Published online Feb 18, 2025. doi: 10.5312/wjo.v16.i2.104095
Revised: December 29, 2024
Accepted: January 23, 2025
Published online: February 18, 2025
Processing time: 64 Days and 16 Hours
Surgical intervention is a critical treatment approach for symptomatic atlantoaxial dislocation. However, vertebral artery injury remains a significant challenge during such procedures. We present a case of successful treatment of atlantoaxial dislocation with concurrent vertebral artery injury using interlaminar screw technology, and review the relevant literature.
A 69-year-old female patient, with no history of trauma, was diagnosed with at
Thorough preoperative evaluation, such as CTA imaging, and the surgeon’s ex
Core Tip: Symptomatic atlantoaxial dislocation can cause persistent spinal cord compression if not treated promptly, potentially leading to paralysis or death. Surgical intervention is currently recommended. Iatrogenic vertebral artery injury (IVAI) is a severe complication of cervical spine surgery, including atlantoaxial dislocation treatment. Vertebral artery anomalies increase the risk of IVAI during the procedure. We treated a patient with atlantoaxial dislocation complicated by vertebral artery anomalies, and the case is reported subsequently
- Citation: Tang RH, Yin J, Zhou ZW. Atlantoaxial dislocation with vertebral artery anomaly: A case report. World J Orthop 2025; 16(2): 104095
- URL: https://www.wjgnet.com/2218-5836/full/v16/i2/104095.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i2.104095
Symptomatic atlantoaxial dislocation can cause persistent spinal cord compression if not treated promptly, potentially leading to paralysis or death. Surgical intervention is currently recommended[1]. Iatrogenic vertebral artery injury (IVAI) is a severe complication of cervical spine surgery, including atlantoaxial dislocation treatment. Vertebral artery anomalies increase the risk of IVAI during the procedure. We treated a patient with atlantoaxial dislocation complicated by vertebral artery anomalies, and the case is reported subsequently.
A 69-year-old women presented with headaches and upper limb numbness lasting > 2 months. She reported that the headaches began without any obvious triggers and were accompanied by shoulder and neck pain. A few days later, she developed numbness in both upper limbs but had no bowel or bladder dysfunction.
Past medical history includes renal cysts and chronic bronchitis.
Denies any significant genetic disorders or family history of diseases.
Physical examination revealed normal vital signs and a visual analogue scale (VAS) score of 4. She exhibited tenderness in the posterior neck and bilateral scapular regions, numbness in both upper arms and hands, and diminished superficial sensation. Neck movement was restricted, and limb muscle strength was rated as IV-V. Both the Eaten and Spurling tests were negative, as were the Tinel’s signs at the elbows and wrists, Hoffmann’s sign, and tendon reflexes.
Serological tests revealed a normal blood count, liver function, kidney function, and rheumatic and immunological markers. Markers of infection, including C-reactive protein, erythrocyte sedimentation rate, and interleukin-6, were within normal limits.
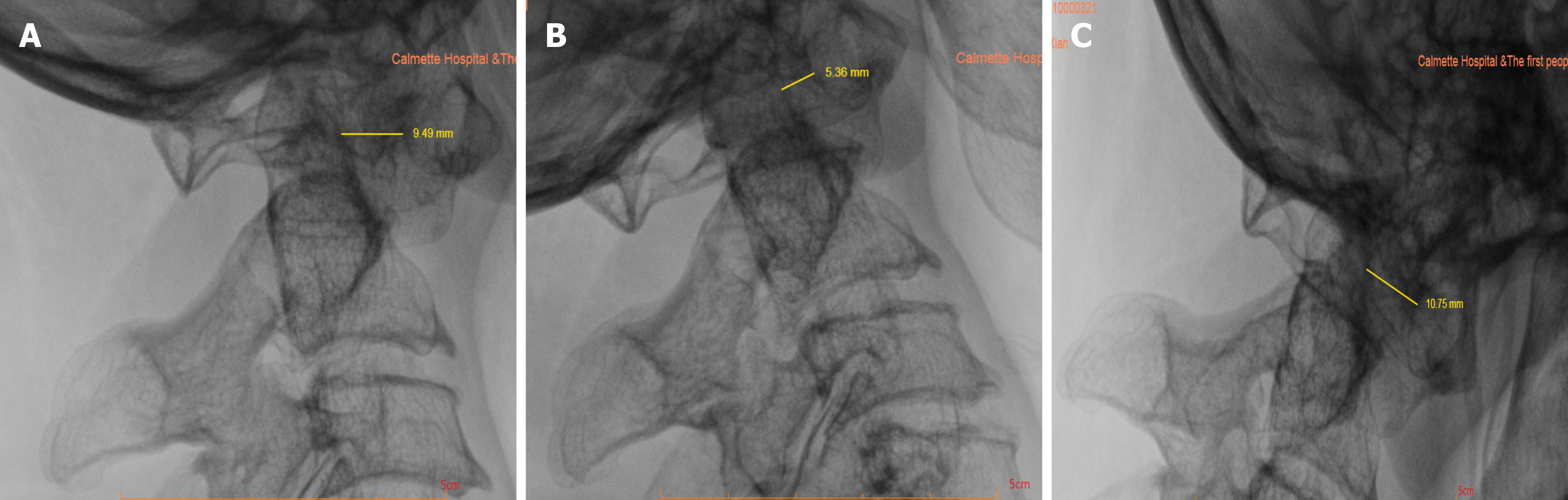
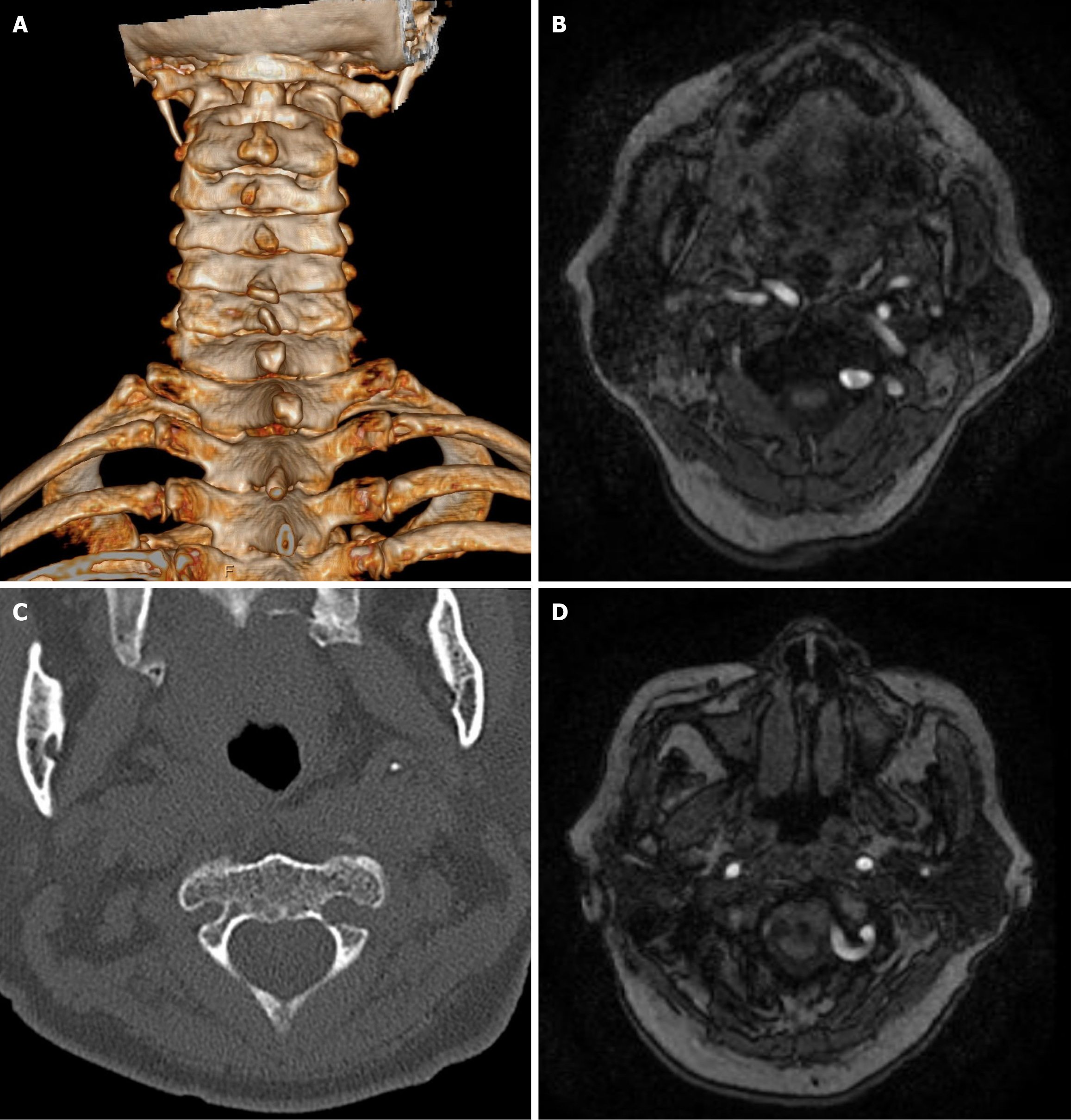
Magnetic resonance imaging (MRI) and computed tomography angiography (CTA) revealed a tortuous right vertebral artery, left vertebral artery dominance, C3/4 and C4/5 disc herniations, synovitis, anterior joint space effusion in the atlantoaxial joint, partial dislocation of the atlantoaxial joint, and posterior displacement of the odontoid process compressing the spinal cord (Figure 1). Dynamic cervical spine radiography revealed instability at C1/2 (Figure 2).
The primary diagnosis was basilar invagination with atlantoaxial dislocation (Goel A).
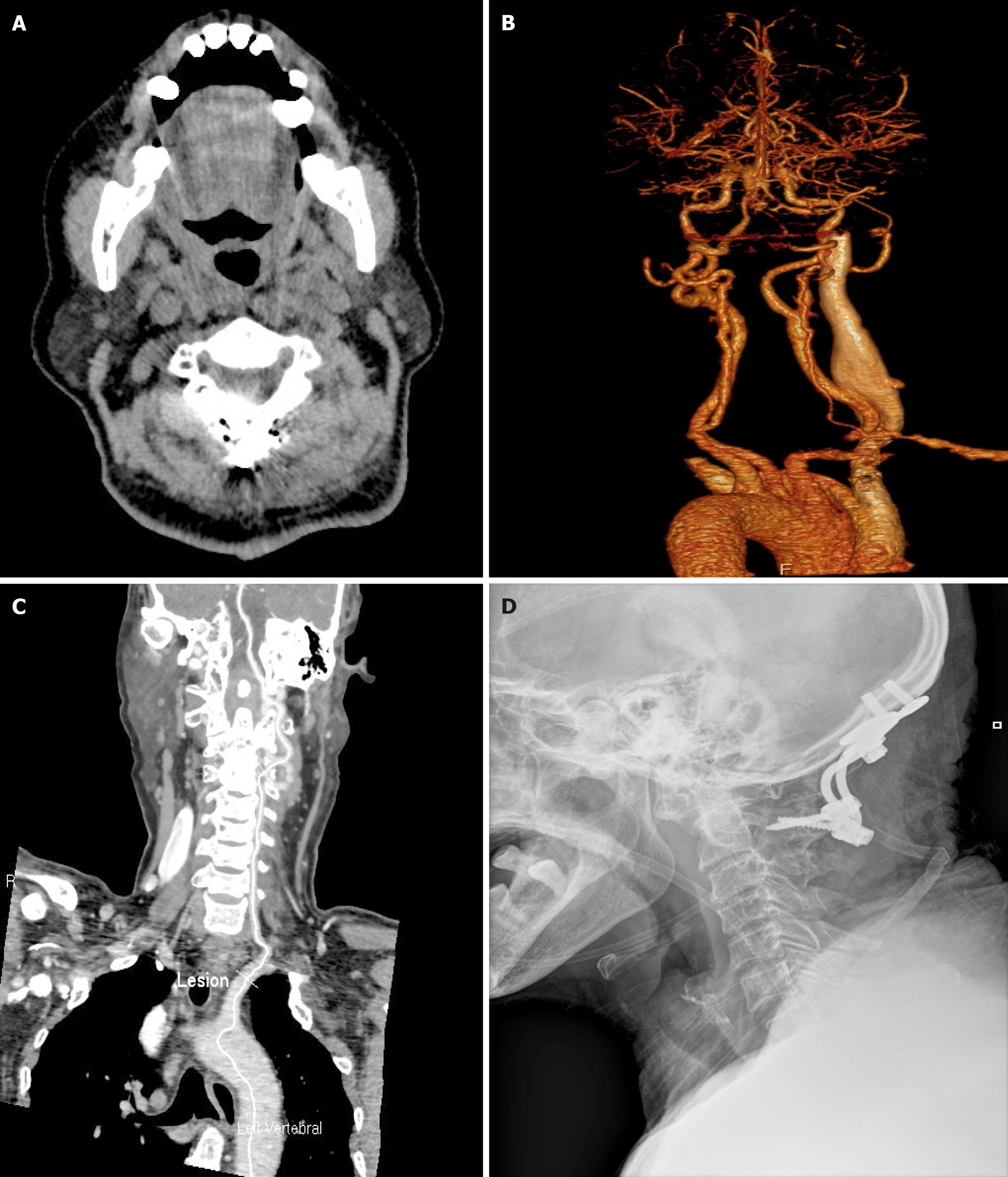
After induction of anesthesia, the patient underwent posterior occipitocervical fusion. Preoperative CTA suggested abnormal development of the vertebral artery, with the left vertebral artery at V3 segment invading the lateral mass of C2, and the left vertebral artery at V4 segment adjacent to the posterior arch of C1 (Figure 3). Active bleeding was observed during the exposure of the left C2 screw placement site, suggesting possible vertebral artery injury. Gelatin sponges and brain cotton pads were used for hemostasis, which partially reduced the bleeding. Continued local pressure with a mixture of bone wax and gelatin sponge controlled the bleeding after approximately 40 minutes of persistent pressure by an assistant. To prevent bilateral vertebral artery injury that could lead to compromised cranial blood supply, we refrained from attempting lateral mass or pedicle screw placement on the right side of C1 and C2. C2 Lamina screws were then placed, followed by the insertion of screws into the occipital bone plate, installation of pre-bent connecting rods, and traction and extension of the cervical spine with locking of the rod tail cap. We choose to perform bone grafting with autogenous iliac bone grafts between the laminae to increase stability. Postoperatively, the patient wore a cervical collar for stabilization, with close monitoring of vital signs, drainage volume and characteristics, and neurological status, including eye-opening, speech, and upper limb sensory and motor function.
The drain was removed on postoperative day 3, following which cervical spine radiography and CT scans were obtained (Figure 4). The patient was discharged on postoperative day 7 with no unsteadiness, dizziness, or discomfort. Headaches significantly improved compared to those at admission, with a VAS score of two, and upper limb numbness also showed improvement. At the postoperative follow-up, the patient recovered well, with the Japanese Orthopaedic Association increasing from 12 preoperatively to 15 postoperatively, indicating a 60% improvement, and no clinical signs of posterior circulation ischemia, such as dizziness, nausea, or vomiting. In the follow-up one year after the surgery, the patient reported no numbness, weakness, or decline in mobility in the limbs. Additionally, there were no reports of dizziness, headaches, gait instability, or increased fall risk, nor any disturbances in bowel or bladder function.
Classic posterior atlantoaxial fixation techniques include wire binding, transarticular screw fixation, pedicle screw/Laminar screw/rod plate systems, and occipitocervical fusion. Anterior approaches include transoral repositioning plate fixation and anterior cervical transarticular screw techniques. Common posterior cervical screw techniques include lateral mass and pedicle screws[2]. Miyakoshi et al[3] introduced the C2 Laminar screw technique, which is an effective alternative to reduce the risk of intraoperative vertebral artery injury in hospitals lacking surgical microscopes and other advanced instruments[2]. However, there is a risk of spinal cord injury from screw insertion into the spinal canal. Researchers have also proposed techniques, such as spinous process double-cortex screws and facet screws (Magerl screws). Magerl screws provide good resistance to flexion, extension, and rotation. However, biomechanically, C1/2 pedicle screws provide the best mechanical strength. Because of the greater amount of cancellous bone in the spinous process and lamina, laminar screws have weaker resistance to lateral bending and anchoring than that of pedicle screws[1]. If a single technique cannot achieve bilateral fixation, a combination of two or more internal fixation techniques is often used. Additionally, transoral or posterior lateral mass joint release may reduce fixation stress[3].
Clinically, the vertebral artery is divided into four segments, with variations commonly occurring in the V2 and V3 segments. The V3 segment is particularly relevant for upper cervical spine surgeries[4]. Vertebral artery development at the craniocervical junction often exhibits variations due to abnormal bone structure development. Researchers have classified developmental anomalies into four types. Types I and III have a low angle of the vertebral artery groove, which facilitates pedicle screw placement, whereas Types II and IV have grooves closer to the inner wall of the pedicle, posing a high risk of screw insertion[5]. Vertebral artery developmental anomalies, such as high-riding vertebral arteries or small pedicles with transverse foramen fusion, pose significant technical challenges for the implantation of C1 Lateral mass screws and C2 pedicle screws, and for surgical procedures in these areas[6]. Detailed preoperative preparation is crucial for surgical safety. Common assessment methods include CTA of the head and neck, vertebral artery angiography, and MRA of the head and neck. Some studies have proposed screw placement assessment methods based on thin-slice CT tomography. For instance, if more than four continuous images of the atlas show a pedicle thickness greater than 4 mm, pedicle screws can be used. If fewer than two layers are visible, lateral mass screws are recommended. The use of 3D-printed guides allows for a clearer assessment of vertebral artery anatomy and variations, improves screw placement accuracy and reduces the risk of intraoperative IVAI[7]. In cases with a dominant-side vertebral artery supply, after a thorough preoperative evaluation, it is preferable to use pedicle screws on the non-dominant side to achieve optimal mechanical strength. Alternative techniques, such as laminar screws or vertebral body screws are recommended to minimize the risk of vertebral artery injury.
The complications of cervical spine surgery include IVAI, venous plexus injury, cerebrospinal fluid leakage, and surgical site infections. Research indicates that the incidence of vertebral artery injury during cervical spine surgery is approximately 8.2%[8]. This can lead to severe complications, such as pseudoaneurysm of the vertebral artery, delayed hemorrhage, cerebral ischemic infarction, or even death. The causes of such injuries include the use of high-speed drills, inadequate exposure of the surgical area, and screw placement in the upper cervical vertebrae. For bleeding in the venous plexus, electrocautery should be avoided during hemostasis. Instead, methods, such as applying gelatin sponges and brain cotton pledgets under pressure, should be used. Once IVAI occurs, treatment goals are to control local bleeding, prevent ischemia and embolism, and minimize the risk of postoperative embolic complications. The primary method is direct packing for hemostasis using materials, such as gelatin sponges, brain cotton, bone wax, and hemostatic gauze. However, packing carries a high risk of delayed bleeding and pseudoaneurysm formation[7]. If the packing fails, life-saving options include surgical ligation, endovascular embolization of the affected vertebral artery, or stent placement. However, ligation and occlusion of the vertebral artery are significantly associated with posterior cerebral circulation ischemia and cerebral infarction. Therefore, when damage occurs to the dominant side of the artery, vascular repair techniques, such as vessel suturing or bypass should be actively considered. However, these methods are technically difficult[9,10].
After the occurrence of IVAI, postoperative vertebral artery CTA or related vascular examinations should be performed to assess the effectiveness of hemostasis, vessel patency, and the presence of pseudoaneurysms. Following a thorough assessment of rebleeding risk, anticoagulant and antiplatelet medications should be used to reduce the impact of local thrombosis on the cerebral blood supply and minimize the occurrence of cerebral infarction and other sequelae. There
| 1. | 1 Wang SL, Tian YL, Xu NF, Li WS. [Clinical effect of posterior hybrid cervical fixations in the treatment of atlantoaxial instability or dislocation]. Zhongguo Jizhujisui Zazhi. 2020;30:338-345. |
| 2. | Moon BJ, Choi KH, Shin DA, Yi S, Kim KN, Yoon DH, Ha Y. Anatomical variations of vertebral artery and C2 isthmus in atlanto-axial fusion: Consecutive surgical 100 cases. J Clin Neurosci. 2018;53:147-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Miyakoshi N, Hongo M, Kobayashi T, Suzuki T, Abe E, Shimada Y. Comparison between Bilateral C2 Pedicle Screwing and Unilateral C2 Pedicle Screwing, Combined with Contralateral C2 Laminar Screwing, for Atlantoaxial Posterior Fixation. Asian Spine J. 2014;8:777-785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Lau SW, Sun LK, Lai R, Luk MS, Ng YS, Wong NM, Lau PY. Study of the anatomical variations of vertebral artery in C2 vertebra with magnetic resonance imaging and its application in the C1-C2 transarticular screw fixation. Spine (Phila Pa 1976). 2010;35:1136-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Wang S, Wang C, Liu Y, Yan M, Zhou H. Anomalous vertebral artery in craniovertebral junction with occipitalization of the atlas. Spine (Phila Pa 1976). 2009;34:2838-2842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Wu XG, Huang J, Jiang YQ, Guo WK, Wang J. [Anatomical study on vertebral artety and its application in transpedicle screw fixation for upper cervical vetebrae]. Zhongguo Gu Shang. 2014;27:772-774. [PubMed] |
| 7. | Wang J, Xia H, Ying Q, Lu Y, Wu Z, Ai F, Ma X. An anatomic consideration of C2 vertebrae artery groove variation for individual screw implantation in axis. Eur Spine J. 2013;22:1547-1552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Chen CQ, Feng WQ, Cheng W, Orthopedics DO. [Vertebral artery injury of upper cervical spine fracture with posterior internal fixation]. Zhongguo Jizhujisui Zazhi. 2018;28:607-612. |
| 9. | Choi JW, Lee JK, Moon KS, Kim YS, Kwak HJ, Joo SP, Kim JH, Kim SH. Endovascular embolization of iatrogenic vertebral artery injury during anterior cervical spine surgery: report of two cases and review of the literature. Spine (Phila Pa 1976). 2006;31:E891-E894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Belykh E, Xu DS, Yağmurlu K, Lei T, Byvaltsev VA, Dickman CA, Preul MC, Nakaji P. Repair of V2 Vertebral Artery Injuries Sustained During Anterior Cervical Diskectomy. World Neurosurg. 2017;105:796-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |