Published online Feb 18, 2025. doi: 10.5312/wjo.v16.i2.98674
Revised: November 19, 2024
Accepted: January 7, 2025
Published online: February 18, 2025
Processing time: 224 Days and 13.9 Hours
Periprosthetic fractures of the tibia are uncommon complications after total knee arthroplasty (TKA). Therefore, there is still clinical debate regarding the appro
A 65-year-old woman was treated for tibial shaft pseudarthrosis after a periprosthetic fracture. The patient underwent rTKA with a tibial component exchange to a long-stemmed implant. At her 1.5-year follow-up visit, partial asymptomatic bone union was noted with no prosthesis loosening. The patient achieved 0° to 120° range of motion and a stable knee, and reported high satisfaction. Impro
There is little consensus in the literature on the management of tibial shaft peri
Core Tip: Periprosthetic tibial fractures after long-stemmed total knee arthroplasties require planning and a personalized approach for each case. We recommend planning intramedullary fixation with long-stemmed implants or revision total knee arthroplasty with intramedullary nailing for fractures localized on the tibial shaft.
- Citation: Kocon M, Grzelecki D. Periprosthetic fractures of the tibial shaft following long-stemmed total knee arthroplasty: A case report. World J Orthop 2025; 16(2): 98674
- URL: https://www.wjgnet.com/2218-5836/full/v16/i2/98674.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i2.98674
Periprosthetic fractures are uncommon complications after total knee arthroplasty (TKA), occurring in 0.3% to 21% of cases[1,2]. The annual incidence of TKA continues to rise, with projections for the United States forecasting an 85% to 673% increase by the year 2030 (from 1.26 million to 3.48 million procedures)[3,4]. Along with the increasing number of primary TKA, the number of periprosthetic fractures is simultaneously increasing.
Risk factors for periprosthetic fractures after TKA include patient-related causes, including female sex, advanced age, osteoporosis, and osteolysis[5]. Moreover, several surgical risk factors exist, including implant malalignment or malrotation, bone defects, and previous procedures such as periarticular osteotomies[5]. Revision TKA (rTKA) is an independent risk factor for periprosthetic fracture and the incidence varies from 1.6% to 38% in those cases[6].
Current literature highlights the significant lack of consensus and established guidelines regarding management of periprosthetic fractures of the tibial shaft. Treatment strategies depend on various factors, including prosthesis stability, implant type, timing of injury, fracture localization, morphology, and bone quality. Nevertheless, definitive guidelines for selecting the appropriate treatment modality for specific fracture types remain elusive[2,7-9]. Nonoperative treatment, such as casting and bracing, is reserved for selected, nondisplaced fractures with well-fixated prosthesis elements[8]. Displaced fractures with stable and properly positioned implants usually require open reduction and internal fixation (commonly referred to as ORIF) with the use of single or double plating[2,10]. One report proposed the use of intra
We present a case report of a patient with a periprosthetic fracture of the tibial shaft and the presence of pseu
To our knowledge, cases treated with the proposed approach have not been previously documented in the medical literature.
Fracture 1: A 65-year-old woman (158 cm, 95 kg, 38.05 kg/m2 body mass index) was admitted to an orthopedic department due to malalignment, instability at the level of the right shin, and soreness of the ipsilateral knee.
Fracture 2: Three years and 3 months after the rTKA with simultaneous shaft fixation, the patient presented for an urgent early follow-up appointment due to pain and swelling in the right lower leg (distal third of lower leg and ankle joint). She reported these symptoms after low energy trauma.
She had undergone surgery 3.5 years earlier due to advanced osteoarthritis with 20° varus deformation and instability of the right knee. The surgery had involved an Advance® Medial-Pivot KneeSystem (MicroPort Orthopedics Inc., Arlington, VA, United States) arthroplasty with simultaneous medial collateral ligament reconstruction.
Fifteen months after the primary surgery, the patient fell from a bicycle and suffered an injury of the right lower limb, resulting in prosthesis component loosening. Revision surgery of the right knee was performed using the Vanguard® Revision Knee System (Zimmer Biomed, Warsaw, IN, United States). One week after the rTKA, a radiographic examination had revealed a periprosthetic fracture of the tibia and fibula shafts at the level of the tibial stem tip. The patient was treated with closed reduction and long leg casting for 6 months. However, the desired therapeutic effect had still not been achieved after this period, and at 18 months after the rTKA the patient was referred to the authors' institution and fitted with a tibial brace.
The history of past illness is not applicable.
The personal and family history is not applicable.
Fracture 1: Physical examination revealed restricted range of motion (ROM) with 100° of flexion range and pain in the right shin. The right lower limb was 4 cm shorter than the left one. No neurovascular disorders were found during the examination. Additionally, the patient reached 74 points in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and 55 points in the clinical and 10 points in the functional knee society scores (KSS) evaluation.
Fracture 2: Examination revealed a deformity in the distal third of the lower leg and palpable pathological mobility around the apex of the femoral component of the endoprosthesis.
The laboratory examinations are not applicable.
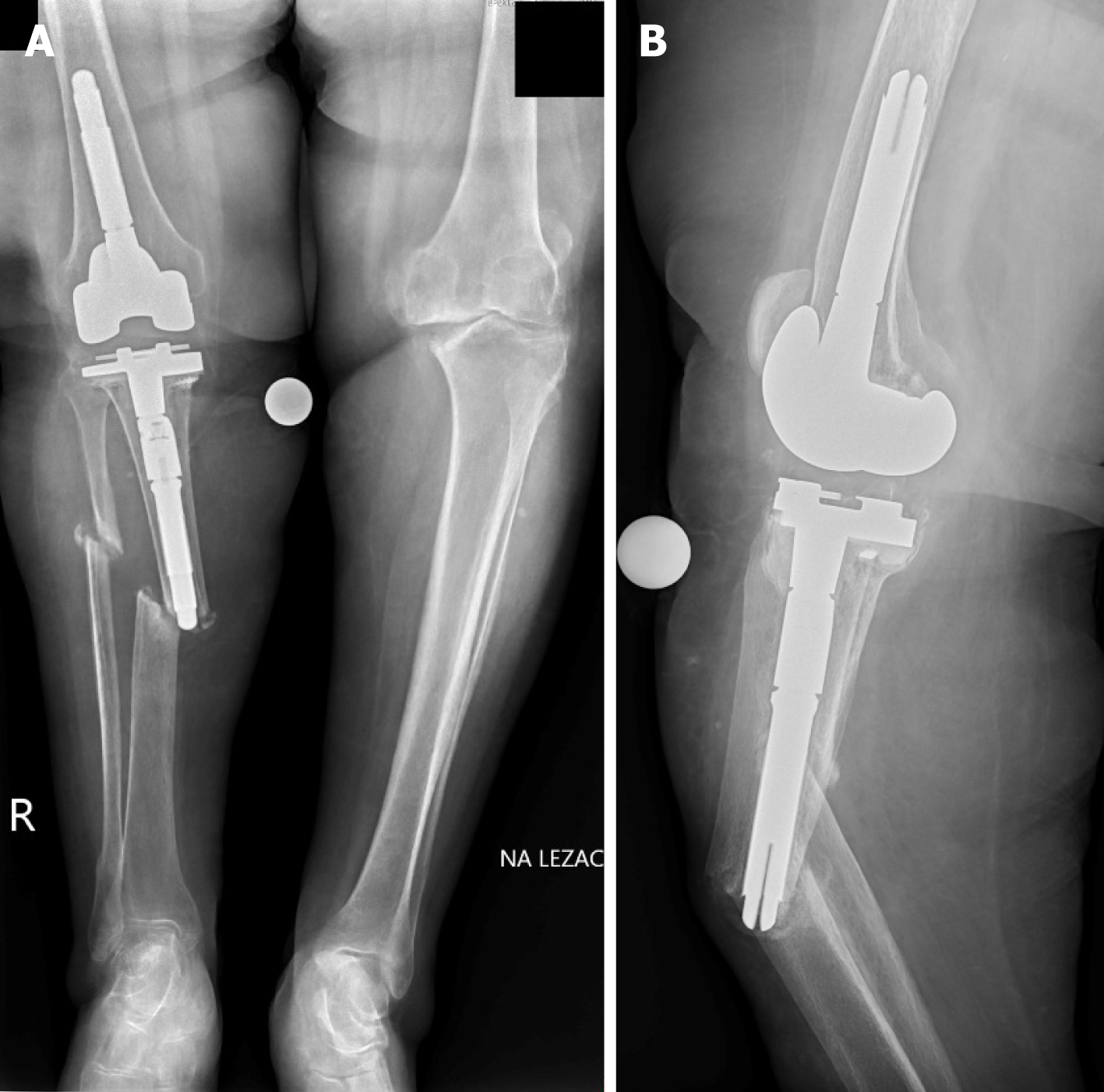
Fracture 1: A standing long leg radiograph examination (anteroposterior and lateral views) revealed a periprosthetic fracture and the presence of pseudarthrosis (Figure 1).
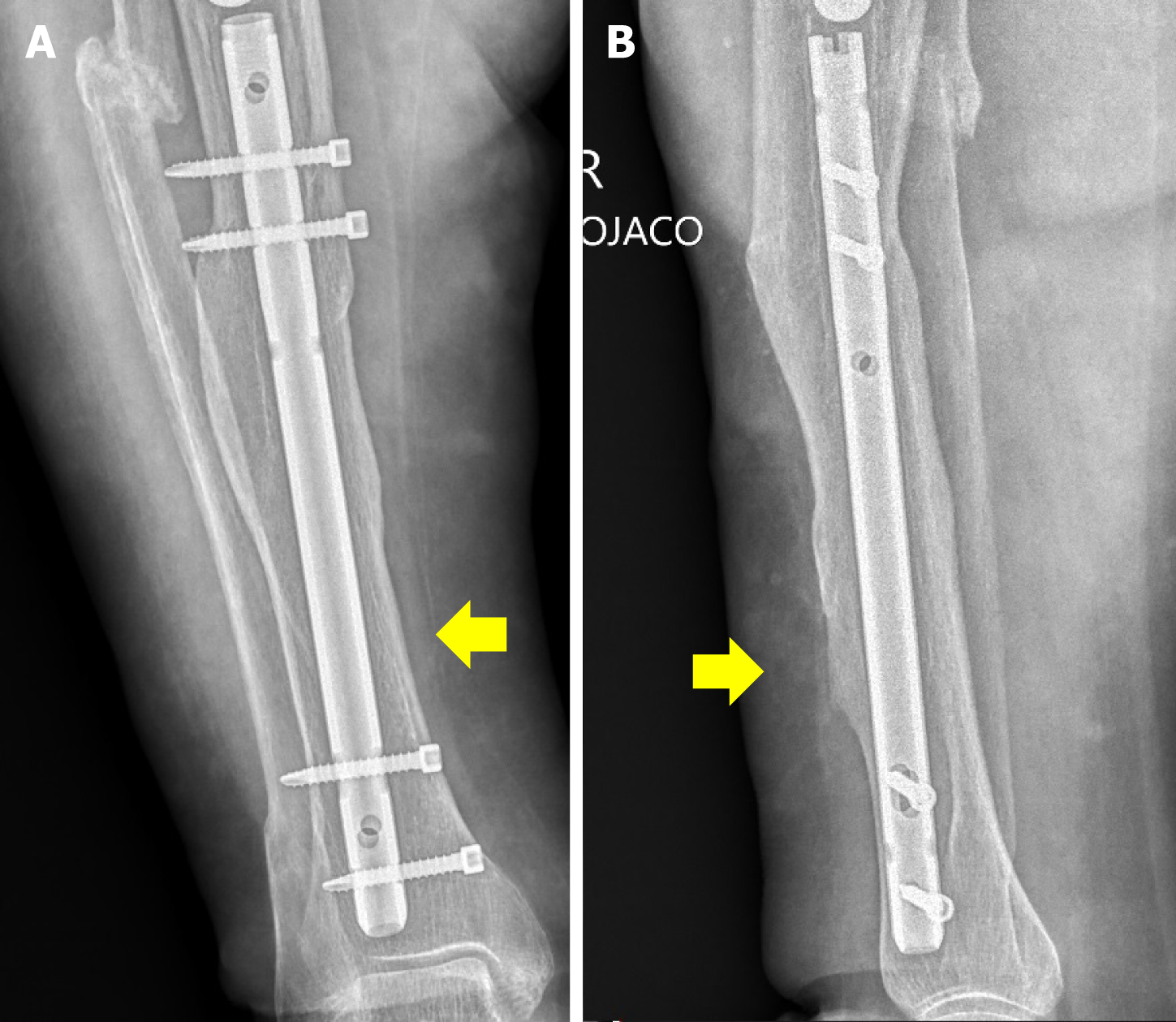
Fracture 2: Anteroposterior and lateral radiographs revealed a periprosthetic fracture at the level of the tibial stem (Figure 2).
Periprosthetic fracture in the tibial and fibular shafts (Felix type 2A) and the presence of pseudarthrosis.
A periprosthetic fracture at the level of the tibial stem and around the apex (Felix type 2A).
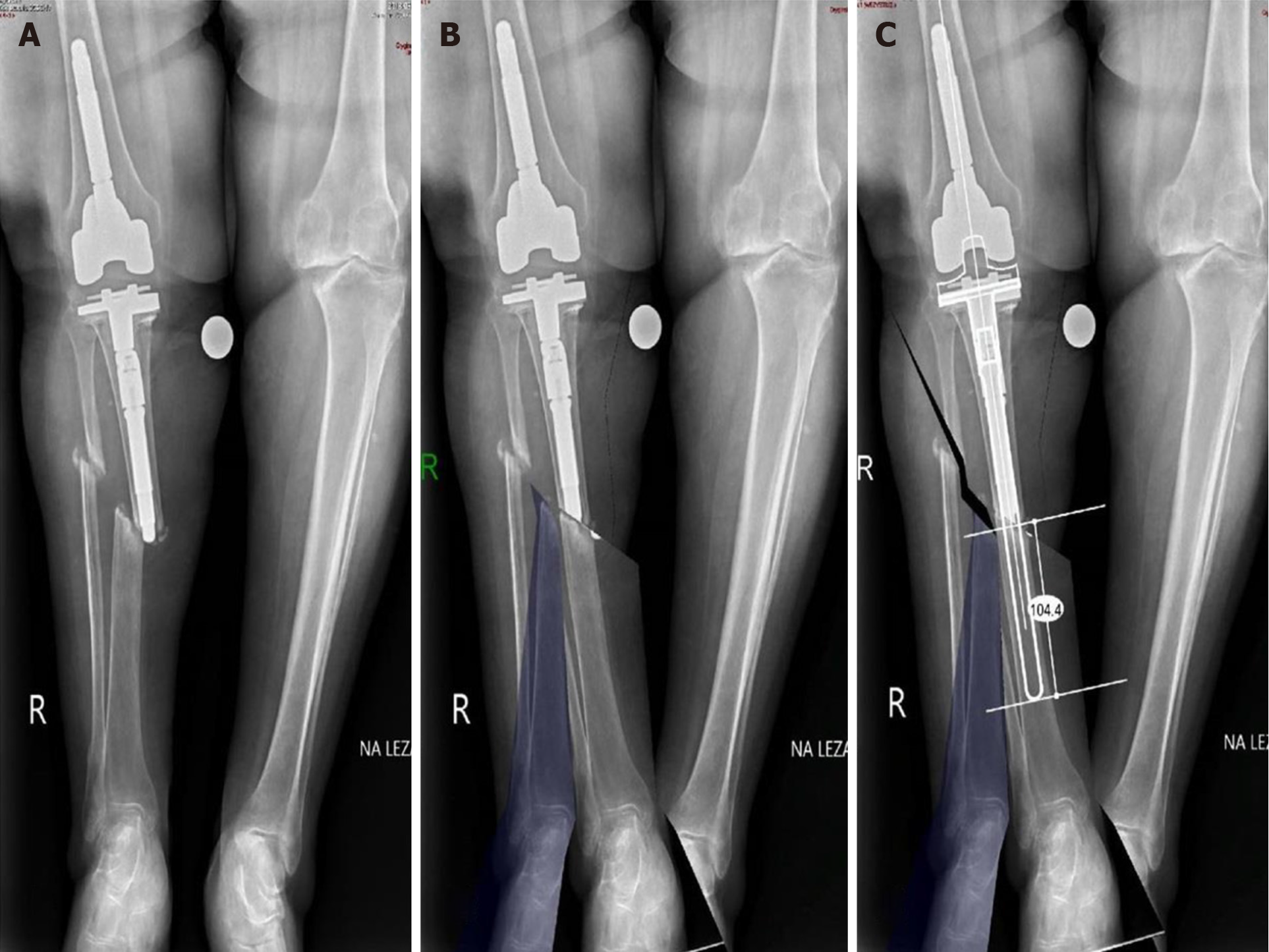
After clinical and radiological assessments, the patient was determined to qualify for rTKA with tibial component replacement and use of the long, uncemented tibial stem to stabilize the intramedullary fracture. Preoperative surgical planning and digital prosthesis templating were performed with the use of Ortho View™ (Materialise, Leuven, Belgium) (Figure 3).
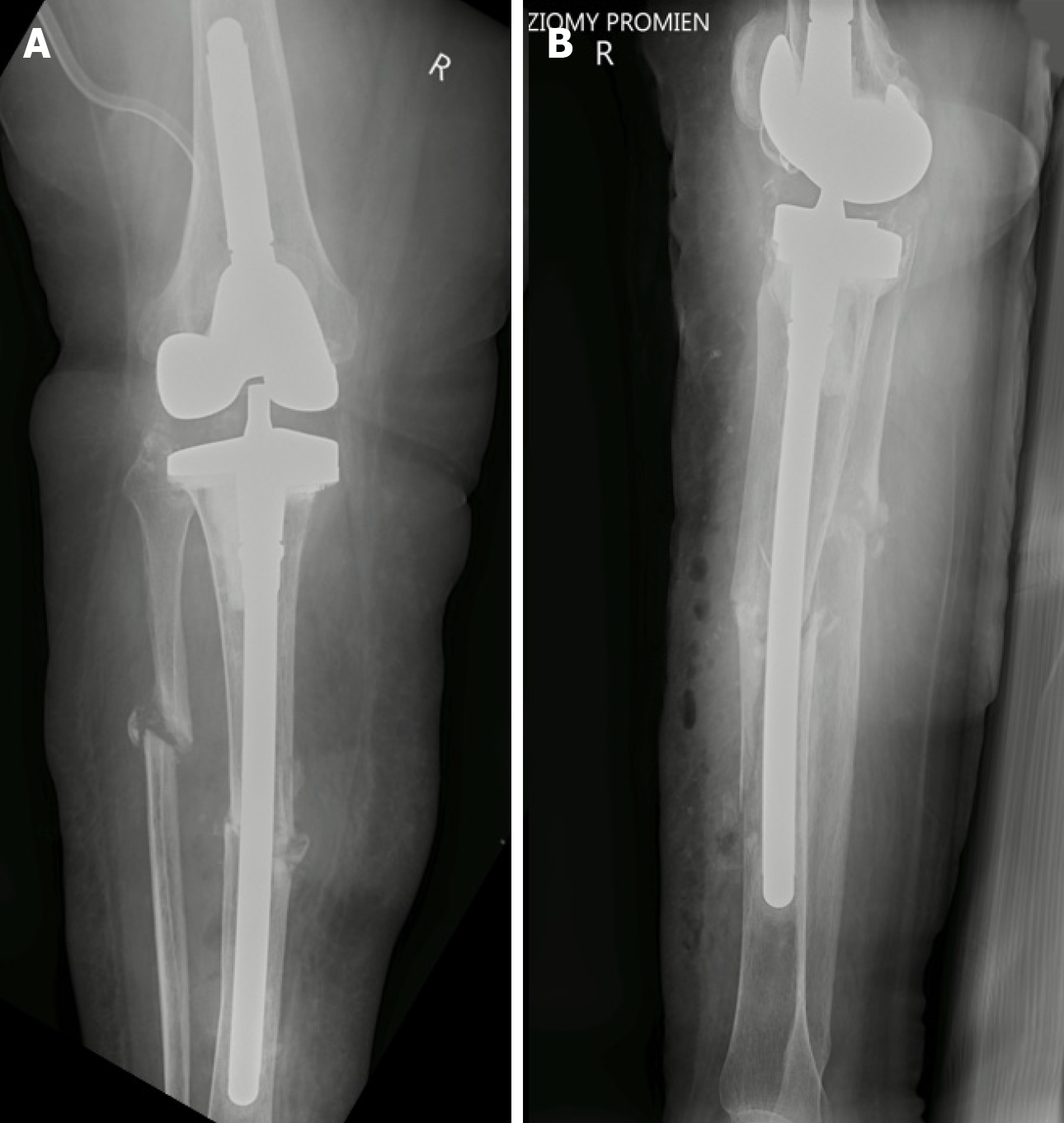
A medial parapatellar approach and wide joint exposure with fibrotic tissue excision was performed. Proper stability of the femoral component was confirmed intraoperatively. The tibial component was removed in order to use a longer stem. Tibial pseudarthrosis was exposed from the incision above the fracture and debrided. A 200 mm bowed stem was fitted through the tibial canal. A tibial baseplate No. 63 with 5 mm medial augment, 20 mm polyethylene CCK insert, and 14 mm/200 mm bowed stem was fitted. At the end of surgery, the patient’s ROM was from 0° to 120°, and proper patellar traction and joint stability were achieved. On post-operative day 1, correct tibial implant, stem position and bone alignment were confirmed by X-ray (Figure 4).
Considering the need for proper fracture stabilization, another rTKA operation was planned to replace the tibial component and endoprosthesis stem with a shorter one and for implantation of an IMN at the height of the fracture.
The rTKA was performed with the Vanguard DA360 system along with periprosthetic tibial fracture fixation antegrade from the knee joint using locked IMN (ChM, Lewickie, Poland). The procedure was performed with a tourniquet. After dissection of the soft tissues, the endoprosthesis components were accessed. The tibial components were removed without bone loss and the proximal end of the tibia was debrided. A probe was inserted into the tibial bone, and the medullary canal was expanded with successive reamers to implant the ChM 12 mm/200 mm locked nail. The nail was inserted and secured with four screws using a dedicated guide, two proximally (40 mm) and two distally (35 mm). Radiographic examination confirmed the correct placement of the nail and screws. The proximal end of the tibia was prepared and a Vanguard DA360 63 mm implant with lateral and medial 5 mm augments was cemented in place. A 16 mm/40 mm extension and a 22 mm mobile bearing insert were used. Proper alignment of the knee joint and stable fixation of the fracture were achieved. Correct tibial tray, stem and IMN positions, and bone alignment were confirmed on the 1st post-operative day by X-ray. After surgery, the limb was immobilized in a Walker boot, and the patient was allowed to partially load the leg and move with the aid of crutches for the next 6 weeks.
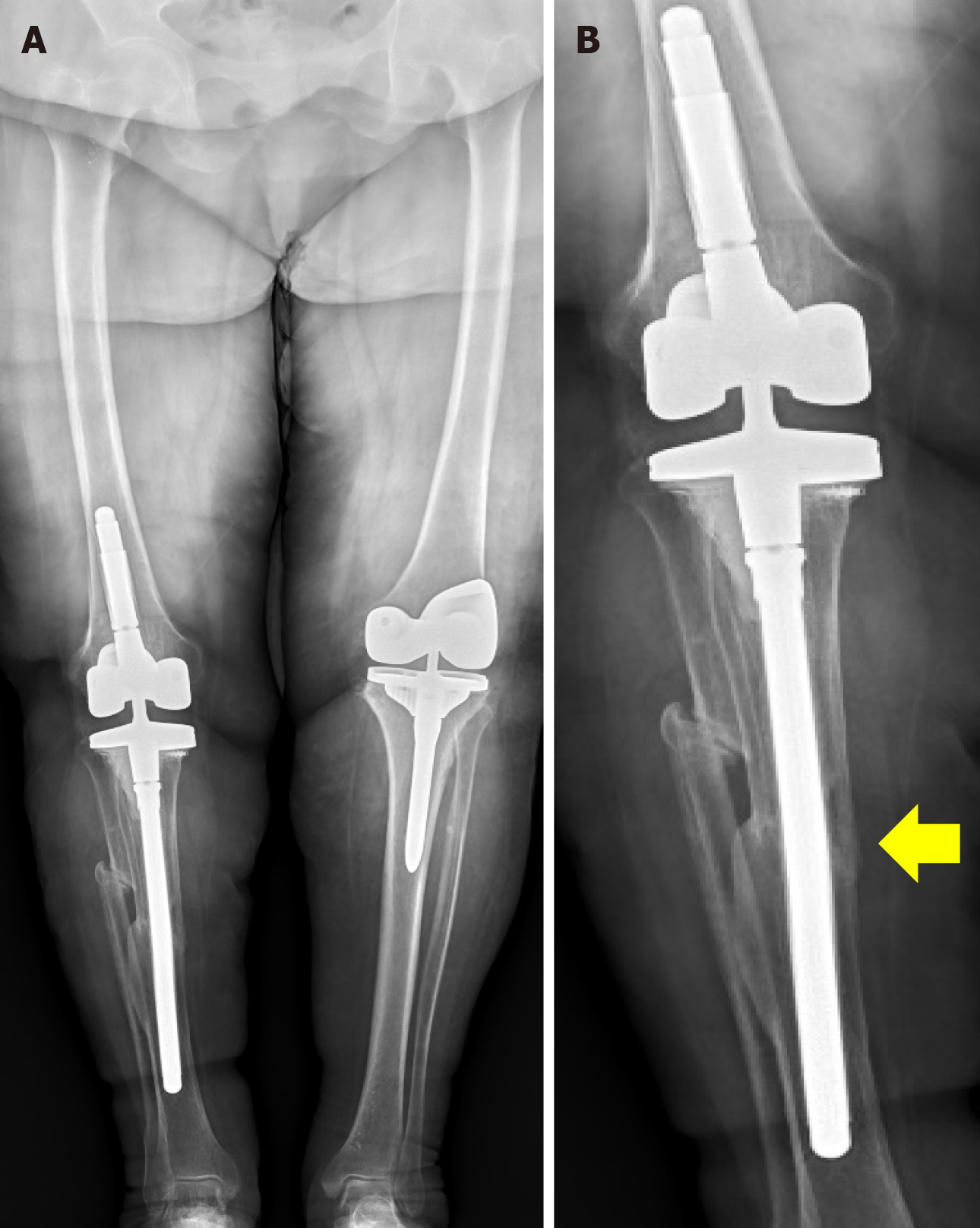
Partial weight-bearing with flexion up to 80° was allowed immediately. The patient was advised to walk with the assistance of two crutches for 6 weeks. The first follow-up visit was 3 months after surgery. Standing long leg radiographs in both anteroposterior and lateral views did not reveal any signs of implant loosening or bone fragment dislocation. During the physical examination, ROM was from 0° to 100° and stability was confirmed in all planes. The patient did not report any pain and walked without crutches. At the 12-month follow-up, we observed partial union of the tibia. The ROM was from 0° to 120°, and there were no clinical signs of knee instability. Subsequently, 1.5 years after the rTKA, when loading the right lower limb was possible, we performed contralateral TKA using the Triathlon Knee System (Stryker, Mahwah, NJ, United States) with tibial stem due to advanced osteoarthritis. At the 2-year follow-up, full bone union of the right tibia was achieved (Figure 5). The WOMAC evaluation revealed 17 points and the clinical and functional KSS scored 91 points and 80 points, respectively. Although we measured a 3.5 cm lower limb inequality, the patient was very satisfied with the therapeutic effect. She was able to move independently and did not have any problems with basic daily activities.
At the first follow-up visit at 6 weeks, the patient did not report any pain. The ROM of the operated knee joint was 0-110˚. X-rays of the limbs under load in the anteroposterior and lateral views revealed proper alignment of the implant. There were no signs of prosthesis loosening (Figure 6).
At the last follow-up visit 26 months after surgery, full bone union was confirmed (Figure 7). The patient was able to move with full weight-bearing on the operated limb without the aid of crutches for distances up to 800 m. She reporting using them as a precaution for longer walks. The ROM of the knee joint was 0˚-120˚ and was painless throughout the entire range. WOMAC and clinical and functional KSS revealed 15 points, 81 points and 80 points, respectively.
Periprosthetic tibial fractures are less commonly described in the literature than femur fractures, and most reports concern case series or case reports[10,11,16,17]. The most demanding cases for surgeons include loosened implants, instability, malalignment and/or poor bone stock, which are also indications for implant exchange with or without osteosynthesis[18,19]. A meta-analysis from 2015 conducted by Ebraheim et al[20] included data of only 144 patients and focused on subtypes according to Schreiner et al[21]. For subtype A (stable prosthesis; 18.75% of cases), they proposed conservative treatment or ORIF and noted a low complication rate. Subtype B (loosened implant; 43.75% of cases) was treated either with or without rTKA. For those who underwent rTKA, bone union was achieved in all cases, but in those without rTKA the revision rate reached 82.1%. In subtype C (intraoperative fractures; 37.5% of cases), additional surgical intervention was not required and all fractures were fixed during the TKA.
Concerning these findings, we agree that assessment of implant stability and/or malalignment is essential before surgery. Nevertheless, partially due to its rarity, there are still no strict recommendations on which fixation method is preferred for each type of fracture. Every case should be analyzed individually. For a fixed prosthesis, Morwood et al[17] recommend dual plating if fracture occurs in the proximal third and either single plating or nailing if it occurs in the middle or distal third. They observed an overall union rate of 76.3%, with the lowest rate in Felix 2A fractures (42.9%) or those near the tibial stem tip. Moreover, the reoperation rate was higher in Felix 2A fractures (71.4%) than in 1A and 3A fractures (0% and 33.3%, respectively). These results are consistent with several other reports of a high overall complication rate (28.6%) with a large percentage of patients requiring revision surgery (21.4%)[21,22]. Similarly, Sim et al[16] analyzed a group of patients with 2A fractures and reported excellent clinical outcomes and well-maintained tibial alignment with the use of minimally invasive, dual-plating osteosynthesis. In the discussed case of a Felix 2A fracture, single or double-plating was considered. However, due to the previously applied revision implant with a long stem, this strategy was risky and could result in non-union due to bone fragment instability.
Some studies propose the use of IMNs in tibial shaft fractures distal to the prosthesis[11,23-26]. However, we found only 11 cases in the literature utilizing this method: (1) 10 antegrade implantations (8 through infrapatellar[11,23,26] and 2 suprapatellar approaches[24]); and (2) 1 retrograde through the calcaneotalotibial axis[25]. All of these patients achieved bone union with a low complication rate, which emphasizes the usefulness of this method for this specific patient group. In the case of our patient, the use of an IMN was technically demanding. Therefore, to treat a patient's first fracture, we proposed another solution that corresponds to a combination of IMN and prosthesis replacement. This concept relies on intramedullary bone fixation, which was made on a well-fitted long stem and intramedullary fixation without the use of additional fixation hardware. To our knowledge, this is the first case of tibial shaft fracture below the total knee prosthesis treated in such a way.
When planning the treatment of a subsequent periprosthetic fracture, the above method could not be used because a longer prosthesis stem was not available. Due to post-operative scarring and low bone quality, we again decided to use intramedullary fixation, but this time with cortical screw locking. In both cases, the procedure proved to be successful, as complete osseointegration was achieved.
An additional complication was the development of tibial shaft pseudarthrosis. This was caused by instability without vascular supply disturbances and/or infection. Therefore, once the fracture was properly stabilized, bone union was achieved with both fracture treatment methods. In addition, axial weight bearing was allowed immediately after surgery to achieve bone fragment compression.
The use of a long intramedullary stem prosthesis in treating periarticular tibial fractures represents a significant advance in orthopedic treatment strategies. By providing increased axial stability and load distribution below the existing knee endoprosthesis, the long stem design eliminates the need for wide surgical access of the fracture site. This modification not only provides sensational fracture stabilization but also reduces the risk of further complications such as lack of fusion, thereby promoting favorable clinical outcomes. In addition, the long stem can transmit loads over the fracture site, allowing compression of the fracture during limb loading, which is crucial for early initiation of rehabilitation. In our opinion, intramedullary stabilization is the technique of choice for the treatment of simple, type II and III periarticular fractures according to the Felix classification.
Long-stemmed revision knee arthroplasty, either without additional fixation material or in conjunction with an IMN, represents a promising treatment modality for the rare occurrence of periprosthetic tibial shaft fractures. Although this approach is technically demanding and requires a high level of surgical skill and expertise, it can yield excellent outcomes in terms of bone union and clinical and functional results. However, further studies are needed on a larger patient cohort to validate our findings and assess the efficacy of this method.
| 1. | Parvizi J, Jain N, Schmidt AH. Periprosthetic knee fractures. J Orthop Trauma. 2008;22:663-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Schreiner AJ, Schmidutz F, Ateschrang A, Ihle C, Stöckle U, Ochs BG, Gonser C. Periprosthetic tibial fractures in total knee arthroplasty - an outcome analysis of a challenging and underreported surgical issue. BMC Musculoskelet Disord. 2018;19:323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2079] [Cited by in RCA: 3261] [Article Influence: 181.2] [Reference Citation Analysis (0)] |
| 4. | Sloan M, Premkumar A, Sheth NP. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100:1455-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 841] [Cited by in RCA: 1449] [Article Influence: 207.0] [Reference Citation Analysis (1)] |
| 5. | Capone A, Congia S, Civinini R, Marongiu G. Periprosthetic fractures: epidemiology and current treatment. Clin Cases Miner Bone Metab. 2017;14:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 89] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 6. | Della Rocca GJ, Leung KS, Pape HC. Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma. 2011;25 Suppl 2:S66-S70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 205] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 7. | Felix NA, Stuart MJ, Hanssen AD. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Relat Res. 1997;113-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 123] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Hanssen AD, Stuart MJ. Treatment of periprosthetic tibial fractures. Clin Orthop Relat Res. 2000;91-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Johnston AT, Tsiridis E, Eyres KS, Toms AD. Periprosthetic fractures in the distal femur following total knee replacement: A review and guide to management. Knee. 2012;19:156-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Kim HJ, Park KC, Kim JW, Oh CW, Kyung HS, Oh JK, Park KH, Yoon SD. Successful outcome with minimally invasive plate osteosynthesis for periprosthetic tibial fracture after total knee arthroplasty. Orthop Traumatol Surg Res. 2017;103:263-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Devendra A, Gupta NP, Zackariya Jaffrulah M, Armstrong BRW, Dheenadhayalan J, Rajasekaran S. Management of Tibial Shaft Fractures Distal to TKA Prosthesis by Intramedullary Nail: A Report of Three Cases. Indian J Orthop. 2020;54:901-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Grzelecki D, Dudek P, Kowalczewski J, Marczak D. Złamanie okołoprotezowe dalszego końca kości udowej po całkowitej alloplastyce stawu kolanowego-opis przypadku. Chir Narzadow Ruchu Ortop Pol. 2016;81:91-95. |
| 13. | Grzelecki D, Szneider J, Marczak D, Kowalczewski J. Total knee arthroplasty with simultaneous tibial shaft osteotomy in patient with multiple hereditary osteochondromas and multiaxial limb deformity - a case report. BMC Musculoskelet Disord. 2020;21:233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Kamal A, Dong RJ, Shah R, Li C. Management of periprosthetic fractures of knee arthroplasty with revision surgery. J Orthop. 2020;22:118-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Radke S, Radke J. Total knee arthroplasty in combination with a one-stage tibial osteotomy: a technique for correction of a gonarthrosis with a severe (>15 degrees) tibial extra-articular deformity. J Arthroplasty. 2002;17:533-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Sim JA, Shon OJ, Joo YB, Sohn HS, Byun SE, Kim JW. Clinical outcomes of osteosynthesis of well-fixed periprosthetic proximal tibial fractures (Felix type 2A) after total knee arthroplasty. Injury. 2021;52:3099-3103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Morwood MP, Gebhart SS, Zamith N, Mir HR. Outcomes of fixation for periprosthetic tibia fractures around and below total knee arthroplasty. Injury. 2019;50:978-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Whitehouse MR, Mehendale S. Periprosthetic fractures around the knee: current concepts and advances in management. Curr Rev Musculoskelet Med. 2014;7:136-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Verma N, Jain A, Pal C, Thomas S, Agarwal S, Garg P. Management of periprosthetic fracture following total knee arthroplasty- a retrospective study to decide when to fix or when to revise? J Clin Orthop Trauma. 2020;11:S246-S254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Ebraheim NA, Ray JR, Wandtke ME, Buchanan GS, Sanford CG, Liu J. Systematic review of periprosthetic tibia fracture after total knee arthroplasties. World J Orthop. 2015;6:649-654. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Schreiner AJ, Gonser C, Ihle C, Zauleck MK, Klopfer T, Stuby F, Stöckle U, Ochs BG. Adverse Events in the Treatment of Periprosthetic Fractures Around the Knee - a Clinical and Radiological Outcome Analysis. Z Orthop Unfall. 2018;156:287-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Triplet JJ, Taylor BC, Brewster J. Outcomes and Review of Periprosthetic Tibial Fractures. Orthopedics. 2020;43:182-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Haller JM, Kubiak EN, Spiguel A, Gardner MJ, Horwitz DS. Intramedullary nailing of tibial shaft fractures distal to total knee arthroplasty. J Orthop Trauma. 2014;28:e296-e300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | Woyski D, Emerson J. Suprapatellar Nailing of Tibial Shaft Fractures in Total Knee Arthroplasty. J Orthop Trauma. 2016;30:e409-e413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Zafra-Jiménez JA, Pretell-Mazzini J, Resines-Erasun C. Distal tibial fracture below a total knee arthroplasty: retrograde intramedullary nailing as an alternative method of treatment: a case report. J Orthop Trauma. 2011;25:e74-e76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Reyes-Cabrera JM, González-Alconada R, García-Mota MD. [Distal tibia peri-implant fracture with an intramedullary nail: a case report]. Rev Esp Cir Ortop Traumatol. 2013;57:443-445. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |