INTRODUCTION
In recent years, the field of orthopedic surgery has witnessed an unprecedented period of advancement and growth. Fluoroscopy is utilized in orthopedic surgery most commonly for assessment of skeletal anatomy during fracture reduction and placement of implants. Because of allowing inexpensive and readily available real-time X-ray imaging in the operating theatre, fluoroscopy becomes an indispensable tool in modern orthopedic surgery with a multitude of indications for use including assessment of fracture and dislocation reduction, positioning of implants, and localization of anatomy[1,2]. Surgeons use fluoroscopic X-ray images acquired during surgery with a mobile fluoroscopic C-arm to determine the relative position and orientation of bones, implants, and surgical instruments. However, several important limitations of X-ray fluoroscopy such as a narrow field of view, limited resolution and contrast, and geometric distortion require the surgeon to frequently acquire images of the surgical situation, precise evaluation, and measuring across images when they place long implants in need. Recent studies have shown that intraoperative C-arm images and postoperative plain film radiographs appear to be 8.2% different, and reflect fracture gap, rotation, and angulation may vary between images[3]. The main reason is attributed to insufficient intraoperative visualization of the entire limb axis[4].
To address these limitations, a technique was introduced to create panoramic X-ray images by merging multiple single X-ray images that have restricted viewing areas[5-7]. Image stitching is a process of overlapping and processing two or more images captured from different perspectives and at different time points, thereby generating a broader panoramic image. In image adjustment and optimization, modeling will be conducted on some areas of adjacent or consecutive images to determine the rationality of the merging position[8]. For intraoperative X-ray stitching, one method was proposed by Wang et al[9] using a standard mobile C-arm. We are confident that the development of panoramic X-ray imaging holds significant promise for integration into daily surgical practices. This technology will enable surgeons to confirm and verify the quality of their procedures in orthopedic and trauma surgeries while reducing radiation exposure. It seems necessary to illustrate the advantages of intraoperative X-ray image stitching having advantages in longer and more complex bone fixation surgeries.
The aim of this research was to assess the use of combined parallax-free panoramic X-ray imaging during surgical procedures by utilizing a mobile C-arm with minimally invasive plate osteosynthesis (MIPO) for managing proximal humeral shaft fractures.
MATERIALS AND METHODS
Patients
All patients were treated at the Department of Trauma and Orthopedics Surgery, First Affiliated Hospital of Wannan Medical College, Yijishan Hospital, and this retrospective study was conducted in accordance with the ethical standards of the 1964 Declaration of Helsinki. Protocols were followed and the publication of patients’ details was approved by the Hospital Ethical Committee. Written informed consent for the publication of their medical details was obtained from patients or their relatives.
We included all 17 (12 males, 5 females) adult patients who had displaced proximal humeral shaft fractures treated using the MIPO technique from July 2019 to March 2021. The indication for operating on these fractures was all displaced fractures of the humerus shaft. All fractures mainly involved the proximal and middle humeral shaft. All patients with open injuries, pre-existing nerve injuries, multiple injuries, or pathological fractures were excluded.
Imaging information
All patients should have plain radiographic anteroposterior and lateral views preoperatively for a proximal humeral shaft fracture. The X-ray images of this study were acquired using the PHILIPS mobile C-arm system (BVlibra) intraoperatively, including image work systems and workstations with image processing software (CANON, Photo Stitch 3.l CH) installed.
Surgical procedures and postoperative management
Under general anesthesia, the patient was placed in a beach chair position and the operation was performed under the control of a C-arm machine. A 5-cm incision was made at the deltoid-pectoralis groove at the proximal end to expose the anterolateral aspect of the greater tuberosity of the humerus. Another 5-cm incision was made on the lateral side of the humeral shaft at the distal end. The brachialis muscle was bluntly dissected along the lateral side of the biceps. When the outer layer of the periosteum was reached, the muscles were bluntly separated to form a submuscular tunnel. The proximal bone fragment was placed in an abducted and internally rotated position. Then, the distal bone fragment was adjusted to achieve satisfactory alignment. A locking compression plate (LCP) (titanium; thickness: 4.2 mm; width: 12 mm; length: 105-231 mm; China Double Engine Medical Devices Co., Ltd.) was inserted from the distal to the proximal end. The proximal end of the plate was temporarily fixed to the anterolateral aspect of the greater tuberosity with Kirschner wires, and the distal end was fixed with screws. According to previous reports[10], the surgical humerus was tracked under panoramic X-ray imaging without parallax distortion to restore its length and coronal alignment.
First, the C-arm was positioned to take the first X-ray. We positioned the C-arm such that the X-ray image included the area of interest (Figure 1A and B). Second, we moved the C-arm parallel along the humeral shaft fractures into a new viewing position. Next, the surgeon, who is well-versed in bone geometries, is aware of the direction in which they want to expand the first X-ray by adding the subsequent one (Figure 1C-F). During the examination process, the system determines the overall image height (calculated as the difference between the starting and ending positions of the detector) and estimates the number of exposures required to minimize overlap between consecutive images. The stitching algorithm in the Photo Stitch 3.l CH software requires an overlapping region between two images to ensure proper alignment. This overlap is achieved by adjusting horizontal and vertical shifts using various values. For each pair of shift values, a cross-correlation coefficient is calculated, with the highest value indicating the smallest difference between overlapping regions, thus achieving the optimal alignment. Once the best alignment is identified, the two images are combined. The algorithm requires an overlapping region of 3-5 cm to achieve a balance between maximizing the cross-correlation and minimizing patient radiation exposure. Using this method, 2-4 exposures were taken, and the corresponding images were merged. The resulting parallax-free panoramic X-ray image demonstrates high accuracy and excellent visual quality. Ultimately, this technique produces a parallax-free panoramic X-ray image that is both precise and visually superior (Figure 2). The anterior-posterior and lateral views of the panoramic X-ray image should both be checked, and rotary restoration should be confirmed. The proximal end was secured using four or five 3.5-mm locking screws, while the distal portion was fastened with two or three 3.5-mm locking screws, in accordance with prior studies[11,12]. The incision was closed layer by layer with sutures. After the operation, the patient was able to engage in unrestricted, voluntary shoulder movements without the need for any additional external stabilization equipment.
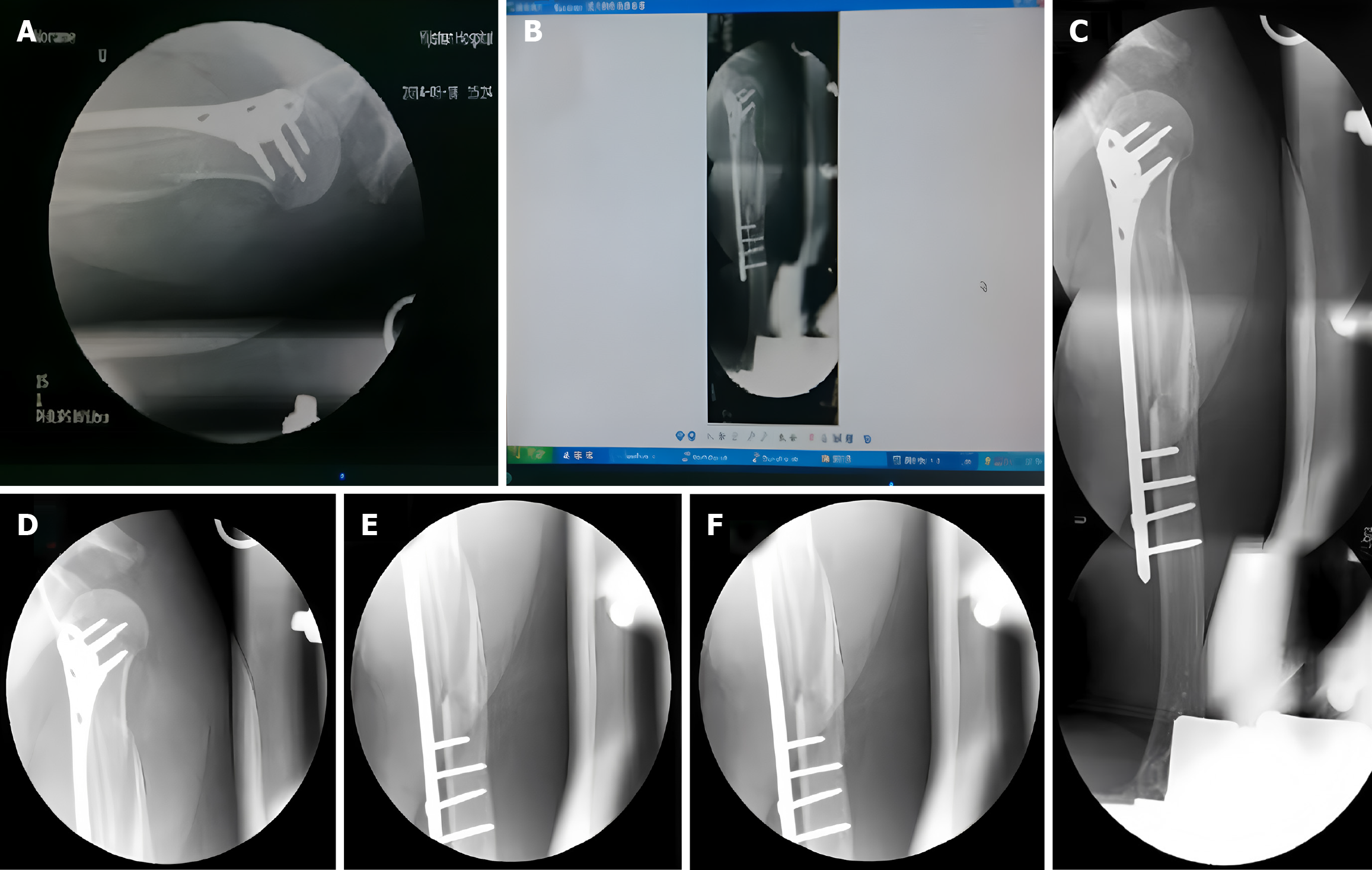
Figure 1 X-ray images.
A: The initial X-ray image taken by the C-arm; B: The professionally spliced X-ray film; C: The magnified X-ray film; D: C-arm fluoroscopy of the proximal humerus; E: C-arm fluoroscopy of the middle segment of the humerus; F: C-arm fluoroscopy of the distal humerus.
Figure 2 Preoperative, intraoperative, and postoperative X-ray images.
A: Anteroposterior view of preoperative fluoroscopy; B: Lateral radiograph taken before the operation; C: Anteroposterior view during intraoperative fluoroscopy; D: Lateral fluoroscopy during the operation; E: Postoperative anteroposterior radiograph; F: Lateral radiograph after surgery; G: Postoperative multi-angle perspective; H: Postoperative multi-angle perspective again.
Outcome measures and data collection
This study mainly evaluated the operation time and fluoroscopy time during the operation, the incidence of postoperative complications, and the Constant-Murley score of the shoulder joint. The patients consented to routine follow-up examinations after surgery, scheduled at intervals of 1, 3, 6, and 12 months. Radiological techniques were employed to assess the position of the bone-plate and the progress of fracture healing. The functional results were measured using the Constant-Murley shoulder evaluation method[13]. The scoring system consists of four components: Pain, Power, Daily Living Activities, and Movement Range. In the subsequent stage of this research, as the sample size increases, comparisons will be made with the standard method.
RESULTS
Operative time was 73 minutes on average (range: 49-95 minutes). The average fluoroscopy time was 57 seconds (range: 36-98 seconds). No intraoperative complications occurred. The fractures healed on average at 16.9 weeks (range: 15-23 weeks). Hardware was removed in one patient due to lateral impingement and in nine for social and personal reasons. The Constant-Murley score was assessed by three surgeons, with the mean calculated for statistical analysis. In terms of movement, the median range was 150° for flexion (range: 120°-160°); 45° for extension (range: 35°-50°); 55° for internal rotation (range: 45°-70°); 65° for external rotation (range: 50°-85°); and 135° for abduction (range: 120°-170°). Regarding pain, 16 patients had none and 1 reported mild pain. The mean Constant-Murley score was 89.5 (range: 75-100) points. No instances of deep-wound infections, nerve damage, or vascular injuries were noted. None of the patients experienced subacromial impingement three months post-procedure. There were no cases of implant loosening or fracture. The alignment was deemed satisfactory from both anteroposterior and lateral perspectives. In the current standard methods, the mean operating time and radiation time were 102 (range: 72-127) minutes. The average fluoroscopy time was 97 (range: 72-139) seconds. The average Constant-Murley score was 80.7 (range: 69-86) points. Subsequently, as the sample size further expands, we will conduct statistical comparisons.
DISCUSSION
In this study, we described the use of parallax-free panoramic X-ray imaging during surgery combined with MIPO with the LCP as a novel method for treating proximal humeral shaft fractures. In all cases, we made two small incisions away from the fractures to prevent damage to the periosteal blood supply and soft tissue compromise. In the process of surgery, parallax-free panoramic X-ray imaging during surgery could timely provide an assessment of closed reduction and internal fixation of fractures and revise the inappropriate places. Moreover, MIPO could preserve the osteogenic hematoma of the fractures and the nutritional arteries of the bone while preventing iatrogenic soft tissue damage[14]. The combination of parallax-free panoramic X-ray imaging during surgery with MIPO in our series is a minimally invasive approach that maximizes tissue preservation and provides reliable stability for fractures. Clinical outcomes were satisfactory, and we gained experience using this technique.
Proximal humeral shaft fractures account for 4%-5% of all fractures and commonly appear in upper-limb injuries[15]. The occurrence of these issues is increasing due to the aging population and a growing number of traffic accidents[16,17]. Around 80% of proximal humerus fractures involve no displacement or only slight misalignment and are typically managed successfully without surgery[18]. A broader population-based study involving 1027 proximal humerus fractures revealed that most injuries occurred in active adults over the age of 60. The highest incidence was observed among women aged 80 to 89[19]. Precise evaluation of fractures, patient adherence, medical comorbidities, and the duration from injury to treatment are key elements that significantly influence the outcome[20]. Many factors must be considered when developing a treatment plan[20,21]. Fractures that cannot be successfully reduced, are unstable, or involve comminution generally require surgical intervention to achieve proper alignment and provide the stability necessary for early shoulder mobility. These types of fractures present a considerable challenge for orthopedic surgeons. The LCP provides angular stability and has been employed in the surgical management of proximal humeral fractures for several years[22]. It combines the principles of conventional plate fixation with locking screws. The locked interface also provides fixed stability, which helps to prevent subsidence in the metaphyseal areas[23-25]. Traditionally, an open reduction method has been employed to ensure precise alignment and prevent neurovascular injury. Nevertheless, extensive soft-tissue dissection during this procedure may lead to inadvertent damage to the radial nerve. Additionally, there is a growing risk of nonunion in such cases. To address these challenges, MIPO was introduced as a technique for achieving biological fixation. This approach not only enhances the rate of bone union but also diminishes complications related to conventional plating, such as infections and iatrogenic radial nerve palsy[26-28].
In our research, with an average postoperative follow-up duration of 13.5 months, we discovered that MIPO is a safe and effective method for treating humeral shaft fractures. The results were favorable, featuring successful fracture healing, fewer complications, and excellent recovery of shoulder function as indicated by the Constant-Murley score. The standard method is prone to increasing errors when assessing the perspective angle and the quality of reduction during the operation, which may lead to incorrect judgments by the surgeon. In addition, it is greatly influenced by the patient's position and posture. Our improved method provides imaging results that are more in line with the anatomy of the humerus and surgical operations. It can also appropriately evaluate whether there is soft tissue entrapment at the fracture end and more intuitively observe the reduction situation of the fracture end. Our study also showed that shorter mean radiation time and time to union, lower incidence of complications, and more excellent Constant-Murley score were observed in dealing with these patients compared with those in a previous study[29]. Traditional fluoroscopy overlooks the influence that variations in the fluoroscopic angle exert on intraoperative decision-making. The improved technique allows for a more distinct and precise observation of the current surgical status during the implantation of surgical plates and screws, and to a certain extent, mitigates the radiation dosage brought to both the doctor and the patient by multiple fluoroscopies. We think that this better clinical outcome results from parallax-free panoramic X-ray imaging during surgery. Fluoroscopy is utilized in orthopedic surgery most commonly for assessment of MIPO during fracture reduction and placement of implants. However, X-ray images acquired by mobile C-arms have a narrow field of view and often cannot visualize the entire bone structure of interest within a single X-ray image, especially in long bone fixation surgery such as humeral shaft fractures. We present a novel method to generate parallax-free panoramic X-ray images during surgery by enabling the mobile C-arm to rotate around its X-ray source center, relative to the patient’s table during MIPO surgery. The incidence of postoperative complications and the rate of nonunion after open reduction of fractures are approximately 13.6% and 10%, respectively. As a result, we can quickly and accurately detect surgical deficiencies and timely correction. At the same time, a complete understanding of the fractured humeral shaft and surrounding anatomy helps to complete the surgery quickly and effectively. Thus, parallax-free panoramic X-ray imaging during surgery combined with MIPO for treating humeral shaft fractures could significantly reduce operative morbidity and also lower the rates of intra- and postoperative complications.
The limitations of the present study were that: (1) This study had a retrospective design and the comparisons were made with data from previous studies rather than real-world clinical practice data from the same center. To further support these results, high-quality randomized controlled trials with larger sample sizes are needed; and (2) The mean follow-up duration was only 13.5 months, representing a relatively short assessment timeframe. Consequently, most cases of posttraumatic arthritis would likely not have emerged at this point. For future research, it would be beneficial to conduct studies with a larger participant pool, incorporating a wider variety of fracture types and extended follow-up intervals.