Published online May 18, 2025. doi: 10.5312/wjo.v16.i5.105734
Revised: March 26, 2025
Accepted: April 11, 2025
Published online: May 18, 2025
Processing time: 100 Days and 9.4 Hours
Supracondylar humeral fractures (SCHF) are the second most common fractures in childhood and can lead to short- and long-term complications. Despite their prevalence, the anatomical factors that predispose children to SCHF remain unclear. This study aimed to determine whether there are significant morphological differences in the elbow by comparing the radiographic angular measure
To determine radiological parameters that may predispose to pediatric elbow fractures.
Radiographs of 78 SCHF patients were analyzed for angular measurements of the contralateral elbow. Two control groups were used: 98 healthy children and 40 patients with DRF. Angular measurements included Baumann angle (BA), hu
Significant differences were found in elbow measurements between SCHF and control groups (P < 0.05). However, the mean values for all groups fell within the ranges described in the literature.
While statistically significant differences were found in elbow morphology between SCHF patients and controls, these differences don't translate into clinically meaningful morphological deviations.
Core Tip: We believe that our study makes a significant contribution to the literature because it provides a detailed com
- Citation: Ülgen NK, Gencer B, Doğan Ö. Comparative analysis of elbow radiographic measurements in patients with supracondylar humerus fractures and healthy controls. World J Orthop 2025; 16(5): 105734
- URL: https://www.wjgnet.com/2218-5836/full/v16/i5/105734.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i5.105734
In children, elbow fractures are the second most common after forearm fractures, with supracondylar humerus fractures (SCHF) being particularly prevalent due to the relative weakness of the distal humerus metaphysis[1]. These fractures frequently require surgical intervention[2] due to the complex anatomy of the elbow and the associated risk of neu
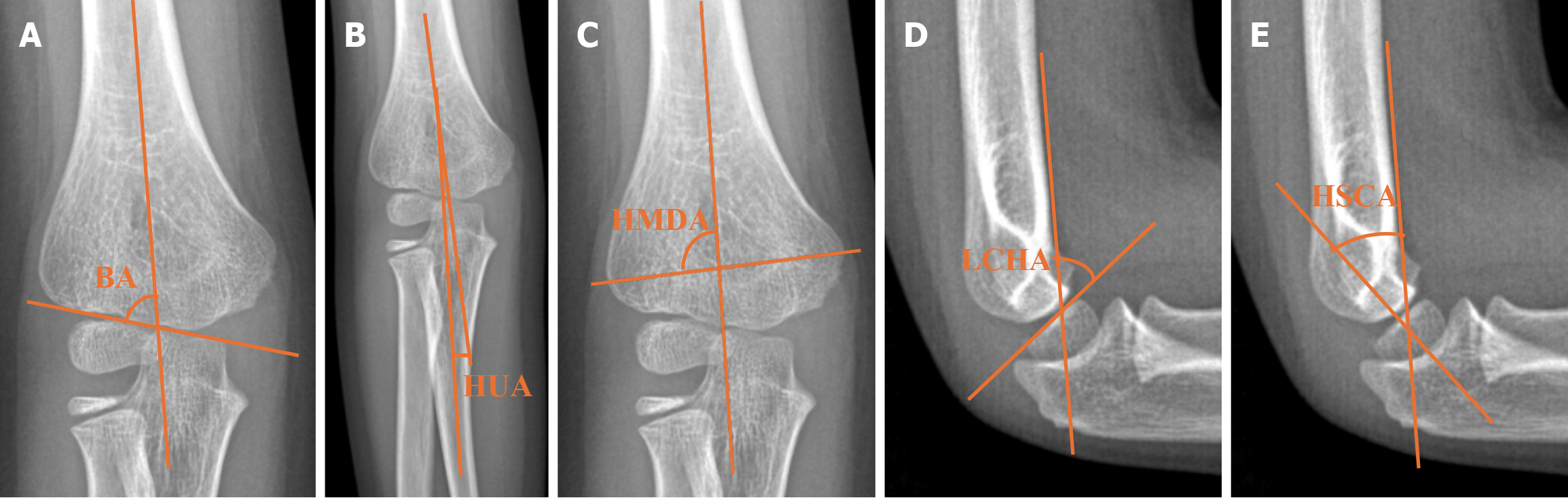
Radiographic angular measurements play a key role in evaluating and managing elbow fractures. In pediatric patients, epiphyseal lines and the long axes of the surrounding bones are critical references for these measurements. Commonly used angular measurements on anteroposterior (AP) elbow radiographs include Baumann's angle (BA), the humeroulnar angle (HUA), and the humeral metaphysis-diaphysis angle (HMDA), while lateral views allow for the assessment of the lateral capitellohumeral angle (LCHA) and the humeral shaft-condylar angle (HSCA)[3-7].
In this study, we aimed to compare the radiographic angular measurements of the intact contralateral elbows of patients with SCHF with those of a healthy population to investigate the presence of any morphological differences that might predispose patients to fractures. The goal is to identify any morphological differences in elbow structure that might predispose children to SCHF. Furthermore, we compared children with sustained distal radius fractures (DRF), the most common fractures in childhood, to explore morphological differences that might lead to different fracture locations. Because appropriate AP elbow radiographs were available for patients with DRF but appropriate lateral elbow ra
Ethical approval for this study was obtained from the local ethics committee, and all patients provided informed consent prior to participation. This study adhered to the STROBE guidelines for reporting observational research. A total of 88 patients with supracondylar humeral fractures treated between June 2019 and December 2022 were included. Patients with multiple or pathological fractures were excluded. Patient demographic data, clinical notes, and radiologic images were retrospectively reviewed using the hospital's automation system and clinical archives. Radiographs were taken in the X-ray room by an experienced technician using standard techniques. True AP and lateral views were included in the study. Radiographic measurements were conducted digitally using the hospital’s picture archiving and communication system.
Angular measurements were performed on the intact contralateral elbows of patients with SCHF. A total of 78 contralateral elbows were suitable for measurement, and the consistency of right and left elbow measurements allowed for the use of the contralateral side as a reference[8]. Two control groups were included: 40 patients with DRF and 98 healthy children without prior fractures or bone pathology. The healthy control group was matched by age to the SCHF group. Due to limitations in lateral imaging of the DRF group, only AP radiographic measurements were available for comparison between the SCHF and DRF groups. Lateral radiographic measurements were compared only between the SCHF and healthy control groups.
Radiographic measurements included BA, the HUA, and the HMDA on AP radiographs. Lateral measurements included the LCHA and the HSCA. BA was defined as the angle between the physeal line of the lateral condyle and the long axis of the humeral diaphysis on AP radiographs, with normal values ranging from 64° to 81°[9]. HUA was mea
Radiographic measurements were independently performed by two observers. To ensure reliability, the measurements were blinded and repeated after a minimum interval of one month. The average values were used for statistical analysis.
Descriptive statistics were calculated using the median, interquartile range, and minimum and maximum values for continuous data, while categorical data were presented as frequencies and percentages. The Kolmogorov-Smirnov test was used to assess the normality of continuous data. For normally distributed data, the Independent Sample t-test was used for comparing two groups, and one-way analysis of variance was used for comparisons among three groups. For non-normally distributed data, the Mann-Whitney U Test was used for paired group comparisons, and the Kruskal-Wallis test was used for comparisons among three groups. Statistical significance was set at a P value of < 0.05. All statistical analyses were performed using IBM® SPSS® version 26.0.0.0.
Radiological analysis revealed statistically significant differences in several angular measurements among the three study groups. BA differed significantly between the groups, with a P-value of 0.012, indicating variation in angular morphology among patients with SCHF, DRF, and healthy controls. Similarly, the HUA demonstrated a statistically significant difference across the three groups (P < 0.001), as did the HMDA (P = 0.005). Detailed data for these measurements are presented in Tables 1 and 2, which outline the mean values and statistical tests applied.
| SCHF (n = 78 hasta) | DRF (n = 40) | Healthy volunteers (n = 98) | P value | |
| Bauman angle | 74.33 ± 4.69 | 75.14 ± 3.39 | 76.16 ± 3.73 | 0.012 |
| Humeroulnar angle | 11.26 ± 4.31 | 9.51 ± 2.99 | 8.52 ± 3.47 | < 0.001 |
| Humerus metaphysis-diaphysis angle1 | 87.2 ± 3.56) | 87.68 ± 2.92 | 88 ± 2.02 | 0.0051 |
| Humerus shaft-condylar angle | 35.5 ± 8.97 | NA2 | 36.67 ± 6.39 | 0.3373 |
| Lateral capitellohumeral angle | 49.77 ± 10.29 | NA2 | 50.15 ± 9.99 | 0.8063 |
| SCHF | DRF | Healthy volunteers | ||
| Bauman angle | SCHF | NA | 0.586 | 0.013 |
| DRF | 0.586 | NA | 0.409 | |
| Healthy volunteers | 0.013 | 0.586 | NA | |
| Humeroulnar angle | SCHF | NA | 0.055 | < 0.001 |
| DRF | 0.055 | NA | 0.367 | |
| Healthy volunteers | < 0.001 | 0.367 | NA | |
| Humerus metaphysis-diaphysis angle | SCHF | NA | 0.160 | 0.001 |
| DRF | 0.160 | NA | 0.187 | |
| Healthy volunteers | 0.001 | 0.187 | NA |
When comparing the contralateral elbows of patients with SCHF to those of the healthy population group, no significant differences were observed in the HSCA or LCHA (P = 0.337 and P = 0.806, respectively). This finding suggests that, despite significant differences in AP view measurements (BA, HUA, and HMDA), lateral view measurements remain consistent between these groups. These results are summarized in Tables 1 and 2.
The primary aim of our study was to determine whether the contralateral elbow angular measurements of patients with SCHF differed from those of the normal population. The relationship between bone morphology and fractures has been previously studied in elderly hip fractures[11-15]. A few studies have examined the relationship between tibial anatomy and tibial stress fractures[16,17]. The number of studies examining the relationship between bone morphology and fractures, other than hip fractures, is limited and, to the best of our knowledge, no study examining the relationship between bone morphology and fractures in pediatric patients exists. Therefore, we aimed to conduct such a study on SCHFX, the second most common fracture in childhood, for pediatric fractures.
We believe that our study makes a significant contribution to the literature because it provides a detailed comparative analysis of elbow radiographic measurements, adding new insights into the anatomical features of pediatric elbows associated with SCHF. While previous research has explored the mechanics of these fractures, our study uniquely focuses on whether variations in elbow morphology contribute to fracture predisposition. This comparison has not been extensively studied in pediatric populations, making our research novel and valuable for understanding fracture risk factors in children.
Radiographic elbow angular measurements of patients with DRF, which occurs through a mechanism similar to that of SCHF, were performed. Patients with DRFs were selected because, although not entirely the same, they occur through a similar mechanism of falling, and elbow radiographs are available owing to their proximity. Additionally, the peak incidence ages of supracondylar humerus and DRF differed. We investigated whether this difference was related to the elbow morphology. However, the lateral radiographs of the elbows in the DRF group did not meet the standards; therefore, the HSCA and LCHA could not be evaluated. Because the radiographs were taken for the forearm, only 40 patients had elbow AP views that met the standards. Consequently, the sample size of the distal radial fracture group was limited.
In comparing radiographic elbow measurements among the three groups, significant differences were observed in BA
Even if a morphological difference that would create a tendency for fracture is detected in larger series studies, it would not be logical to take a screening elbow film of children. The role of artificial intelligence in interpreting medical images is increasing day by day, and such systems that can evaluate a large number of images simultaneously have already been introduced[18]. Furthermore, artificial intelligence programs designed to recognize pediatric elbow fractures have been reported[19,20]. By evaluating the angular parameters evaluated in our study with a high number of images by artificial intelligence-supported programs, a real morphological difference can be quickly detected[21]. In this way, an artificial intelligence-supported program can analyze a child’s elbow X-ray taken for an unrelated reason, determine the tendency for fracture, and inform both the child and their family, allowing protective and preventative measures to be taken. Similar methods can be applied to fractures in other regions with future studies.
The relationship between SCHF and DRF is also of interest, as both fractures result from similar mechanisms, typically falls onto an outstretched arm. However, lateral radiographs of the elbows in the DRF group were insufficient for accurate measurement of the HSCA and LCHA, limiting our ability to draw robust comparisons. The small sample size of the DRF group further constrained the study's power.
Our study has several limitations. First, the wide normative ranges for elbow angles make it difficult to assess the clinical significance of the detected differences. Second, the sample size, particularly for patients with DRF, was relatively small, limiting the robustness of our comparisons. Additionally, the absence of lateral radiographs for many DRF patients restricted our ability to evaluate HSCA and LCHA in this group. Future studies should aim to stratify patients by age group and ensure complete imaging data for more precise angular comparisons.
This study demonstrated statistically significant differences in the elbow radiographic measurements of patients with SCHF compared to other groups. However, despite these statistical differences, the average angular measurements in all groups remained within the normative ranges described in the literature. While the detection of statistically significant differences is noteworthy, the clinical relevance of these findings remains unclear. Therefore, no substantial morphological differences between the elbows of patients with SCHF and those of the normal population could be concluded. It was important to detect statistically significant differences between groups. Future studies should focus on refining angular measurements by narrowing the range according to specific age groups, as this may reveal more meaningful morphological differences. Additionally, expanding the sample size and exploring other factors that may influence elbow morphology could provide further insights into the predisposition to SCHF and improve diagnostic approaches.
| 1. | Farnsworth CL, Silva PD, Mubarak SJ. Etiology of supracondylar humerus fractures. J Pediatr Orthop. 1998;18:38-42. [PubMed] |
| 2. | Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am. 2008;90:1121-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 312] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 3. | Skaggs DL, Flynn JM. Supracondylar fractures of the distal humerus. In: Kasser JR, Beaty JH, editors. Rockwood and Wilkins’ fractures in children. Philadelphia: Lipincott Williams and Wilkins, 2010, 487–532. |
| 4. | Suangyanon P, Chalayon O, Worawuthangkul K, Kaewpornsawan K, Ariyawatkul T, Eamsobhana P. Pediatric elbow measurement parameters: Evaluation of the six angles in inter- and intra-observer reliability. J Clin Orthop Trauma. 2019;10:792-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Shank CF, Wiater BP, Pace JL, Jinguji TM, Schmale GA, Bittner RC, Bompadre V, Stults JK, Krengel WF 3rd. The lateral capitellohumeral angle in normal children: mean, variation, and reliability in comparison to Baumann's angle. J Pediatr Orthop. 2011;31:266-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Simanovsky N, Lamdan R, Hiller N, Simanovsky N. The measurements and standardization of humerocondylar angle in children. J Pediatr Orthop. 2008;28:463-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Turhan E, Aksoy C, Ege A, Bayar A, Keser S, Alpaslan M. Sagittal plane analysis of the open and closed methods in children with displaced supracondylar fractures of the humerus (a radiological study). Arch Orthop Trauma Surg. 2008;128:739-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Miyazaki CS, Maranho DA, Agnollitto PM, Nogueira-Barbosa MH. Study of Secondary Ossification Centers of the Elbow in the Brazilian Population. Acta Ortop Bras. 2017;25:279-282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Silva M, Pandarinath R, Farng E, Park S, Caneda C, Fong YJ, Penman A. Inter- and intra-observer reliability of the Baumann angle of the humerus in children with supracondylar humeral fractures. Int Orthop. 2010;34:553-557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Sukvanich P, Samun P, Kongmalai P. Diagnostic accuracy of the shaft-condylar angle for an incomplete supracondylar fracture of elbow in children. Eur J Orthop Surg Traumatol. 2019;29:1673-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Tokyay A, Güven M, Encan ME, Okay E, Akbaba O. The influence of acetabular morphology on prediction of proximal femur fractures types in an elderly population. Hip Int. 2017;27:489-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Zhuang H, Li Y, Lin J, Cai D, Cai S, Yan L, Yao X. Cortical thickness in the intertrochanteric region may be relevant to hip fracture type. BMC Musculoskelet Disord. 2017;18:305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Zhu DC, Lu SQ, Ge B, Lei SF. Newly developed hip geometry parameters are associated with hip fracture. J Orthop Sci. 2021;26:616-621. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Vlachos C, Ampadiotaki MM, Papagrigorakis E, Galanis A, Zachariou D, Vavourakis M, Rodis G, Vasiliadis E, Kontogeorgakos VA, Pneumaticos S, Vlamis J. Distinctive Geometrical Traits of Proximal Femur Fractures-Original Article and Review of Literature. Medicina (Kaunas). 2023;59:2131. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Hu ZS, Liu XL, Zhang YZ. Comparison of Proximal Femoral Geometry and Risk Factors between Femoral Neck Fractures and Femoral Intertrochanteric Fractures in an Elderly Chinese Population. Chin Med J (Engl). 2018;131:2524-2530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Koltun KJ, Sekel NM, Bird MB, Lovalekar M, Mi Q, Martin BJ, Nindl BC. Tibial Bone Geometry Is Associated With Bone Stress Injury During Military Training in Men and Women. Front Physiol. 2022;13:803219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Tommasini SM, Nasser P, Schaffler MB, Jepsen KJ. Relationship between bone morphology and bone quality in male tibias: implications for stress fracture risk. J Bone Miner Res. 2005;20:1372-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 101] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 18. | Zech JR, Jaramillo D, Altosaar J, Popkin CA, Wong TT. Artificial intelligence to identify fractures on pediatric and young adult upper extremity radiographs. Pediatr Radiol. 2023;53:2386-2397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Kekatpure A, Kekatpure A, Deshpande S, Srivastava S. Development of a diagnostic support system for distal humerus fracture using artificial intelligence. Int Orthop. 2024;48:1303-1311. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Binh LN, Nhu NT, Nhi PTU, Son DLH, Bach N, Huy HQ, Le NQK, Kang JH. Impact of deep learning on pediatric elbow fracture detection: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2025;51:115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 21. | Patton D, Ghosh A, Farkas A, Sotardi S, Francavilla M, Venkatakrishna S, Bose S, Ouyang M, Huang H, Davidson R, Sze R, Nguyen J. Automating Angle Measurements on Foot Radiographs in Young Children: Feasibility and Performance of a Convolutional Neural Network Model. J Digit Imaging. 2023;36:1419-1430. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |