Published online Feb 18, 2025. doi: 10.5312/wjo.v16.i2.102483
Revised: December 17, 2024
Accepted: January 14, 2025
Published online: February 18, 2025
Processing time: 116 Days and 5.8 Hours
Pelvic fractures are often associated with significant morbidity, including injuries to the urinary tract. Understanding the incidence and risk factors for urinary tract injury in these patients is crucial for prompt diagnosis and management. This meta-analysis aims to synthesize existing evidence to determine the overall inci
To determine the incidence and risk factors for urinary tract injuries in patients with pelvic fractures.
A systematic search of PubMed, EMBASE, Scopus, and the Cochrane Library was conducted without date restrictions. Studies examining the incidence and risk factors of urinary tract injuries in patients with pelvic fractures were included. Data extracted included demographics, injury mechanism, pelvic fracture type, urinary tract injury incidence, mortality, and discharge disposition. Review Mana
Ten studies comprising 22700 patients were included. The pooled incidence of urinary tract injury associated with pelvic fracture was 6.88% (95%CI: 6.20%-7.55%). Vehicle, motorcycle, and pedestrian accidents were identified as risk fac
Urinary tract injury occurs in nearly 7% of patients with pelvic fractures. Motorcycle accidents, pubic fractures, and pelvic ring disruptions are significant risk factors. Urinary tract injury following pelvic fracture is associated with increased mortality.
Core Tip: This meta-analysis investigates the incidence of urinary tract injuries associated with pelvic fractures, revealing a prevalence of 6.88%. It identifies key risk factors, including vehicle and motorcycle accidents, and highlights the significant associations between specific fracture types, such as pubic fractures and pelvic ring disruptions, and urinary injuries. The findings underscore the importance of early detection and intervention to reduce morbidity and mortality in affected patients.
- Citation: Mariscal G, Dway A, Barrios C. Hidden dangers of pelvic fracture: A meta-analysis on urinary tract injury incidence and risk factors. World J Orthop 2025; 16(2): 102483
- URL: https://www.wjgnet.com/2218-5836/full/v16/i2/102483.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i2.102483
Pelvic fractures are a significant consequence of high-energy trauma and are often observed in patients who have suffe
Owing to the potential severity of pelvic fractures, early diagnosis and treatment are essential[5]. In many cases, pelvic fractures require surgery to repair the damage and restore function of the affected organs and structures. It is also essential to involve a multidisciplinary team of surgeons, including urologists and colorectal surgeons, in the treatment of pelvic fractures to ensure that all injuries are appropriately managed[6]. The diagnosis of pelvic fractures can be cha
The treatment of pelvic fractures can be complicated and management often requires a significant amount of resources. The direct cost of pelvic fractures can be significant, with estimates ranging from $30000 to $50000 per patient[7]. Additionally, the indirect costs of pelvic fractures, including lost wages, can be significant, particularly for young patients[7,8].
Given the complexity and potential severity of pelvic fractures, it is essential to identify the risk factors and trends in associated injuries to improve early detection and management. Several studies have identified predictors of mortality in patients with pelvic fractures, including age, Injury Severity Score, and blood transfusion[1,9]. However, research on the association between pelvic fractures and genitourinary injuries[10].
This meta-analysis aimed to determine the actual incidence of genitourinary injuries associated with pelvic fractures and to identify risk factors or associations that may help surgeons detect these injuries early. By identifying these factors, surgeons can improve the management of pelvic fractures and reduce morbidity and mortality associated with these injuries.
In this study, a protocol was established to guide the justification of the study, inclusion criteria, literature search, data extraction, and outcome assessment. The study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines to ensure transparency and completeness in reporting[11]. The search strategy followed the PICOS framework, where P referred to patients with pelvic fractures and urinary tract injury, I referred to studies that included patients with pelvic fractures and urinary tract injury, C referred to patients with pelvic fractures without urinary tract injury, O referred to the outcomes of interest, including the incidence of pelvic-fracture-associated urinary tract injury and risk factors, and S referred to studies that analyzed these incidence rates. These criteria were used to ensure that the studies included in the analysis were directly relevant to the research question and that the results were comparable and interpretable. Exclusion criteria were duplicate data, incomplete data, studies that did not share variable and studies with a high risk of bias.
The following information sources were used to conduct this meta-analysis: PubMed, EMBASE, Scopus, and the Co
We used the following search terms to search all studies registers and databases: ((pelvic fracture AND urinary tract) OR (pelvic fracture AND bladder)) OR (pelvic fracture AND urethra). Two reviewers independently agreed on selection of eligible studies and achieved consensus on which studies to include.
Regarding data extraction, two authors also independently reviewed the studies. An initial screening of titles and abstracts was performed to eliminate studies that were obviously outside the scope of the review. In cases of uncertainty based on title or abstract, the full text of each article was examined for further evaluation. If consensus was not reached, a third review author was asked to complete the data extraction form and discuss the article with the other two authors until consensus was reached. All disagreements were resolved by discussion. Data extraction was performed by two reviewers via an Excel spreadsheet. The baseline characteristics of each study were obtained: Study, type of study, region, period, number of participants, and number of patients with urinary tract injuries. The primary outcome was the inci
The risk of bias in the included studies was evaluated using the Methodological Index for Non-Randomized Studies[12]. A maximum score of 24 was assigned to comparative studies, while non-comparative studies were rated on a scale of 0-16. A score of 0-4 was considered very low quality, 5-7 as low quality, 8-12 as fair quality, and ≥ 13 as high quality for non-comparative studies. For comparative studies, a score of 0-6 was considered very low quality, 7-10 as low quality, 11-15 as fair quality, and ≥ 16 as high quality[12]. Two reviewers independently evaluated the studies, and in cases where there was a lack of consensus in the scoring, a third reviewer was consulted to resolve any discrepancies (Supplementary Table 1).
For the statistical analysis, we used the Review Manager 5.4 software package provided by the Cochrane Collaboration. Pooled incidences with 95%CI were calculated using a random-effects model. Since the SE was not reported, we calcu
To assess the risk of bias across the studies, we used the Review Manager software package to conduct a visual inspection of the funnel plots and interpret them accordingly. Funnel plots are graphical representations of the relationship between effect size and sample size. They can be used to identify potential publication bias or other sources of heterogeneity across the studies. We visually inspected the funnel plots and interpreted any asymmetry as a potential indication of publication bias[14].
To assess the robustness of our findings, we conducted a sensitivity analysis using the Review Manager 5.4 software package. Specifically, we eliminated the top-weight study from the comparisons in all outcomes to evaluate the consis
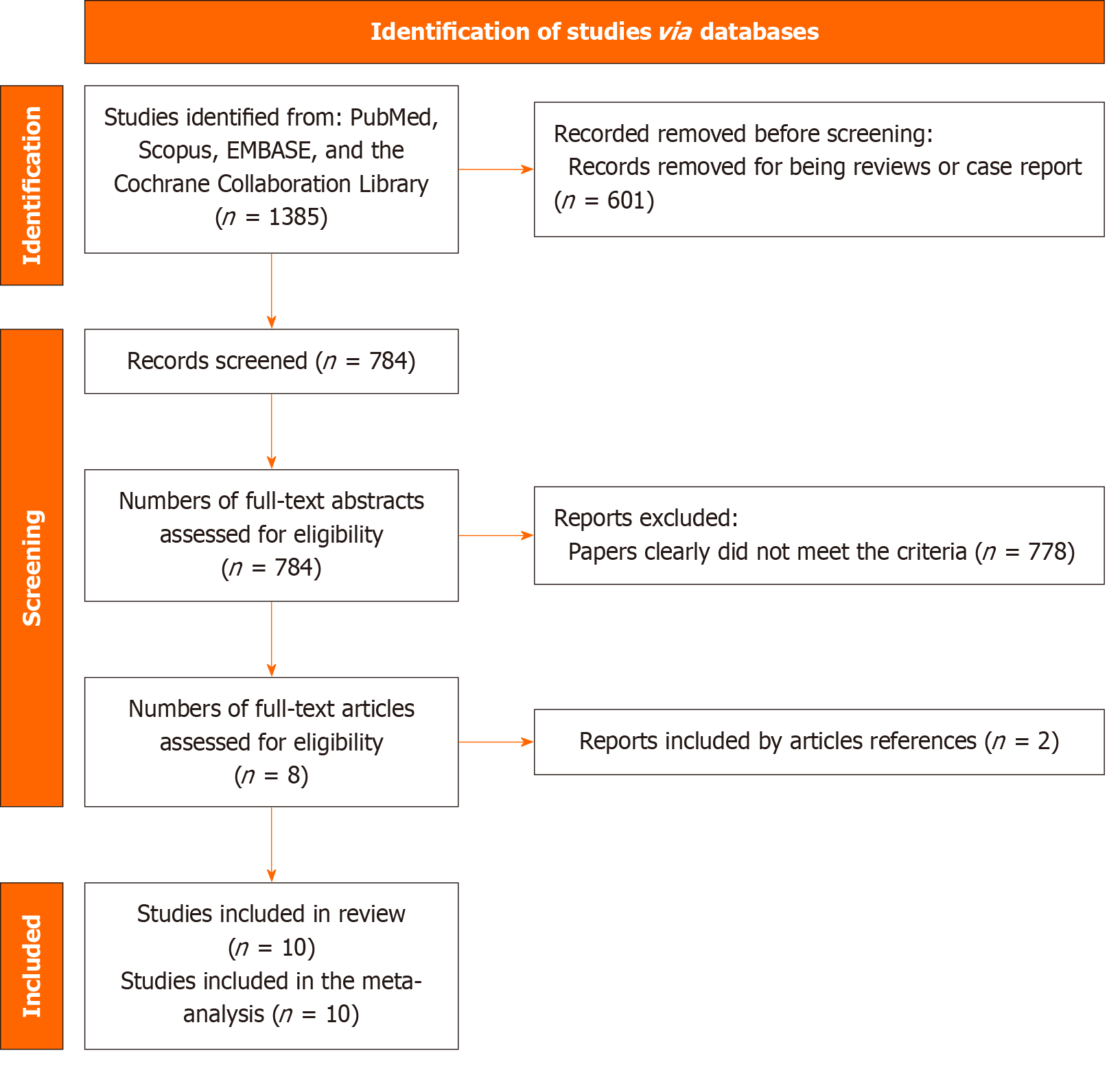
The initial search yielded 1385 results, from which review studies and case reports were eliminated, resulting in a total of 784 articles. After reviewing the titles and abstracts, eight articles met the inclusion criteria. After reviewing the references of the included articles, we then found two additional studies that met the inclusion criteria. Thus, 10 studies were included in the meta-analysis (Figure 1)[2,8,10,15-21].
Table 1 shows the main characteristics of the included studies[2,8,10,15-21]. These 10 studies included a pool of 22700 patients. Eight studies were published in the United States, one in Egypt, and one in the United Kingdom. Seven articles were cohort studies, and one of the studies was prospective. The follow-up period varied among the studies, but all had at least 1 year of follow-up. Ages ranged from 12 to 59 years. Gender varied because some articles focused on a certain gender (two studies focused only on men, and one study focused only on women). Two studies focused on bladder injuries, two studies on urethral injuries, and six studies on the entire genitourinary tract. For the non-comparative studies, the quality of the studies was low (two studies) or very low (one study). For the comparative studies, one study presented low quality, four presented fair quality, and two presented high quality.
| Ref. | Region | Type of study | Period | Age | Male | Patients, n | Urinary tract injury, n |
| Avey et al[17], 2006 | United States | Retrospective cohort | 1997-2003 | 37 | 448 | 783 | 36 |
| Bjurlin et al[20], 2009 | United States | Retrospective cohort | 2001-2005 | NA | NA | 29936 | 1444 |
| Bott et al[21], 2022 | United Kingdom | Retrospective serie | 1994-2005 | 59 | 177 | 177 | 5 |
| Delaney et al[19], 2016 | United States | Retrospective cohort | 2010-2012 | 12 | 0 | 2639 | 81 |
| Demetriades et al[8], 2002 | United States | Retrospective cohort | 1993-2000 | 37 | 937 | 1545 | 90 |
| Hochberg et al[15], 1993 | United States | Retrospective serie | 1993 | 39 | 53 | 103 | 10 |
| Johnsen et al[2], 2017 | United States | Retrospective cohort | 2000-2014 | NA | 3416 | 5518 | 233 |
| Koraitim et al[16], 1996 | Egypt | Prospective serie | 1990-1992 | 31 | 203 | 203 | 51 |
| Lowe et al[18], 1988 | United States | Retrospective cohort | 1979-1985 | NA | 405 | 405 | 21 |
| Velazquez et al[10], 2020 | United States | Retrospective cohort | 2010-2014 | 35 | NA | 180931 | 6140 |
The incidence of urinary tract anomalies associated with pelvic fracture was 6.88% (95%CI: 6.20%-7.55%). Among the studies that could be compared, female sex was not a risk factor (OR 1.39, 95%CI: 0.22-8.94). In contrast, Demetriades et al[8] showed that male sex was an increased risk of urinary tract injury (RR 1.8 95%CI: 1.1-2.8; P = 0.01).
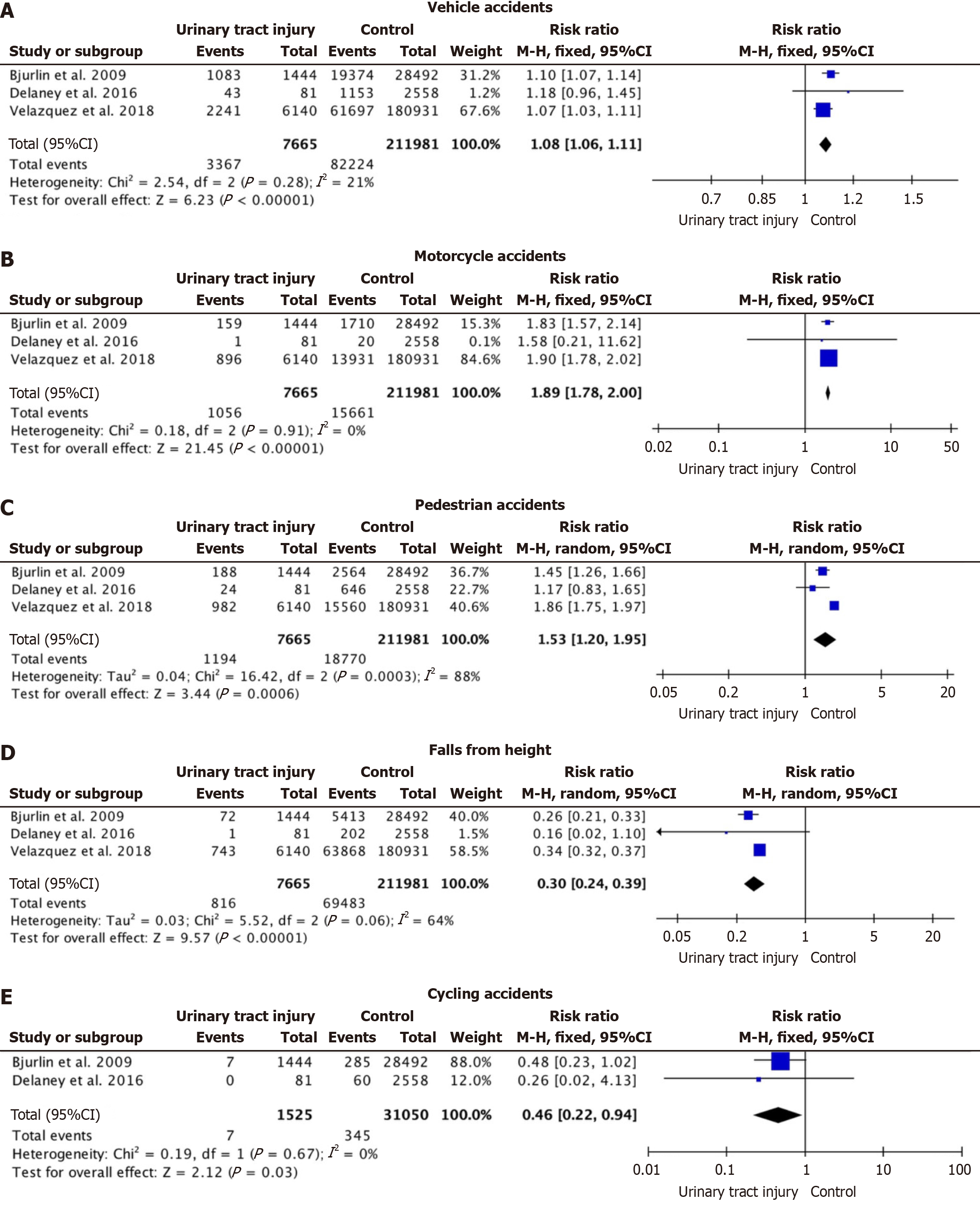
Regarding the mechanism of injury (Figure 2), vehicle accidents, motorcycle accidents, and pedestrian accidents were risk factors for urinary tract injury: (RR 1.08, 95%CI: 1.06-1.11; participants = 220251; studies = 4; I2 = 21%), (RR 1.89, 95%CI: 1.78-2.00; participants = 219646; studies = 4; I2 = 21%), and (RR 1.53, 95%CI: 1.20-1.95; participants = 219646; studies = 4; I2 = 88%), respectively. In contrast, falls from height or cycling accidents were more frequent in the control group without urinary tract damage: (RR 0.30, 95%CI: 0.24-0.39; participants = 219646; studies = 4; I2 = 64%) and (RR 0.46, 95%CI: 0.22-0.94; participants = 32575; studies = 2; I2 = 0%), respectively.
Regarding individual studies, Hochberg and Stone[15], and Johnsen et al[2] showed similar proportions. Hochberg and Stone[15] showed 49% of urinary tract injuries in pelvic fractures were pedestrian accidents and up to 32% in vehicle and 7% in motorcycle accidents. Johnsen et al[2] showed 47% vehicle accidents, 17% motorcycle, and 8% pedestrian. Koraitim et al[16] observed that traffic accidents accounted for up to 71% of occurrences and falls from height for 25%. For Deme
Regarding hemodynamic instability, patients with urinary tract injury when in emergency departments did not present greater hemodynamic instability (OR 0.99, 95%CI: 0.03-36.08; studies = 3). Hochberg and Stone[15] observed that 23% of patients with urinary tract injury showed hypotension (less than 90 mmHg). There was also no difference with respect to the Glasgow Coma Scale (GSC) (OR 2.54, 95%CI: 0.60-10.69; studies = 2).
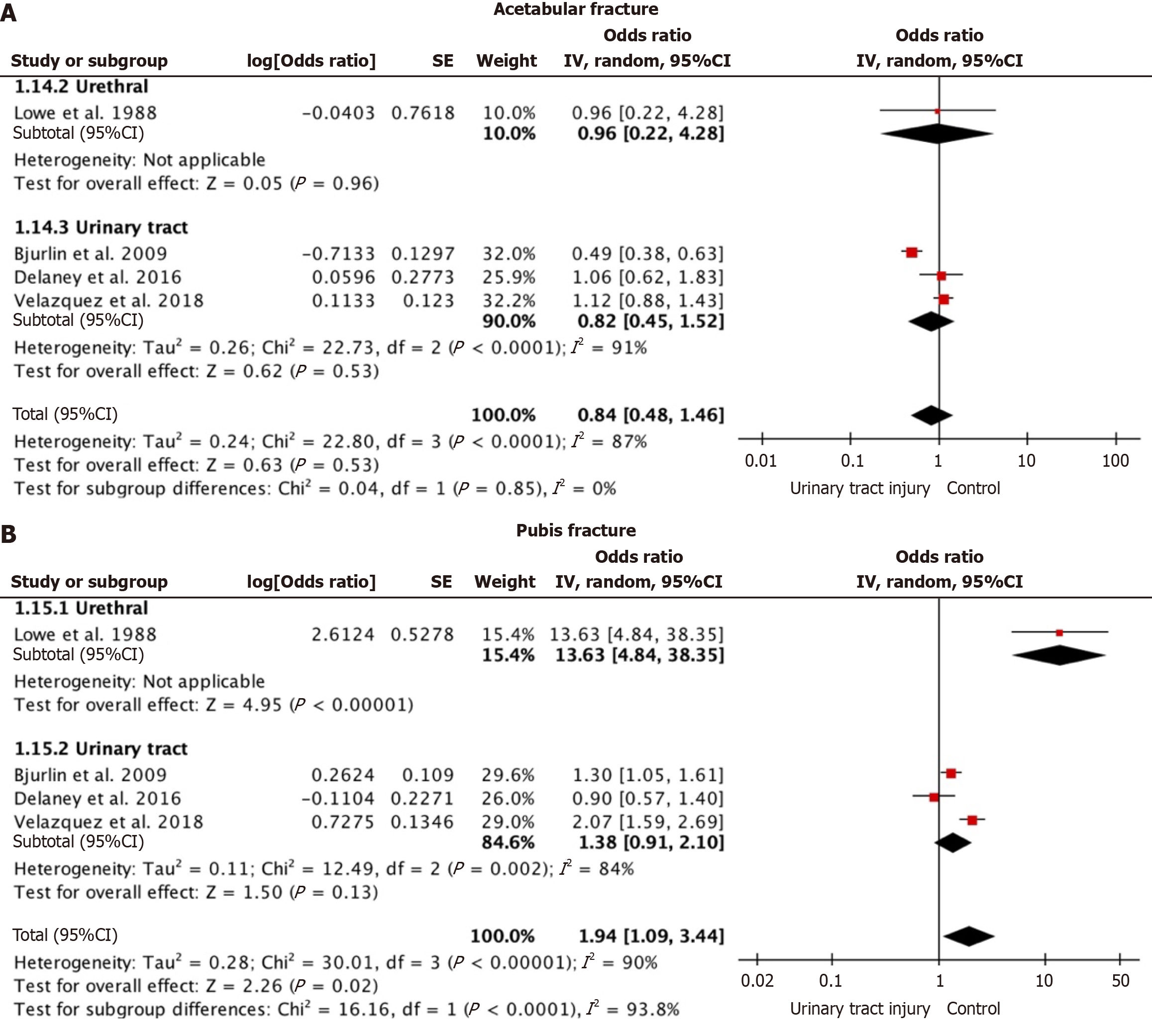
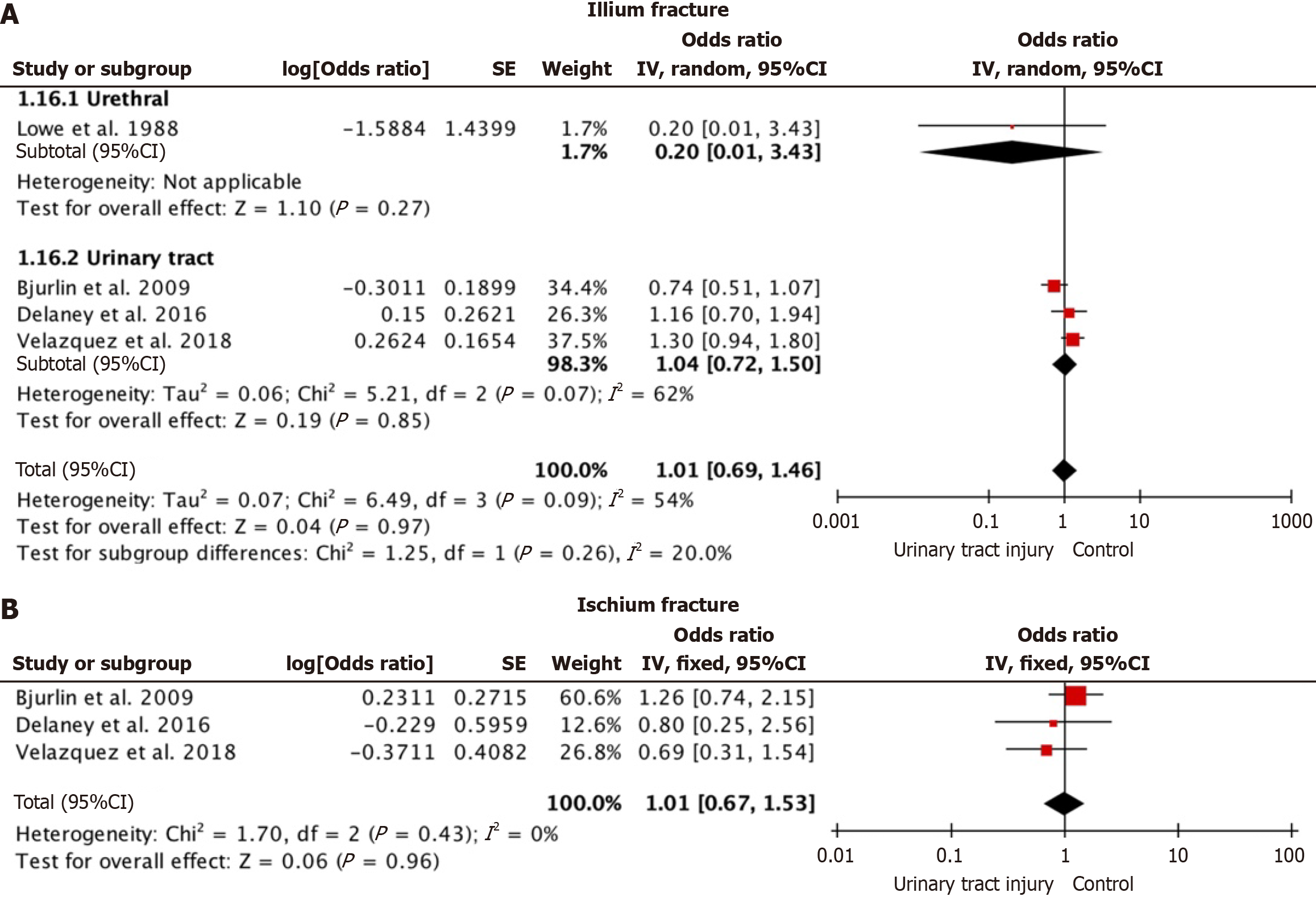
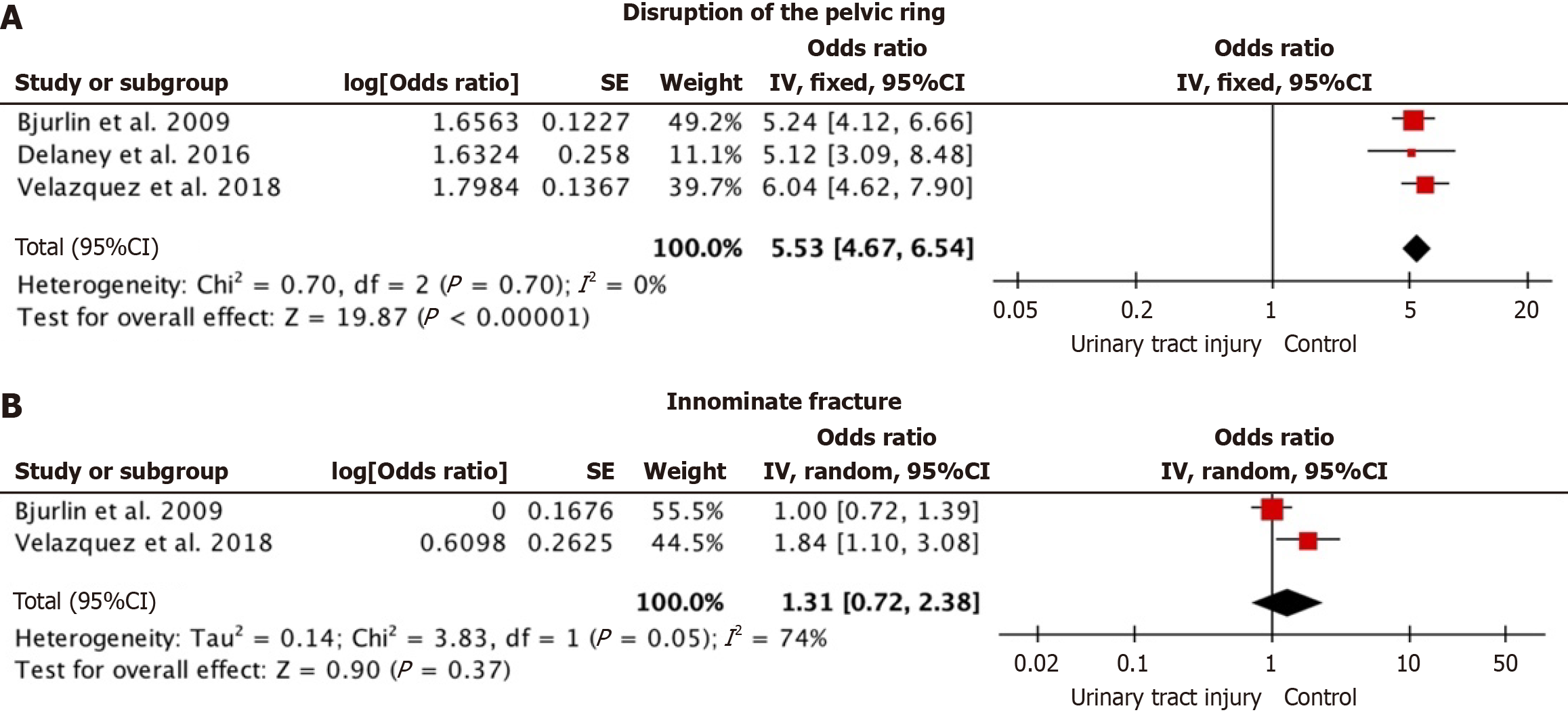
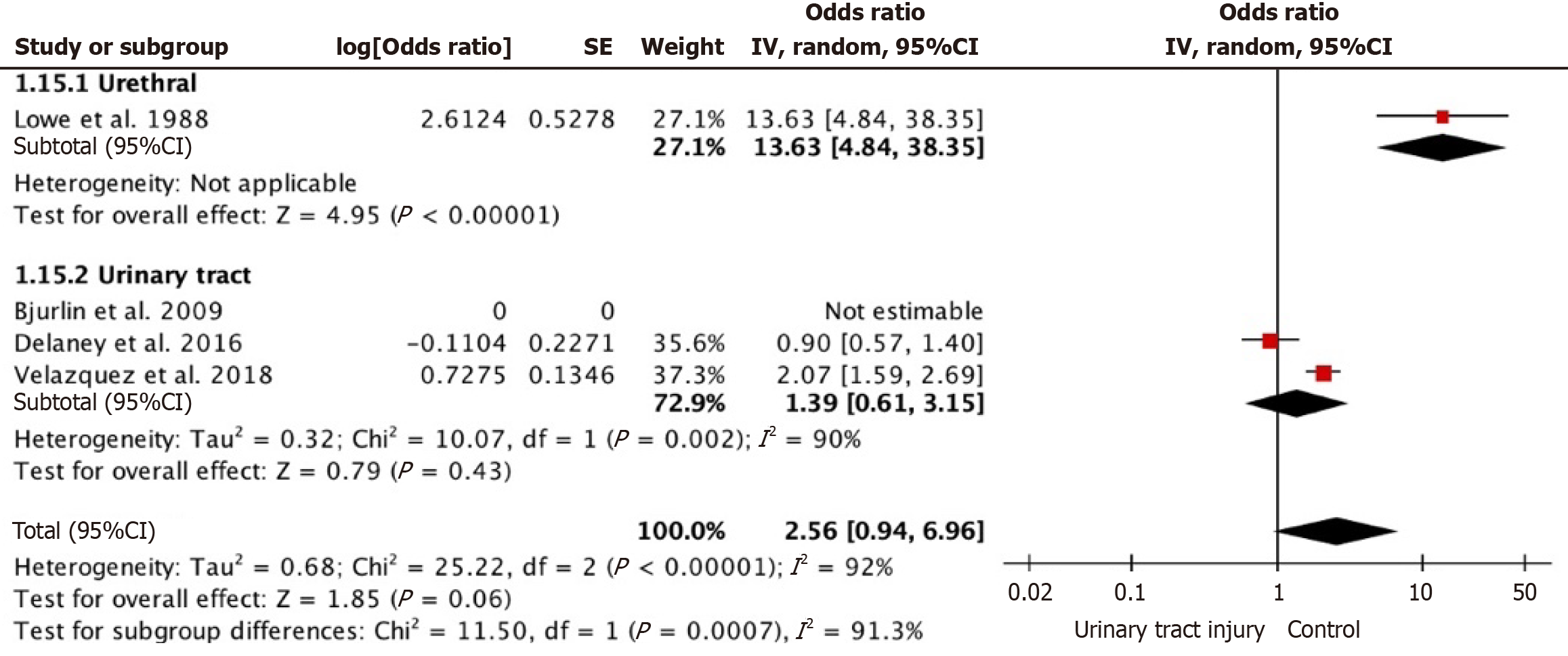
Regarding the type of fractures with a higher risk of urinary tract injury, acetabulum fractures did not show an increased risk (OR 0.84, 95%CI: 0.48-1.46; studies = 5) (Figure 3A). Pubic fractures did show a risk factor (OR 1.94, 95%CI: 1.09-3.44; studies = 4) (Figure 3B); however, when subgroup analysis was performed, pubic fractures were significantly more associated with specific urethral injury (OR 13.63, 95%CI: 4.84-38.35) vs complete urinary tract injury (OR 1.38, 95%CI: 0.91-2.10). Fractures of the ilium did not show an increased risk (OR 1.01, 95%CI: 0.69-1.46; studies = 4) (Figure 4A). Likewise, ischium fractures were not shown to be a risk factor (OR 1.01, 95%CI: 0.67-1.53; studies = 3) (Figure 4B). Pelvic ring disruption showed an increased incidence of associated urinary tract injury (OR 5.53, 95%CI: 4.67-6.54; studies = 3) (Figure 5A). Finally, innominate/pelvic rim fracture did not show an increased risk of associated urinary tract injury (OR 1.31, 95%CI: 0.72-2.38; studies = 2) (Figure 5B).
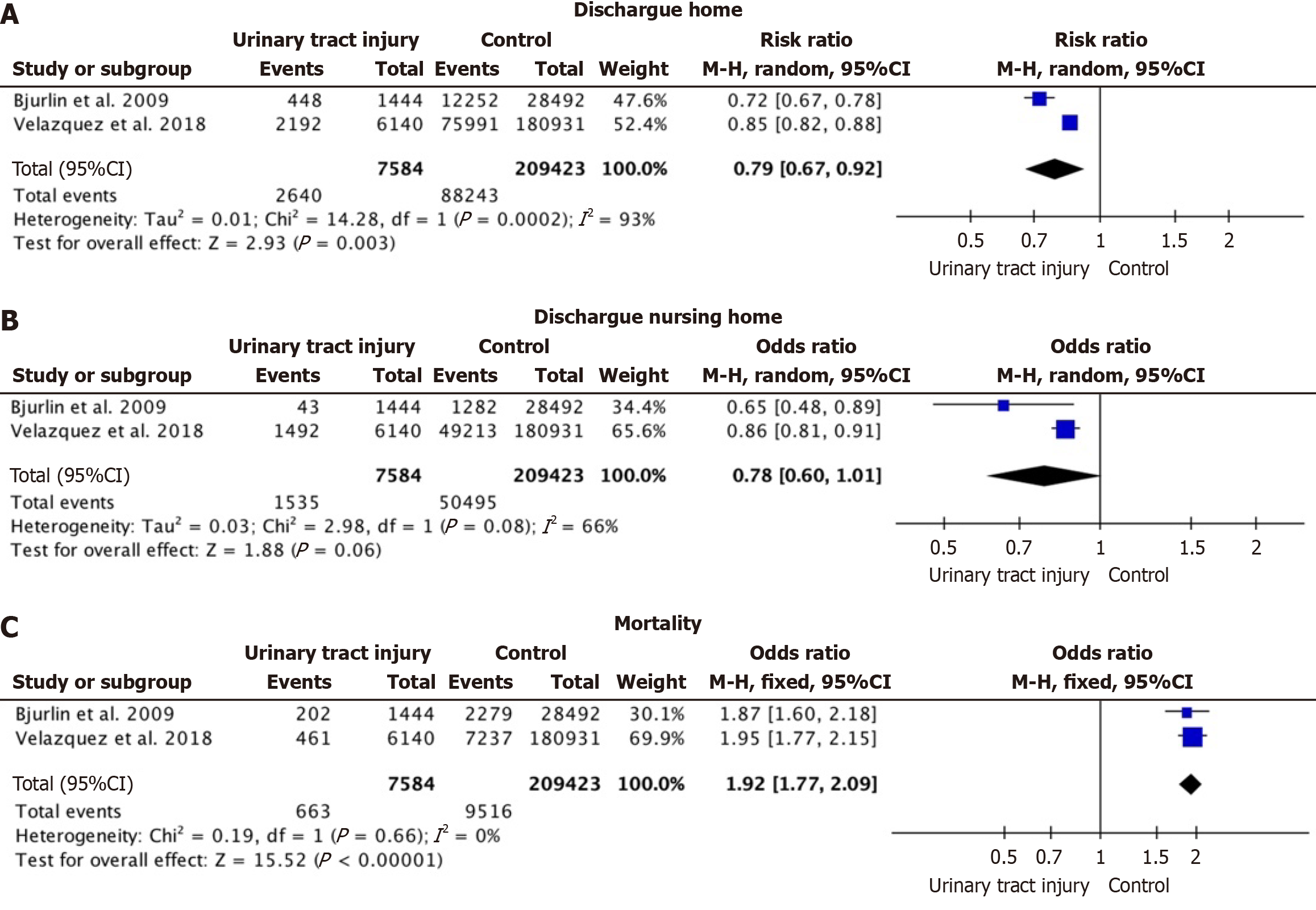
In relation to discharge, patients without urinary tract injury were more likely to discharge home (RR 0.79, 95%CI: 0.67-0.92; participants = 217007; studies = 2; I2 = 93%) (Figure 6A), but there were no differences with respect to those dischar
There were other variables analyzed by individual studies or series that did not compare the results. For one, macro- or microscopic hematuria was detected in 25% and 59% of patients, respectively, by Hochberg and Stone[15]. In the case of Avey et al[17] all patients with bladder rupture presented hematuria. Regarding the length of stay (LOS), Hochberg and Stone[15] observed a mean of 27 days (range 8 to 80 days). Moreover, Velazquez et al[10] observed significant differences with respect to LOS. Patients with urinary tract injury 14.5 days and without urinary tract injury 9.1 days (P < 0.01), with urinary tract injury patients spending an average of 8.5 days in the intensive care unit (ICU) vs 7.1 days for patients without associated urinary tract injuries (P < 0.01)[10]. Bjurlin et al[20] also observed differences between those with and without urinary tract injuries in terms of total LOS and ICU stay. In total LOS, those with urinary tract injuries had on average 10 days vs 6 days for those without such injuries; in ICU stay, those with urinary tract injuries had 3 days vs only 1 day on average for those without such injuries[20]. Finally, the number of patients undergoing surgical exploration was nine of 10 (90%) for bladder ruptures in the study by Hochberg and Stone[15], while Velazquez et al[10] observed that 1658 of 6140 (27%) patients with urinary tract injury underwent repair surgery.
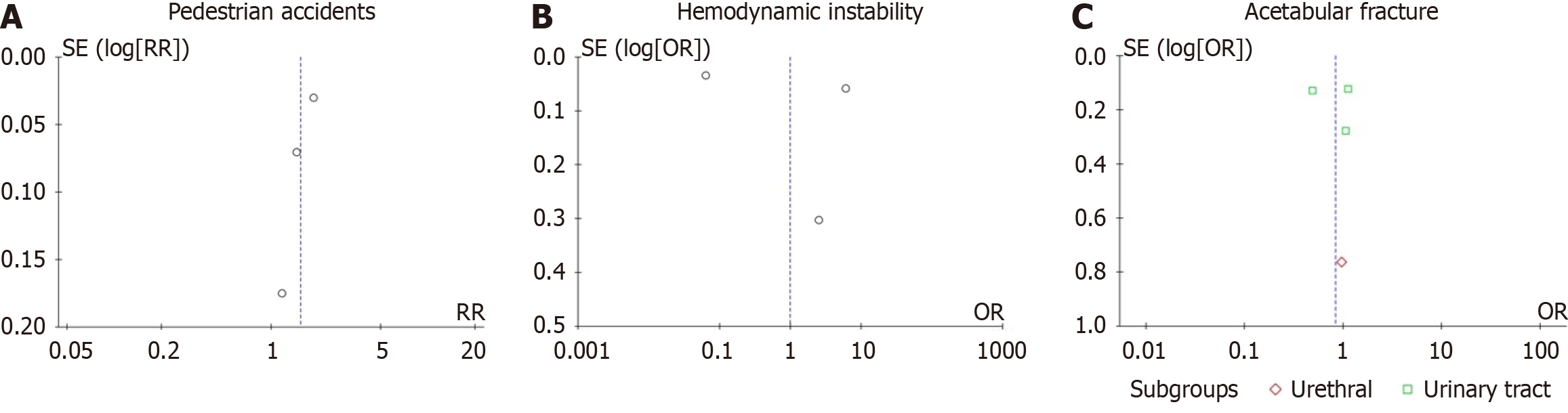
Regarding the sensitivity analysis, the variables shared by only two studies that were compromised when the study with the highest weight was eliminated and changed the direction of the overall results were innominate/pelvic rim fracture and discharge to nursing home. Pubic fracture also changed the direction of the overall results when the top-weighted study was removed (Figure 7). The publication bias analysis using funnel plots showed asymmetry, which indicated publication bias (Figure 8).
This study is a meta-analysis that examined the incidence and trends of urinary injuries related to pelvic fractures. The meta-analysis showed that the overall incidence of urinary tract injury associated with pelvic fracture was 6.88%. Vehicle accidents, motorcycle accidents, and pedestrian accidents were closely associated with urinary injury. Additionally, patients with urinary injury did not present greater hemodynamic instability. Also, pubic fractures together with pelvic ring disruptions were factors that increased the frequency of associated urinary injury. The quality of the non-comparative studies was low, but the quality was fair for most of the comparative studies. It is important not to underestimate the incidence of urinary injuries associated with pelvic fractures because previous studies warn of the associated morbidity[6].
With respect to the rupture or lesions of the bladder, in the studies that described these in isolation, the incidence observed was 7.15%. Extraperitoneal ruptures are produced by bone spicules or shearing although injuries by bone fragments explain only 35% of the cases[17]. In contrast, intraperitoneal injuries usually occur when the bladder is distended[5]. Approximately 30% of bladder ruptures are intraperitoneal and require surgical treatment[5].
With respect to urethral injuries, women are at lower risk due to the shorter length of the urethra and greater mobility because it is not attached to the pubis[22]. This meta-analysis, however, showed no differences with respect to gender when the results were compared. These injuries are believed to be the result of avulsion of the bulbomembranous urethra fixed to the urogenital diaphragm or injury by bony fragments and strongly associated with rupture of the anterior pelvic arch[10,17]. Although Lowe et al[18] observed that anterior arch fractures along with combined pubic or sacroiliac branch fractures could predict urethral injury[18], Koraitim et al[16] observed that sacroiliac fracture increased the risk of urethral injury.
Regarding the association of urinary tract injury with the type of pelvic fracture, not all available associations could be compared. Koraitim et al[16] showed that a Malgaigne pelvic fracture was associated with urethral injuries in their study due to the rupture of the posterior pelvic arch and its close relationship with the bulbomembranous urethra[16]. In this meta-analysis, pubic fractures increased the probability of urinary injury almost twofold because the bulbomembranous junction is firmly attached to the pubic arch; however, diastasis of the pubic symphysis and sacroiliac joint were indepen
Although it is logical to think that urinary injury is associated with a worse hemodynamic status, this result was not observed in this study. This is probably due to the low number of studies included. Velazquez et al[10] proposed that a SBP less than 90 mmHg is probably a direct reflection of combined urinary injury.
In relation to the mechanism of injury, it was observed that vehicle, motorcycle, and pedestrian accidents had higher probabilities of urinary injury. The findings have strong ramifications for the management of traumatic injury. Indeed, these patients with pelvic fractures due to high-risk mechanism carriers show an increased need for a high index of suspicion and pro-active assessment for urinary tract injuries; this would involve, for example, early imaging studies such as cystography or urethrography and early urology consultations. With early recognition and management of injuries, patient morbidity from long-term sequelae, such as incontinence, strictures, and sexual dysfunction, can greatly be reduced.; thus, when a patient presents with this type of mechanism of injury, medical professionals could further investigate whether the patient has a urinary tract injury. Likewise, knowing which type of fracture is most frequently associated with urinary tract injury is important so that medical professionals can pay more attention during examinations and avoid late diagnoses. In this study, the fractures most frequently associated with urinary tract injury were pubic fractures and pelvic ring disruptions.
Finally, mortality was higher in the group with associated urinary tract injuries. This finding is contrary to the hemodynamic instability outcome. This is probably due to the low number of studies included, and it could indicate that the destabilization of the patient with urinary tract injury occurs later than when the patient arrives at the emergency department, which is when the instability constants are measured in most studies by blood pressure. These results could also suggest that mortality is not related to urinary injury and is due to the association with other related injuries. However, the presence of urinary lesions may coincide with a torpid hospital evolution with increased morbidity and mortality[4,10]. It would be useful to include in future studies information on the moment of destabilization of patients with pelvic fractures.
The socioeconomic impact of these injuries is crucial to consider since such patients consume large amounts of resources due to longer hospital and ICU stays as a result of loss of mobility. In addition, the highest costs are those for rehabilitation work, mortality, and absenteeism since many of these patients are young and active[7].
This study had several limitations. For one, there is a dearth of studies focused on clinical signs that are able to detect the risk of urinary injury. Only one study analyzed this fact. Secondly, some data had to be estimated according to Cochrane criteria such as interquartile ranges or the use of percentages over the total number of patients. In addition, much information was extracted from the figures using WebPlotDigitizer. Some fractures with great clinical implications such as sacral or sacroiliac fractures could not be examined since some fractures were described in association with different fractures or not were directly evaluated by the studies. Studies that did not clearly state the type of fracture or combined fractures were eliminated from the analysis. Bladder, urethral, or whole urinary tract injuries were also analyzed together. Finally, different evaluation criteria were used for the GSC scale; in one study, fewer than eight criteria were used, and in another study, fewer than thirteen.
This meta-analysis showed that the overall incidence of urinary tract injury associated with pelvic fracture was 6.88%. It was also observed that the mechanism of injury of vehicle, motorcycle, and pedestrian accidents should suggest a greater probability of urinary injury. Similarly, pubic fractures and pelvic ring disruptions are more frequently associated with urinary tract injury. Early diagnosis is important since a higher mortality rate was observed in these patients with longer hospital stays. Recognition of these associations can help traumatologists and urologists to identify earlier subjects at risk of urethral injury. Finally, this study encourages medical professionals to be clear about the mechanism of action, to be alert to specific fractures, or to request further complementary tests to rule out early urinary tract injuries.
| 1. | Smith W, Williams A, Agudelo J, Shannon M, Morgan S, Stahel P, Moore E. Early predictors of mortality in hemodynamically unstable pelvis fractures. J Orthop Trauma. 2007;21:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 148] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 2. | Johnsen NV, Dmochowski RR, Young JB, Guillamondegui OD. Epidemiology of Blunt Lower Urinary Tract Trauma With and Without Pelvic Fracture. Urology. 2017;102:234-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Corriere JN Jr, Sandler CM. Management of the ruptured bladder: seven years of experience with 111 cases. J Trauma. 1986;26:830-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 102] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Horiguchi A. Management of male pelvic fracture urethral injuries: Review and current topics. Int J Urol. 2019;26:596-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Brandes S, Borrelli J Jr. Pelvic fracture and associated urologic injuries. World J Surg. 2001;25:1578-1587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 81] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Vaccaro JP, Brody JM. CT cystography in the evaluation of major bladder trauma. Radiographics. 2000;20:1373-1381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 92] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Aprato A, Joeris A, Tosto F, Kalampoki V, Stucchi A, Massè A. Direct and indirect costs of surgically treated pelvic fractures. Arch Orthop Trauma Surg. 2016;136:325-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Demetriades D, Karaiskakis M, Toutouzas K, Alo K, Velmahos G, Chan L. Pelvic fractures: epidemiology and predictors of associated abdominal injuries and outcomes. J Am Coll Surg. 2002;195:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 301] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 9. | Ziran BH, Chamberlin E, Shuler FD, Shah M. Delays and difficulties in the diagnosis of lower urologic injuries in the context of pelvic fractures. J Trauma. 2005;58:533-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Velazquez N, Fantus RJ, Fantus RJ, Kingsley S, Bjurlin MA. Blunt trauma pelvic fracture-associated genitourinary and concomitant lower gastrointestinal injury: incidence, morbidity, and mortality. World J Urol. 2020;38:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11206] [Cited by in RCA: 11041] [Article Influence: 690.1] [Reference Citation Analysis (0)] |
| 12. | Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3743] [Cited by in RCA: 5642] [Article Influence: 256.5] [Reference Citation Analysis (0)] |
| 13. | Allagh KP, Shamanna BR, Murthy GV, Ness AR, Doyle P, Neogi SB, Pant HB; Wellcome Trust- PHFI Folic Acid project team. Birth prevalence of neural tube defects and orofacial clefts in India: a systematic review and meta-analysis. PLoS One. 2015;10:e0118961. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 14. | Lorente A, Mariscal G, Lorente R. Incidence and risk factors for complex regional pain syndrome in radius fractures: meta-analysis. Arch Orthop Trauma Surg. 2023;143:5687-5699. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Hochberg E, Stone NN. Bladder rupture associated with pelvic fracture due to blunt trauma. Urology. 1993;41:531-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Koraitim MM, Marzouk ME, Atta MA, Orabi SS. Risk factors and mechanism of urethral injury in pelvic fractures. Br J Urol. 1996;77:876-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 115] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Avey G, Blackmore CC, Wessells H, Wright JL, Talner LB. Radiographic and clinical predictors of bladder rupture in blunt trauma patients with pelvic fracture. Acad Radiol. 2006;13:573-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Lowe MA, Mason JT, Luna GK, Maier RV, Copass MK, Berger RE. Risk factors for urethral injuries in men with traumatic pelvic fractures. J Urol. 1988;140:506-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 44] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Delaney KM, Reddy SH, Dayama A, Stone ME Jr, Meltzer JA. Risk factors associated with bladder and urethral injuries in female children with pelvic fractures: An analysis of the National Trauma Data Bank. J Trauma Acute Care Surg. 2016;80:472-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Bjurlin MA, Fantus RJ, Mellett MM, Goble SM. Genitourinary injuries in pelvic fracture morbidity and mortality using the National Trauma Data Bank. J Trauma. 2009;67:1033-1039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 115] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 21. | Bott A, Nicol G, Odutola A, Halliday R, Acharya MR, Ward A, Chesser TJS. Long-term patient reported sexual and urological dysfunction in males after operatively treated pelvic ring injuries Do generic outcome measures identify genitourinary health problems? Injury. 2022;53:2139-2144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Basta AM, Blackmore CC, Wessells H. Predicting urethral injury from pelvic fracture patterns in male patients with blunt trauma. J Urol. 2007;177:571-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 23. | Aihara R, Blansfield JS, Millham FH, LaMorte WW, Hirsch EF. Fracture locations influence the likelihood of rectal and lower urinary tract injuries in patients sustaining pelvic fractures. J Trauma. 2002;52:205-208; discussion 208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Wright JL, Nathens AB, Rivara FP, MacKenzie EJ, Wessells H. Specific fracture configurations predict sexual and excretory dysfunction in men and women 1 year after pelvic fracture. J Urol. 2006;176:1540-1545; discussion 1545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |