Published online May 18, 2025. doi: 10.5312/wjo.v16.i5.104438
Revised: March 22, 2025
Accepted: April 14, 2025
Published online: May 18, 2025
Processing time: 147 Days and 12.7 Hours
Operative reports (OP-Rs) are essential for communication among healthcare providers. They require accuracy and completeness to serve as a quality indicator of patient care. Objective assessment of primary total knee replacement (TKR) OP-Rs has never been reported. Therefore, a standardized benchmark for assessment and factors affecting the completeness of TKR OP-Rs needs to be evaluated.
To evaluate the completeness rate of primary TKR OP-Rs in a teaching hospital and to assess the factors affecting completeness.
A retrospective review of 58 consecutive primary TKR OP-Rs in a tertiary te
After analyzing 58 cases, we found that the time to documentation was 1.5 hours. Out of the 52 mandatory variables, a median of 30 variables were documented yielding a completeness of 58%. Administrative, procedural, exposure, and im
Multiple variables were left undocumented on the unstructured primary TKR OP-Rs. The completeness percentage will likely improve after the implementation of a standardized structured OP-R.
Core Tip: Operative reports (OP-Rs) are a crucial part of patient care and safety. Currently, there is no standardized method for the documentation of the primary total knee replacement (TKR) procedure. A standardized list of documentation variables was created and the completeness of the primary TKR OP-Rs was assessed. It was found that multiple mandatory variables were infrequently documented. This study proposes a standardized method for documenting primary TKR OP-R to improve the reliability of this crucial document.
- Citation: Almousa SA. Quality of primary total knee arthroplasty operative reports in a tertiary teaching hospital. World J Orthop 2025; 16(5): 104438
- URL: https://www.wjgnet.com/2218-5836/full/v16/i5/104438.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i5.104438
Operative reports (OP-Rs) provide a detailed account of the performed procedure as well as a legal record of the operation[1,2]. The accuracy and completeness of OP-Rs are essential for communication among healthcare providers particularly for procedures where postoperative care is dependent on the detailed information contained in the report. Variables included in OP-Rs may serve as a quality indicator that can be used as a surrogate for health care outcome data[3,4]. The American College of Surgeons and the Royal College of Surgeons have issued guidelines outlining the essential components of a surgical report[5,6]. They include patient identification, preoperative diagnosis, a detailed description of the procedure, and postoperative care plans. However, studies have shown a wide variation in the adherence to these guidelines in many surgical specialties[7-10]. Orthopedic surgery OP-Rs, including joint arthroplasty, were found to be lacking in critical aspects of the procedure[11,12].
Several factors influence the quality of OP-Rs, including the surgeon’s experience[13], the use of templates[14], and the method of dictation. Structured templates ensure that all essential components are included. This method reduces the likelihood of omitting critical information[15]. Newer dictation methods such as speech recognition software and electronic health record-integrated templates have demonstrated improvement in the consistency and accuracy of OP-Rs[16]. The primary objective of this retrospective review was to assess the completeness of primary total knee replacement (TKR) OP-Rs utilizing document analysis of six subsets of standardized variables that were created by consensus of subspecialized arthroplasty surgeons. The secondary objective was to explore the factors affecting the completeness of these reports.
After institutional review board approval (No. IRB-2024-01-682), a retrospective review of the OP-Rs of all patients who underwent primary TKR at a single tertiary academic hospital from August 2023 through August 2024 was performed. Primary TKR was performed by three subspeciality trained surgeons. Operative notes were documented utilizing an electronic medical record that allows typed notes, verbal dictation, or documentation via preset templates (Trakcare InterSystems Corporation, Cambridge, MA, United States). Revision TKR cases were excluded. Patient demographics including age, sex, body mass index, sequence of the operation on the operative list, duration of the operation, presence of complications, and length of hospital stay were collected. The level of experience of the documenter and the time from the end of surgery to completion of the OP-R were recorded.
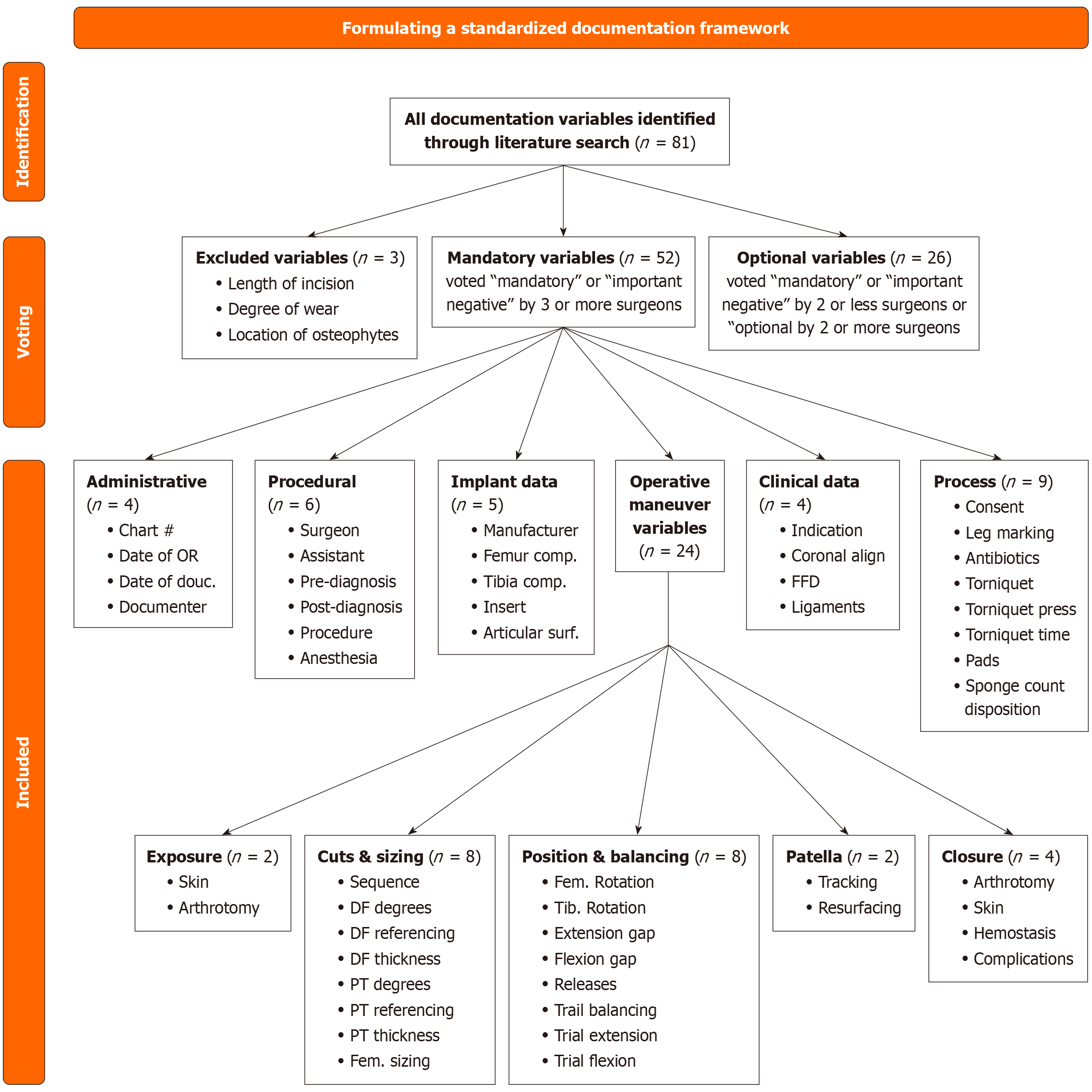
We formulated a preset list of variables to analyze the content of the OP-Rs. First an inclusive list of all variables relevant to the TKR procedure based on a literature review was compiled. The variables were subdivided into six categories of each element of the procedure. The categories included administrative, procedural, implant data, clinical data, process, and operative maneuver. The operative maneuver category was further subdivided into five divisions including exposure, bone cuts and sizing, position and balancing, patella, and closure. This inclusive list was evaluated by four arthroplasty subspecialized surgeons who labeled each variable as being either mandatory, important, optional, or not required. A variable was included for the evaluation of the completeness of the OP-R if it was voted mandatory or important by at least three surgeons. Variables voted mandatory or important by two or fewer surgeons or optional by two or more surgeons were not used for the scoring of the completeness of the OP-Rs. The list for the analysis included a total of 78 variables, 52 of which were mandatory or important and 26 of which were optional (Figure 1).
Summary statistics for patient demographics and documentation variables were calculated. The completeness of each variable was calculated individually. Continuous variables were summarized by means for normally distributed data and by medians with interquartile ranges for non-normally distributed data. Categorical variables were reported as frequencies and percentages. The completeness of documentation was evaluated based on quartiles for both mandatory and optional items. Further analysis examined the association of patient and documenter-related factors with do
A total of 64 primary TKR cases were identified. The OP-Rs were not documented in the electronic record system for 6 patients and were excluded. A total of 58 OP-Rs were analyzed. The patient demographics revealed that 16 patients (27.6%) were male and 42 patients (72.4%) were female. The mean age was 63.1 ± 9.4 years, and the median body mass index was 32.4 (28.7-37.3). Eight patients (13.8%) were diabetic. Three cases reported an intraoperative complication: One case had a medial femoral condyle fracture requiring reduction and fixation with screws; and two cases had a lateral collateral ligament rupture and medial collateral ligament proximal avulsion requiring repair and fixation in addition to a constraint articular surface. Of the cases analyzed, 37 (63.8%) were the first case of the day, 20 (34.5%) were the second cases of the day, and one (1.72%) was the third case of the day. The average operation duration was 177.0 ± 43.1 minutes. The median length of hospital stay was 4 days (3-4), indicating consistency in hospital stays across cases. The median time from the end of surgery to OP-R documentation was 1.5 hours (0.2-11.7). OP-R documentation was completed by a consultant with arthroplasty subspeciality training in 3 cases (5.2%), a registrar who completed orthopedic board training in 1 case (1.7%), a fourth-year resident in 32 cases (53.4%), a third-year resident in 11 cases (19.0%), a second-year resident in 8 cases (13.8%), and first-year resident in 4 cases (6.9%) (Table 1).
| Case demographics | n = 58 |
| Sex | |
| Female | 42 (72.4) |
| Male | 16 (27.6) |
| Age | 63.1 (9.4) |
| Body mass index | 32.4 (28.7-37.3) |
| Diabetic | |
| Yes | 8 (13.8) |
| No | 50 (86.2) |
| Sequence of the case | |
| First | 37 (63.8) |
| Second | 20 (34.5) |
| Third | 1 (1.7) |
| Complications | |
| LCL injury | 1 (1.7) |
| MCL avulsion | 1 (1.7) |
| Femoral condyle fracture | 1 (1.7) |
| Length of stay in days | 4.00 (3.0-4.0) |
| Duration of operation in minutes | 177 (43.1) |
| Documenter demographics | |
| Level of documenter | |
| R1 | 4 (6.9) |
| R2 | 8 (13.8) |
| R3 | 11 (19.0) |
| R4 | 31 (53.4) |
| Registrar | 1 (1.7) |
| Attending consultant | 3 (5.2) |
| Time to documentation in hours | 1.5 (0.2-11.7) |
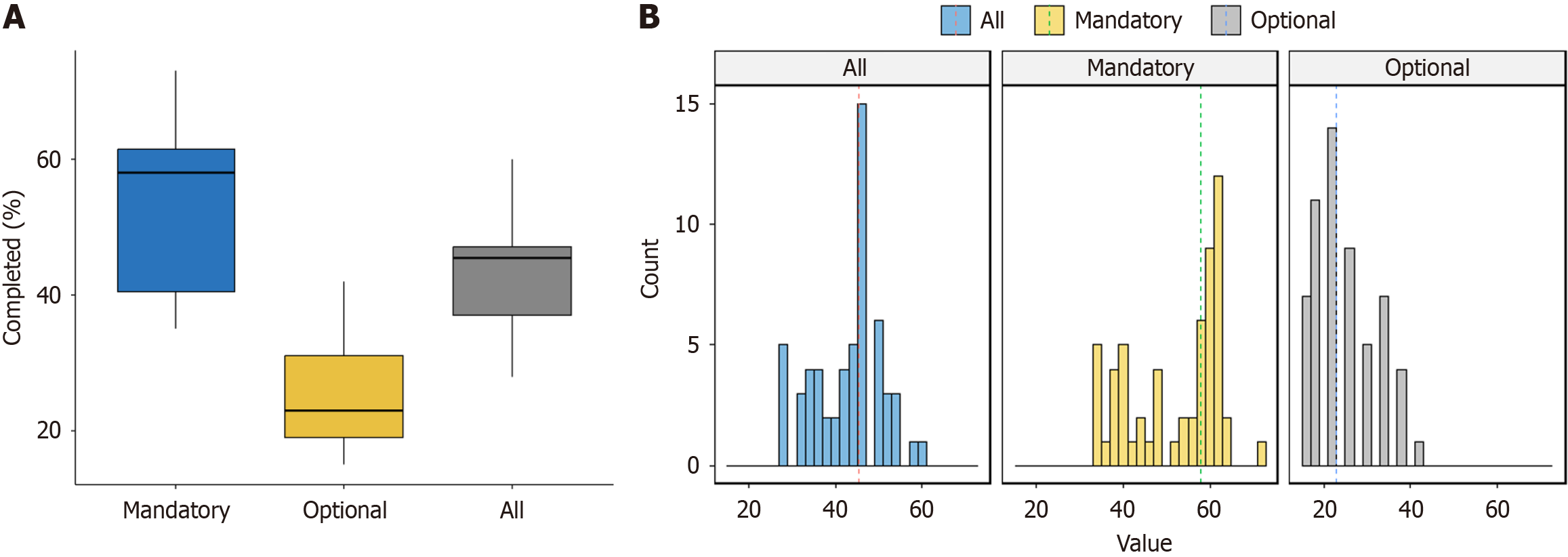
A total of 52 mandatory items and 26 optional items were evaluated in the OP-Rs. The median number of documented mandatory items was 30.0 (18.0-38.0), with a completeness percentage of 58.0% (35.0%-73.0%). The median number of documented optional items was 6.0 (4.0-11.0), with a completeness percentage of 23.0% (15.0%-42.0%) (Figure 2). In the administrative category all four mandatory variables were documented in 100% of cases. In the procedural category the six mandatory variables were almost always documented, with rates of 100% for surgeon, assistant, and procedure, and 98.3% for type of anesthesia. Preoperative diagnosis was documented in 63.8% of cases, while postoperative diagnosis was documented in 50.0%. The median of documented mandatory items was 5.5 (3.0-6.0), showing variability in documentation. Documentation of patient position was optional and was documented in 98.3% of cases.
The implant category had high documentation rates for the mandatory variables: 86.2% for manufacturer; 93.1% for femoral component size; 93.1% for tibial component size; 96.6% for insert thickness; and 63.8% for articular surface type. The median of documented mandatory items was 5.00 (1.0-5.0). In the clinical data category, the documentation of mandatory variables was low. Indication for surgery was documented in 25.9% of cases, while coronal alignment, fixed flexion deformity, and ligament testing were not documented in any cases (0%) with a median of 0.0 (0.0-1.0). Optional variables such as presence of comorbidities, patella tendon height, calcified popliteal artery, and urgency of surgery were also not documented (0%).
The process category had variable documentation rates. Consent obtained and leg marked were each documented in 3.5% of cases, antibiotic prophylaxis was documented in 58.6%, tourniquet applied was documented in 87.9%, tourniquet pressure was documented in 15.5%, tourniquet duration was documented in 44.8%, and disposition was documented in 79.3%. The use of protective pads and count of sponges variables were not documented in any cases (0%). The median of documented mandatory variables was 3.0 (1.0-5.0). Optional variables such as the American Society of Anesthesiologists status (0%), timeout performed (39.7%), deep vein thrombosis prophylaxis (0%), and postoperative neurovascular assessment (8.62%) were infrequently documented (Table 2).
| Mandatory variables | n (%) | Optional variables | n (%) |
| Administrative | |||
| Chart number | 58 (100) | ||
| Date of procedure | 58 (100) | ||
| Date of dictation | 58 (100) | ||
| Dictating physician | 58 (100) | ||
| Median (range) | 4.0 (4.0-4.0) | ||
| Procedural | |||
| Surgeon | 58 (100) | Position | 57 (98.3) |
| Assistant | 58 (100) | ||
| Preoperative diagnosis | 37 (63.8) | ||
| Postoperative diagnosis | 29 (50.0) | ||
| Procedure | 58 (100) | ||
| Type of anesthesia | 57 (98.3) | ||
| Median (range) | 5.5 (3.0-6.0) | ||
| Implant data | |||
| Manufacturer | 50 (86.2) | Patellar implant | 1 (1.7) |
| Femoral component size | 54 (93.1) | Use of stems | 0 (0) |
| Tibial component size | 54 (93.1) | Use of augments | 4 (6.9) |
| Insert thickness | 56 (96.6) | ||
| Articular surface type | 37 (63.8) | ||
| Median (range) | 5.0 (1.0-5.0) | Median (range) | 0.0 (0.0-2.0) |
| Clinical data | |||
| Indication for surgery | 15 (25.9) | Presence of comorbidities | 0 (0) |
| Coronal alignment | 0 (0) | Patella tendon Hight | 0 (0) |
| Fixed flexion deformity | 0 (0) | Calcified popliteal artery | 0 (0) |
| Ligament testing | 0 (0) | Urgency of surgery | 0 (0) |
| Median | 0.0 (0.0-1.0) | Median | 0.0 (0.0-0.0) |
| Process | |||
| Consent obtained | 2 (3.5) | ASA status | 0 (0) |
| Leg marked | 2 (3.5) | Timeout performed | 23 (39.7) |
| Antibiotic prophylaxis | 34 (58.6) | DVT prophylaxis | 0 (0) |
| Torniquet applied | 51 (87.9) | Postoperative NV assessment | 5 (8.62) |
| Torniquet pressure | 9 (15.5) | ||
| Torniquet duration | 26 (44.8) | ||
| Use of protective pads | 0 (0) | ||
| Count of sponges | 0 (0) | ||
| Disposition | 46 (79.3) | ||
| Median | 3.0 (1.0-5.0) | Median | 0.0 (0.0-2.0) |
The operative maneuver variables were further divided into five divisions. Exposure data were well-documented, with skin incision recorded in 91.4% of cases and arthrotomy description in 98.3%, with a median of 2.00 (0.0-2.0). Bone cuts and sizing data had documentation variability. The sequence of bone cuts was recorded in 98.3% of cases, the degrees of distal femur cut in 55.2%, and referencing of the distal femur cut in 58.6%. Thickness of the distal femur cut was rarely documented (5.2%), while degrees of the proximal tibia cut (63.8%) and referencing of the proximal tibia cut (58.6%) were documented more frequently. Femoral sizing was recorded in 70.7% of cases. The median of documented mandatory items was 5.5 (0.0-8.0).
The position and balancing division also had variable documentation. Referencing of the femoral rotation was documented in 55.2% of cases, while referencing of the tibial rotation was not documented at all (0%). Extension gap balance was recorded in 36.2% of cases, flexion gap balance in 29.3%, and description of releases in 27.6%. Trial balance findings were documented in 96.6% of cases, but trial knee extension degrees and flexion degrees were rarely recorded (1.72% and 6.90%, respectively). The median of documented mandatory items was 2.00 (0.0-6.0).
The patella division was documented infrequently. Patellar tracking was documented in 32.8% of cases, while patellar resurfacing was not recorded at all (0%). Patellar facetectomy was recorded in 12.1% of cases and patellar denervation in 10.3%. Finally, the closure division had variable documentation. Arthrotomy closure and skin closure were documented in 50.0% and 91.4% of cases, respectively. Cementing technique had a high documentation rate of 93.1%. Hemostasias was recorded in 17.2% of cases, capsule infiltration in 13.8%, and intraoperative complications in 12.1%. The median of documented mandatory items was 7.00 (1.0-10.0) (Table 3).
| Mandatory variables | n (%) | Optional variables | n (%) |
| Exposure | |||
| Skin incision | 53 (91.4) | Release of LPFL | 1 (1.7) |
| Arthrotomy description | 57 (98.3) | Excision of synovium | 29 (50.0) |
| Excision of fat pad | 38 (65.5) | ||
| Patella flipped or slid | 47 (81.0) | ||
| Median (range) | 2.0 (0.0-2.0) | Median (range) | 2.0 (0.0-3.0) |
| Bone cuts and sizing | |||
| Sequence of bone cuts | 57 (98.3) | Box cutting | 22 (37.9) |
| Degrees of distal femur cut | 32 (55.2) | ||
| Referencing of distal femur cut | 34 (58.6) | ||
| Thickness of distal femur cut | 3 (5.2) | ||
| Degrees of proximal tibia cut | 37 (63.8) | ||
| Thickness of proximal tibia cut | 4 (6.9) | ||
| Referencing of proximal tibia cut | 34 (58.6) | ||
| Femoral sizing | 41 (70.7) | ||
| Median (range) | 5.5 (0.0-8.0) | ||
| Position and balancing | |||
| Referencing of femoral rotation | 32 (55.2) | ||
| Referencing of tibial rotation | 0 (0) | ||
| Extension gap balance in mm | 21 (36.2) | ||
| Flexion gap balance in mm | 17 (29.3) | ||
| Description of releases | 16 (27.6) | ||
| Trial balance finding | 56 (96.6) | ||
| Trial knee extension degrees | 1 (1.7) | ||
| Trial knee flexion degrees | 4 (6.9) | ||
| Median (range) | 2.0 (0.0-6.0) | ||
| Patella | |||
| Patellar tracking | 19 (32.8) | Patellar facetectomy | 7 (12.1) |
| Patellar resurfacing performed | 0 (0) | Patellar denervation | 6 (10.3) |
| Median (range) | 0.0 (0.0-1.0) | Median (range) | 0.0 (0.0-2.0) |
| Closure | |||
| Arthrotomy closure | 29 (50.0) | Cementing technique | 54 (93.1) |
| Skin closure | 53 (91.4) | TXA injection | 9 (15.5) |
| Haemostasias | 10 (17.2) | Capsule infiltration | 8 (13.8) |
| Intraoperative complications | 7 (12.1) | Use of vancomycin powder | 15 (25.9) |
| Intraoperative transfusion | 0 (0) | ||
| Drain | 0 (0) | ||
| Type of dressing | 0 (0) | ||
| Median (range) | 7.0 (1.0-10.0) | Median (range) | 2.0 (1.0-5.0) |
The level of completeness of the OP-Rs was divided into quartiles (Q) and compared. The time from the end of surgery to documentation showed no significant differences (P = 0.167), though Q3 had the longest median time (5.53 hours) compared with the other quartiles. The training level of the documenter did not show significant differences across quartiles (P = 0.153), with fourth year residents being the most common training level across all quartiles. When the training level was divided into junior resident (years 1 and 2), senior residents (years 3 and 4), and board certified (consultants and registrars), the quartiles did not differ significantly (P = 0.117). Q4 had a higher proportion of junior residents (44.4%) compared with the other quartiles. We observed that senior residents had the highest completeness rate for the procedural and process mandatory variables. Board-certified surgeons had the highest median for documenting mandatory variables in the bone cuts and sizing and closure divisions. The order of the case was not significantly different between quartiles (P = 0.954). The operative duration differed significantly across quartiles (P = 0.002), with Q2 having the longest median duration (202 minutes) and Q3 the shortest (147 minutes). Complications were rare across quartiles, and no significant differences were observed (P = 0.353). The length of hospital stay was similar across quartiles, with no significant differences (P = 0.974) (Table 4).
| Factors | Q1 | Q2 | Q3 | Q4 | P value |
| Sex | 0.152 | ||||
| Female | 13 (86.7) | 13 (68.4) | 12 (80.0) | 4 (44.4) | |
| Male | 2 (13.3) | 6 (31.6) | 3 (20.0) | 5 (55.6) | |
| Age | 63.3 (10.2) | 65.7 (8.9) | 58.9 (10.1) | 64.4 (5.6) | 0.208 |
| Body mass index | 32.0 (30.7-33.8) | 33.2 (27.3-39.0) | 33.3 (29.6-38.7) | 31.1 (24.1-35.9) | 0.542 |
| Diabetes | 0.142 | ||||
| No | 13 (86.7) | 16 (84.2) | 15 (100) | 6 (66.7) | |
| Yes | 2 (13.3) | 3 (15.8) | 0 (0) | 3 (33.3) | |
| Sequence of the case | 0.954 | ||||
| First | 9 (60.0) | 13 (68.4) | 9 (60.0) | 6 (66.7) | |
| Second | 6 (40.0) | 6 (31.6) | 5 (33.3) | 3 (33.3) | |
| Third | 0 (0.00) | 0 (0.00) | 1 (6.7) | 0 (0.00) | |
| Operation duration in minutes | 175 (32.7) | 202 (43.9) | 147 (36.8) | 180 (37.8) | 0.002 |
| Presence of complication | 0.353 | ||||
| LCL rupture | 0 (0) | 1 (5.3) | 0 (0) | 0 (0) | |
| MCL avulsion | 1 (6.7) | 0 (0) | 0 (0) | 0 (0) | |
| Medial condyle fracture | 0 (0) | 0 (0) | 0 (0) | 1 (11.1) | |
| Length of hospital stay in days | 4.00 (3.00, 4.00) | 4.00 (3.00, 4.00) | 3.00 (3.00, 4.00) | 4.00 (3.00, 5.00) | 0.974 |
| Time to documentation in hours | 0.40 (0.15-5.21) | 0.72 (0.12-4.38) | 5.53 (0.54-17.8) | 3.18 (0.07-5.08) | 0.167 |
| Training level of documenter | 0.153 | ||||
| Consultant | 0 (0) | 2 (10.5) | 0 (0) | 1 (11.1) | |
| R1 | 1 (6.7) | 0 (0) | 1 (6.7) | 2 (22.2) | |
| R2 | 3 (20.0) | 2 (10.5) | 1 (6.7) | 2 (22.2) | |
| R3 | 1 (6.7) | 6 (31.6) | 2 (13.3) | 2 (22.2) | |
| R4 | 10 (66.7) | 8 (42.1) | 11 (73.3) | 2 (22.2) | |
| Specialist | 0 (0) | 1 (5.3) | 0 (0) | 0 (0) | |
| Grouped training level of the documenter | 0.117 | ||||
| Junior resident | 4 (26.7) | 2 (10.5) | 2 (13.3) | 4 (44.4) | |
| Senior resident | 11 (73.3) | 14 (73.7) | 13 (86.7) | 4 (44.4) | |
| Board certified | 0 (0) | 3 (15.8) | 0 (0) | 1 (11.1) |
The main objective of this study was to assess the completeness of primary TKR OP-Rs. TKR is a straight-forward procedure with consistent intraoperative maneuvers and minimal variations between cases. It was hypothesized that this consistency would have a positive effect on the completeness of the OP-Rs. The secondary objective explored the factors that may affect the completeness of the OP-Rs. To the best of our knowledge there is not a standardized set of criteria to assess the completeness of TKR OP-Rs. Therefore, we created a list of 52 mandatory variables to complete our objectives. Our analysis revealed that the TKR OP-Rs were frequently incomplete, with an average of 58% completeness and ranging from as low as 35% to as high as 73%. This low completeness rate indicates that the TKR OP-Rs are a poor source of data for patient care and quality assurance.
Administrative, procedural, and implant variables were often documented, likely due to the automatic prompting by the documentation system in our hospital. In contrast, clinical and process variables, which are documented based on documenter discretion, were frequently omitted. There was 0% documentation of preoperative limb alignment and preoperative ligament testing, both of which have implications for the operative maneuvers performed. Operative maneuver documentation showed variability with the exposure division having a high documentation rate. The bone cuts and sizing division had a moderate-to-low documentation rate, and implant position and balancing were rarely documented. Flexion and extension gap balancing and the description of soft tissue release were documented in less than one-third of the cases. These observations indicate that a documentation system prompting the documentation of a certain variable will result in a higher completeness rate in comparison with a system in which documentation is at the documenter’s discretion. Although it may be difficult to tailor a documentation scaffold mandating data variables for each and every surgical procedure (especially due to the variability amongst procedures even within the same specialty), this method should be considered for prevalent procedures with consistent operative steps such as TKR.
The findings of this study are similar to prior orthopedic surgical documentation analyses. An audit conducted by Coughlan et al[9] showed 100% documentation of date, surgeon name, assistant name, and procedure. Diagnosis was documented in 74.6% of cases, and closure details in 98.3% cases, while incision details (23.8%) and documentation of torniquet if used (0%) were documented infrequently. Mustafa et al[8] assessed the quality of orthopedic notes in 59 cases and showed frequent documenting of the date (86%), diagnosis (85%), operating surgeon (90%), assistants’ names (86%), operative procedure (98%), and detailed postoperative instructions (98%). Zahid et al[17] assessed the adherence to the Royal College of Surgeons guidelines. They found frequent documentation of administrative and procedural variables including date of surgery (97.4%), surgeon’s name (99.0%), anesthetist name (86.7%), and procedure (95.9%) and infrequent documentation for operative diagnosis (6.2%).
This study did not show any association between the completeness of the OP-Rs and documentation variables or case outcome variables. In a study evaluating the OP-Rs of pancreatic surgery, Wiebe et al[3] found no significant association between documenter level and the completeness of all collected variables except for documenting the timeout, which was reported more often by fellows, and for anastomosis type and specimen disposition, which were reported more often by residents. Wiebe et al[3] documented a positive association between report completeness and operative time with no association with the length of hospital stay or the presence of perioperative complications. The lack of association in this study may have resulted from the small number of cases included. A well-powered study may be needed to further explore the association between OP-R completeness and other factors.
Despite the wide adoption of electronic health records in many hospital facilities and their potential benefits in improving the quality of procedural documentation, there are still improvements to be made. Electronic health records may contain inaccurate information and do not always tell a complete story about a patient. The development of informatic frameworks may be able to address these caveats[18]. For example, incorporating a procedural framework that is specific for a procedure (such as framework constructed for TKR in this manuscript) would lead to improvement for the completeness of the OP-R as well as increase the quality of the documentation.
In contrast to narrative operative reporting, alternative reporting methods have been increasingly adopted. Standardized operative reporting, also referred to as synoptic reporting, uses template-based reports. They are often reported as a list in data point format. Synoptic reporting templates can be computerized and incorporated in electronic health records. They have the potential of improving the quality and efficiency of operative reporting[19,20]. The standardized TKR documentation framework presented in this manuscript could serve as a reference to formulate a TKR synoptic reporting templates. The potential to improve the completeness, quality, and efficacy of operative reporting will have benefits in healthcare communication. Systematic video documentation where the surgeon records a video of key elements of a procedure has also been shown to improve the quality of operative reporting[21]. However, this may be useful for arthroscopic procedures only and may not be practical in open procedures such as TKR.
It is important to acknowledge certain limitations of this study. OP-Rs were missing for 6 cases, all of which were excluded. This may have skewed the results of the analysis towards a better completeness rate. A second limitation is the small sample size which may explain the lack of statistically significant association between the documenter and outcome variables with the completeness of the OP-Rs. Another limitation was the retrospective nature of the study. It is impossible to guarantee that the procedure performed was documented exactly and correctly. It was also difficult to assess if there was a dictation or supervision effect on the OP-Rs completed by a junior documenter. To confirm our findings future research should consider a prospective assessment of OP-Rs to assess both the completeness and the correctness of the reports. An assessment of interventions, such as educational sessions and standardized templates, aimed at improving the completeness of the reports should also be undertaken.
Unstructured TKR OP-Rs led to infrequent documentation of several mandatory operative variables. The incompleteness of the OP-Rs may adversely affect future clinical management, research quality assurance, and medicolegal value. Implementation of standardized and structured operative reporting education in surgical training programs should be explored to improve this crucial documentation step in healthcare departments.
The author would like to thank Ahmad Kamal for his statistical advice.
| 1. | Thomas J. Medical records and issues in negligence. Indian J Urol. 2009;25:384-388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Khalid A, Shahzad MZUA, Ahmed H, Gilani A, Khan KH. Audit of Operative Notes Against Royal College of Surgeons Guidelines in a Tertiary Health Care Surgical Unit in Lahore. Cureus. 2022;14:e29313. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 3. | Wiebe ME, Sandhu L, Takata JL, Kennedy ED, Baxter NN, Gagliardi AR, Urbach DR, Wei AC. Quality of narrative operative reports in pancreatic surgery. Can J Surg. 2013;56:E121-E127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Mathioudakis A, Rousalova I, Gagnat AA, Saad N, Hardavella G. How to keep good clinical records. Breathe (Sheff). 2016;12:369-373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 5. | Royal College of Surgeons of England. Good Surgical Practice. [cited 29 October 2024]. Available from: https://www.rcseng.ac.uk/standards-and-research/gsp/. |
| 6. | Royal College of Surgeons of England. Record Your Work Clearly, Accurately and Legibly. [cited 29 October 2024]. Available from: https://rcseng.ac.uk/standards-and-research/gsp/domain-1/1-3-record-your-work-clearly-accurately-and-legibly/. |
| 7. | Severn Audit and Research Collaborative in Orthopaedics (SARCO). Assessing the quality of operation notes: a review of 1092 operation notes in 9 UK hospitals. Patient Saf Surg. 2016;10:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Mustafa MKE, Khairy AMM, Ahmed ABE. Assessing the Quality of Orthopaedic Operation Notes in Accordance With the Royal College of Surgeons Guidelines: An Audit Cycle. Cureus. 2020;12:e9707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Coughlan F, Ellanti P, Ní Fhoghlu C, Moriarity A, Hogan N. Audit of Orthopaedic Surgical Documentation. Surg Res Pract. 2015;2015:782720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Tuteja S, Tiwari A, Bhanushali J, Bagaria V. Results of an Audit of Orthopaedic Operation Notes from a Tertiary Care Centre: Are We Doing It Right and Can We Do More? Indian J Orthop. 2022;56:2223-2227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Morgan D, Fisher N, Ahmad A, Alam F. Improving operation notes to meet British Orthopaedic Association guidelines. Ann R Coll Surg Engl. 2009;91:217-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Barritt AW, Clark L, Cohen AM, Hosangadi-Jayedev N, Gibb PA. Improving the quality of procedure-specific operation reports in orthopaedic surgery. Ann R Coll Surg Engl. 2010;92:159-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Porterfield JR Jr, Altom LK, Graham LA, Gray SH, Urist MM, Hawn MT. Descriptive operative reports: teaching, learning, and milestones to safe surgery. J Surg Educ. 2011;68:452-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Sneddon F, Fritsch N, Mackenzie S, Skipsey D, Rankin IA. Orthopaedic surgical documentation: pre-templated operation notes significantly improve documentation of surgical procedures. J Orthop Surg Res. 2023;18:48. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Makary MA, Holzmueller CG, Thompson D, Rowen L, Heitmiller ES, Maley WR, Black JH, Stegner K, Freischlag JA, Ulatowski JA, Pronovost PJ. Operating room briefings: working on the same page. Jt Comm J Qual Patient Saf. 2006;32:351-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Singh M, Pal TR. Voice recognition technology implementation in surgical pathology: advantages and limitations. Arch Pathol Lab Med. 2011;135:1476-1481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Zahid MJ, Ijaz A, Hidayat W, Jan MA, Rafi H, Nawaz H, Khan H. Assessing Adherence to Royal College of Surgeons Guidelines: A Closed-Loop Audit of Operation Notes in a Tertiary Healthcare Unit. Cureus. 2023;15:e45743. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Hersh WR, Weiner MG, Embi PJ, Logan JR, Payne PR, Bernstam EV, Lehmann HP, Hripcsak G, Hartzog TH, Cimino JJ, Saltz JH. Caveats for the use of operational electronic health record data in comparative effectiveness research. Med Care. 2013;51:S30-S37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 376] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 19. | Stogryn S, Hardy KM, Abou-Setta AM, Clouston KM, Metcalfe J, Vergis AS. Advancement in the quality of operative documentation: A systematic review and meta-analysis of synoptic versus narrative operative reporting. Am J Surg. 2019;218:624-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 20. | Park J, Pillarisetty VG, Brennan MF, Jarnagin WR, D'Angelica MI, Dematteo RP, G Coit D, Janakos M, Allen PJ. Electronic synoptic operative reporting: assessing the reliability and completeness of synoptic reports for pancreatic resection. J Am Coll Surg. 2010;211:308-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 21. | van de Graaf FW, Lange MM, Spakman JI, van Grevenstein WMU, Lips D, de Graaf EJR, Menon AG, Lange JF. Comparison of Systematic Video Documentation With Narrative Operative Report in Colorectal Cancer Surgery. JAMA Surg. 2019;154:381-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |