Published online Mar 18, 2025. doi: 10.5312/wjo.v16.i3.100481
Revised: December 8, 2024
Accepted: February 19, 2025
Published online: March 18, 2025
Processing time: 206 Days and 12.4 Hours
Clinical studies using Trabecular Titanium™ acetabular cups have shown promising short and medium-term results. This material, due to its macro and micro surface roughness, provides a substrate for osseointegration and enhances implant stability. However, there is a lack of evidence in the literature on the use of this material in patients with femoral neck fracture.
To evaluate the short-term clinical-functional and radiographic outcomes in patients with femoral neck fractures undergoing total hip arthroplasty (THA) with Trabecular Titanium™ acetabular cup implants.
The study included 104 patients with medial femoral neck fractures who underwent THA between January 2020 and December 2020 with the Delta TT acetabular cup (Lima Corporate, Villanova di San Daniele del Friuli, Italy). The mean age of the patients was 69.57 ± 10.16 years (range: 36-85 years). The follow-up period ranged from a minimum of 3 to a maximum of 4 years. Three questionnaires (Harris Hip Score, Oxford Hip Score, and EQ5D) were administered along with radiographic evaluations. Statistical methods included the Student's t-test and one-way analysis of variance for comparisons (with significance set at 0.05), and the Kaplan-Meier curve for prosthetic implant survival.
The mean follow-up was 41.5 months. The Harris Hip Score (HHS) showed a mean increase of 2.74 points (mean HHS 88.52 at 6 months postoperatively and mean HHS 91.26 at the last follow-up) with statistical significance. Similarly, the Oxford Hip Score demonstrated a statistically significant difference between follow-up groups. However, the EQ5D did not show statistically significant differences among the three groups (preoperative, 6-month follow-up, and last follow-up). Revision surgery was required in 6 patients. According to Moore's criteria, 96% of the acetabular components were radiographically stable and well-integrated at the last follow-up. The Kaplan-Meier curve showed a 96% survival rate.
The clinical and radiographic results obtained in the short to medium term confirm the excellent performance of the Delta TT acetabular cup in terms of osseointegration, providing an optimal solution both for young patients with high functional recovery demands and for fragile patients requiring optimal stability of the acetabular component to reduce the risk of implant failure.
Core Tip: This retrospective study assessed the outcomes of 104 patients with medial femoral neck fractures treated with total hip arthroplasty using Trabecular Titanium™ acetabular cups. With an average follow-up of 41.5 months, the results showed significant improvements in Harris Hip and Oxford Hip Scores, indicating successful clinical outcomes. The EQ5D score showed no significant differences. Radiographic evaluations revealed 96% implant stability, and the Kaplan-Meier curve indicated a 96% survival rate. The Delta TT acetabular cup demonstrated excellent performance in osseointegration and stability, making it suitable for both young, active patients and older, fragile individuals.
- Citation: Jannelli E, Boggio E, Castelli A, Pasta G, Grassi FA, Mosconi M. Trabecular titanium acetabular cup in patients with medial femoral neck fracture: Survivorship analysis and clinical and radiological outcomes. World J Orthop 2025; 16(3): 100481
- URL: https://www.wjgnet.com/2218-5836/full/v16/i3/100481.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i3.100481
Hip arthroplasty, or total hip arthroplasty (THA), is one of the most frequently performed and successful procedures in orthopedic surgery[1]. It is indicated for osteoarthritis, rheumatoid arthritis, osteonecrosis, tumors, past pediatric conditions affecting the hip joint, and femoral fractures. These fractures are increasingly common, especially in the elderly population, although they can occur at any age. Aging is associated with changes in biomechanics and bone strength, increasing the risk of fragility fractures due to falls from a standing position or low-intensity trauma[2].
Despite excellent clinical outcomes and implant survival rates, acetabular component mobilization remains the most frequent cause of implant failure and revision[3,4]. Poor bone quality in elderly patients and underlying conditions like osteoporosis negatively impact long-term clinical results. To reduce the risk of aseptic loosening, there has been continuous evolution in prosthetic design and materials in recent years.
Trabecular Titanium™, in particular, is a titanium alloy material with continuity between the core and the external porous structure, mimicking bone structure to optimize mechanical strength and ensure primary stability and osseointegration. The entire hemispherical profile with a 1 mm press-fit ensures tight initial contact with the vital native bone[5-7]. The macro-roughness of the cup supports high friction, while the micro-roughness promotes adhesion, proliferation, and differentiation of osteogenic cells, which are crucial for anchorage.
Trabecular Titanium™ provides a scaffold for cell colonization and bone tissue vascularization. Optimal porosity and pore size enhance vascularization and mineralization, promoting the formation of new bone tissue[8]. Stem cells (hASCs) grown on Trabecular Titanium™ scaffolds have been shown to adhere, proliferate, and differentiate into osteoblasts even in the absence of osteogenic factors[9,10].
The aim of this retrospective study was to evaluate the short-term clinical-functional and radiographic outcomes in patients with femoral neck fractures undergoing THA with Trabecular Titanium™ acetabular cup implants.
From January 2020 to December 2020, 116 patients with medial femoral neck fractures underwent THA using Delta–TT cups® (Lima Corporate, Villanova di San Daniele del Friuli, Italy). All surgeries were performed using a posterolateral approach with the patients in the lateral decubitus position, executed by two senior surgeons. The acetabulum was reamed up by 1 mm (line-to-line fixation) to accommodate the surface interference of the Delta-TT cup. The acetabular component was impacted with abduction and anteversion angles adapted to the patient’s anatomy. All femoral heads were made of BIOLOX® Delta ceramic (CeramTec GmbH, Plochingen, Germany), with sizes ranging from 28 to 36 mm. Cups were paired with the H-MAX stem (Lima Corporate) in all cases. Among these, 30 stems were cemented (29%) and 74 were uncemented (71%).
The inclusion criteria for the study were: Presence of a medial femoral neck fracture, age ≤ 85 years, fewer than three comorbidities, a Nottingham score ≤ 4 (predicted 30-day postoperative mortality of 6.2%), no use of walking aids before the traumatic event, and completion of the follow-up process by January 31, 2024. Of the 116 patients, 6 were excluded due to being lost to follow-up, and 6 because they had passed away.
The sample consisted of 79 female (84%) and 25 male (16%) patients, aged between 36 and 85 years, with a mean age of 69.57 years (± 10.16 SD). The follow-up period ranged from a minimum of 37 months to a maximum of 48 months (mean follow-up of 41.5 months).
The study population had a mean body mass index (BMI) of 23.38 (range: 19.07–43.7). A total of 11.4% of patients smoked more than 10 cigarettes per day, and no patients were identified as alcohol abusers. Cardiovascular comorbidities were present in 71 patients (68.2%), of whom 21 patients (30%) were on oral anticoagulant therapy prior to surgery. Diabetes was identified as the second most common comorbidity, affecting 35 patients (33.6%). All patients underwent antithromboembolic prophylaxis with low molecular-weight heparin.
Hemoglobin levels were assessed on the first and third postoperative days. On the second postoperative day, before the initiation of ambulatory physiotherapy, pain was evaluated using the Numeric Rating Scale (NRS).
All patients were clinically and radiographically evaluated preoperatively and at 1, 3, 6, and 12 months postoperatively, with annual check-ups thereafter. Three clinical questionnaires were administered: The Harris Hip Score (HHS) at 6 months and the last follow-up, the Oxford Hip Score (OHS), and the EQ-5D-5 L preoperatively, at 6 months, and at the last follow-up. Each patient also underwent a weight-bearing anteroposterior pelvis X-ray at the last follow-up to assess the correct positioning of the prosthesis, the osseointegration process of the bone-implant system, and any present alterations. The Engh Grading Scale and Moore's criteria were chosen as the main parameters for evaluating osseointegration[11,12].
With regard to our rehabilitation protocol, on the first postoperative day, all patients underwent an anteroposterior and axial X-ray of the hip. Following the X-ray, if no complications related to implant positioning were identified, patients were referred to a specialist in physical and rehabilitation medicine who initiated the rehabilitation protocol.
The protocol involved assuming an upright position and beginning weight-bearing ambulation as tolerated with the assistance of a walker starting from the second postoperative day. Additionally, isometric strengthening exercises for the quadriceps and gluteal muscles, along with range of motion exercises in bed, were performed. From the fifth postoperative day, patients were trained to ambulate using crutches and were provided with guidance on positions to avoid, such as flexion and internal rotation, to minimize the risk of dislocation.
The analysis of data extracted from the aforementioned questionnaires was performed using a one-tailed Student's t-test for independent variables for the HHS. For three-group comparisons involving the OHS and the EQ-5D-5 L, the one-way analysis of variance test followed by the Tukey HSD post hoc analysis (beta) was applied. In all cases, a significance level of 0.05 was considered. Associations between variables were evaluated using P-values to determine the statistical significance of the results (P < 0.05).
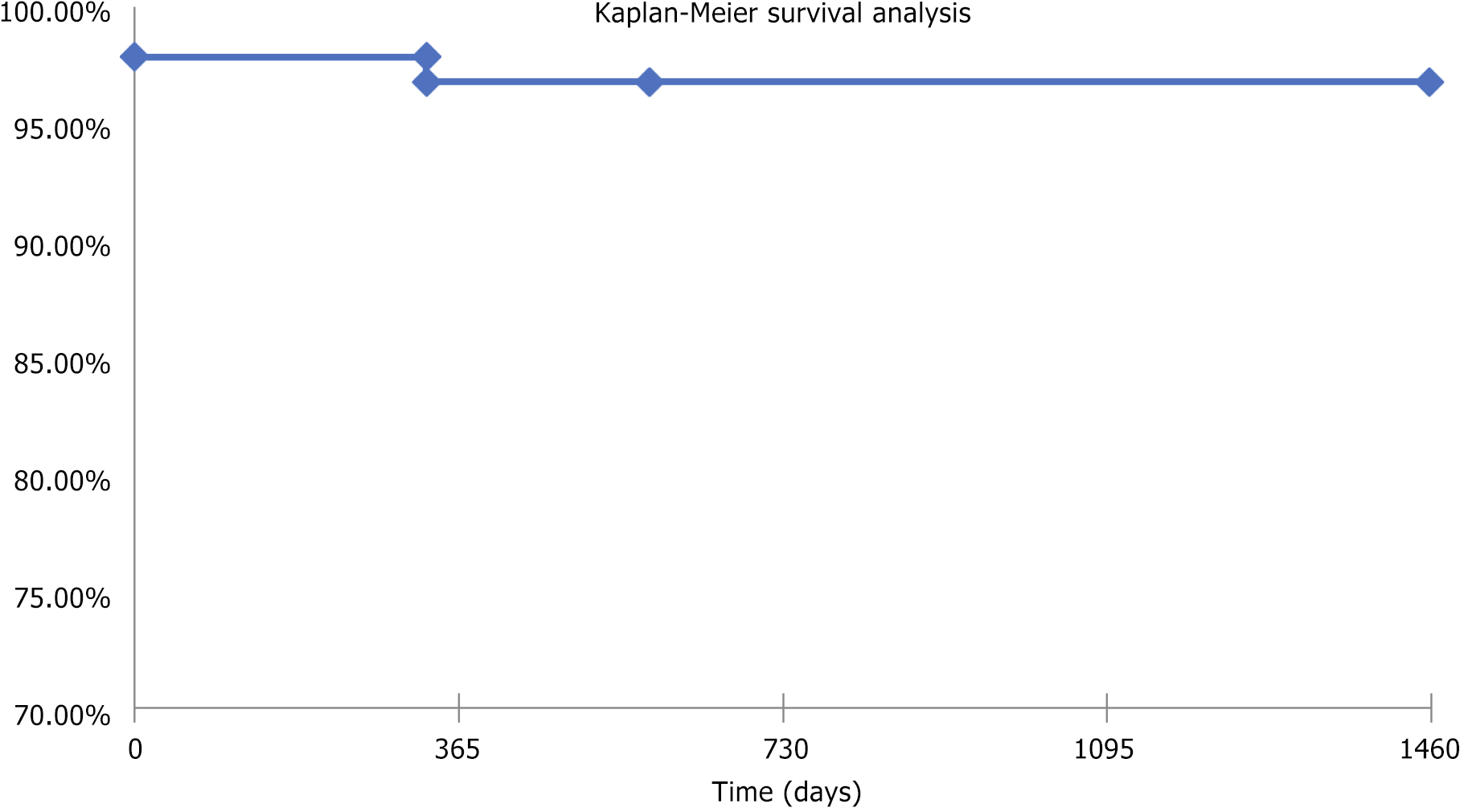
Finally, prosthetic implant survival was studied using the Kaplan-Meier curve, considering revisions of any prosthetic component as the endpoint and patient loss to follow-up or death as censures. Two specific complications required revision surgery: One periprosthetic fracture necessitating stem replacement and one posterior dislocation treated with acetabular insert replacement. Approval of the Institutional Review Board of the IRCCS Policlinico San Matteo in Pavia was obtained for this study, and all subjects provided informed consent prior to participation.
Analysis of operative times revealed an average procedure duration of 77 minutes (range: 65–95 minutes). No postoperative complications related to bleeding were observed that required reoperation for hematoma evacuation or embolization. The mean hemoglobin level on the first postoperative day was 9.7 g/dL (range: 8.8–11), while on the third postoperative day, the mean value decreased to 9.2 g/dL (range: 7.7–10.2). Blood transfusion was required in 14 patients (13.4%). The mean NRS score recorded on the second postoperative day, prior to the initiation of deambulation, was 5.5/10 (range: 4–7).
The average HHS at 6 months post-surgery was 88.52 points ± 10.45. At the last follow-up, the average HHS increased to 91.26 points ± 11.23, showing a statistically significant improvement of 2.74 points (P < 0.05).
The average OHS was 46.50 points ± 2.64 preoperatively, six months after surgery, the average OHS decreased to 41.81 points ± 5.04 (P < 0.05). At last follow-up OHS showed a statistically significant improvement at 43.97 points ± 5.06 (P < 0.05).
The preoperative average EQ-5D-5 L score was 0.90 ± 0.168. Six months post-surgery, the average score dropped to 0.65 ± 0.22, and at the last follow-up, it improved to 0.77 ± 0.22. However, the differences between these groups were not statistically significant (P > 0.05) (Table 1).
| Mean | Preop | 6 months | LFU | P value |
| HHS | X | 88.52 | 91.26 | < 0.05 |
| OHS | 46.50 | 41.81 | 43.97 | < 0.05 |
| EQ5D5 L | 0.90 | 0.65 | 0.77 | > 0.05 |
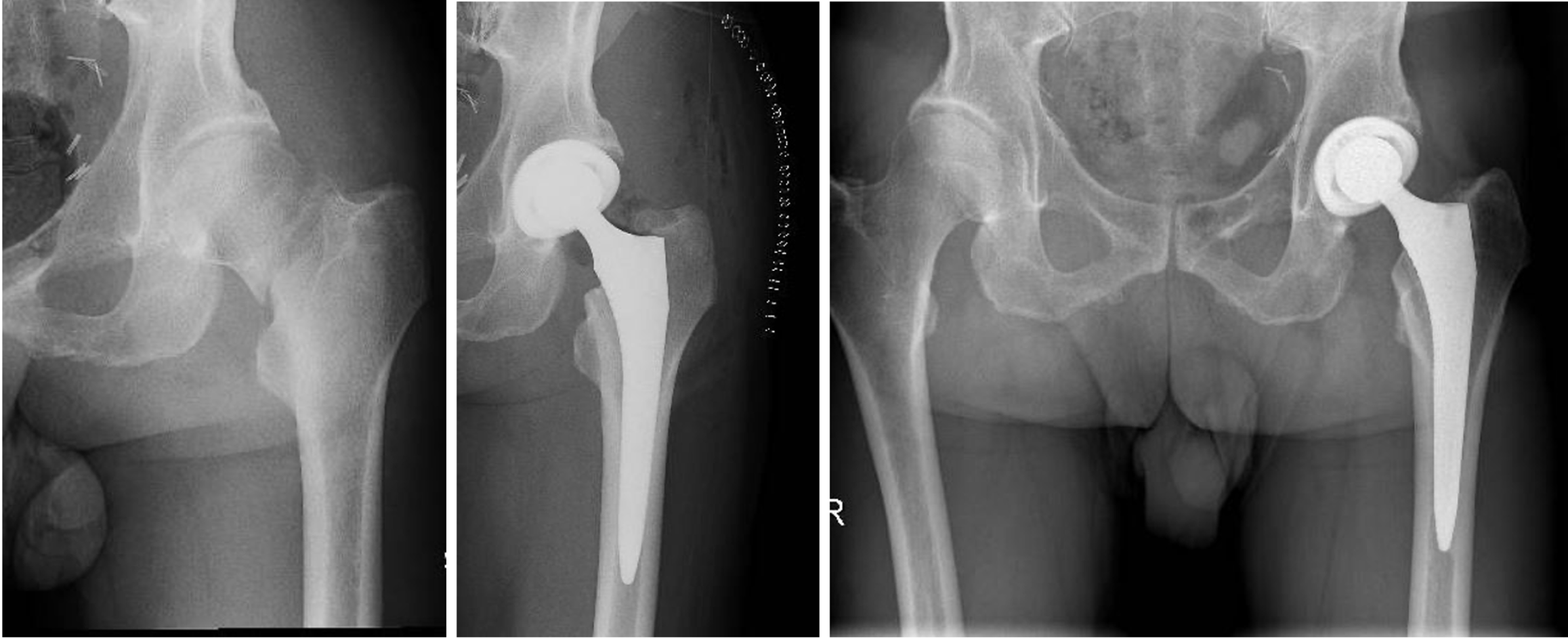
Using the Engh Grading Scale, the average score was 21.91 points. According to Moore’s criteria[11], 100% of the cups were radiographically stable at the last follow-up, showing evident signs of bone remodeling and integration, without any radiolucent lines, sclerotic areas or periprosthetic osteolysis (Figure 1).
The Kaplan-Meier analysis indicated a 96.8% implant survival rate, with a 95% confidence interval (Figure 2). These results indicate significant improvements in clinical scores postoperatively, high rates of radiographic integration, and excellent overall implant survival.
Twenty percent of patients with displaced intracapsular fractured neck of femur are mobile and independent. Squires and Bannister[13], in 1999, showed that these patients have a vastly superior functional outcome at 3 ± 4 years if treated with THA rather than hemiarthroplasty.
In a systematic review by Ramadanov et al[14], comparing treatments for medial femoral neck fractures using cannulated screws, hemiarthroplasty, and THA, the findings were consistent with existing meta-analyses. Although many studies suggest that THA is superior in terms of functional outcomes and quality of life, others report little difference between the two. Cannulated screws and dynamic hip screw fixation are associated with higher reoperation rates compared to prosthetic procedures (HA and THA).
When selecting materials, key factors to consider include biocompatibility, porosity, and elasticity. Regarding porosity, the studies by Karageorgiou et al[15] and Frosch et al[16] demonstrated that optimal bone infiltration and osseointegration occur with pore sizes between 150–600 μm. Additionally, the porosity percentage must strike a balance, allowing sufficient bone growth without compromising the material's mechanical properties, as highlighted by Fujibayashi et al[17].
Another critical consideration is the nature of the pores: They should be open, interconnected, and irregular to ensure complete material permeability and promote perfusion, which is essential for initiating bone growth. Trabecular titanium features an open porosity of 65% and an average pore size of 640 μm. These characteristics ensure a low modulus of elasticity without reducing the material's strength, which remains high due to the use of 3D-printing additive manufacturing techniques. Unlike porous coatings, which literature associates with the risk of titanium particle delamination[18], 3D-printed constructs offer superior durability and mechanical stability.
Current literature offers a limited number of publications regarding the clinical-functional evaluation of patients undergoing THA for medial femoral neck fractures using Trabecular Titanium™ cups (Figure 3). However, numerous studies have reported short and medium-term results of various uncemented acetabular cups.
Squires and Bannister[13] showed a modified HHS of 91 after THA on displaced femoral neck fracture, with good stability of the implants at 4 year follow-up. These results are in line with our study considering the last follow-up. In a RCTS of 2019[19] the authors reported an HHS of 76 ± 15 at 2 years follow-up, with a progressive improvement observed over time, furthermore the authors described an Eq5d value of 0.66 ± 0.27. Our results appear to improve those reported by Chammout et al[19], although we must consider that the population of this study was composed of only octogenarians.
Clinical studies using Trabecular Titanium™ acetabular cups have shown promising short and medium-term results. Trabecular Titanium™ has an elastic modulus similar to that of native bone, significantly lower than other available materials with highly porous hexagonal structures. This characteristic benefits bone remodeling and the subsequent osseointegration of the prosthesis.
Perticarini et al[20], in a study on THA for osteoarthritis, dysplasia, and revisions using a trabecular titanium acetabular component, showed excellent clinical and radiographic results at medium-term with a 5-year survival rate of 99.3%, and a significant improvement in quality of life and functional status.
Naziri et al[21] reported no cases of cup mobilization or radiolucent lines in 252 patients using highly porous titanium cups with a minimum follow-up of 3 years.
In our study, we observed excellent short-term clinical and radiographic results with good quality of life and return to pre-fracture functional status, and an implant survival rate of 96.8% at 4 years.
From the analysis of clinical data obtained through PROMs, a reduction in scores at the 6-month follow-up is observed compared to the preoperative evaluation. However, there is a clear trend of improvement between the 6-month scores and those at the last follow-up.
A study by Cacciola et al[22] on 523 revision surgeries highlighted a 93.4% survival rate for Trabecular Titanium™ cups in patients with acetabular bone defects, showing good clinical results with a complication rate comparable to or lower than those reported with other implants.
Tamaki et al[18] compared clinical and radiographic outcomes of THA using Trabecular Titanium™ cups and hydroxyapatite-coated titanium cups. The clinical results were excellent, although radiographic follow-ups at 3, 6, and 12 months for Trabecular Titanium™ cups showed radiolucent lines in zone 2, in 3%, 5%, and 5% of cases, respectively[24]. Moore et al[11] attribute the formation of radiolucent lines in zone 2 to stress shielding due to reduced load in the apical acetabular region, which occurs with good superolateral and inferomedial osseointegration. Thus, the appearance of radiolucent lines in zone 2 does not necessarily indicate a poor outcome.
In our study, all cups showed excellent primary stability and good osseointegration despite poor bone quality, highlighting that the two revision events were due to diaphyseal fracture and insert change rather than acetabular component mobilization. Radiographic analysis revealed no radiolucent lines or areas of periprosthetic osteolysis, supporting that Delta TT® cups are designed to favor physiological load distribution, minimizing stress shielding and bone resorption.
Yoshioka et al[25] also found significant functional recovery and pain relief in all cases with no differences in clinical results between the groups using the Japanese Orthopedic Association (JOA) score. The average JOA score improved from 48.3 ± 12.4 SD (range 14–75) preoperatively to 92.0 ± 10.3 SD (range 63–100) at the last follow-up in the Titanium group and from 49.3 ± 11.7 SD (range 14–75) to 91.7 ± 10.8 SD (range 46–100) in the Trident group. No differences were observed in terms of clinical results. Significant functional recovery and pain relief were recorded in all cases.
The goal of our study was to evaluate clinical improvement or at least a return to the pre-trauma health state, considering the advanced age at the time of surgery and the impact of the traumatic event on elderly patients.
From the analysis of the clinical data obtained through PROMs, a reduction in scores was observed at the 6-month follow-up compared to the preoperative evaluation. However, there was a noticeable trend of improvement between the scores at 6 months and those at the last follow-up.
To further characterize the results, it is important to highlight that the population in our study had an average BMI of 23.38. Our findings, therefore, corroborate those of previous studies[26] demonstrating that a higher BMI negatively impacts the outcomes of THA.
Additionally, the use of low-molecular-weight heparin proved to be both effective and safe in preventing thromboembolic events, as supported by a recent study[27]. Analyzing the complications, we reported a case of periprosthetic fracture that required femoral stem replacement, and a case of dislocation that required insert replacement. A recent paper in 2024[28] shows that patients with osteoporosis are at higher risk for periprosthetic femoral fractures and aseptic loosening following THA. The considerable importance of dual-energy X-ray absorptiometry (DEXA) scanning in identifying patients with severe osteoporosis is well known, but this study also emphasized the importance of additional preventive measures in the early identification of the condition. This factor is crucial because there is a high prevalence of undertreatment of osteoporosis in patients undergoing THA, with one study showing that 73% of osteoporosis patients were not diagnosed until the preoperative DEXA scan[29]. Moreover, in another 2019 study, the authors demonstrated that, although 25% of patients met the criteria for pharmacological treatment, only 5% received such medications in the perioperative period[30]. Therefore, raising awareness about the early identification of patients with osteoporosis is vital, especially since appropriate treatment with bisphosphonates can significantly reduce the risk of revision and increase implant survival in the osteoporosis population[31].
The clinical results obtained in our study are encouraging considering the population examined, primarily consisting of individuals over 65 years of age. These patients were in good osteoarticular health before the traumatic event, unlike those with hip dysplasia or severe osteoarthritis. Therefore, prosthetic replacement surgery plays a crucial role in returning patients to their previous state of well-being while minimizing the risk of subsequent complications. Trabecular Titanium™ cups combine excellent clinical results with good osseointegration. Despite their higher cost compared to other materials, their use is justified even for the elderly population, as hospitalization costs for revision surgeries are significantly higher. The lack of statistical significance observed for some scores, for example EQ-5D-5L, may also be explained by the slower functional recovery seen in elderly patients after a femoral neck fracture. Furthermore, it must be considered that these scores, although useful for assessing the well-being and perception of the patient's health status after surgery, are burdened by low sensitivity.
The present study is a retrospective study and is therefore potentially associated with selection bias; furthermore it involves a limited number of patients with a short to medium-term follow-up. Additionally, there are no preoperative clinical scores, as the evaluation relies solely on PROMs. Furthermore, there is no control group and data collection was conducted without the implementation of blinding procedures.
In our experience, the clinical and functional results obtained in a population of patients with medial femoral neck fractures suggest that the Delta TT cup (trabecular titanium) is an excellent solution not only for young patients with high functional demands but also for elderly patients. For the elderly, recovering their pre-fracture functional status is essential to minimize the risk of complications such as revisions, infections, and prolonged hospitalizations. The retrospective design, subject to potential selection biases, and the absence of a control group are the main limitations of this study. Future developments may include expanding the sample size, extending the follow-up period in order to assess the maintenance of the obtained results in the long-term, as well as using multivariate analysis to evaluate how different patient characteristics (e.g., BMI, comorbidities) may influence the outcomes.
| 1. | Knight SR, Aujla R, Biswas SP. Total Hip Arthroplasty - over 100 years of operative history. Orthop Rev (Pavia). 2011;3:e16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 123] [Cited by in RCA: 128] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 2. | Yuan H, Yu H, Zhu Y, Xiang L, Wang H. Effect of Age on the Patterns of Traumatic Femoral Fractures: Seven Years of Experience at a Regional Tertiary Hospital. Orthop Surg. 2022;14:2132-2140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Russell RD, Estrera KA, Pivec R, Mont MA, Huo MH. What's new in total hip arthroplasty. J Bone Joint Surg Am. 2013;95:1719-1725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Howard JL, Kremers HM, Loechler YA, Schleck CD, Harmsen WS, Berry DJ, Cabanela ME, Hanssen AD, Pagnano MW, Trousdale RT, Lewallen DG. Comparative survival of uncemented acetabular components following primary total hip arthroplasty. J Bone Joint Surg Am. 2011;93:1597-1604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Banerjee S, Issa K, Kapadia BH, Pivec R, Khanuja HS, Mont MA. Highly-porous metal option for primary cementless acetabular fixation. What is the evidence? HIP Int. 2013;23:509-521. [DOI] [Full Text] |
| 6. | Marin E, Pressacco M, Fusi S, Lanzutti A, Turchet S, Fedrizzi L. Characterization of grade 2 commercially pure Trabecular Titanium structures. Mater Sci Eng C Mater Biol Appl. 2013;33:2648-2656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Marin E, Fusi S, Pressacco M, Paussa L, Fedrizzi L. Characterization of cellular solids in Ti6Al4V for orthopaedic implant applications: Trabecular titanium. J Mech Behav Biomed Mater. 2010;3:373-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 83] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Sato T, Pajarinen J, Behn A, Jiang X, Lin TH, Loi F, Yao Z, Egashira K, Yang F, Goodman SB. The effect of local IL-4 delivery or CCL2 blockade on implant fixation and bone structural properties in a mouse model of wear particle induced osteolysis. J Biomed Mater Res A. 2016;104:2255-2262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Gastaldi G, Asti A, Scaffino MF, Visai L, Saino E, Cometa AM, Benazzo F. Human adipose-derived stem cells (hASCs) proliferate and differentiate in osteoblast-like cells on trabecular titanium scaffolds. J Biomed Mater Res A. 2010;94:790-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Benazzo F, Botta L, Scaffino MF, Caliogna L, Marullo M, Fusi S, Gastaldi G. Trabecular titanium can induce in vitro osteogenic differentiation of human adipose derived stem cells without osteogenic factors. J Biomed Mater Res A. 2014;102:2061-2071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Moore MS, McAuley JP, Young AM, Engh CA Sr. Radiographic signs of osseointegration in porous-coated acetabular components. Clin Orthop Relat Res. 2006;444:176-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 167] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 12. | Muir SW, Al-Ahaideb A, Huckell J, Johnson MA, Johnston DB, Beaupre LA. Radiographic assessment of uncemented total hip arthroplasty: reliability of the Engh Grading Scale. Can J Surg. 2011;54:185-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Squires B, Bannister G. Displaced intracapsular neck of femur fractures in mobile independent patients: total hip replacement or hemiarthroplasty? Injury. 1999;30:345-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 62] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Ramadanov N, Jóźwiak K, Hauptmann M, Lazaru P, Marinova-Kichikova P, Dimitrov D, Becker R. Cannulated screws versus dynamic hip screw versus hemiarthroplasty versus total hip arthroplasty in patients with displaced and non-displaced femoral neck fractures: a systematic review and frequentist network meta-analysis of 5703 patients. J Orthop Surg Res. 2023;18:625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 15. | Karageorgiou V, Kaplan D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials. 2005;26:5474-5491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4452] [Cited by in RCA: 3689] [Article Influence: 184.5] [Reference Citation Analysis (0)] |
| 16. | Frosch KH, Barvencik F, Viereck V, Lohmann CH, Dresing K, Breme J, Brunner E, Stürmer KM. Growth behavior, matrix production, and gene expression of human osteoblasts in defined cylindrical titanium channels. J Biomed Mater Res A. 2004;68:325-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 61] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Fujibayashi S, Neo M, Kim HM, Kokubo T, Nakamura T. Osteoinduction of porous bioactive titanium metal. Biomaterials. 2004;25:443-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 245] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 18. | Otsuka Y, Kojima D, Mutoh Y. Prediction of cyclic delamination lives of plasma-sprayed hydroxyapatite coating on Ti-6Al-4V substrates with considering wear and dissolutions. J Mech Behav Biomed Mater. 2016;64:113-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Chammout G, Kelly-Pettersson P, Hedbeck CJ, Stark A, Mukka S, Sköldenberg O. HOPE-Trial: Hemiarthroplasty Compared with Total Hip Arthroplasty for Displaced Femoral Neck Fractures in Octogenarians: A Randomized Controlled Trial. JB JS Open Access. 2019;4:e0059. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 20. | Perticarini L, Zanon G, Rossi SM, Benazzo FM. Clinical and radiographic outcomes of a trabecular titanium™ acetabular component in hip arthroplasty: results at minimum 5 years follow-up. BMC Musculoskelet Disord. 2015;16:375. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Naziri Q, Issa K, Pivec R, Harwin SF, Delanois RE, Mont MA. Excellent results of primary THA using a highly porous titanium cup. Orthopedics. 2013;36:e390-e394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Cacciola G, Giustra F, Bosco F, De Meo F, Bruschetta A, De Martino I, Risitano S, Sabatini L, Massè A, Cavaliere P. Trabecular titanium cups in hip revision surgery: a systematic review of the literature. Ann Jt. 2023;8:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 23. | Tamaki Y, Goto T, Takasago T, Wada K, Hamada D, Sairyo K. Clinical and radiological outcomes of total hip arthroplasty using a highly porous titanium cup or a conventional hydroxyapatite-coated titanium cup: A retrospective study in Japanese patients. J Orthop Sci. 2022;27:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Delee JG, Charnley J. Radiological Demarcation of Cemented Sockets in Total Hip Replacement. Clin Orthop Relat Res. 1976;121:20-32. [RCA] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 215] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 25. | Yoshioka S, Nakano S, Kinoshita Y, Nakamura M, Goto T, Hamada D, Sairyo K. Comparison of a highly porous titanium cup (Tritanium) and a conventional hydroxyapatite-coated porous titanium cup: A retrospective analysis of clinical and radiological outcomes in hip arthroplasty among Japanese patients. J Orthop Sci. 2018;23:967-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 26. | Liu P, Meng J, Tang H, Xiao Y, Li X, Wu Y, Liu W, Xiong Y, Gao S. Association between bariatric surgery and outcomes of total joint arthroplasty: a meta-analysis. Int J Surg. 2024;111:1541-1546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 27. | Meng J, Liu W, Xiao Y, Tang H, Wu Y, Gao S. The role of aspirin versus low-molecular-weight heparin for venous thromboembolism prophylaxis after total knee arthroplasty: a meta-analysis of randomized controlled trials. Int J Surg. 2023;109:3648-3655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 28. | Layson JT, Hameed D, Dubin JA, Moore MC, Mont M, Scuderi GR. Patients with Osteoporosis Are at Higher Risk for Periprosthetic Femoral Fractures and Aseptic Loosening Following Total Hip Arthroplasty. Orthop Clin North Am. 2024;55:311-321. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 29. | Delsmann MM, Strahl A, Mühlenfeld M, Jandl NM, Beil FT, Ries C, Rolvien T. High prevalence and undertreatment of osteoporosis in elderly patients undergoing total hip arthroplasty. Osteoporos Int. 2021;32:1661-1668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 30. | Bernatz JT, Brooks AE, Squire MW, Illgen RI 2nd, Binkley NC, Anderson PA. Osteoporosis Is Common and Undertreated Prior to Total Joint Arthroplasty. J Arthroplasty. 2019;34:1347-1353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 31. | Khatod M, Inacio MC, Dell RM, Bini SA, Paxton EW, Namba RS. Association of Bisphosphonate Use and Risk of Revision After THA: Outcomes From a US Total Joint Replacement Registry. Clin Orthop Relat Res. 2015;473:3412-3420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |