Published online Feb 18, 2025. doi: 10.5312/wjo.v16.i2.103416
Revised: December 25, 2024
Accepted: January 18, 2025
Published online: February 18, 2025
Processing time: 84 Days and 18.1 Hours
Gas-containing pseudocysts rarely cause of lumbar radiculopathy. This report describes successful treatment of a gas-containing pseudocyst using percutaneous transforaminal endoscopy.
A 48-year-old man presented with severe pain and numbness in his right leg, which worsened upon walking or weight bearing. Computed tomography and magnetic resonance imaging revealed a gas-containing cyst compressing the left L5 nerve root at the L4–5 level. The pseudocyst was successfully removed using a percutaneous transforaminal endoscopic discectomy. Vivid and clear endoscopic imaging of the pseudocysts was performed intraoperatively. The patient experi
Transforaminal endoscopy offers excellent surgical visualization and facilitates meticulous operative manipulation, making it a minimally invasive approach for treating gas-containing pseudocysts in the intervertebral foramen.
Core Tip: This study described a successful treatment of lumbar radiculopathy caused by gas-containing pseudocyst through percutaneous transforaminal endoscopy (PTE). Combining preoperative images with details of intraoperative videos such as bubble formation, we determined that the diagnosis was a gas-containing pseudocyst. Additionally, it confirms that PTE can be used to excise gas-containing pseudocysts within the intervertebral foramen.
- Citation: Jiang ZX, Ren JB, Li YC, Chen L. Percutaneous transforaminal endoscopic treatment of gas-containing pseudocyst compressing the L5 nerve root: A case report. World J Orthop 2025; 16(2): 103416
- URL: https://www.wjgnet.com/2218-5836/full/v16/i2/103416.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i2.103416
Lumbar radiculopathy is attributed to a multitude of pathological factors[1-3], and gas-containing pseudocysts are a rare cause[4-8]. The etiology of gas-containing pseudocysts remains unclear[6,8-11]. Although gas-containing pseudocysts have been treated with conservative management such as pharmacotherapy and nerve blockade[8,9,11-13], the analgesic efficacy is often suboptimal, and percutaneous aspiration is associated with a high rate of recurrence[9,14]. Open surgical interventions permit a more thorough excision of the pseudocyst, resulting in favorable clinical outcomes, but an acc
A 48-year-old man presented with severe radiating pain in the right leg for 10 months.
Symptoms were exacerbated after walking. Conservative treatments, including narcotics, physical therapy, and a series of root blocks, were ineffective.
The patient denied any previous diseases and surgical history.
Denied smoking, alcohol, drug use, industrial toxins history.
Sensory impairment was observed in the L5 dermatome of the right leg; however, no motor weakness was observed in either limb. The straight leg raise test yielded positive results for the right leg but negative results for the left leg.
All laboratory tests did not show any significant abnormalities.
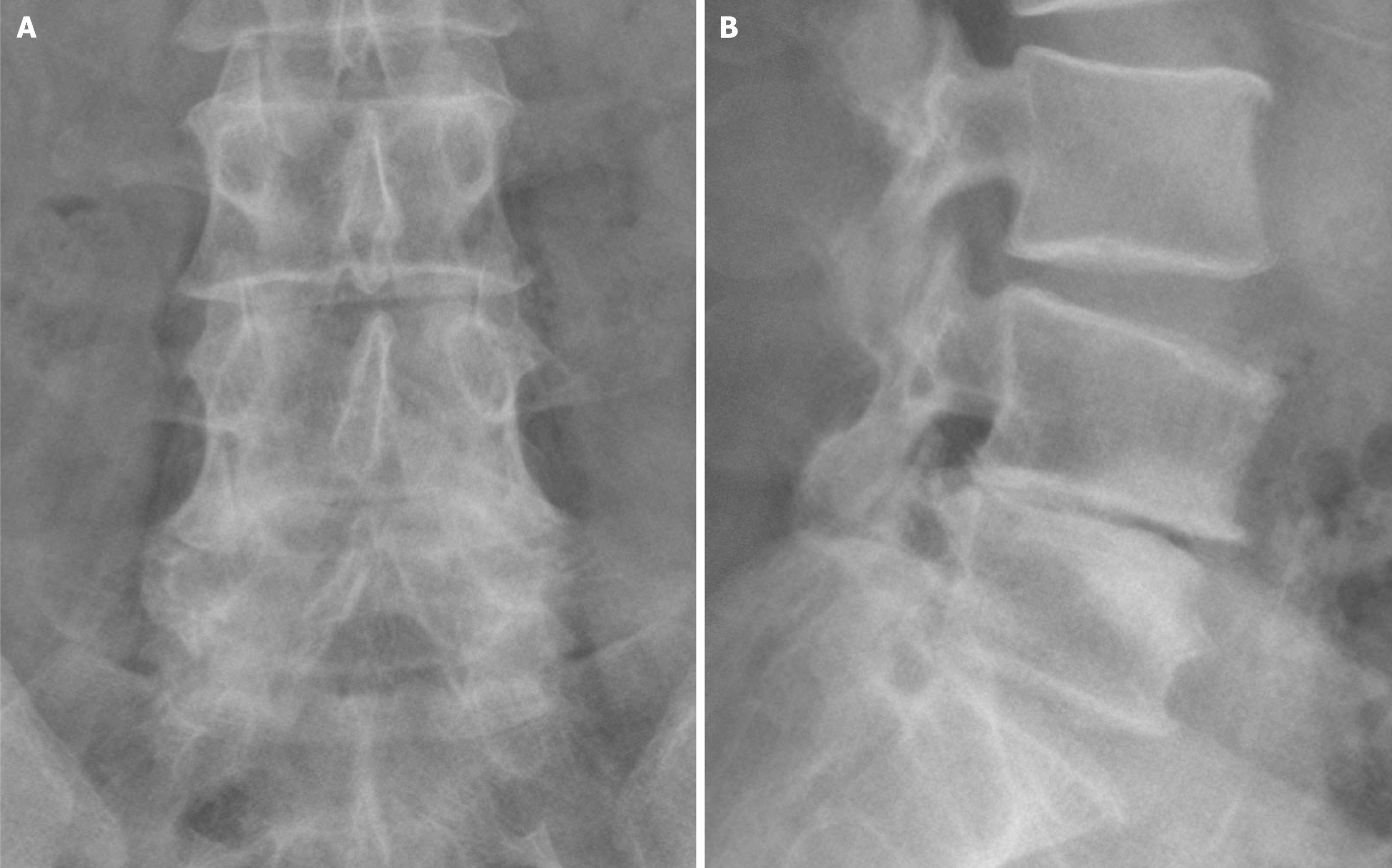
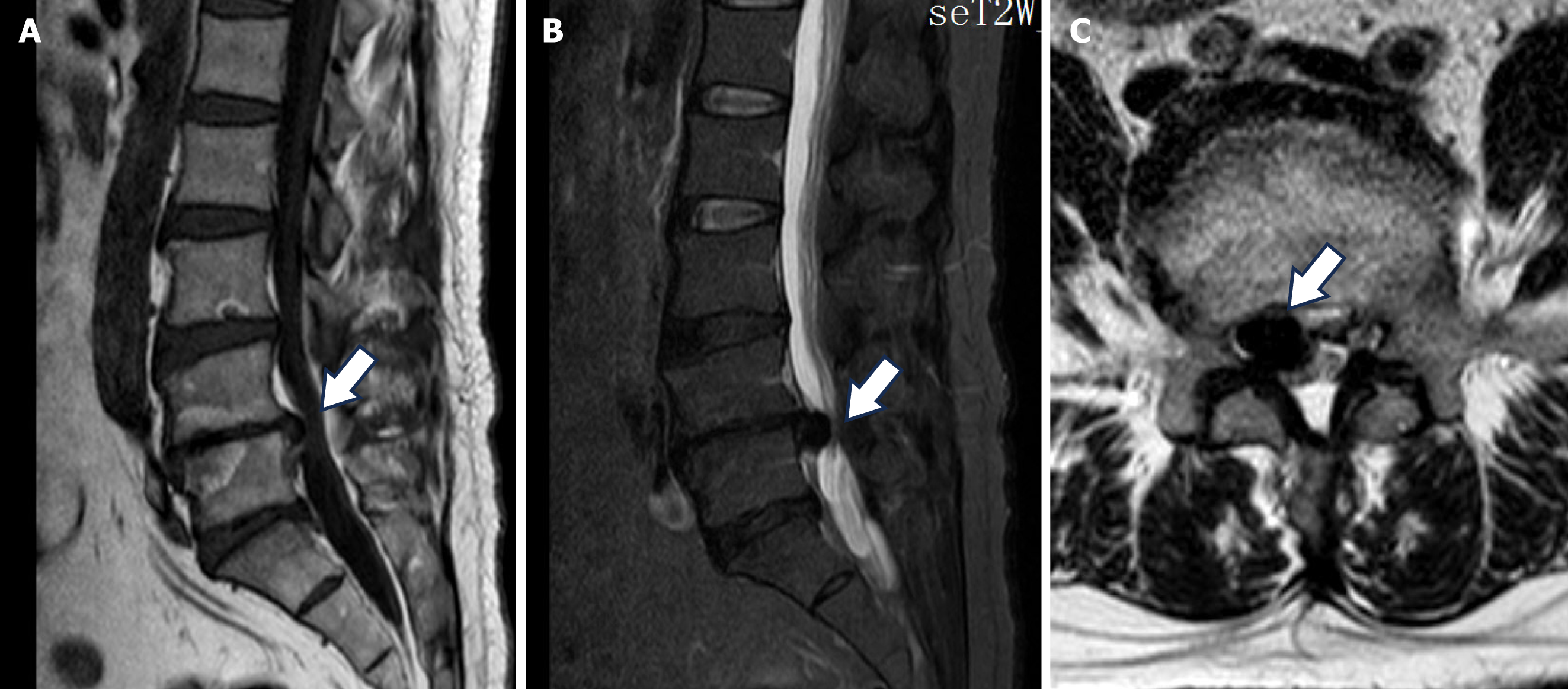
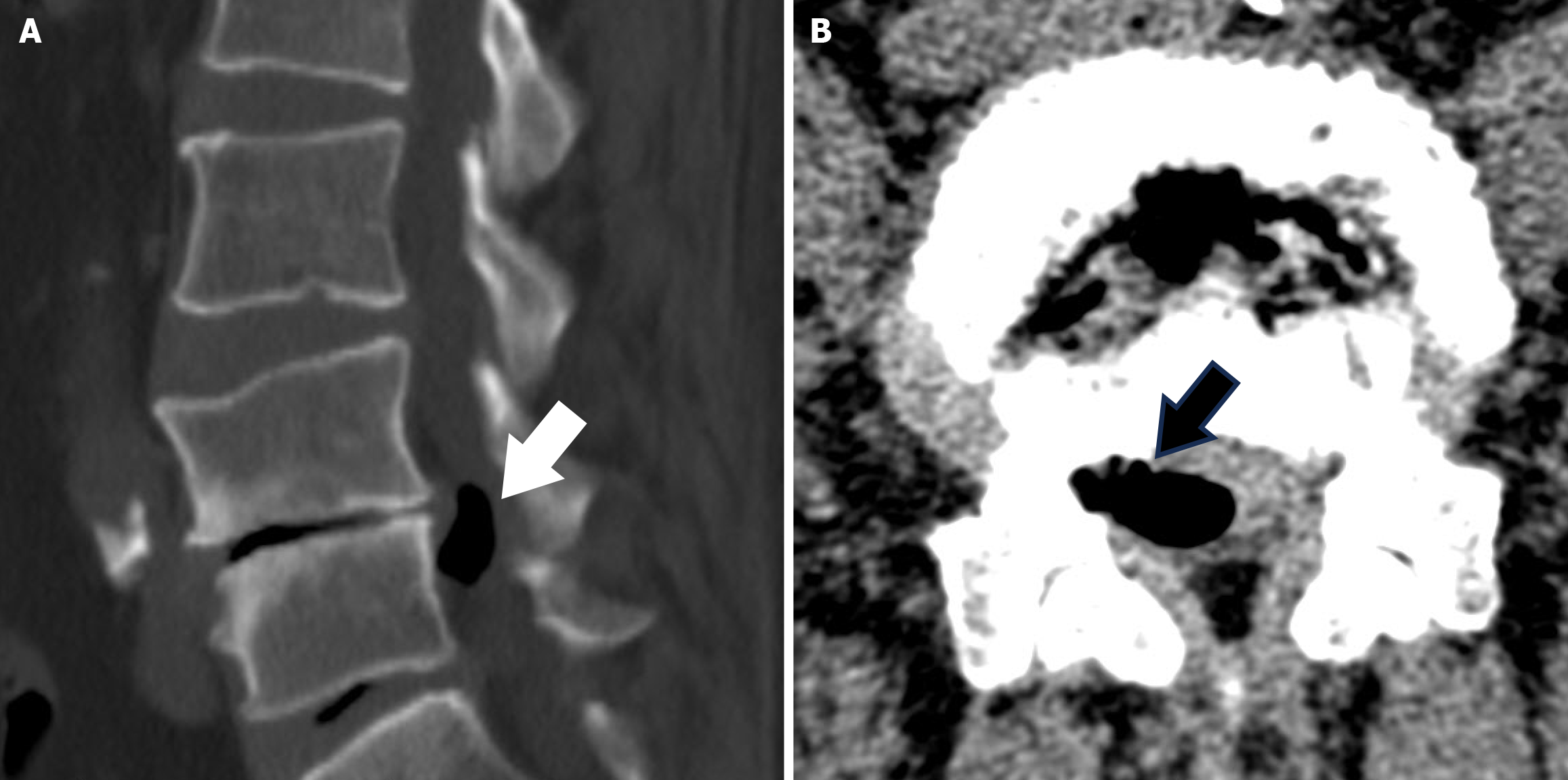
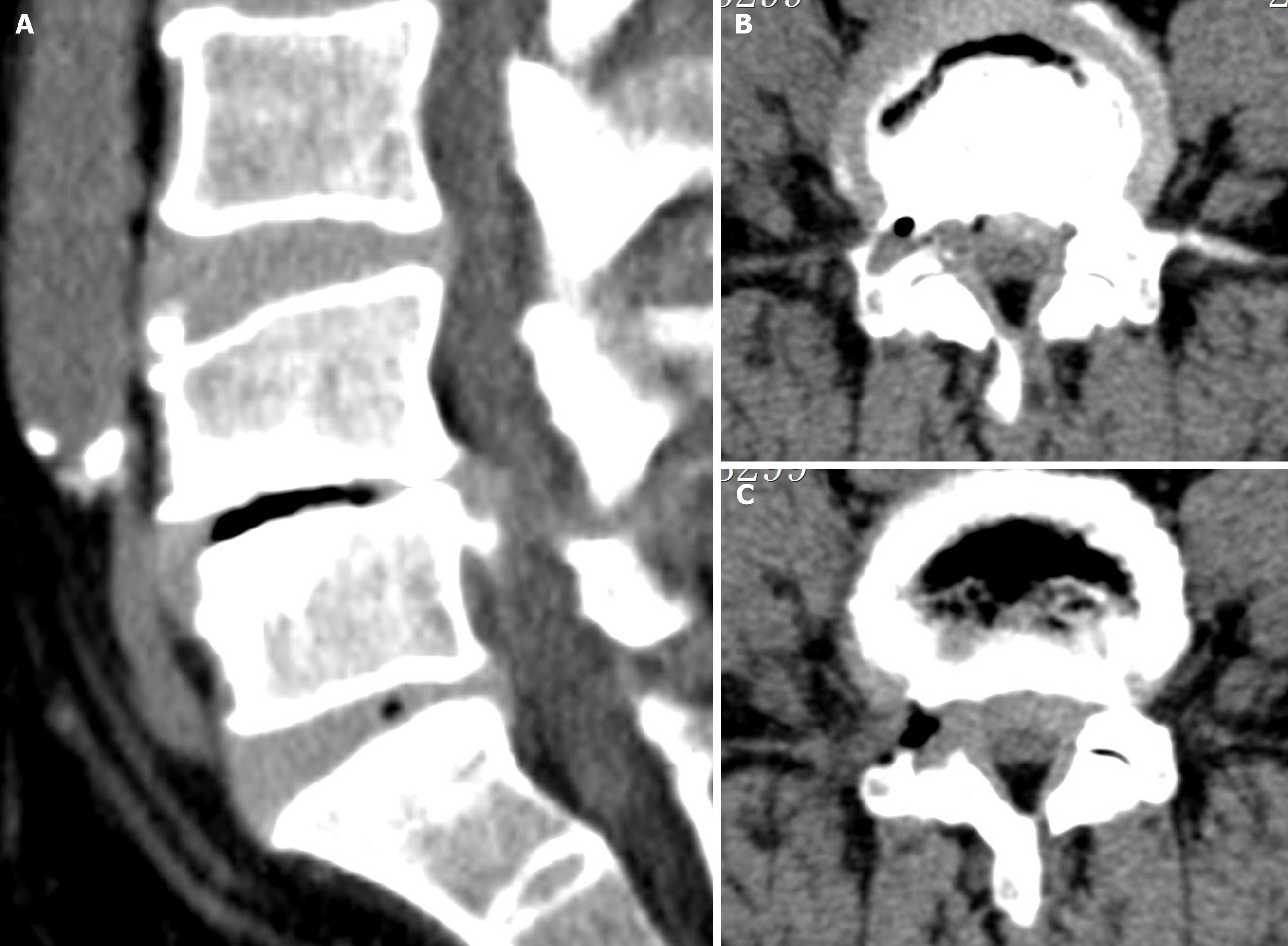
Radiography revealed a narrowed disc space at the L4/5 level (Figure 1). Magnetic resonance imaging (MRI) showed a mass with a low signal intensity in the epidural space on both T1-weighted (T1WI) and T2-weighted (T2WI) sequences (Figure 2). Axial MRI revealed a revealed that the mass compressing the right L5 nerve root. Computed tomography (CT) scans confirmed that the low-signal mass was gas, with Hounsfield units ranging from -1000 to -800. An intervertebral vacuum was observed at the L4/5 level (Figure 3).
Combined with the preoperative symptoms, physical exam, imaging, the final diagnosis of a gas-containing pseudocyst was confirmed.
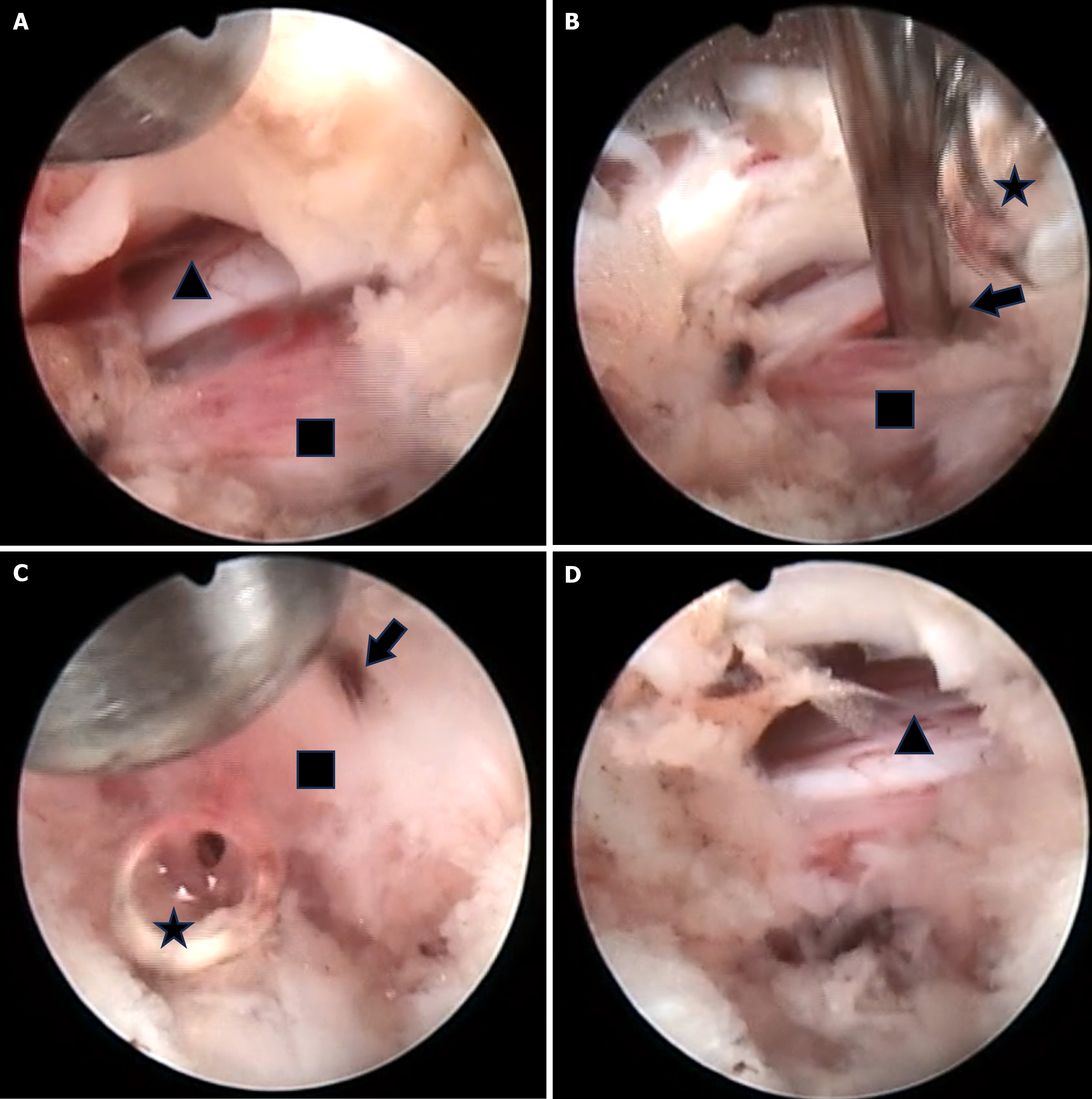
After other potential causes were ruled out, and PTE surgery was performed. The patient was placed in the left lateral decubitus position. A working tube was inserted at the L4/5 level under the guidance of C-arm radiography, and foraminoplasty was performed. After a portion of the ligamentum flavum was removed, the pseudocyst compressing the nerve root was exposed (Figure 4A). Moreover, air bubbles escaped from the pseudocyst when it was punctured with a probe (Video 1 demonstrates air bubbles escaping from the gas-containing pseudocyst when it was punctured).
In addition, fluid-like material also trickled out (Figure 4B and C). No disc-like tissue was observed within the pseudocyst. Subsequently, the pseudocyst wall was removed using a straight flexible grasper (Video 2 shows the air bubbles escaping from the gas-containing pseudocyst when the wall was removed). Connections with the intradiscal space were not observed during pseudocyst removal. The ventral space of the right L5 nerve root was completely decompressed (Figure 4D).
The patient's right leg pain disappeared postoperatively. Moreover, the straight leg raise test result was negative. Postoperative CT confirmed removal of the gas-containing pseudocyst (Figure 5). On the following day, the patient was discharged and returned to work. The numbness in the right leg returned to normal within 6 months. At the one-year follow-up after surgery, there was no symptom recurrence.
Gas-containing pseudocysts in the spinal canal are extremely rare[5-12]. The etiology and pathogenesis of pseudocysts are still not understood, and several hypotheses have been proposed to explain their underlying pathology. The most widely accepted theory suggests that the gas-containing pseudocysts originates from the degenerated disc, the effusion of fluid and gas from the herniated disc material, and triggers pseudocyst formation[15]. This case presentation further reinforces this notion, as evidenced by CT findings revealing that gas-containing pseudocysts are potentially associated with intervertebral vacuum phenomena[15]. However, several reports have mentioned that extradural abscesses, iatrogenic introduction of air during surgical or lumbar puncture procedures, or trauma may causes of gas-containing pseudocysts[9,11].
Gas-containing pseudocysts can be misdiagnosed as simple intervertebral disc herniations. Therefore, radiographic data are imperative. Although radiographic imaging of the lumbar spine fails to visualize pseudocysts, anteroposterior and lateral views are required. This is a quick and cost-effective initial examination that offers a critical assessment of alignment. CT and MRI revealed high values for evaluating pseudocyst manifestations. Gas-containing pseudocysts demonstrate a low signal intensity on both T1WI and T2WI, which may indicate calcification or air[7,10]. Subsequently, the diagnosis was confirmed using CT. Gas-containing pseudocysts are low-density on CT and typically measure less than zero Hounsfield units[8]. In this case report, the Hounsfield units ranged from -1000 to -800, and the presence of gas within the intervertebral disc and spinal canal were accurately identified and confirmed using CT images[7,8,10,12]. The presence of vacuum in the discs also served as additional evidence. Considering the clinical manifestations, physical examination finding, and radiographic evidence, a diagnosis of a gas-containing pseudocyst was considered. The escaped air of bubbles when the pseudocyst was punctured during the surgery confirmed the diagnosis.
The treatment approach depends on the patient’s symptoms. Surgery may not be necessary in the absence of early-stage symptoms. However, as the pseudocysts grow, patients may exhibit symptoms, such as back pain, numbness, or radiculopathy. Several authors recommended surgical intervention[8,10,16]. Although percutaneous puncture aspiration may relieve symptoms, it also predisposes patients to recurrence. Surgical intervention has an unequivocal clinical efficacy. The symptoms caused by compression of the lumbosacral nerve roots by the pseudocyst are often resolved or alleviated after excision[8,16]. PTE enables the meticulous resection of pseudocysts via a minimally invasive incision. Anatomical structures can be easily identified through PTE surgery, allowing for the meticulous manipulation the pathology through magnified endoscopic visualization and the acquisition of detailed surgical information[6,8]. The surgical incision was minimized, and the surrounding soft tissues were minimally disrupted. An et al[5] have reported the successful removal of a gas-containing pseudocyst using unilateral biportal endoscopy. All procedures were performed meticulously using a magnified endoscopic view. After careful dissection of the gap between the cyst and its surrounding structures, vivid endoscopic surgical images of the gas-containing pseudocysts were obtained. The walls of gas-containing cysts are extremely delicate and can easily rupture during traditional open surgical procedures, leading to their inadvertent absence of gas-containing pseudocysts. However, pseudocysts can be distinguished from the surrounding structures through endoscopic visualization, thereby minimizing neural injury. The diagnosis of a gas-containing pseudocyst was confirmed when the pseudocyst wall was punctured with a probe in the water releasing gas from the pseudocyst. Furthermore, the intraoperative straight leg raise test can be performed intraoperatively under local anesthesia, enabling the confirmation of successful pain relief and determination of the surgical effect.
However, this study had several limitations. First, the single case restricts the generalizability of the findings to a broader population. Second, the durability of surgical results requires long-term follow-up. Despite these limitations, this study provides valuable insights and a basis for further investigation.
The case suggests that when diagnosing lumbar radiculopathy, it is crucial to consider the presence of epidural gas within the spinal canal. A combination of preoperative MRI and CT can help distinguish gas-containing pseudocysts from other conditions. PTE provides exceptional surgical visualization and precise operative manipulation and serves as a minimally invasive treatment approach for gas-containing pseudocysts in the intervertebral foramen.
| 1. | Schoenfeld AJ, Laughlin M, Bader JO, Bono CM. Characterization of the incidence and risk factors for the development of lumbar radiculopathy. J Spinal Disord Tech. 2012;25:163-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Patriat Q, Prigent FV, Aho S, Lenfant M, Ramon A, Loffroy R, Lambert A, Ornetti P. Diagnostic Value of an Additional Sequence (Large-Field Coronal Stir) in a Routine Lumbar Spine MR Imaging Protocol to Investigate Lumbar Radiculopathy. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 3. | Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, Cho CH, DePalma MJ, Dougherty P 2nd, Fernand R, Ghiselli G, Hanna AS, Lamer T, Lisi AJ, Mazanec DJ, Meagher RJ, Nucci RC, Patel RD, Sembrano JN, Sharma AK, Summers JT, Taleghani CK, Tontz WL Jr, Toton JF; North American Spine Society. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014;14:180-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 397] [Article Influence: 36.1] [Reference Citation Analysis (0)] |
| 4. | Şakir Ekşi M, Ece Özcan-Ekşi E, Orhun Ö, Akkaş A, Harun Yaşar A, Zarbizada M, Canbolat Ç, Güdük M, Bozkurt B, İmre Usseli M, Erşen-Danyeli A, Hamit Aytar M, Kalelioğlu M, Özgen S, Necmettin Pamir M, Benzel EC. Could gas-filled pseudocyst mimick extruded disc herniation? J Clin Neurosci. 2021;93:147-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | An JW, Lee CW. Surgical Treatment of Extraforaminal Gas-Containing Pseudocyst Compressing L5 Nerve Root by Using Unilateral Biportal Endoscopy. World Neurosurg. 2019;124:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Zhu K, He D. Transforaminal percutaneous endoscopic discectomy for symptomatic gas-filled discal cysts-report of three cases and literature review. J Orthop Surg Res. 2021;16:251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Okuyama K, Kido T, Miyakoshi N, Shimada Y. Histological demonstration of the gas precursor in a symptomatic L5-S1 disc herniation containing gas: A case report. Acta Orthop Traumatol Turc. 2020;54:647-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Zhu B, Jiang L, Liu XG. Transforaminal Endoscopic Decompression for a Giant Epidural Gas-Containing Pseudocyst: A Case Report and Literature Review. Pain Physician. 2017;20:E445-E449. [PubMed] |
| 9. | Lee CW, Yoon KJ, Ha SS, Kang JK. Radicular compression by intraspinal epidural gas bubble occurred in distant two levels after lumbar microdiscectomy. J Korean Neurosurg Soc. 2014;56:521-526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Hidalgo-Ovejero AM, García-Mata S, Gozzi-Vallejo S, Izco-Cabezón T, Martínez-Morentín J, Martínez-Grande M. Intradural disc herniation and epidural gas: something more than a casual association? Spine (Phila Pa 1976). 2004;29:E463-E467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Guo J, Ma X, Liu Y, Li G, Wang D, Wang Z, Li S. Dura sac compression due to spinal epidural gas pseudocyst after lumbar decompression surgery: a case report. BMC Musculoskelet Disord. 2019;20:296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Akhaddar A, Eljebbouri B, Naama O, Boucetta M. Sciatica due to lumbar intraspinal gas pseudocyst. Intern Med. 2010;49:2647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Kakitsubata Y, Theodorou SJ, Theodorou DJ, Yuko M, Ito Y, Yuki Y, Wada S, Maehara T. Symptomatic epidural gas cyst associated with discal vacuum phenomenon. Spine (Phila Pa 1976). 2009;34:E784-E789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Bosser V, Dietemann JL, Warter JM, Granel de Solignac M, Beaujeux R, Buchheit F. L5 radicular pain related to lumbar extradural gas-containing pseudocyst. Role of CT-guided aspiration. Neuroradiology. 1990;31:552-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Yoshida H, Shinomiya K, Nakai O, Kurosa Y, Yamaura I. Lumbar nerve root compression caused by lumbar intraspinal gas. Report of three cases. Spine (Phila Pa 1976). 1997;22:348-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Clark R, Weber RP, Kahwati L. Surgical Management of Lumbar Radiculopathy: a Systematic Review. J Gen Intern Med. 2020;35:855-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |