Published online Jul 18, 2025. doi: 10.5312/wjo.v16.i7.105111
Revised: April 13, 2025
Accepted: June 7, 2025
Published online: July 18, 2025
Processing time: 187 Days and 0.1 Hours
Difficult total hip replacements (THRs) are hip arthroplasties performed on patients with compromised or severely altered bone or soft tissue. Difficult THR indications are common in low-income countries, where access to care is often delayed. In these contexts, patients generally consult us with severe impairments that require significant technical adaptations, as well as adaptation to available resources and local conditions.
To describe the results and difficulties encountered following difficult THR in the study center.
This bi-centric retrospective study was conducted over a 10-year period (2013-2023) and included 50 patients operated on for difficult THR. The mean age of the patients was 37.8 years. Surgical difficulties were recorded from operative reports, and the strategies employed to overcome these difficulties were analyzed, taking into account the types of implants used.
At last follow-up, functional results were considered good to excellent according to the Postel-Merle d'Aubigné score, with significant improvement after surgery (P < 0.005). Mean operative time was 177 minutes (range: 90-290 minutes), with a mean blood loss of 568 mL (range: 200-900 mL). The short-term and medium-term post-operative complication rate was 6%.
Even in difficult conditions, THR can produce favorable results through careful planning, adaptation of techniques and targeted approaches to overcoming challenges.
Core Tip: Difficult total hip replacement is all the more of a challenge in a developing country, due to the difficulty of surgery, the lack of equipment and the limited availability of implants. However, adapting techniques could greatly improve functional results for patients long handicapped by underlying pathologies, in most cases evolving since childhood.
- Citation: Manasse H, Daoulas T, Rohimpitiavana AS, Solofomalala GD, Dubrana F, Razafimahandry HJC. Surgical techniques and outcomes of difficult total hip replacements: A challenge in a low-income country. World J Orthop 2025; 16(7): 105111
- URL: https://www.wjgnet.com/2218-5836/full/v16/i7/105111.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i7.105111
A difficult total hip replacement (THR ) is defined by several authors as a primary THR in patients with compromised bone or soft tissue conditions, including but not limited to: (1) Post-traumatic coxarthrosis; (2) Dysplastic hips; (3) Ankylosed hips; (4) Certain neuromuscular pathologies; and (5) Sequelae of childhood pathology such as hip epiphysiolysis or Legg-Calvé-Perthes disease[1,2]. These conditions are often aggravated by the development of secondary osteoarthritis, complicating the underlying primary pathologies[1]. Total hip arthroplasty is one of the most widely performed procedures in France, with over 149000 prostheses performed each year, coxarthrosis being the main indication[3]. It is considered one of the most successful surgical procedures in the field of orthopedics[4,5]. In contexts such as Madagascar, difficult THR cases are of particular importance, offering solutions to patients who previously had no alternative for treating their hip pathologies[2]. Since the introduction of new ranges of ancillaries and implants, as well as improved surgical techniques, the indications for these procedures have expanded beyond simple primary coxarthrosis, even outside humanitarian missions. The hypothesis of this study is that, despite the anatomical constraints and technical challenges associated with THR placement on these difficult hips, satisfactory clinical and functional results can be achieved if appropriate surgical techniques and rigorous implant selection are implemented.
The aim of this study was to describe the difficulties encountered during these procedures, to present the different techniques available to deal with them, and to evaluate the results obtained with these difficult THR.
This was a bi-centric, retrospective, observational study of patients undergoing THR on difficult hips. Revision THRs were excluded. The study population consisted of 50 patients operated on for THRs. All THR considered “difficult” were included in this study, including: (1) Post-traumatic coxarthrosis; (2) Dysplastic coxarthrosis; (3) Protrusive coxarthrosis; (4) Hip ankylosis; (5) Neglected hip dislocations; and (6) Sequelae of childhood diseases such as Legg-Calvé-Perthes disease, epiphysiolysis of the hip or juvenile idiopathic arthritis (Table 1).
| Patients | Frequency (n = 50) | Percentage (%) |
| Age (years) | ||
| Under 35 | 25 | 50 |
| 35-60 | 17 | 34 |
| Over 60 | 8 | 16 |
| Sex | ||
| Male | 26 | 52 |
| Female | 24 | 48 |
| Hip disease | ||
| Childhood disease sequelae | 16 | 32 |
| Post-traumatic coxarthrosis | 15 | 30 |
| Dysplastic coxarthrosis | 7 | 14 |
| Ankylosis of the hip | 7 | 14 |
| Neglected hip dislocations | 3 | 6 |
| Protrusive coxarthrosis | 2 | 4 |
All cases included in the study involved primary THRs performed on native joints. Primary THRs that did not present any particular surgical difficulties (such as primary osteoarthritis, recent femoral neck fractures, or osteonecrosis of the femoral head) were excluded from the study, as were revision THRs. The analyzed period corresponds to the early stages of THR procedures being performed in Madagascar, in a context where access to such interventions remains limited. The study population consisted of 50 patients who underwent a THR, representing 18.72% of the 276 THRs performed in the two centers under study between 2013 and 2023. Four patients were excluded due to missing data (Figure 1).
All cases included in the study corresponded to primary THR performed on native joints. Primary THRs without particular surgical difficulties (such as primary osteoarthritis, recent femoral neck fractures, or osteonecrosis of the femoral head) were excluded from the study, as well as revision THRs.
The analyzed period corresponds to the early phase of THR procedures in Madagascar, in a context where access to this type of surgery remains limited.
The study population consisted of 50 patients who underwent a THR, representing 18.72% of the 276 THRs performed in the two study centers between 2013 and 2023. Four patients were excluded due to missing data.
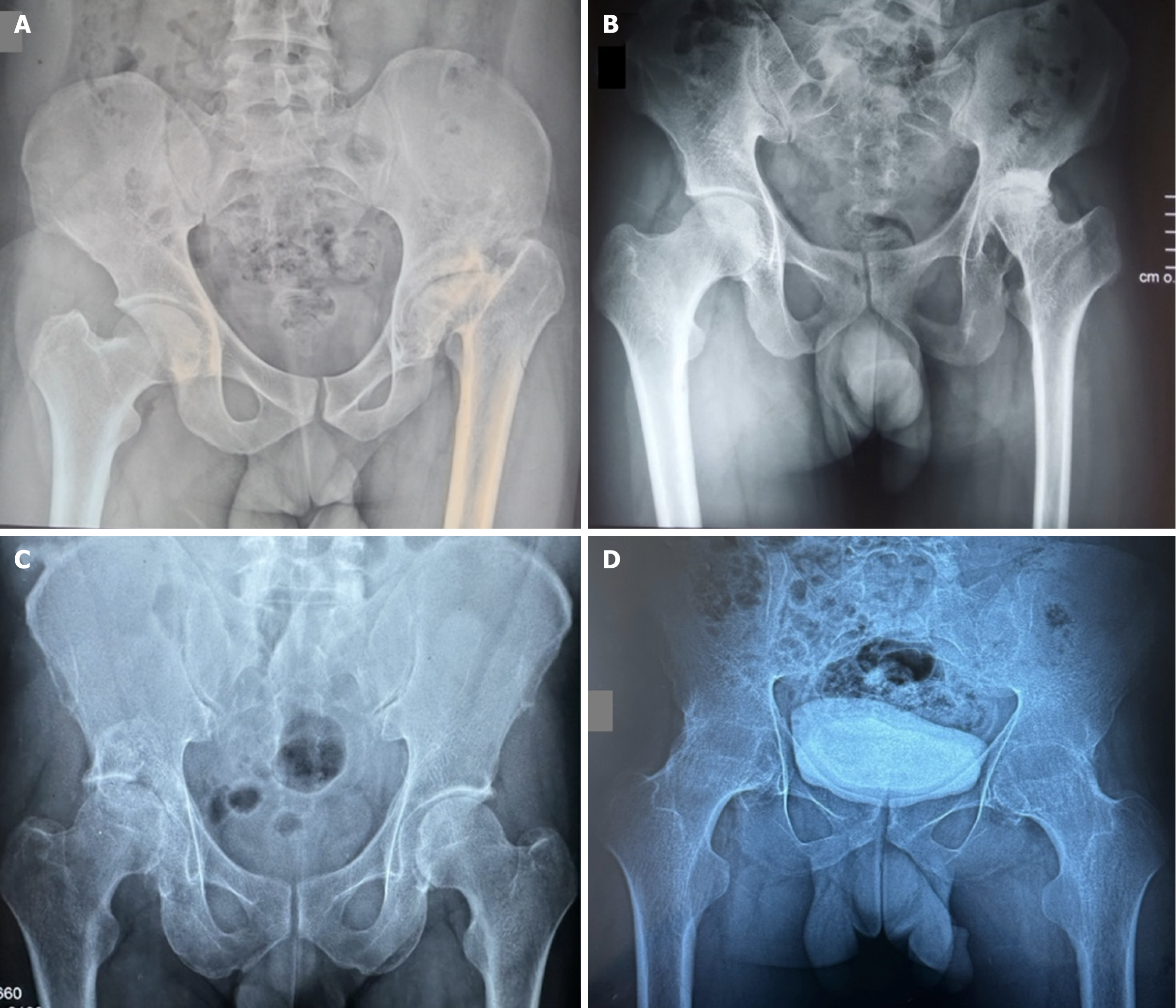
The study population included seven cases of hip osteoarthritis on dysplasia with insufficient acetabular coverage (4 cases of Crowe type III and 3 cases of Crowe type IV), and 15 cases of post-traumatic hip osteoarthritis (3 cases classified as Paprosky type I, 9 as Paprosky type II, and 5 as Paprosky type III).
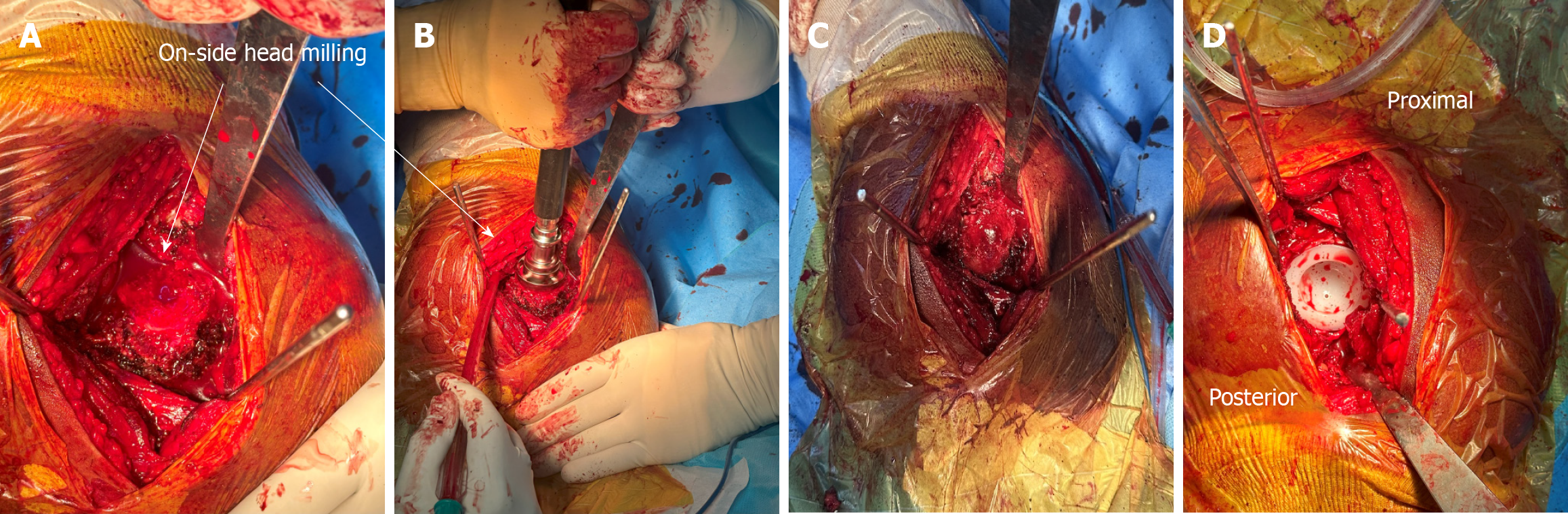
Surgery was performed by three senior surgeons, under general anesthesia (86%) or spinal anesthesia (14%). All patients underwent the Moore posterolateral approach[6]. The surgical techniques and choice of implants were adjusted according to the specific difficulties encountered during surgery (Table 2). In 7 (14%) cases of severe ankylosis preventing dislocation, prior osteotomy of the femoral neck was required (Figure 2). In 7 (14%) patients with dysplastic coxarthrosis and insufficient acetabular coverage, bone grafting of the acetabular roof was performed, synthesized with osteosynthesis screws.
| Technical difficulties | Surgical techniques to overcome difficulties | Number of patients (n = 50) | Percentage (%) |
| Malunion acetabular bone defect | Acetabular autologous bone graft from the femoral head | 5 | 10 |
| Difficulty removing material | Careful, gradual material removal: Use of adapted materials. Cementing implants | 6 | 12 |
| Insufficient acetabular coverage, shallow and porous neoacetabulum or paleoacetabulum, difficulty identifying the true acetabular cavity | Shelf operation and/or bone grafting ± fixation with screws. Progressive reaming until achieving a sufficiently deep acetabular cavity | 7 | 14 |
| Difficult or impossible hip dislocation | Initial osteotomy followed by dislocation and fragmentary removal of the femoral head ± creation of a new acetabulum if difficulty arises during the removal of the head from the acetabulum | 9 | 18 |
| Cavitary defect in the acetabular floor, fusion of the femoral head and acetabulum | Impaction of autogenous bone graft from the femoral head and cemented cup ± use of support rings or anti-protrusion cages if available | 4 | 8 |
| Proximal femoral ascent: Limb length discrepancy Narrow femoral canal | Careful and progressive hip dislocation. Small, long-stem prosthesis | 12 | 24 |
| Soft tissue contracture | Careful and progressive hip dissection | 25 | 50 |
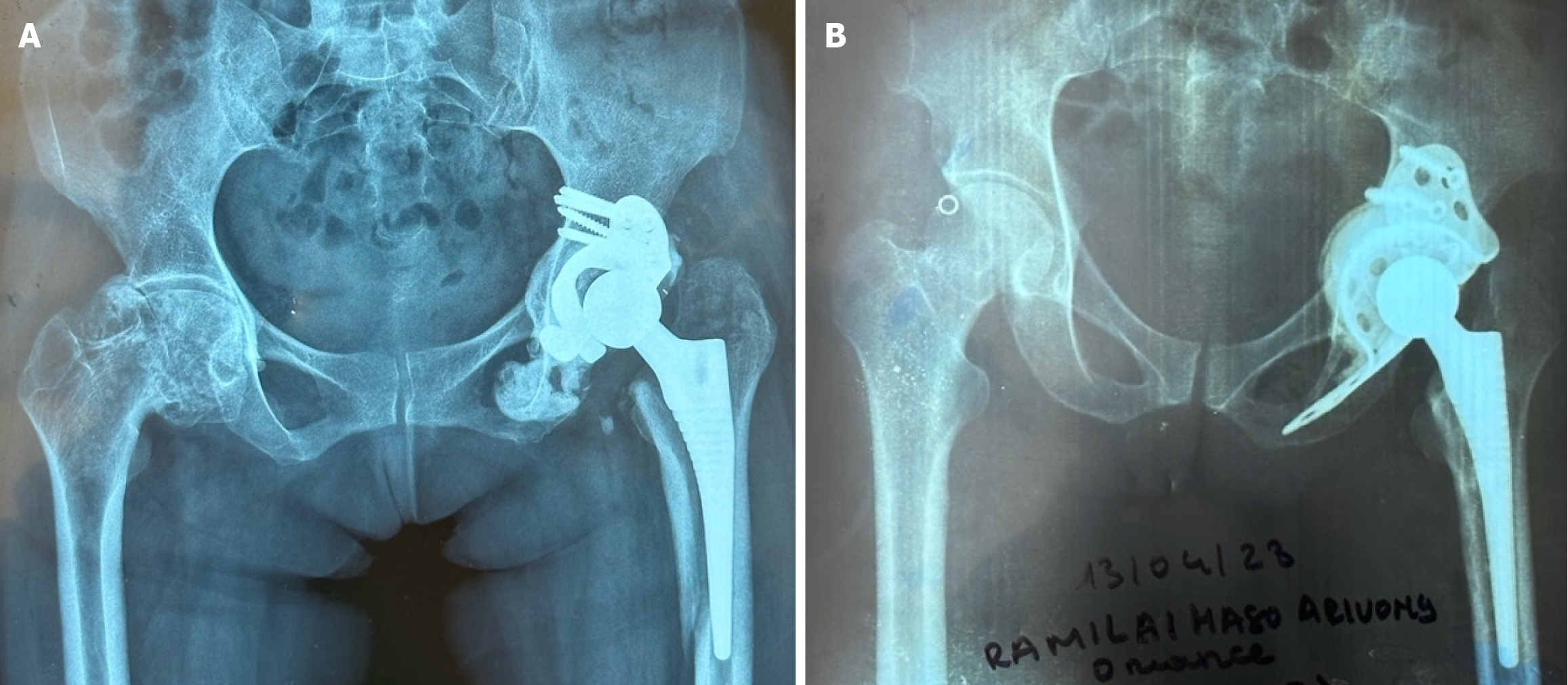
The choice of implants was determined by several factors, including material availability, hip type and the surgeon's final decision, as presented in Table 3. Four patients (8%) required acetabular reinforcement for improved stability.
| Number of patients (n = 50) | Frequency (%) | |
| Year of surgery | ||
| 2013-2018 | 19 | 38 |
| 2019-2023 | 31 | 62 |
| Implant type | ||
| Dual-mobility | 7 | 14 |
| Conventional | 43 | 86 |
| Fixation methods | ||
| Cemented | 44 | 88 |
| Uncemented | 1 | 2 |
| Reverse hybrid | 5 | 10 |
| Bearing couples | ||
| Metal-polyethylene | 29 | 58 |
| Ceramic-polyethylene | 21 | 42 |
| Support ring/anti-protrusion cage | 4 | 8 |
Two types of devices were used: (1) Kerboull-type support ring; and (2) Burch-Schneider anti-protrusion cage (Figure 3).
These devices were chosen according to the degree of acetabular deficiency.
The statistics for this study were produced jointly with the local bio-statistics committee. Cases were analyzed by a single, non-operator observer, based on medical records and follow-up telephone calls. The data collected were analyzed using Statistical Package for the Social Sciences 26.0 software (IBM France 17 avenue de l'Europe 92275 Bois-Colombes Cedex). We conducted a descriptive analysis of our results. Quantitative variables were presented as means with their standard deviation, as well as their extremes (minimum and maximum). Qualitative variables were presented as proportions and percentages. Quantitative data were compared using Student's t-test. The primary endpoint was quantification of the Postel Merle d'Aubigné (PMA) functional score preoperatively and postoperatively[7].
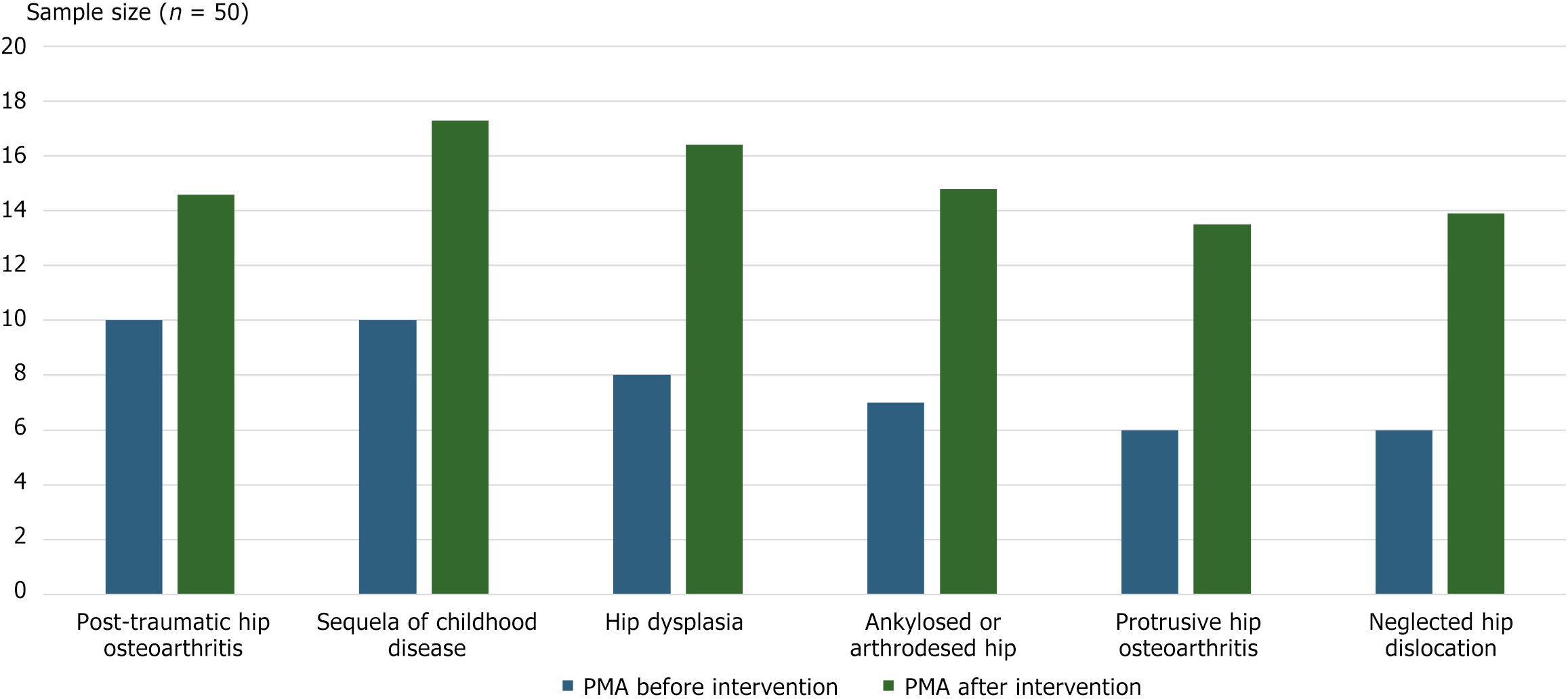
The mean follow-up was 7.5 years (1.5-10 years). There was a significant improvement in functional score after surgery, with a mean PMA score before surgery 8.36 ± 0.85 and after surgery 16.14 ± 1.26 (P < 0.005, 95%CI: 95%). All patients achieved scores classified as good or excellent (Figure 4). The mean duration of intervention was 177 minutes ± 62.14 minutes or 2.95 hours (90-290 hours).
The longest procedure involved a THR after failure of screw fixation of the femoral neck, requiring removal of the osteosynthesis material and placement of the THR in one stage. Mean intraoperative blood loss was 568 mL ± 71.46 mL (200-900 mL).
Intraoperative complications: One patient (2%) presented an intraoperative complication, with a fracture of the greater trochanter during THR for sequelae of epiphysiolysis. The fracture was treated with a three-month weight-bearing ban. Radiographic consolidation was achieved at six months.
Postoperative complications: Three patients (6%) presented postoperative medical-surgical complications: (1) One femoral shaft fracture on Vancouver B2 prosthesis at J11 post-op, treated with cerclage osteosynthesis. Radiographic consolidation was achieved at six months[8]; (2) Femoral stem loosening five years after initial prosthesis insertion for dysplastic coxarthrosis, necessitating stem revision; and (3) Pulmonary embolism in a 77-year-old hypertensive patient, operated on for dysplastic coxarthrosis, treated with curative anticoagulants, without complications after initiation of anticoagulants.
THR is an effective treatment option for many hip pathologies, even in the most complex cases. It offers a treatment option in situations such as post-traumatic osteoarthritis following a neglected acetabular fracture, or failed osteosynthesis of a hip fracture. THR is also indicated in the management of degenerative osteoarthritis, such as in cases of dysplasia or sequelae of Legg-Calvé-Perthes disease[9,10]. The prevalence of difficult THR varies between studies. Vidyarthi et al[11] reported a prevalence of complex THR of 42% over a four-year period. Anyaehie et al[2] observed 43.4% of difficult THRs in their series. Dilogo et al[12] observed 35.8% of difficult THRs in their series. In our series, the rate of complex THR remains relatively moderate, as these procedures were initially performed mainly during humanitarian missions, where conditions are optimized by the provision of specialized equipment. Local surgeons began to perform these complex procedures alongside experienced mission surgeons. After several years of gradual learning and collaboration, local surgeons have acquired the skills needed to perform these difficult THRs independently, even outside humanitarian missions. However, the intra-operative and post-operative management of these difficult THRs requires a long learning curve, and these procedures are not yet performed routinely throughout the year. The recent arrival of new ranges of implants and instruments, thanks to collaboration with new suppliers, has also enabled indications to be extended to more complex pathologies.
As the majority of patients operated on in low-income countries are younger, single mobility implants have often been preferred. However, an increasing number of series are demonstrating that dual mobility implants can also be used in younger populations[13]. The use of dual mobility implants could be considered more and more frequently in the future, even for young patients, in order to limit the risk of prosthetic dislocation and de facto emergency treatment in sometimes precarious conditions.
However, only seven patients were able to benefit, as these implants are not yet available in Madagascar, or only on order, two of them having been fitted during humanitarian missions.
The difficulties encountered during surgery were comparable to those described in the literature[14,15]. For acetabular bone defects, autogenous grafting by direct impaction of the femoral head has been used, followed by careful milling and placement of a cemented implant. This technique is well documented and suitable for cavitary defects behind the cup, and is enhanced by the addition of cancellous or impaction grafts[11,12]. Although it requires considerable experience, it is highly appropriate in this context for regaining the hip's center of rotation. For acetabular protrusions, several authors recommend the use of support rings or anti-protrusion cages[16], an approach adopted for four patients in our series.
In cases of neglected hip dislocation, the reduction of the prosthetic joint is often challenging due to soft tissue contractures and the risk of nerve injuries. To facilitate this reduction, Talwar et al[17] recommend a femoral shortening osteotomy combined with the use of a long, modular, uncemented stem and an acetabular cup. However, this technique is complex, and it is essential to identify the original acetabulum. If the cup is placed in the pseudo-acetabulum, there is an increased risk of dislocation, persistent limp, and implant loosening[18]. In our series, as the original acetabulum was intact, dislocation was not required. A femoral neck osteotomy was performed, followed by the progressive removal of femoral head fragments and reaming of the acetabulum. This technique has also been described by Viamont-Guerra et al[19] in cases of ankylosis.
In cases of dysplasia, a bone deficit in the superolateral part of the acetabulum is often observed, leaving part of the cup uncovered. Coverage of at least 70% by native bone is necessary to ensure optimal stability. When this bone deficit is significant, various alternatives have been proposed, including acetabular augmentation with cement or autograft, porous metal augments, or the use of a support ring[20,21]. In 14% of the cases in our series, this technique was used, primarily during humanitarian missions, where it facilitated knowledge transfer that was beneficial for the success of the procedures.
Early management of pediatric diseases through conservative surgeries could help limit these difficulties, although a THR is often necessary in the long term[22]. according to De Salvo et al[23], in pediatric conditions requiring a THR, deformities of the proximal femur and the narrowness of the diaphyseal canal can prevent the use of standard stems, sometimes requiring custom-made implants. However, these custom stems have drawbacks, such as prolonged manufacturing times and high costs, which can pose problems when the available options are not suitable during the procedure[24,25].
Finally, the hard-on-hard bearing couple is another potential option for these populations[26], although this solution has limitations in our series. However, several patients with sequelae from childhood diseases or epiphysiolysis were able to benefit from THR with available implants, and short-term and medium-term results were satisfactory. However, long-term outcomes remain uncertain, particularly due to the high functional demands of these patients.
Despite the surgical challenges, greater blood loss, and prolonged procedures, a significant improvement in the PMA score was observed in all patients, both post-operatively and in the long term. While several studies have already shown these results, particularly in post-traumatic coxarthrosis[25,27], patients with sequelae from childhood diseases achieved better functional outcomes, likely because only the proximal femur, and not the acetabulum, was affected. Additionally, these younger patients benefited from shorter procedures and faster recovery, contributing to better results[28].
Contrary to literature claims that challenging THRs are associated with a higher complication rate[2], our series did not show significantly more peri-operative or post-operative complications compared to standard THRs. The complication rate was optimized through careful anticipation of medical complications, as well as rigorous selection of patients capable of understanding and adhering to postoperative instructions, particularly regarding dislocating movements and rehabilitation. The relatively low complication rate can also be explained by the young average age of the patients, who presented with few comorbidities.
However, total hip arthroplasty in patients with pediatric pathologies is still associated with a higher risk of complications, such as periprosthetic fractures, nerve palsies, infections, and heterotopic ossification[23]. In our series, a case of greater trochanter fracture on epiphysiolysis was treated with per-operative cerclage, a complication similar to that described by Kenanidis et al[24].
A case of aseptic loosening of the femoral stem was observed in a 29-year-old patient with dysplastic coxarthrosis. Aseptic loosening is the most common cause of THR revision in patients operated on before the age of 30 years[29], with an incidence comparable to that reported by Di Martino et al[30]. This complication can be explained by the incongruence between the proximal and distal femoral canal diameters, posing a major problem for stem fixation in cases of dysplasia, where the femoral canal is often narrow[31].
The management of these difficult THRs is challenging both surgically and anesthetically. The main issues are bleeding, especially for rare blood types, and the long duration of the procedures, increasing the risk of infection. Pain management is complicated by the absence of nerve blocks, due to the high cost of needles and the lack of ultrasound equipment. Finally, general anesthesia is often necessary for these complex procedures, even though the patients are typically young and without major comorbidities.
| 1. | Boisgard S, Descamps S, Bouillet B. Complex primary total hip arthroplasty. Orthop Traumatol Surg Res. 2013;99:S34-S42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Anyaehie UE, Eyichukwu GO, Nwadinigwe CU, Katchy AU. Complex primary hips for total hip replacement surgery at a tertiary institution in Nigeria. SICOT J. 2018;4:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Erivan R, Villatte G, Dartus J, Reina N, Descamps S, Boisgard S. Progression and projection for hip surgery in France, 2008-2070: Epidemiologic study with trend and projection analysis. Orthop Traumatol Surg Res. 2019;105:1227-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 69] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 4. | Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1477] [Cited by in RCA: 1790] [Article Influence: 99.4] [Reference Citation Analysis (0)] |
| 5. | Bostian PA, Grisez BT, Klein AE, Frye BM. Complex Primary Total Hip Arthroplasty: Small Stems for Big Challenges. Arthroplast Today. 2021;8:150-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Dubrana F, Le Nen D, Gunepin F-X, Lefèvre C. Manuel des voies d’abord en Chirurgie Orthopédique et Traumatologique. 2nd. Netherlands: Elsevier, 2014. |
| 7. | Biau DJ, Brand RA. Robert Merle d'Aubigné, 1900-1989. Clin Orthop Relat Res. 2009;467:2-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293-304. [PubMed] |
| 9. | Marcinko M, Sadhwani S, Dahl R, Ali M. The Practicality of the Robotic Total Hip Arthroplasty for the Treatment of Complex Bilateral Adult Hip Dysplasia. Technology Makes It Easy. Arthroplast Today. 2023;24:101249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Biant LC, Bruce WJ, Assini JB, Walker PM, Walsh WR. Primary total hip arthroplasty in severe developmental dysplasia of the hip. Ten-year results using a cementless modular stem. J Arthroplasty. 2009;24:27-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Vidyarthi AR, Barman R, Kisku L, Akhtar MN, Keshkar S. Total Hip Arthroplasty for Complex Primary Hips – A Tertiary Center Experience. J Orthop Trauma Reha. 2021;13:117-121. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Dilogo IH, Fahrudhin MT, Canintika AF. How is the outcome of primary difficult total hip arthroplasty? A cross-sectional study. Int J Surg Open. 2019;21:68-72. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Viricel C, Boyer B, Philippot R, Farizon F, Neri T. Survie et complications des prothèses totales de hanche à double mobilité de troisième génération avec du polyéthylène non réticulé chez des patients de moins de 55 ansSurvival and complications of total hip arthroplasty using third-generation dual-mobility cups with non-cross-linked polyethylene liners in patients younger than 55 years. RCOT. 2022;108:161-168. [DOI] [Full Text] |
| 14. | Wu H, Cheng WD, Jing J. Total hip arthroplasty by direct anterior approach in the lateral position for the treatment of ankylosed hips. Eur J Orthop Surg Traumatol. 2020;30:993-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Jewett BA, Collis DK. High complication rate with anterior total hip arthroplasties on a fracture table. Clin Orthop Relat Res. 2011;469:503-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 216] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 16. | Shi XT, Li CF, Cheng CM, Feng CY, Li SX, Liu JG. Preoperative Planning for Total Hip Arthroplasty for Neglected Developmental Dysplasia of the Hip. Orthop Surg. 2019;11:348-355. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | Talwar J, Agarwal S, Agarwal S, Krishna LG, Rustagi A. Step-Cut Subtrochanteric Osteotomy Combined with Total Hip Arthroplasty for Neglected Traumatic Hip Dislocations. Clin Orthop Surg. 2022;14:205-212. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 18. | Bicanic G, Barbaric K, Bohacek I, Aljinovic A, Delimar D. Current concept in dysplastic hip arthroplasty: Techniques for acetabular and femoral reconstruction. World J Orthop. 2014;5:412-424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 43] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 19. | Viamont-Guerra MR, Chen AF, Stirling P, Nover L, Guimarães RP, Laude F. The Direct Anterior Approach for Total Hip Arthroplasty for Severe Dysplasia (Crowe III and IV) Provides Satisfactory Medium to Long-Term Outcomes. J Arthroplasty. 2020;35:1642-1650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Wang Y. Current concepts in developmental dysplasia of the hip and Total hip arthroplasty. Arthroplasty. 2019;1:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Iwase T, Morita D, Ito T, Takemoto G, Makida K. Favorable Results of Primary Total Hip Arthroplasty With Acetabular Impaction Bone Grafting for Large Segmental Bone Defects in Dysplastic Hips. J Arthroplasty. 2016;31:2221-2226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Migaud H, Putman S, Berton C, Lefèvre C, Huten D, Argenson JN, Gaucher F. Does prior conservative surgery affect survivorship and functional outcome in total hip arthroplasty for congenital dislocation of the hip? A case-control study in 159 hips. Orthop Traumatol Surg Res. 2014;100:733-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | De Salvo S, Sacco R, Mainard N, Lucenti L, Sapienza M, Dimeglio A, Andreacchio A, Canavese F. Total hip arthroplasty in patients with common pediatric hip orthopedic pathology. J Child Orthop. 2024;18:134-152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 24. | Kenanidis E, Kakoulidis P, Panagiotidou S, Leonidou A, Lepetsos P, Topalis C, Anagnostis P, Potoupnis M, Tsiridis E. Total hip arthroplasty in patients with slipped capital femoral epiphysis: a systematic analysis of 915 cases. Orthop Rev. 12:8549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 25. | Scott CEH, MacDonald D, Moran M, White TO, Patton JT, Keating JF. Cemented total hip arthroplasty following acetabular fracture. Bone Joint J. 2017;99-B:1399-1408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 26. | Girard J, Bocquet D, Fron D, Herbaux B, Migaud H. [Revision of total hip arthroplasty in patients younger than 30 years old]. Rev Chir Orthop Reparatrice Appar Mot. 2008;94 Suppl:S188-S191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Krause PC, Braud JL, Whatley JM. Total hip arthroplasty after previous fracture surgery. Orthop Clin North Am. 2015;46:193-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Lehmann TG, Engesaeter IØ, Laborie LB, Lie SA, Rosendahl K, Engesaeter LB. Total hip arthroplasty in young adults, with focus on Perthes' disease and slipped capital femoral epiphysis: follow-up of 540 subjects reported to the Norwegian Arthroplasty Register during 1987-2007. Acta Orthop. 2012;83:159-164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 29. | Mainard D. La prothèse totale de hanche chez les sujets très jeunes. Revue du Rhumatisme Monographies. 2020;87:83-87. [DOI] [Full Text] |
| 30. | Di Martino A, Castagnini F, Stefanini N, Bordini B, Geraci G, Pilla F, Traina F, Faldini C. Survival rates and reasons for revision of different stem designs in total hip arthroplasty for developmental dysplasia: a regional registry study. J Orthop Traumatol. 2021;22:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 31. | Liu T, Wang S, Huang G, Wang W. Treatment of Crowe IV developmental dysplasia of the hip with cementless total hip arthroplasty and shortening subtrochanteric osteotomy. J Int Med Res. 2019;47:3223-3233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |