them accordingly.
Other parameters do not show significant changes. PI being a morphological parameter does not change for an individual and we had insignificant change in this study. Our inclusion criterion for studies that have recorded SSA pre-TKA and post-TKA. Loss of LL has been identified as the cornerstone of the spinal degenerative cascade. The degenerative changes create a fixed lumbar spine spinal curvature, which does not get corrected by TKA[23]. Therefore, only the compensation mechanism done by the hip/pelvis could be corrected, as seen in our study.
Fontalis et al[7] demonstrated a correlation between SS angle and the knee in reverse, indicating that degenerative alterations in the knee that reduce its extension are offset in the spine by a reduction in LL. Their findings have been reiterated by Batibay et al[8] who found an increase in LL following TKA. But the same was not seen in our pooled effect. Kim et al[13,24] characterised lumbar flexibility (LF) as the differential in LL between extension and flexion while pelvic flexibility (PF) was defined as PI. They reported increased LL in patients exhibiting better LF and change in SS with higher PF (PI) following TKA. We agree with Obeid et al[21] that while these parameters are closely interlinked, it is consistently challenging to ascertain which parameter serves as the primary factor and which acts as a compensatory factor. Jalai et al[22] conducted a further evaluation of the correlation among adult spinal deformity, obesity, and compensatory mechanisms. The authors indicated that the compensation mechanism occurred via the lower extremities in obese patients, whereas in non-obese patients, it was mediated through the pelvic mechanisms.
There are a few drawbacks to our study. We have not separated patients based on unilateral or bilateral TKA and those with or without FC. The SSA could not be translated to change in visual analog score, back pain, or oswestry disability index since most studies lacked the data. While all included studies in our analysis had a standing X-ray, one study by Batibay et al[8] evaluated parameters on a supine lateral view.
The sagittal alignment of the body is a complex equilibrium involving pelvic, spinal, and lower extremity parameters. TKA, while having the potential to correct the FC, can be seen to correct PT, but the primary SSA for spinal pathology, i.e., LL, may not be corrected in patients with co-existent spinal degenerative disease. However, well-conducted randomized controlled trials should be conducted to find out the effect of unilateral or bilateral TKA on spino-pelvic alignment.
| 1. | Steinhaus ME, Christ AB, Cross MB. Total Knee Arthroplasty for Knee Osteoarthritis: Support for a Foregone Conclusion? HSS J. 2017;13:207-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 2. | Hussain SM, Neilly DW, Baliga S, Patil S, Meek R. Knee osteoarthritis: a review of management options. Scott Med J. 2016;61:7-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 108] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 3. | Daher M, Daniels AH, Knebel A, Balmaceno-Criss M, Lafage R, Lenke LG, Ames CP, Burton D, Lewis SM, Klineberg EO, Eastlack RK, Gupta MC, Mundis GM, Gum JL, Hamilton KD, Hostin R, Passias PG, Protopsaltis TS, Kebaish KM, Kim HJ, Schwab F, Shaffrey CI, Smith JS, Line B, Bess S, Lafage V, Diebo BG; International Spine Study Group (ISSG). Impact of Knee Osteoarthritis and Arthroplasty on Full-body Sagittal Alignment in Adult Spinal Deformity Patients. Spine (Phila Pa 1976). 2025;50:508-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 4. | Vigdorchik JM, Shafi KA, Kolin DA, Buckland AJ, Carroll KM, Jerabek SA. Does Low Back Pain Improve Following Total Hip Arthroplasty? J Arthroplasty. 2022;37:S937-S940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Jain M, Mohapatra A, Tripathy SK, Mohakud S, Das A, Sethy SS. Do Spinopelvic Parameters Relate with Secondary Hip Spine Syndrome in Secondary Hip Arthritis? Indian J Orthop. 2022;56:1937-1943. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 6. | Hambrecht J, Köhli P, Chiapparelli E, Zhu J, Guven AE, Evangelisti G, Burkhard MD, Tsuchiya K, Duculan R, Altorfer FCS, Shue J, Sama AA, Cammisa FP, Girardi FP, Mancuso CA, Hughes AP. The spinopelvic alignment in patients with prior knee or hip arthroplasty undergoing elective lumbar surgery. Spine J. 2025;25:45-54. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Fontalis A, Buchalter D, Mancino F, Shen T, Sculco PK, Mayman D, Haddad FS, Vigdorchik J. Contemporary insights into spinopelvic mechanics. Bone Joint J. 2024;106-B:1206-1215. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Batibay S, Akgul T, Koca H, Camur S, Kaya O, Bayram S, Saglam N. Effects of bilateral knee arthroplasty on sagittal spinopelvic balance in patients with primer degenerative osteoarthritis. Ann Med Res. 2020;27:233. [DOI] [Full Text] |
| 9. | Shichman I, Ben-Ari E, Sissman E, Singh V, Hepinstall M, Schwarzkopf R. Total knee arthroplasty in patients with lumbar spinal fusion leads to significant changes in pelvic tilt and sacral slope. Arch Orthop Trauma Surg. 2023;143:2103-2110. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Kitagawa A, Yamamoto J, Toda M, Hashimoto Y. Spinopelvic Alignment and Low Back Pain before and after Total Knee Arthroplasty. Asian Spine J. 2021;15:9-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Puthiyapura LK, Jain M, Tripathy SK, Puliappadamb HM. Effect of osteoarthritic knee flexion deformity correction by total knee arthroplasty on sagittal spinopelvic alignment in Indian population. World J Clin Cases. 2022;10:7348-7355. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Reference Citation Analysis (0)] |
| 12. | Han HS, Yun KR, Cho K, Kim TW, Kang SB. Relationships between the changes in flexion contracture and standing flexion angle of the knee and sagittal spinal alignment after total knee arthroplasty. Knee. 2021;29:374-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Kim SC, Kim JS, Choi HG, Kim TW, Lee YS. Spinal Flexibility Is an Important Factor for Improvement in Spinal and Knee Alignment after Total Knee Arthroplasty: Evaluation Using a Whole Body EOS System. J Clin Med. 2020;9:3498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 39257] [Article Influence: 9814.3] [Reference Citation Analysis (2)] |
| 15. | StataCorp. Stata Statistical Software: Release 12. United States: StataCorp LP. 2011. [cited 13 June 2025]. Available from: https://www.stata.com/stata12/. |
| 16. | Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7683] [Cited by in RCA: 10684] [Article Influence: 1187.1] [Reference Citation Analysis (2)] |
| 17. | Dalton JE, Bolen SD, Mascha EJ. Publication Bias: The Elephant in the Review. Anesth Analg. 2016;123:812-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 211] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 18. | Lee SM, Yoon MG, Moon MS, Lee BJ, Lee SR, Seo YH. Effect of correction of the contractured flexed osteoarthritic knee on the sagittal alignment by total replacement. Asian Spine J. 2013;7:204-211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Le Huec JC, Charosky S, Barrey C, Rigal J, Aunoble S. Sagittal imbalance cascade for simple degenerative spine and consequences: algorithm of decision for appropriate treatment. Eur Spine J. 2011;20 Suppl 5:699-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 137] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 20. | Ferrero E, Liabaud B, Challier V, Lafage R, Diebo BG, Vira S, Liu S, Vital JM, Ilharreborde B, Protopsaltis TS, Errico TJ, Schwab FJ, Lafage V. Role of pelvic translation and lower-extremity compensation to maintain gravity line position in spinal deformity. J Neurosurg Spine. 2016;24:436-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 21. | Obeid I, Hauger O, Aunoble S, Bourghli A, Pellet N, Vital JM. Global analysis of sagittal spinal alignment in major deformities: correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J. 2011;20 Suppl 5:681-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 158] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 22. | Jalai CM, Cruz DL, Diebo BG, Poorman G, Lafage R, Bess S, Ramchandran S, Day LM, Vira S, Liabaud B, Henry JK, Schwab FJ, Lafage V, Passias PG. Full-Body Analysis of Age-Adjusted Alignment in Adult Spinal Deformity Patients and Lower-Limb Compensation. Spine (Phila Pa 1976). 2017;42:653-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 23. | Lee CS, Park SJ, Chung SS, Lee KH. The effect of simulated knee flexion on sagittal spinal alignment: novel interpretation of spinopelvic alignment. Eur Spine J. 2013;22:1059-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 24. | Kim SC, Choi HG, Kim JS, Kim TW, Lee YS. Effects of Total Knee Arthroplasty on Coronal and Sagittal Whole-Body Alignments: Serial Assessments Using Whole-Body EOS. J Clin Med. 2021;10:3242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |