Published online May 18, 2025. doi: 10.5312/wjo.v16.i5.105590
Revised: April 3, 2025
Accepted: April 27, 2025
Published online: May 18, 2025
Processing time: 107 Days and 21.7 Hours
In pediatric age group patients (< 18 years old) treated operatively for distal radius/both bone fractures extending imaging beyond the initial postoperative period -particularly in uncomplicated cases - appears to provide limited addi
To determine the necessary number of follow-up X-rays to use resources effi
Participants included in this study are pediatric age group patients who were treated operatively for distal radius/both bone fractures and were identified from a prospected collected data from the operating room database between the years 2009 and 2017. The data in the study included patients who had distal radius fractures and underwent fixation surgery (n = 88).
When assessing the difference in the odds of conducting 1 or less X-ray compared to 2 or more X-rays in regard to the type of fixation, the only significant difference is the closed reduction fixation method. Patients who underwent closed reduction method procedure have significantly lower odds of having 2 more X-rays com
The findings of this study reveal notable absence of a statistically significant association between the frequency of postoperative X-rays and the outcome of children with distal radius fractures.
Core Tip: The study of patients who underwent fixation surgery subsequent to distal radius fracture unveiled several noteworthy findings. To determine the necessary number of follow-up X-rays to use resources efficiently. A total of 88 individuals were included. The findings of this study reveal notable absence of a statistically significant association between the frequency of postoperative X-rays and the outcome of patients with distal radius fractures.
- Citation: Alomran AK, Alzahrani BA, Alamoud DS, Alsultan LS, AlSaud MM, Althobaiti RG, Alruwaili BS. Role of post-operative X-rays in distal-radius fractures among pediatric patients. World J Orthop 2025; 16(5): 105590
- URL: https://www.wjgnet.com/2218-5836/full/v16/i5/105590.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i5.105590
Fractures of the distal radius are the most frequently encountered type of orthopedic injury among children. The yearly rate of these fractures has risen due to children engaging in sports at an earlier age, a rise in body mass index, and a fall in bone mineral density[1]. A fall on an extended arm, leading to axial compression of the limb, or direct impact to the limb, typically causes these fractures. The Salter-Harris classification system is used to categorize physeal (growth plate) fractures of the distal radius. Distal radius fractures that do not involve the growth plate are classified as either incom
The escalating expenses within the healthcare sector have come under heightened scrutiny, particularly regarding the utilization and expenses associated with imaging services, which have surged at twice the rate of other healthcare technologies[2]. Furthermore, the proliferation of unnecessary follow-up appointments, coupled with prolonged waiting times for imaging procedures, exacerbates the financial burden. In addition to financial considerations, there is growing apprehension regarding the potential adverse effects of ionizing radiation exposure on patients. Medical imaging constitutes the primary source of ionizing radiation exposure for the United States population[3]. While the exact consequences of low-level radiation exposure remain somewhat uncertain, researchers argue that the risk of cancer[4] and cardiovascular[5] ailments correlates with radiation dosage. Moreover, radiographs performed in operating rooms (ORs) pose radiation exposure risks to both patients and hospital personnel.
According to a study conducted in Eastern province, Saudi Arabia, which showed unexpected and concerning results, indicating a noteworthy link between radiation exposure levels in various hospitals, especially related to X-ray and computed tomography scan procedures, with a significant association observed (P < 0.01). Although most hospitals are equipped with lead aprons and thyroid shields for radiation protection, approximately half do not provide lead glasses and lead shields, highlighting a deficiency in critical safety equipment. Additionally, the use of radiation dosimeters is surprisingly low, with only 57.7% and 68.9% adherence rates, underlining a gap in protective measures, which only raises further concerns regarding safety of physicians as well[6].
Therefore, it is imperative to reserve imaging studies for instances where they are clinically warranted to minimize exposure risks. Hence, the excessive utilization of imaging services warrants particular attention and scrutiny. A study conducted in 2010, in Turkey, encompassing 40 cases of forearm fractures treated with open reduction and plate internal fixation, underscored the pivotal role of routine postoperative X-rays in assessing rotational function for such fractures[7]. Conversely, a study in 2015 concluded in Jazan, Saudi Aabia, showed that postoperative radiography, particularly during the initial visit, is primarily instrumental in identifying radiographic changes, including loss of reduction, hardware failure, and hardware migration[8]. These findings suggest a nuanced approach to the timing and necessity of postoperative X-rays.
These conflicting findings underscore the necessity for a comprehensive review of existing literature and real-life clinical practices to elucidate the role of postoperative X-rays in distal radius fractures among pediatric patients. Such insights are crucial for optimizing patient care, minimizing unnecessary radiation exposure, and streamlining healthcare costs. Our aim is To evaluate post-treatment X-rays’ effectiveness in patients with distal radius fractures. This study seeks to determine the necessary number of follow-up X-rays to use resources efficiently. With the high incidence of distal radius fracture among children, it is important to revise the clinical practice done routinely following intervention with consideration of the exposure to ionizing radiation, cost, convenience, and availability of X-rays.
This study was conducted at King Fahad Hospital of the University in Al Khobar using the hospital’s electronic record system and the OR database.
Pediatric patients treated operatively at King Fahad Hospital of the University for distal radius fractures were identified from prospectively collected data in the OR database between 2009 and 2017. For patients meeting the criteria, their post-operative notes and follow-up visit notes were reviewed to extract relevant information.
Inclusion criteria including: (1) Pediatric age group (< 18 years old); (2) Treatment period from 2009 to 2017; and (3) Complete follow-up data and no missing information.
Exclusion criteria including: (1) Patients not meeting the inclusion criteria; (2) Missing information in the system; and (3) Sampling technique and sample size all applicable records meeting the inclusion criteria were included in the study, resulting in a sample size of 88 records from 2009 to 2017.
Demographics: Age, gender, date of admission. Fracture-related information: Site of the fracture, type of fixation, complications, changes in the management plan, and whether a second operation was required. A change in the management plan was defined as any deviation from the anticipated post-surgical pathway or treatment strategy. This included additional intraoperative or post-operative imaging requests, further surgical procedures, and adjustments in the schedule of follow-up visits.
The number of post-operative X-rays performed on each patient.
A data collection sheet was developed, listing patients obtained from the OR database for pediatric distal radius fractures between 2009 and 2017. Data for all relevant variables were extracted from the electronic medical records and entered into the sheet.
Following Institutional Review Board approval, a list of cases involving pediatric distal radius fractures from 2009 to 2017 was obtained from the OR records. Data were collected from medical records at King Fahad University Hospital in the Eastern Province of Saudi Arabia. The data were organized, coded, and imported into an Excel spreadsheet for analysis using the SPSS.
Frequencies and percentages were calculated to summarize the study variables. The Kruskal-Wallis H test and Mann-Whitney U test were used to evaluate the bivariate association between the study variables and the average number of X-rays performed per patient. A significance threshold of 0.05 was applied, and all analyses were conducted using SPSS software version 27 (IBM Corp, 2017). Crude odds ratios and their corresponding 95% confidence intervals were also determined.
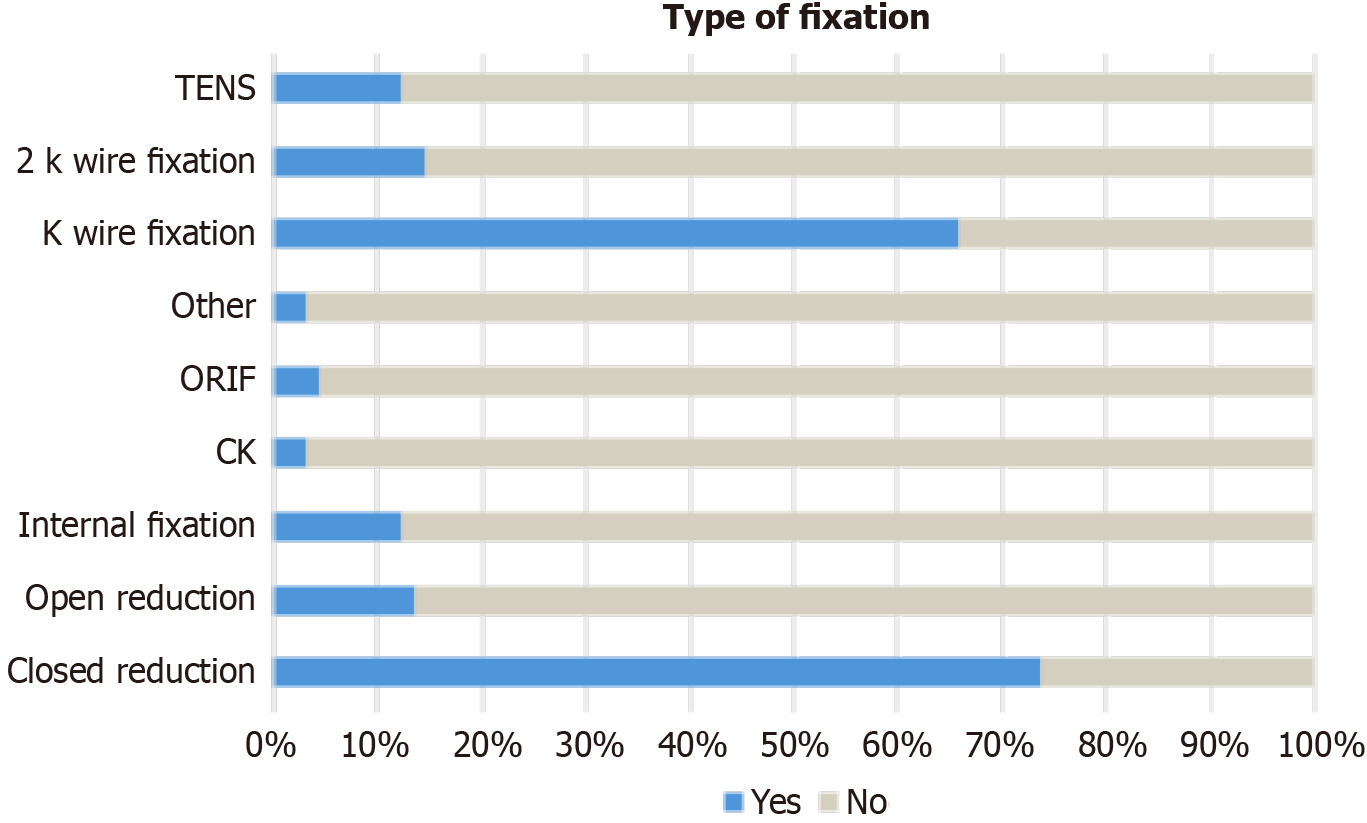
The data in the study included patients who have had distal radius fracture and underwent fixation surgery (n = 88). The majority of patients in the study were males (n = 77, 87.5%). The kind of fracture in the study appears to be more popular in the age group 12 to 14 (41%). Most fractures occurred within the diaphysis of the radius bone (n = 46, 52.3%). Furthermore, most patients underwent closed reduction fixation (n = 65, 73.9%), followed by K-wire fixation (n = 58, 65.9%), while close reduction and internal fixation (CRIF), open reduction and internal fixation, debridement, were minimally utilized. Table 1 illustrates patient characteristics. Most patients experienced no complications (n = 86, 97.7%), and almost all patients required no change in the management plan (n = 80, 90.9%). Finally, only 5% of the patients required a second operation (Table 1).
| Variable | Group | Frequency (%) |
| Gender | Male | 77 (87.5) |
| Female | 11 (12.5) | |
| Age (arbitrary classifications) | 3-5 years old | 17 (19.3) |
| 6-8 years old | 16 (18.2) | |
| 9-11 years old | 18 (20.5) | |
| 12-14 years old | 36 (40.9) | |
| Site of fracture | Epiphyseal | 15 (17.0) |
| Metaphyseal | 27 (30.7) | |
| Diaphyseal | 46 (52.3) | |
| Type of fixation/surgery | Closed reduction | 65 (73.9) |
| Open reduction | 12 (13.6) | |
| Internal fixation | 11 (12.5) | |
| CRIF | 1 (1.1) | |
| ORIF | 1 (1.1) | |
| Debridement | 1 (1.1) | |
| Epiphysiodesis | 1 (1.1) | |
| One K wire fixation | 58 (65.9) | |
| Two K wire fixation | 13 (14.8) | |
| TENS | 11 (12.5) | |
| Complications | Yes | 2 (2.3) |
| No | 86 (97.7) | |
| Change in management plan | Yes | 8 (9.1) |
| No | 80 (90.9) | |
| Second operation | Yes | 4 (4.5) |
| No | 84 (95.5) |
The few patients requiring a change in their management plan (n = 8, 9.1%) had various reasons. Some transitioned from cast to surgical intervention following a second X-ray, revealing a displaced greenstick fracture with angulation. Others were prescribed oral antibiotics with outpatient department follow-up, while some had scheduled follow-up appointments in another hospital. In cases where initial closed reduction in the emergency room was unsuccessful, patients were admitted under general anesthesia. Additionally, after a patient fell again, the cast was replaced. Fur
| X-ray post op | Frequency (%) |
| 1-2 weeks | 54 (61.4) |
| 3-4 weeks | 40 (45.5) |
| 5-6 weeks | 14 (15.9) |
| 7-8 weeks | 19 (21.6) |
| 9-10 weeks | 4 (4.5) |
| 11-12 weeks | 4 (4.5) |
| 13-14 weeks | 4 (4.5) |
| 4 months | 3 (3.4) |
| 5 months | 6 (6.8) |
| 6 months | 2 (2.3) |
| 7 months | 1 (1.1) |
| 8 months | 2 (2.3) |
| 9 months | 1 (1.1) |
| 10 months | 2 (2.3) |
| 11 months | 1 (1.1) |
| 1 year | 5 (5.7) |
| 1 year and a half | 1 (1.1) |
| 2 years | 2 (2.3) |
| 3-4 years | 1 (1.1) |
| Second operation X-ray | Frequency (%) |
| 1-2 weeks | 2 (50) |
| 3-4 weeks | 2 (50) |
| 6 weeks | 2 (50) |
| 9 weeks | 2 (50) |
| 3 months | 1 (25) |
| 9 months | 1 (25) |
None of the study variables appear to be significantly associated with the number of X-rays conducted on patients, using the Mann-Whitney U test and Kruskall-Wallis H test. Table 4 illustrates the influence of the number of X-rays on the study variables. Table 5 show that regardless of the type of fixation, the number of X-rays done to the patients does not differ significantly between the different types of fixations used. Tables 6 and 7 shows the odds ratio of variables influencing the number of X-rays done to each patient (≤ 1 X-ray or ≥ 2 X-rays) after the mandatory post op X-ray. The odds of having 2 or more X-rays when the patient is a male is almost 3 times higher than females, however, this difference is not significant (OR males = 2.897, P = 0.112). In addition, patients between 9 years to 11 years old undergo 2 or more X-rays three times higher than their younger counter parts aged 3 years to 5 years old. This difference, however, is not statistically significant (OR 9-11 years old = 3.111, P = 0.129). Figure 1 describe the types of fixations in the study.
| Variable | Frequency (%) | Total X-rays (median) (IQR) | Test (P value) |
| Gender | - | - | Mann-Whitney U = 348.500 (0.328) |
| Male | 77 (87.5) | 2.00 (1) | |
| Female | 11 (12.5) | 1.00 (3) | |
| Age | Kruskal-Wallis H = 0.378 (0.223) | ||
| 3-5 years old | 17 (19.3) | 2.00 (2) | |
| 6-8 years old | 16 (18.2) | 2.00 (1) | |
| 9-11 years old | 18 (20.5) | 2.00 (2) | |
| 12-14 years old | 36 (40.9) | 2.00 (2) | |
| Site of fracture | Kruskal-Wallis H = 0.201 (0.905) | ||
| Epiphyseal | 15 (17.0) | 2.00 (1) | |
| Metaphyseal | 27 (30.7) | 2.00 (1) | |
| Diaphyseal | 46 (52.3) | 2.00 (2) | |
| Complications | Mann-Whitney U = 75.00 (0.774) | ||
| Yes | 2 (2.3) | 1.50 (0) | |
| No | 86 (97.7) | 2.00 (1) | |
| Change in management plan | Mann-Whitney U = 307.00 (0.845) | ||
| Yes | 8 (9.1) | 2.00 (3) | |
| No | 80 (90.9) | 2.00 (1) | |
| Second operation | Mann-Whitney U = 148.500 (0.706) | ||
| Yes | 4 (4.5) | 1.50 (3) | |
| No | 84 (95.5) | 2.00 (1) | |
| Type of fixation | Frequency (%) | Total X-rays Median (IQR) | Mann-Whitney U test (P value) |
| Closed reduction | 65 (73.9) | 2.00 (1) | 584.00 (0.108) |
| Open reduction | 12 (13.6) | 2.00 (1) | 317.50 (0.082) |
| Internal fixation | 11 (12.5) | 2.00 (1) | 312.00 (0.146) |
| ORIF | 4 (4.5) | 1.00 (2) | 110.00 (0.261) |
| One K wire fixation | 58 (65.9) | 2.00 (1) | 778.00 (0.403) |
| Two K wire fixation | 13 (14.8) | 2.00 (2) | 431.00 (0.492) |
| TENS | 11 (12.5) | 2.00 (4) | 387.00 (0.634) |
| Other1 | 3 (3.4) | 3.00 (0) | 95.00 (0.481) |
| Variables | OR1 | 95%CI |
| Gender | ||
| Female | 1 | - |
| Male | 2.897 (0.112) | 0.780-10.758 |
| Age | ||
| 3-5 years old | 1 | - |
| 6-8 years old | 1.143 (0.849) | 0.290-4.507 |
| 9-11 years old | 3.111 (0.129) | 0.720-13.443 |
| 12-14 years old | 0.993 (0.991) | 0.313-3.155 |
| Site of fracture | ||
| Epiphyseal | 1 | - |
| Metaphyseal | 1.273 (0.710) | 0.357-4.542 |
| Diaphyseal | 1.361 (.607) | 0.421, 4.405 |
| Complications | ||
| No | 1 | - |
| Yes | 0.686 (0.793) | 0.042-11.342 |
| Change in management plan | ||
| No | 1 | - |
| Yes | 1.170 (0.837) | 0.261-5.239 |
| Second operation | ||
| No | 1 | - |
| Yes | 0.680 (0.707) | 0.091-5.064 |
| Type of fixation | OR1 | 95%CI |
| Closed reduction | 0.305 (0.035) | 0.101-0.919 |
| Open reduction | 4.048 (0.084) | 0.830-19.731 |
| Internal fixation | 3.558 (0.119) | 0.721-17.568 |
| ORIF | 0.680 (0.707) | 0.091-5.064 |
| K wire fixation | 0.615 (0.300) | 0.246-1.542 |
| 2 K wire fixation | 1.674 (0.424) | 0.473-5.924 |
| TENS | 1.244 (0.743) | 0.336-4.609 |
| Other2 | 3.723 (0.240) | 0.416-33.308 |
Surprisingly, patients with reported complications and patients requiring a second operation have lower number of X-rays compared to those without complications or those who do not require a second operation, this difference, although important, is not significant. Finally, there appears to be no difference in the number of X-rays according to the site of fracture, nor the change in the management plan. When assessing the difference in the odds of conducting 1 or less X-ray compared to 2 or more X-rays in regard to the type of fixation, the only significant difference is the closed reduction fixation method. Patients who underwent closed reduction method procedure have significantly lower odds of having 2 more X-rays compared to those who didn’t have closed reduction method (OR closed reduction = 0.305, P = 0.035). open reduction, internal fixation, and other fixation methods (CRIF, debridement, epiphysiodesis, or close k-wire insertion) have higher odds of having two or more X-rays compared to patients who did not receive these methods; however, these odds are not statistically significant.
The study of patients who underwent fixation surgery subsequent to distal radius fracture unveiled several noteworthy findings. Out of the 88 individuals scrutinized, a majority were male, comprising 87.5% of the total sample. Remarkably, individuals aged 12 to 14 seemed more prone to this specific fracture type, constituting a substantial 41% of cases observed. Most fractures were concentrated within the diaphysis of the radius bone. Closed reduction fixation stood out as the prevailing surgical approach, closely followed by K-wire fixation, while other methods like CRIF and open reduction and internal fixation were comparatively less utilized. Incidences of complications were rare, with only 9.1% of patients necessitating a modification in their management plan, often due to factors like displaced fractures or postoperative complications. Moreover, a minority of patients required a subsequent operation. X-rays formed an integral part of patient care, with the majority undergoing postoperative imaging at 1-2 weeks and 3-4 weeks, with some extending up to 3-4 years postoperatively. Intriguingly, the study unearthed no significant correlation between patient demographics, fracture type, or surgical approach with the frequency of X-rays administered. Furthermore, regardless of the method of fixation employed, there was no noticeable discrepancy in the number of X-rays administered to patients. These findings serve to deepen our comprehension of postoperative care and management tactics for distal radius fractures, emphasizing the efficacy and uniformity of current practices within this medical realm.
The study findings illuminate crucial aspects of managing distal radius fractures. One notable finding is the absence of a clear link between study variables and the frequency of X-rays conducted on patients, regardless of the type of fixation employed. These results stand in contrast to one study, which identified a subset of patients necessitating extra postope
Furthermore, the study highlights the overall low incidence of complications and the limited need for altering ma
Current guidelines on postoperative imaging in pediatric fractures emphasize a patient-specific approach, balancing the need for imaging against potential risks and costs. For example, the American Academy of Orthopaedic Surgeons suggests postoperative radiographs primarily when there are clinical indications such as suspected complications or persistent pain. The findings of this study underscore the potential to streamline imaging protocols, particularly in uncomplicated cases, aligning with broader efforts to reduce healthcare costs and minimize radiation exposure in pe
Additionally, prior studies highlight conflicting evidence regarding the frequency and utility of postoperative X-rays, with some advocating for routine imaging to monitor healing while others emphasize its limited clinical value. For example, research by[17,18] found that routine X-rays often failed to alter management decisions, raising questions about their necessity in standard practice. Conversely, a subset of literature[19-23], identifies scenarios where additional ima
The timing and frequency of postoperative X-rays, as highlighted in this study, remain a critical area for future exploration. The current practice of performing imaging at 1-2 weeks and 3-4 weeks post-surgery aligns with standard protocols for monitoring healing and identifying early complications[24-26]. However, extending imaging beyond the initial postoperative period - particularly in uncomplicated cases - appears to provide limited additional benefit. Studies like recommend restricting routine imaging to high-risk cases, such as those involving complex fractures or postoperative concerns, to optimize resource utilization without compromising patient outcomes[11]. This approach could be further refined through risk stratification models that consider factors such as fracture severity, patient age, and surgical tech
In summary, this study contributes to the understanding of distal radius fracture management by emphasizing the limited role of repetitive postoperative X-rays. While the findings support current efforts to reduce unnecessary imaging, further research is needed to develop evidence-based protocols that balance clinical needs with resource efficiency. Incorporating these insights into practice would enhance patient care, reduce healthcare burdens, and align with evolving guidelines in pediatric orthopedic management.
The findings of this study reveal notable absence of a statistically significant association between the frequency of post
We would like to extend our sincere appreciation to Dr. Arwa Alomran for her invaluable assistance in data analysis and data cleaning.
| 1. | Murphy RJ, Blundell CM. Are routine postoperative X-rays needed following surgery for hallux valgus? An evaluation of their use after scarf osteotomy. Ann R Coll Surg Engl. 2007;89:281-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Leschber G, May CJ, Simbrey-Chryselius N. [Do thoracic surgery patients always need a postoperative chest X-ray?]. Zentralbl Chir. 2014;139 Suppl 1:S43-S49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Nair V, Mirle V, Hynes K, Strelzow J. Efficacy of post-operative X-rays after operatively treated ankle fractures: What is their role? Injury. 2024;55:111595. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Cooney AD, Campbell AC. Do check X-rays influence the management of patients who have undergone hip fracture fixation using image intensifier guidance? Injury. 2006;37:763-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Chakravarthy J, Mangat K, Qureshi A, Porter K. Postoperative radiographs following hip fracture surgery. Do they influence patient management? Int J Clin Pract. 2007;61:421-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Segal D, Palmanovich E, Faour A, Marom E, Feldman V, Yaacobi E, Slevin O, Kish B, Brin YS. Routine early post-operative X-ray following internal fixation of intertrochanteric femoral fractures is unjustified: a quality improvement study. J Orthop Surg Res. 2018;13:189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Mercure CI, Hardcastle TC, Rocher AGL. The value of immediate postoperative radiographs following fluoroscopically-guided orthopaedic surgery in a polytrauma ICU setting in KwaZulu-Natal, South Africa. Injury. 2020;51:930-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Teo T, Schaeffer E, Cooper A, Mulpuri K. Do Immediate Postoperative Radiographs Change Patient Management After Fracture Fixation? A Systematic Review. J Orthop Trauma. 2018;32:211-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Hassan S, Wall A, Ayyaswamy B, Rogers S, Mills SP, Charalambous CP. Is there a need for early post-operative x-rays in primary total knee replacements? Experience of a centre in the UK. Ann R Coll Surg Engl. 2012;94:199-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Nair S, Nambiar M, Pope A, Parkes M, De Jong K, Hau R. Intraoperative fluoroscopy alone versus routine post-operative X-rays in identifying return to theatre after fracture fixation. ANZ J Surg. 2021;91:392-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Johnson SP, Chung KC, Zhong L, Sears ED, Waljee JF. Use of Postoperative Radiographs following Operative Fixation of Distal Radius Fractures. Plast Reconstr Surg. 2016;138:1255-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Miniaci-Coxhead SL, Martin EA, Ketz JP. Quality and Utility of Immediate Formal Postoperative Radiographs in Ankle Fractures. Foot Ankle Int. 2015;36:1196-1201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Kröner A, Beenen L, du Raan M, Meijer P, Spronk PE, Stoker J, Hollmann MW, Schultz MJ. The clinical value of routinely obtained postoperative chest radiographs in post-anaesthesia care unit patients seems poor-a prospective observational study. Ann Transl Med. 2018;6:360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Sjølander HJ, Jauffred S, Brix M, Gundtoft PH. X-ray Follow-up after Open Reduction Internal Fixation of Distal Forearm Fracture. J Wrist Surg. 2021;10:150-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Bergin D, Kearns S, Cullen E. Postoperative imaging of the ankle and foot. Semin Musculoskelet Radiol. 2011;15:408-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Brown ML, Michel D, Narayanan A, McCauley JC, Bugbee WD. Are immediate postoperative X-Rays valuable in evaluating complications of primary total hip arthroplasty? Arthroplasty. 2022;4:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 17. | Saggi SS, Kuah LZD, Toh LCA, Shah MTBM, Wong MK, Bin Abd Razak HR. Optimisation of postoperative X-ray acquisition for orthopaedic patients. BMJ Open Qual. 2022;11:e001216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 18. | Goodwin ML, Buchowski JM, Sciubba DM. Why X-rays? The importance of radiographs in spine surgery. Spine J. 2022;22:1759-1767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Piazzolla A, Montemurro V, Bizzoca D, Parato C, Carlucci S, Moretti B. Accuracy of plain radiographs to identify wrong positioned free hand pedicle screw in the deformed spine. J Neurosurg Sci. 2019;63:372-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Herman A, Landau Y, Gutman G, Ougortsin V, Chechick A, Shazar N. Radiological evaluation of intertrochanteric fracture fixation by the proximal femoral nail. Injury. 2012;43:856-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Tufescu T. Working toward reducing postoperative fracture radiographs: a survey of Canadian surgeons. Can J Surg. 2016;59:26-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Hartog TD, Bozoghlian M, Christensen G, Meeker D, Nepola JV, Patterson BM. Utility of Recovery Room vs Post-Operative Day 1 Radiographs Following Shoulder Arthroplasty. Iowa Orthop J. 2024;44:99-103. [PubMed] |
| 23. | Galata C, Cascant Ortolano L, Shafiei S, Hetjens S, Müller L, Stauber RH, Stamenovic D, Roessner ED, Karampinis I. Are Routine Chest X-rays Necessary following Thoracic Surgery? A Systematic Literature Review and Meta-Analysis. Cancers (Basel). 2022;14:4361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 24. | Park JH, Kim DH, Chai JW, Kim HJ, Seo J, Son JY. [Imaging Evaluation of Early and Long-Term Complications Associated with the Postoperative Spine]. J Korean Soc Radiol. 2024;85:36-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 25. | Hertzberg M, Maier L, Heil H, Hoegler J, Guthrie ST, Hakeos W. Postoperative Chest X-Rays After Open Reduction Internal Fixation of Clavicle Fractures May Not Be Cost-Effective or Necessary. J Orthop Trauma. 2023;37:e270-e273. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Buenter IR, Kremo V, Schelbert P, van Veelen NM, Diwersi N, Knobe M, Link BC, Babst R, Beeres FJP, van de Wall BJM. Is there a need for standardized postoperative X-rays after operative treatment of clavicular fractures? Eur J Trauma Emerg Surg. 2022;48:2477-2482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |