Published online Jul 18, 2025. doi: 10.5312/wjo.v16.i7.107087
Revised: April 12, 2025
Accepted: May 28, 2025
Published online: July 18, 2025
Processing time: 124 Days and 18 Hours
Retrograde pubic ramus screw placement is an effective technique but requires substantial surgical expertise and specialized equipment. The management of osteoporotic anterior pelvic ring injuries remains challenging due to technical difficulties and a high risk of complications.
To introduce a novel and simplified surgical approach that utilizes a custom-designed handheld pelvic alignment guide (HPAG) in combination with a 6.0 mm hollow screw, aiming to enhance the accuracy, efficiency, and safety of retrograde pubic ramus screw fixation in osteoporotic pelvic fragility fractures.
The HPAG and 6.0 mm hollow screw were employed during surgical treatment. A 2.0-3.0 cm incision was made to expose the optimal screw entry point. Intraoperative pelvic inlet and obturator oblique views were used to monitor fracture reduction and guide screw insertion. Clinical outcomes and fracture reduction quality were evaluated using Matta, visual analog scale, and Majeed scores during follow-ups. A representative case is presented to demonstrate the surgical procedure in detail.
No perioperative complications were observed. The mean operative time was 35.2 ± 6.97 minutes, with a screw insertion time of 7.25 ± 1.86 minutes, an average incision length of 2.8 ± 0.67 cm, and mean blood loss of 43.25 ± 15.64 mL. At one-year follow-up, seven patients achieved excellent Majeed scores and three achieved good scores.
The HPAG technique significantly shortens operative time, minimizes surgical trauma, and facilitates accurate screw placement. It presents a promising and efficient approach for managing fragility fractures of the pelvis, especially in osteoporotic patients.
Core Tip: This technical report introduces a novel handheld pelvic alignment guide (HPAG) combined with 6.0 mm hollow screws, specifically designed for accurate and minimally invasive retrograde pubic ramus screw insertion in osteoporotic pelvic fragility fractures. The technique reduces operative time, incision size, and intraoperative fluoroscopy, minimizing surgical trauma. HPAG simplifies a technically demanding procedure, enables wider adoption, and demonstrates excellent clinical outcomes, highlighting its potential as a standard surgical approach in osteoporotic anterior pelvic ring injuries.
- Citation: Wang Y, Tan ZY, He JM, Shu YX, Pan Z, Zhu DG, Wang J. Novel handheld pelvic alignment guide for hollow screw fixation in osteoporotic pelvic fragility fractures. World J Orthop 2025; 16(7): 107087
- URL: https://www.wjgnet.com/2218-5836/full/v16/i7/107087.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i7.107087
With the aging of the population, the incidence of fragility fractures of the pelvis (FFPs) continues to rise[1,2]. Pelvic fractures account for approximately 3% of all fractures, and the incidence of FFPs is projected to increase by 2.4-fold by 2030[3]. Osteoporotic pelvic fractures often result in prolonged bed rest, higher mortality rates, and increased healthcare costs, placing substantial economic burdens on patients and society[4,5].
The anterior pelvic ring, composed of the pubic symphysis and the superior and inferior pubic rami, contributes to ~40% of overall pelvic stability[6]. In cases of FFPs, up to 98% of patients present with anterior pelvic ring injuries[7]. Traditionally, types I and II FFPs have been managed conservatively. However, post-fracture instability of the anterior pelvic ring often leads to persistent pain and immobility in elderly patients, resulting in severe complications[8,9]. Studies have shown that even isolated pubic ramus fractures are associated with an one-year mortality rate of 17.5% to 24.0%[10]. As a result, there is growing acceptance of surgical interventions for the treatment of osteoporotic anterior pelvic ring injuries.
Currently, primary surgical techniques for anterior pelvic ring injuries include open reduction and internal fixation (ORIF), external fixation, and percutaneous screw fixation[11]. Compared with traditional ORIF using plating, retrograde screw fixation through the superior pubic ramus provides comparable biomechanical stability while resulting in less surgical trauma, reduced blood loss, and a lower risk of neurovascular injury[12]. Despite these advantages, the technique requires a high degree of precision and surgical skill. Furthermore, because FFP patients are often elderly women with smaller, osteoporotic bones, concerns remain regarding the appropriate screw diameter for achieving optimal fixation[13]. Therefore, improving the success rate and safety of screw placement, while minimizing operative time and blood loss, is crucial for the effective treatment of FFPs.
In this study, we modified the design of hollow screws by selecting 6.0 mm partially threaded screws for retrograde fixation through the superior pubic ramus, adapting the design to accommodate anatomical variations across different populations. Additionally, we developed a handheld pelvic alignment guide (HPAG) to simplify the screw placement process and improve accuracy. This novel approach demonstrates significant potential for the treatment of osteoporotic anterior pelvic ring injuries.
Recent advances in three-dimensional (3D) printing and computer-assisted navigation technologies have significantly improved the safety and precision of screw placement in orthopedic surgery[14,15]. However, these methods often require high-end equipment, incur substantial costs, and remain challenging to implement widely in routine clinical practice. Compared to these advanced techniques, the HPAG device offers several distinct advantages. While 3D-printed surgical guides and navigation systems provide high accuracy, they are limited by the need for complex infrastructure and specialized training. In contrast, the HPAG is a cost-effective, portable, and intuitive tool that does not rely on sophisticated equipment. Its simplified design facilitates rapid clinical adoption, making it particularly suitable for primary healthcare institutions and low-resource settings. These advantages position the HPAG as a practical and widely accessible solution for enhancing surgical accuracy in the treatment of osteoporotic pelvic fragility fractures.
This single-center, retrospective clinical trial was conducted at Tongren Hospital, School of Medicine, Shanghai Jiao Tong University from January 2021 to December 2022. The study protocol was approved by the Institutional Ethics Committee of Tongren Hospital (Approval No. K2024-006-001). Written informed consent was obtained from all participants prior to enrollment.
Ten patients diagnosed with unstable anterior pelvic ring injuries were enrolled. All fractures were classified as FFPs type I or II according to the Rommens and Hofmann classification system, with four patients presenting type I fractures and six presenting type II fractures (Table 1). All injuries resulted from low-energy lateral falls. The mean age at the time of injury was 67.2 years (range, 64-82 years), with three males and seven females. Osteoporosis was confirmed in all patients by dual-energy X-ray absorptiometry (DXA), with a T-score ≤ –2.5. Surgery was performed once the patients' conditions were adequately stabilized.
| No. | Age | Sex | Operation time (min) | Blood loss (mL) | Incision length (cm) | SSIT | IFC | Screw length (mm) | VAS score | |
| Pre OP | Post OP | |||||||||
| 1 | 64 | F | 98 | 105 | 3 | 12 | 15 | 50, 70 | 9 | 3 |
| 2 | 65 | F | 35 | 30 | 3 | 7 | 6 | 70 | 6 | 2 |
| 3 | 60 | F | 32 | 50 | 2 | 6.5 | 6 | 65 | 5 | 1 |
| 4 | 64 | M | 30 | 20 | 2 | 6 | 6 | 70 | 6 | 2 |
| 5 | 75 | F | 42 | 35 | 3.5 | 7.5 | 6 | 65 | 7 | 1 |
| 6 | 67 | F | 60 | 80 | 3 | 7 | 6 | 55, 50 | 8 | 2 |
| 7 | 67 | M | 35 | 50 | 3 | 6.5 | 6 | 80 | 6 | 1 |
| 8 | 82 | M | 28 | 30 | 2.5 | 5 | 6 | 75 | 5 | 2 |
| 9 | 64 | F | 58 | 100 | 2 | 7 | 6 | 55, 55 | 9 | 4 |
| 10 | 64 | F | 84 | 150 | 4 | 8 | 9 | 60, 65 | 7 | 3 |
| Average | 67.5 | 35.2 | 43.25 | 2.8 | 7.25 | 7 | 62.5 | 6.8 | 2.1 | |
The inclusion criteria were: (1) Age ≥ 60 years; (2) Radiologically confirmed FFPs type I or II with anterior pelvic ring involvement; (3) T-score ≤ –2.5 on DXA scan; and (4) Ability to tolerate surgery and provide informed consent.
The exclusion criteria were: (1) Posterior pelvic ring instability requiring additional fixation; (2) Pathological fractures due to tumor or infection; (3) Polytrauma or multiple fractures; and (4) Severe comorbidities such as uncontrolled cardiovascular, hepatic, or renal disease.
All patients underwent surgical treatment using the HPAG and 6.0 mm hollow screws, as described in the Surgical Procedure section.
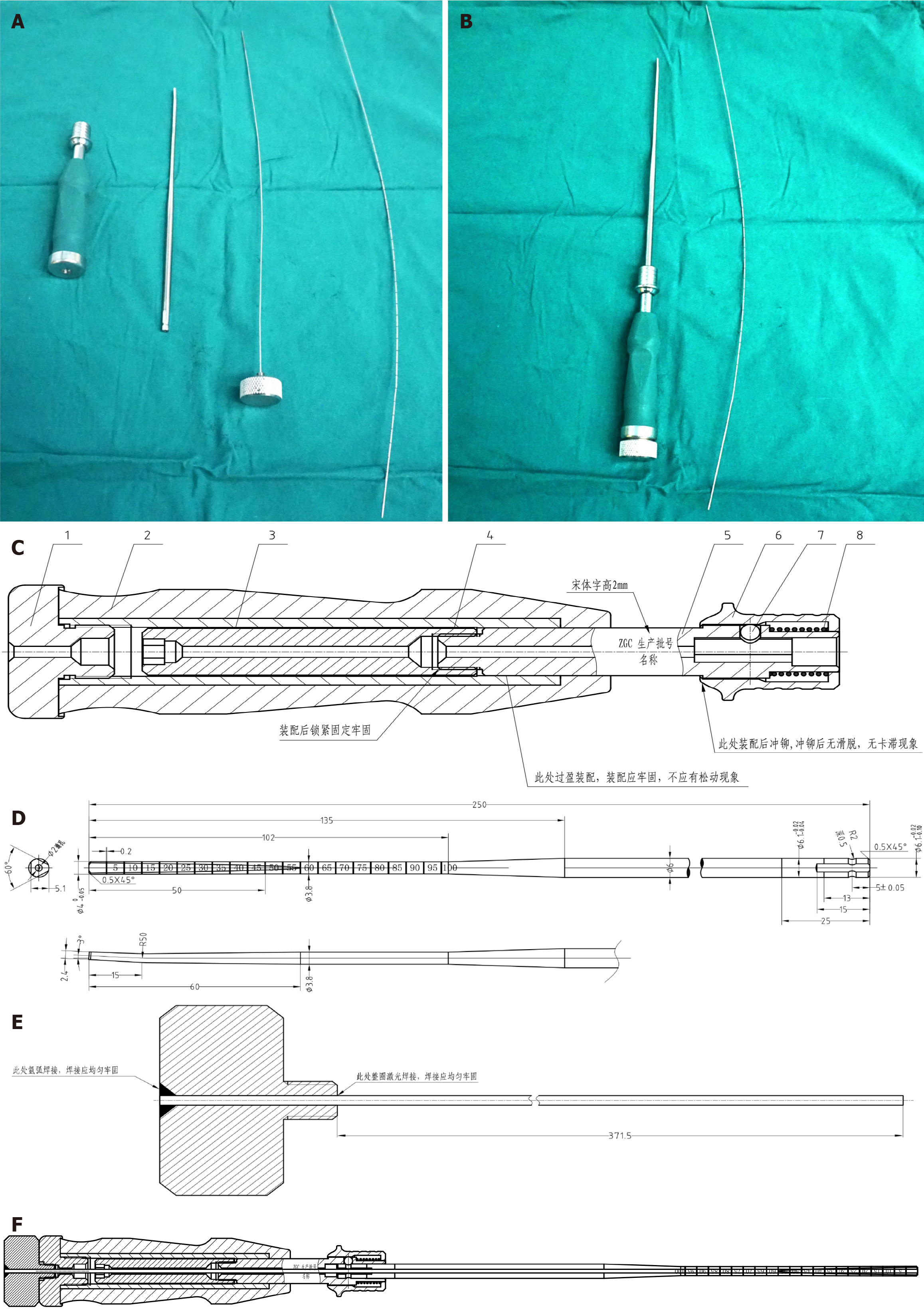
The HPAG device, developed by our research team, has been granted a Chinese national utility model patent (Supplementary material, Blinded for Review). The device consists of a guide pin, handle, and probe, sequentially connected (Figure 1A). Both the handle and probe contain central through-holes, allowing the guide pin to slide within them (Figure 1B). The guide pin is connected to the handle via a threaded cap (Figure 1C). A spring mechanism at the front end of the handle allows for secure attachment of the probe (Figure 1C). The probe is prismatic, marked with graduated scales, and features a 3-7° inclined tip (Figure 1D). This design provides high structural strength during use, facilitates fracture reduction, and guides the wire away from the acetabulum. The threaded connection between the guide pin and handle prevents complications such as bone blockage within the probe and guide pin dislodgement (Figure 1E). The graduations on the probe allow direct measurement of the required screw length, significantly reducing operative time and procedural steps (Figure 1F).
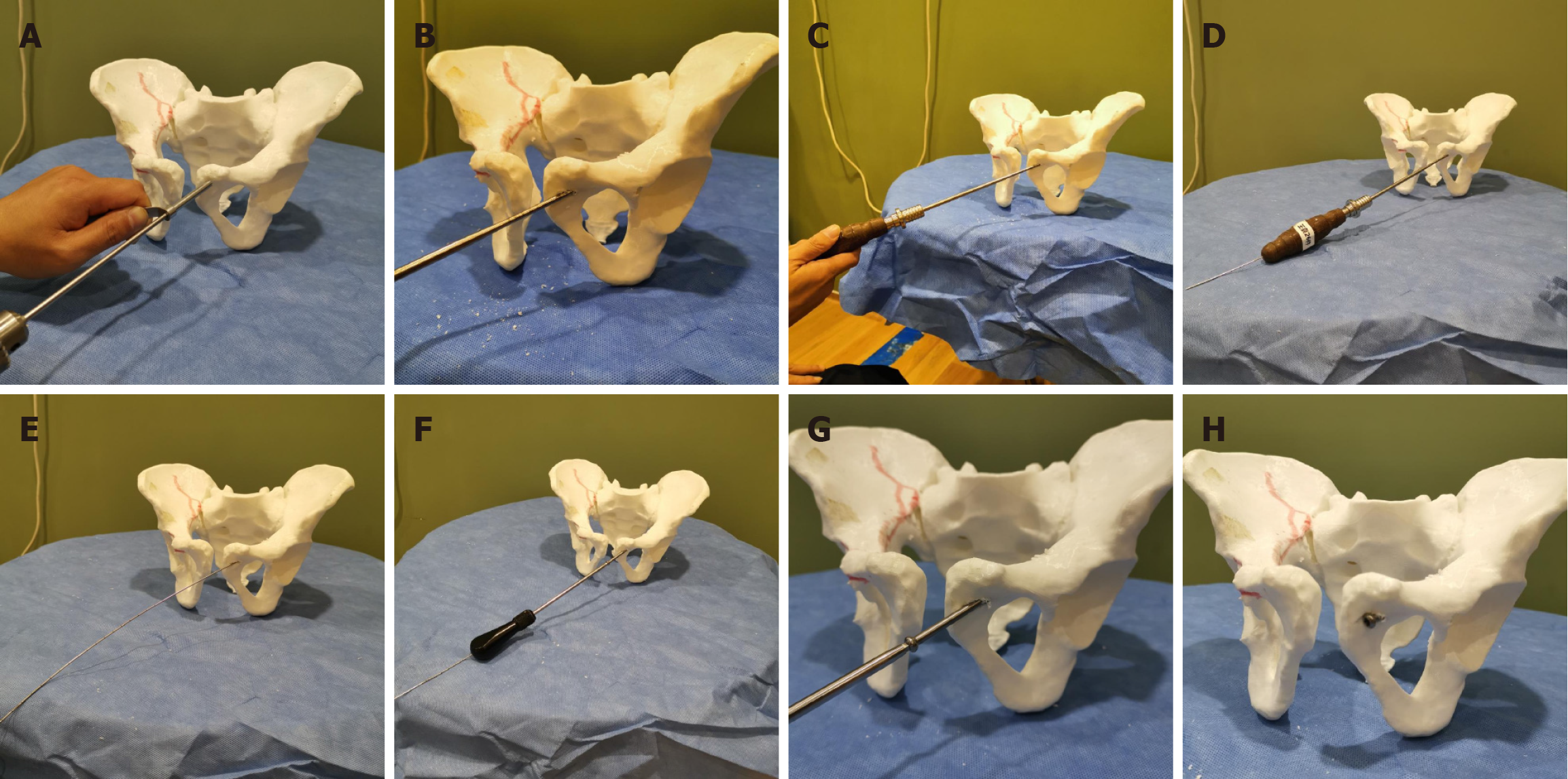
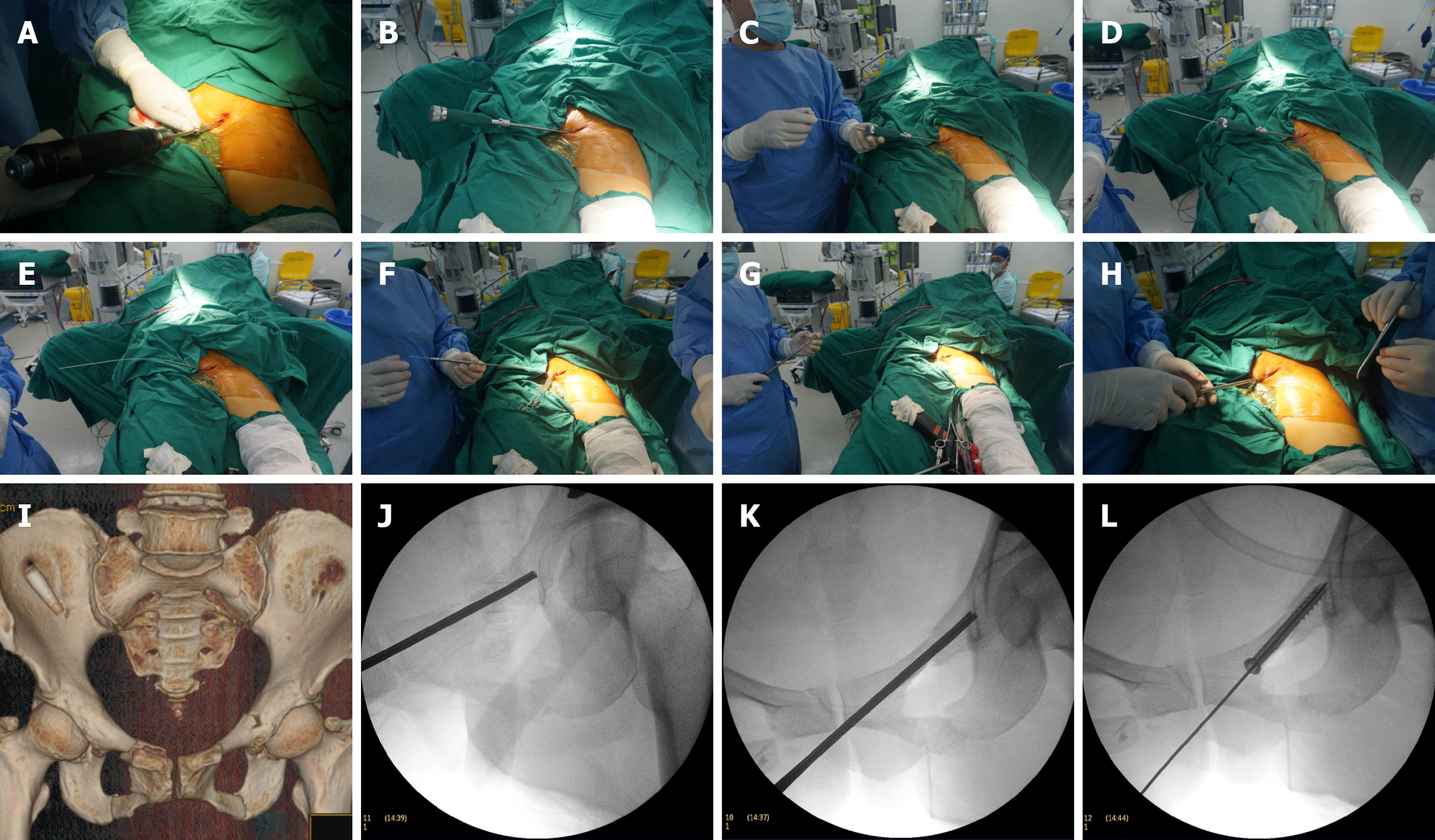
Surgery was performed under general anesthesia with the patient in a supine position on an orthopedic traction table. Following surgical traction, satisfactory reduction was confirmed using C-arm fluoroscopy. Routine disinfection and sterile draping were then performed. A 2-cm lateral incision was made at the pubic symphysis, and a 3.5-mm drill bit was used to create an initial hole (Figure 2A; Figure 3A). The HPAG handle was used to insert the probe head into the superior pubic ramus, which was gently rotated through the fracture site under fluoroscopic guidance (Figure 2B and C; Figure 3B). Intraoperative fluoroscopy included two views: (1) Pelvic inlet view with 30° cranial tilt to assess the anterior cortex of the pubis and detect any penetration of the pelvic ring; and (2) Obturator oblique view with 45° ipsilateral rotation to evaluate the screw trajectory and detect posterior cortical breach.
Once the position was confirmed under fluoroscopy, the probe's surface markings were read to determine the appropriate length of the 6.0-mm hollow screw (Figure 2D; Figure 3C and D). The inner core, handle, and probe were sequentially removed, leaving the guide wire in place (Figure 2E and F and Figure 3E and F). The hollow screw was then inserted along the guide wire. Its position was confirmed under fluoroscopy before the incision was irrigated and sutured (Figure 2G and H; Figure 3G-L).
Perioperative data, including operative time, fluoroscopy frequency per screw, intraoperative blood loss, incision length, and perioperative complications, were recorded. Postoperative pelvic radiographs and computed tomography (CT) scans of the pelvis were obtained on postoperative day 2[16]. Fracture reduction was assessed according to Matta's criteria, where a maximum displacement of ≤ 4 mm was classified as excellent, 5-10 mm as good, 10-20 mm as fair, and > 20 mm as poor. Pain was assessed using the visual analog scale (VAS), a standardized 10-point scale, where 0 indicates "no pain" and 10 indicates "worst imaginable pain". Patients rated their pain levels at rest and during ambulation at each follow-up visit. Outpatient follow-ups were conducted at 1, 3, 6, and 12 months postoperatively. Clinical outcomes were evaluated using the Majeed pelvic function score at 12 months[17].
Quantitative data are expressed as the mean ± SD or SEM, and group comparisons were performed using independent samples t-tests. Categorical data, presented as percentages, were compared using χ2 tests. Comparisons of ordinal data were performed using Wilcoxon rank-sum tests. Statistical analyses were conducted using SPSS 27.0 software. P < 0.05 was considered statistically significant.
Surgical outcomes were evaluated in ten patients (3 males and 7 females; mean age, 67.2 ± 6.48 years; range, 64-82 years) (Table 1). Fracture types were classified according to the Rommens and Hofmann system, with six patients presenting with FFPs type I and four with FFPs type II. All injuries resulted from low-energy lateral falls on a horizontal surface. The average interval from injury to surgery was 5.6 ± 2.5 days.
Among the ten patients, six had unilateral injuries and four had bilateral injuries, resulting in the implantation of 14 hollow 6.0 mm screws. The average screw length was 62.5 ± 9.32 mm. No cases of screw misplacement or acetabular penetration were observed. The mean surgical duration was 35.2 ± 6.97 minutes, and the average time to insert a single screw was 7.25 ± 1.86 minutes. The intraoperative fluoroscopy frequency count per screw (IFC) was 7.2 ± 2.90 times. Mean intraoperative blood loss was 43.25 ± 15.64 mL. For the four patients with FFPs type II, stabilization of the posterior pelvic ring was performed using minimally invasive techniques such as external fixation or sacroiliac screw fixation. The surgical time and blood loss associated with these additional procedures were included in the overall calculations.
Clinical outcomes were evaluated using preoperative and postoperative day 2 VAS scores, Matta scores, and Majeed scores at the 12-month follow-up. All ten patients completed follow-ups at 1, 3, 6, and 12 months postope
| No. | Majeed score (12 months)/100 | Matta score (mm) | Complication | |||||
| Pain/30 | Work/20 | Sitting/10 | Sex life/4 | Standing/36 | Total | |||
| 1 | 25 | 20 | 10 | 3 | 32 | 90 | 2 | / |
| 2 | 30 | 16 | 8 | 2 | 32 | 88 | 3 | / |
| 3 | 30 | 16 | 8 | 4 | 32 | 90 | 5 | / |
| 4 | 25 | 16 | 10 | 4 | 30 | 85 | 4 | / |
| 5 | 30 | 20 | 10 | 0 | 30 | 90 | 3 | / |
| 6 | 25 | 12 | 8 | 3 | 32 | 80 | 5 | / |
| 7 | 25 | 16 | 8 | 4 | 32 | 85 | 3 | / |
| 8 | 30 | 12 | 8 | 0 | 30 | 80 | 3 | / |
| 9 | 25 | 16 | 8 | 2 | 30 | 81 | 4 | / |
| 10 | 30 | 20 | 8 | 3 | 32 | 93 | 8 | / |
| Average | / | / | / | / | / | 86.2 | 4 | / |
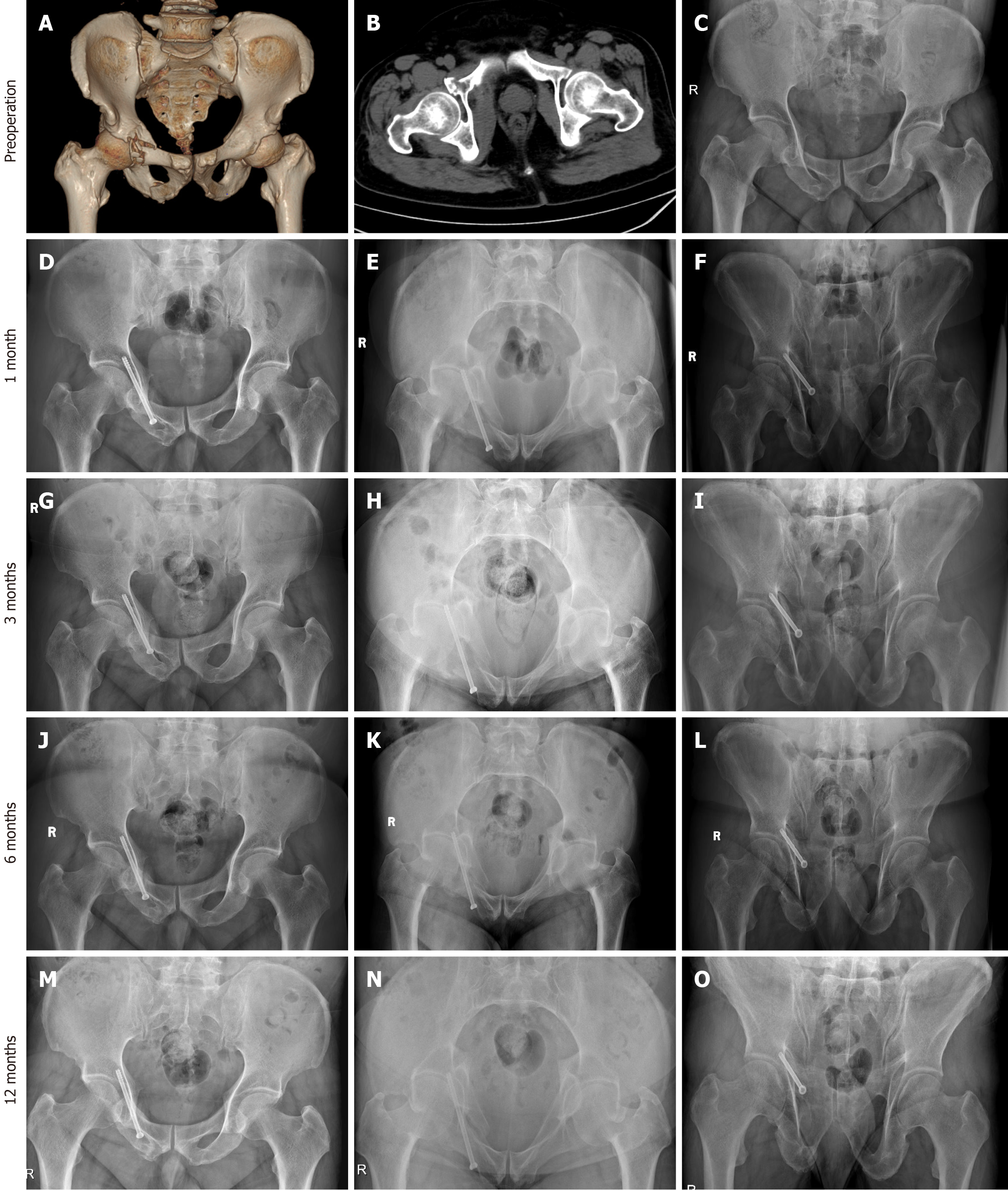
An 82-year-old male patient sustained a right pubic fracture from a fall at home, classified as FFP type I and AO/OTA type A1. Preoperative X-rays and 3D CT scans are shown in Figure 4. The patient had a history of hypertension and diabetes and experienced severe pain that prevented movement and bed turning. Initial temporary fixation was performed using a pelvic external fixator on the day of injury. After thorough assessment, it was determined that the patient could not tolerate prolonged bed rest. As there were no absolute contraindications to surgery, the patient underwent HPAG-guided surgery on the third day post-injury. The total surgical time was 28 minutes, with screw insertion requiring 5 minutes and intraoperative blood loss totaling 30 mL. The incision length was 2.5 cm. On the second postoperative day, the patient was able to turn over and sit up in bed. The VAS score decreased from 5 preoperatively to 2 postoperatively. The patient was discharged on the 7th postoperative day. Follow-ups at 1, 3, 6, and 12 months postoperatively revealed fracture healing by the third month. At 12 months, the Majeed score was 80, indicating a good functional outcome.
This technical report presents the application of 6.0 mm hollow screws in combination with the HPAG for treating osteoporotic anterior pelvic ring injuries in ten patients. Traditionally, unstable anterior pelvic ring injuries have been managed using anterior plate fixation[18]. However, conservative management in elderly patients is associated with high rates of mortality and complications. Percutaneous retrograde hollow screw fixation has emerged as a minimally invasive alternative; however, it presents significant challenges regarding screw placement accuracy and procedural safety[3]. The technique described herein simplifies the screw insertion process, enhances procedural safety, and results in favorable clinical outcomes for patients with FFPs.
Percutaneous retrograde screw fixation for anterior pelvic ring injuries has been investigated as a minimally invasive technique in several studies[19,20]. Due to the anatomical characteristics of the superior pubic ramus, precise angulation and inclination of the guide pin and screw are required during insertion to prevent cortical breaches and screw misplacement. Wang et al[16] reported an improved success rate for percutaneous retrograde pubic ramus screw insertion by utilizing a spinal surgery hollow reamer. Recent advancements in 3D printing and computer navigation technologies have significantly improved the safety of screw placement; however, their widespread application is limited by high equipment costs and technical complexity[14,15,21,22]. In response, we developed the HPAG, featuring a hollow design with an internal threaded core to prevent blockage by bone debris during navigation. The curved tip facilitates adjustment of the guide pin trajectory, aiding fracture reduction and preventing acetabular penetration. This innovation simplifies the surgical procedure and improves success rates of screw placement. In our study, the mean surgical duration was 35.2 minutes, and the mean screw insertion time was 7.25 minutes, thereby reducing the risks associated with prolonged anesthesia.
FFPs predominantly affect elderly women, who typically have smaller and more osteoporotic bones, raising concerns regarding the optimal screw diameter for stable fixation. Screws that are too thin may lead to loosening and instability, whereas screws that are too thick may cause cortical breaches. Previous studies have demonstrated that single screws (6.5 mm or 7.3 mm) or two 3.5 mm screws are feasible for achieving stable fixation[23,24]. The narrowest segment of the anterior pelvic ring is located between the superior pubic ramus and the anterior margin of the acetabulum. Anatomical studies have reported that the permissible diameter for tension screws ranges from 5.70 to 14.10 mm in males and from 4.40 to 10.40 mm in females[25]. In our study, all patients underwent fixation with 6.0 mm hollow screws. At one-year follow-up, excellent fixation was achieved, with no cases of screw loosening or displacement.
The HPAG is a minimally invasive device designed to simplify the surgical procedure for anterior pelvic ring injuries. However, several limitations of this study should be acknowledged. First, the sample size was relatively small, and the follow-up period was limited to 12 months. Second, although the clinical outcomes were encouraging, the HPAG device has not yet undergone formal biomechanical validation. Quantitative evaluation of its mechanical stability and performance under physiological loading conditions is necessary to provide more robust evidence supporting its effectiveness. Third, although all patients met diagnostic criteria for osteoporotic fragility fractures, individual bone mineral density (BMD) measurements were neither recorded nor analyzed. Considering the critical role of BMD in fracture healing and implant fixation, future studies should incorporate BMD-based stratification and analysis. Larger cohorts with extended follow-up durations, along with additional biomechanical and BMD-related data, are needed to more comprehensively validate the safety and efficacy of this technique for managing osteoporotic anterior pelvic ring injuries.
In conclusion, the combination of 6.0 mm hollow screws and the HPAG provides a technically feasible, safe, and efficient solution for the treatment of osteoporotic anterior pelvic ring injuries. Our clinical results demonstrate high screw placement accuracy, shorter operative times, and improved functional outcomes with minimal complications. Given its simplicity, minimal invasiveness, and cost-effectiveness, this technique shows strong potential for widespread clinical application, especially in resource-limited settings.
| 1. | Sivapathasuntharam D, Smith G, Master MA, Bates P. Fragility fractures of the pelvis in the older population. Age Ageing. 2022;51:afac063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 2. | Nanninga GL, de Leur K, Panneman MJ, van der Elst M, Hartholt KA. Increasing rates of pelvic fractures among older adults: The Netherlands, 1986-2011. Age Ageing. 2014;43:648-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 3. | Rollmann MF, Herath SC, Holstein JH, Pohlemann T, Menger MD, Histing T. Surgical treatment of pelvic ring fractures in the elderly now and then: a pelvic registry study. Aging Clin Exp Res. 2017;29:639-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Petryla G, Uvarovas V, Bobina R, Kurtinaitis J, Khan SA, Versocki A, Porvaneckas N, Šatkauskas I. The one-year mortality rate in elderly patients with osteoporotic fractures of the pelvis. Arch Osteoporos. 2020;15:15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Maier GS, Kolbow K, Lazovic D, Horas K, Roth KE, Seeger JB, Maus U. Risk factors for pelvic insufficiency fractures and outcome after conservative therapy. Arch Gerontol Geriatr. 2016;67:80-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 74] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 6. | Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop Relat Res. 1989;83-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 136] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Henry SM, Pollak AN, Jones AL, Boswell S, Scalea TM. Pelvic fracture in geriatric patients: a distinct clinical entity. J Trauma. 2002;53:15-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 83] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Reito A, Kuoppala M, Pajulammi H, Hokkinen L, Kyrölä K, Paloneva J. Mortality and comorbidity after non-operatively managed, low-energy pelvic fracture in patients over age 70: a comparison with an age-matched femoral neck fracture cohort and general population. BMC Geriatr. 2019;19:315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 9. | Alnaib M, Waters S, Shanshal Y, Caplan N, Jones S, St Clair Gibson A, Kader D. Combined pubic rami and sacral osteoporotic fractures: a prospective study. J Orthop Traumatol. 2012;13:97-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Spiegl UJA, Schnake KJ, Osterhoff G, Scheyerer MJ, Ullrich B, Bula P, Siekmann H. Imaging of Sacral Stress and Insufficiency Fractures. Z Orthop Unfall. 2019;157:144-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Culemann U, Scola A, Tosounidis G, Pohlemann T, Gebhard F. [Concept for treatment of pelvic ring injuries in elderly patients. A challenge]. Unfallchirurg. 2010;113:258-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Shieh AK, Hayes CB, Shelton TJ, Chip Routt ML Jr, Eastman JG. Low Superior Pubic Ramus Screw Failure Rate With Combined Anterior and Posterior Pelvic Ring Fixation. J Orthop Trauma. 2021;35:175-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Hutchings L, Roffey DM, Lefaivre KA. Fragility Fractures of the Pelvis: Current Practices and Future Directions. Curr Osteoporos Rep. 2022;20:469-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 14. | Hiyama A, Ukai T, Nomura S, Watanabe M. The combination of intraoperative CT navigation and C-arm fluoroscopy for INFIX and percutaneous TITS screw placement in the treatment of pelvic ring injury: technical note. J Orthop Surg Res. 2022;17:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Hiyama A, Ukai T, Ogasawara S, Tanaka T, Watanabe M. Minimally Invasive 360° Fusion Using a Combination of INFIX and Minimally Invasive Spinopelvic Fixation by Intraoperative Computed Tomography Navigation for Unstable Pelvic Ring Fracture: A Technical Note. Orthop Surg. 2023;15:1405-1413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 16. | Wang H, Wu G, Chen CY, Qiu YY, Xie Y. Percutaneous screw fixation assisted by hollow pedicle finder for superior pubic ramus fractures. BMC Surg. 2022;22:216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 17. | Majeed SA. Grading the outcome of pelvic fractures. J Bone Joint Surg Br. 1989;71:304-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 308] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 18. | Oh HK, Choo SK, Kim JJ, Lee M. Stoppa Approach for Anterior Plate Fixation in Unstable Pelvic Ring Injury. Clin Orthop Surg. 2016;8:243-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Yuan Y, Wang T, Yuan J, Qu G, Hao P, Zeng Z, Luo B, Yang J. [Treatment of Day type Ⅱ pelvic crescent fracture by using percutaneous cannulated screw fixation technique]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2018;32:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 20. | Rommens PM, Graafen M, Arand C, Mehling I, Hofmann A, Wagner D. Minimal-invasive stabilization of anterior pelvic ring fractures with retrograde transpubic screws. Injury. 2020;51:340-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 21. | Takao M, Hamada H, Sakai T, Sugano N. Clinical Application of Navigation in the Surgical Treatment of a Pelvic Ring Injury and Acetabular Fracture. Adv Exp Med Biol. 2018;1093:289-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Florio M, Capasso L, Olivi A, Vitiello C, Leone A, Liuzza F. 3D - Navigated percutaneous screw fixation of pelvic ring injuries - a pilot study. Injury. 2020;51 Suppl 3:S28-S33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 23. | Acklin YP, Zderic I, Grechenig S, Richards RG, Schmitz P, Gueorguiev B. Are two retrograde 3.5 mm screws superior to one 7.3 mm screw for anterior pelvic ring fixation in bones with low bone mineral density? Bone Joint Res. 2017;6:8-13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Flanagan CD, Fairchild R, McCaskey M, Sajid MI, Watson D, Mir H. Union and displacement characteristics following percutaneous screw fixation of superior pubic rami fractures. Eur J Orthop Surg Traumatol. 2024;34:3535-3541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 25. | Bai Y, Liu Q. [Digital study of the ideal position of lag screw internal fixation in the anterior column of the acetabulum]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35:684-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |