Published online Feb 18, 2025. doi: 10.5312/wjo.v16.i2.101197
Revised: January 2, 2025
Accepted: January 17, 2025
Published online: February 18, 2025
Processing time: 153 Days and 5 Hours
Intra-articular hip injections (IAHIs) are commonly used for diagnostic and thera
To investigate the difference between anticipated and experienced pain during IAHIs and the impact of pre-injection local anesthesia.
This prospective study enrolled 60 patients undergoing IAHI, 30 receiving pre-injection superficial local anesthesia and 30 serving as a control group without pre-injection local anesthesia. Pain levels were assessed using numeric rating scales.
Patients significantly overestimated anticipated pain compared to experienced pain (6.43 ± 2.48 vs 3.68 ± 2.37, P < 0.001). Pre-injection local anesthesia did not significantly reduce experienced pain (3.19 ± 2.38 vs 4.20 ± 2.29, P = 0.130).
Patients overestimate anticipated pain during IAHIs. Pre-injection local anesthesia does not reduce experienced pain.
Core Tip: This study evaluated anticipated vs experienced pain during intra-articular hip injections (IAHIs) in 60 prospectively recruited patients, with or without pre-injection local anesthesia. Anticipated pain was significantly overestimated compared to experienced pain, and pre-injection local anesthesia did not affect the experienced pain. These results suggest that the hip joint capsule may significantly contribute to nociception during IAHI, more so than the superficial soft tissues along the needle trajectory. Ultimately, these findings provide valuable insight into the pain experienced during IAHI and may help improve patient experiences.
- Citation: Albagli A, Rath E, Druckmann I, Efrima B, Kazum E, Parnes N, Sandler AB, Tyler J, Amar E. Pre-injection local anesthesia does not affect experienced pain in intra-articular hip injections. World J Orthop 2025; 16(2): 101197
- URL: https://www.wjgnet.com/2218-5836/full/v16/i2/101197.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i2.101197
Intra-articular hip injections (IAHIs) are routinely performed for diagnostic and therapeutic purposes. While IAHI-specific injection-related pain is poorly characterized in existing literature, the deep nature of the hip joint and need for longer needles can cause substantial concerns regarding IAHI-related pain, apprehension, and anxiety among patients. While injection-related pain is largely recognized, the disparity between the expected and experienced pain during injection procedures is a known and well-studied phenomenon in many medical fields including dentistry[1], obstetrics[2], and urology[3], yet it remains poorly elucidated in the orthopedic practice of IAHI injections. Unlike other medical injections, IAHIs involve the navigation of deep extraarticular anatomy to reach the hip joint and needle penetration of the hip capsule, which is densely innervated with nociceptive fibers[4]. Additionally, the implications of hip injections for a chronic painful joint associated with conditions such as osteoarthritis may further influence procedural pain perception and warrant an investigation of procedural pain specific to IAHI[5].
A meta-analysis conducted by McLenon and Rogers[6] demonstrates treatment avoidance due to patients’ fear of needles, and factors such as needle size, injection speed, and patient anxiety have been shown to contribute to injection-related pain perception[7,8]. Therefore, there is value in understanding how to minimize injection-related pain and how to optimize pain management strategies and reduce experienced pain and anxiety associated with IAHI. Multiple tech
A total of 60 patients were prospectively enrolled into one of two injection groups: Group A, which received superficial local anesthesia administered prior to intra-articular injection (study group), and group B, which underwent IAHI without local pre-injection anesthesia (control group).
Institutional Review Board approval was granted before study enrollment. Data were prospectively collected from patients undergoing IAHI between January 2021 to January 2022. Inclusion criteria selected for patients undergoing first-time IAHI as indicated by an orthopedic surgeon either for diagnostic (e.g. lidocaine test, arthrography) and/or therapeutic (steroid injection for osteoarthritis) purposes. Participants were 18 years of age or older, had no previous hip joint injections, and could fill in the survey questionnaire. Exclusion criteria excluded patients under 18 years of age, patients with a known history of hypersensitivity or allergy to the injectant material (e.g. local anesthetics, steroids), and patients lacking the ability to sign informed consent or to complete a survey questionnaire. Patients with previous hip joint injections were also excluded, due to the possibility that these patients could recall the prior pain experienced.
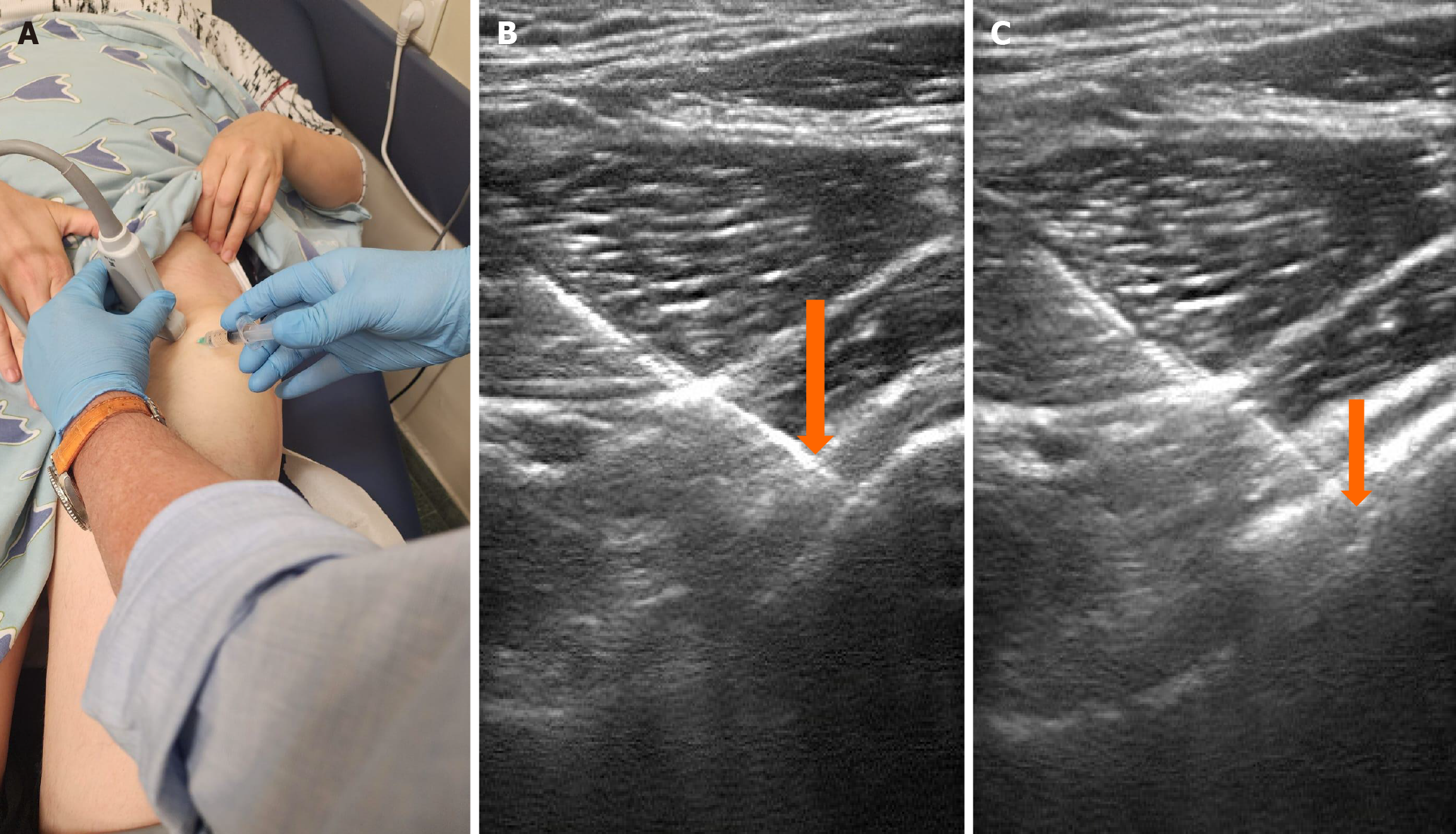
With the patient positioned supine, antiseptic solution was administered in a circular manner over the hip. A linear 13-6 MHz transducer (SonoSite™ M turbo; SonoSite Inc., Bothell, WA 98021, United States) was placed in an oblique longitudinal plane over the femoral neck (Figure 1A). Once the anatomic landmarks were identified, patients in group A underwent local anesthesia infiltration with 5 mL 1% lidocaine injected along the planned trajectory of the intra-articular injection using a 38 mm 21-gauge needle. The 38 mm 21-gauge needle was then replaced with a 90 mm 21-gauge spinal needle, maintaining the needle in an in-plane manner to ensure constant needle visualization. The needle was then advanced under direct visualization through the joint capsule (Figure 1B) at the anterior joint recess at the femoral head and neck junction (Figure 1C). Subsequently, 1 mL of 1% lidocaine was injected to confirm intra-articular position under sonographic visualization and unresisted flow of the local anesthesia prior to the administration of the diagnostic or therapeutic injection. The same technique was used for injection among patients in group B without the pre-injection infiltration of local anesthesia in the needle trajectory.
Prior to IAHI, a questionnaire about pain and anxiety related to the procedure was administered. The questionnaire was comprised of three sections, including: (1) Two numeric rating scales (NRS) scores scaled from numbers 0 to 10, where 0 represented no pain and 10 represented the worst pain imaginable[12], with the first score measuring anticipated pain before the injection and the second score measuring experienced pain during the procedure; (2) The Beck Anxiety Inventory (BAI) scale, which is used to assess anxiety level[13], consists of 21 items, each scored from 0-3 points totaling 0-63 cumulatively. Final scores ranging from 0-7 reflect a minimal level of anxiety, while scores 8-15 reflect mild anxiety, 16-25 moderate anxiety, and 26-63 severe anxiety. After answering the BAI scale, a history of any anxiety disorders was documented, as well as any consumption of prescribed anxiety medications; and (3) A numeric evaluation of five factors that may influence the patient’s fear of injections as suggested by Nir et al[14], including pain, appearance of the needle and syringe, needle size, seeing others receiving the injection, and negative previous injection experiences outside of IAHI, with each factor graded between 0 (no influence) and 5 (maximal influence). The data from the aforementioned questionnaires were collected and pooled for analysis.
As projected from existing research, a sample size of 25 subjects per treatment group was estimated to provide a statistical power of 80%[15]. Hypothesis testing was conducted using both parametric and non-parametric methods, depending on the distribution of the data. For continuous outcomes, analyses of variance were used to evaluate between-group differences with treatment group established as a fixed effect. Paired t-tests were used for within-group compari
Sixty patients were ultimately deemed eligible for inclusion. The mean age was 38.4 (SD = 14.09, range: 18-75) years. Ultimately, 29 of the patients were male with a mean age of 34.9 (SD = 10.98, range: 18-61) years while 31 were female with a mean age of 41.9 (SD = 16.19 range: 18-75) years. The mean age was not significantly different between male and female patients (P = 0.08). There was also no significant difference in age between the local anesthesia and control groups (P = 0.161).
There was no significant difference between local anesthesia and control groups regarding the patient-estimated NRS score (local anesthesia: 6.19 vs control: 6.68, P = 0.489) and experienced NRS score (local anesthesia: 3.19 vs control: 4.20, P = 0.130). However, there was a significant difference among the entire cohort regarding anticipated vs experienced pain, with anticipated pain estimated at an NRS score of 6.43 (SD = 2.48) vs experienced pain reported at 3.68 (SD = 2.37) (P < 0.001).
When stratified by study group, significant differences were similarly observed among anticipated and experienced pain, with participants receiving local anesthetic reporting anticipated and experienced pain scores of 6.19 (SD = 2.48) and 3.19 (SD = 2.38), respectively (P < 0.001) and participants in the control group reporting scores of 6.68 (SD = 2.51) and 4.2 (SD = 2.29), respectively (P < 0.001) (Table 1). The net difference in anticipated and experienced pain did not differ between injection methods (local anesthesia: Δ = 3.0 vs control: Δ = 2.48; P = 0.498).
Discrepancies among anticipated and experienced pain remained statistically significant when participants were stra
| Parameter | n | Factors influencing anxiety | |||||
| Fear of pain | Appearance of the needle and syringe | Needle size | Seeing others receiving injection | Negative previous experience | BAI | ||
| Study population | 60 | 2.84 | 2.54 | 2.51 | 1.23 | 1.23 | 4.26 |
| Use of local anesthesia | |||||||
| Study (local anesthesia) | 30 | 2.68 | 2.2 | 2.23 | 1.25 | 1.06 | 4.33 |
| Control (no local anesthesia) | 30 | 3 | 2.88 | 2.77 | 1.23 | 1.42 | 4.15 |
The results of the BAI questionnaire are presented in Table 3. Stratifying both study groups by the local anesthetic and control populations as well as by sex (Table 2) did not yield significant differences in BAI measures or associated anxiety-inducing factors. However, a low to moderate correlation was found between anticipated mean NRS score and BAI, fear of pain, needle visualization, needle size, seeing others receiving an injection, and previous injection experience (0.288, 0.587, 0.511, 0.394, 0.202, and 0.420, respectively).
| Anticipated pain vs experienced pain | Factors influencing anxiety | |||||||||
| Sex | n | Anticipated pain, mean ± SD | Experienced pain, mean ± SD | Net difference (Δ) | Fear of pain | Appearance of the needle and syringe | Needle size | Seeing others receiving injection | Negative previous experience | BAI |
| Males | 29 | 6.0 ± 2.87a | 3.26 ± 2.09 | 2.74 | 2.78 | 2.54 | 2.4 | 0.92 | 1.36 | 3.44 |
| Females | 31 | 6.88 ± 1.96a | 4.12 ± 2.60 | 2.76 | 2.9 | 2.58 | 2.59 | 1.5 | 1.05 | 5.15 |
The findings of this study offer several key insights into IAHI-related pain. Firstly, there are significant differences between anticipated and experienced pain in IAHI, with patients overestimating anticipated procedural pain. Secondly, the administration of pre-injection local anesthesia did not significantly affect the ultimate experienced pain of IAHI. Finally, anticipated pain only weakly correlates with BAI scores and other injection-related factors including fear of pain, needle visualization, needle size, and prior injection experiences. There were no significant differences among anticipated and experienced pain when stratified by patient sex. These findings confirmed our hypothesis and demonstrated a high overestimation of anticipated pain, which may have important implications for patient education and managing expectations.
The hip joint capsule is considered an important trigger of nociception that may modulate experienced pain during IAHI. Saxler et al[17] showed a significantly higher density of afferent nerve fibers in the hip capsules of patients with painful osteoarthritis than those without antecedent hip pain. The abundant distribution of nociceptors in the painful hip capsule may explain how both patients in both study groups, one with pre-injection local anesthesia and one control, experienced similar levels of pain. The results of the present study and lack of significant pain modulation with pre-injection local anesthesia may support a substantial capsular contribution to experienced pain in IAHI.
Additionally, anticipated IAHI pain was consistently and significantly higher than experienced pain. This finding reinforces existing research demonstrating a significant discrepancy between anticipated and experienced pain during injection procedures in a variety of medical specialties[1-3]. These results further validate the phenomenon of overestimating pain perception prior to medical interventions and subsequently emphasize the importance of realistically managing patient expectations regarding procedural pain in IAHI. Educating patients regarding the tendency to overestimate anticipated pain in IAHI may offer value in managing procedure-related anxiety and closing the gap in anticipated and experienced pain. Psychological interventions, such as cognitive-behavioral therapy (CBT), offer a promising approach to managing injection-related anxiety and enhancing patient experiences. Previous studies have shown that even a single session of CBT can be both effective and practical in significantly reducing symptoms of needle phobia[18,19]. Given the high propensity for study participants to overestimate anticipated pain, applying psychological principles targeted towards fear reduction pre-IAHI may prove beneficial in improving patient experiences.
Understanding the factors that contribute to injection-related anxiety may increase our understanding of anticipated IAHI pain. Patients with a fear of needles report avoidance of medical care involving needles[20]. For example, vaccine-related pain contributes to vaccine non-adherence[21], dental injections contribute to dental anxiety and avoidance of dental care[22], and injection anxiety and needle phobia contribute to avoidance of recommended treatments among patients with insulin-dependent diabetes[23]. Along these lines, Nir et al[14] described how factors such as fear of pain, needle size, a history of fainting, and the act of watching others undergo injections are highly and independently associated with a fear of injections. In the present study, however, the correlation between anticipated pain and BAI, fear of pain, needle visualization, needle size, and previous injection experiences only reached low to moderate significance. This discrepancy may be explained by the differences in outcome measures, as Nir et al[14] defined fear of injections according to subjectively recorded perceptions of fear rather than pain scores, like in the present study. Regardless, extrapolating the specific sources of injection-related fear may offer value in understanding anticipated pain.
In the present study, there were no appreciable differences between male and female participants in either anticipated or experienced pain, with only slight variations in mean anticipated and experienced pain scores observed (6.88 vs 6.00, 4.12 vs 3.26, respectively). In general, women may have higher levels of anticipated and experienced pain in healthcare settings than men[24]. Additionally, prior research suggests that biological factors such as hormonal modulation, nociceptive fiber density, and pain receptor distribution may contribute to variability between these demographics[25,26]. Furthermore, cultural differences and gender norms or expectations may affect willingness to disclose pain[27]. Regardless, both male and female participants in the present study experienced similar levels of anticipated and expe
This study has limitations. Firstly, the use of self-reported pain scores introduces subjectivity, as individual pain per
The findings of the present study demonstrate significantly overestimated anticipated vs experienced pain during IAHI. Additionally, pre-injection local anesthesia does not offer benefits in decreasing IAHI-related pain, suggesting that the hip joint capsule may significantly contribute to nociception during IAHI more than superficial soft tissues in the needle trajectory. Ultimately, these findings offer value in understanding experienced pain during IAHI and can be applied to improve patient experiences with IAHI.
| 1. | Watkins CA, Logan HL, Kirchner HL. Anticipated and experienced pain associated with endodontic therapy. J Am Dent Assoc. 2002;133:45-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Karasahin E, Gungor S, Goktolga U, Keskin U, Gezginc K, Baser I. Anticipated and perceived pain from midtrimester amniocentesis. Int J Gynaecol Obstet. 2008;101:290-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Baird B, Wajswol E, Ericson C, Anderson A, Broderick G. Pre- and Post-Injection Needle Pain in Patients Undergoing First Intracavernosal Injection. J Sex Med. 2022;19:590-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 4. | Laumonerie P, Dalmas Y, Tibbo ME, Robert S, Durant T, Caste T, Vialla T, Tiercelin J, Gracia G, Chaynes P. Sensory Innervation of the Hip Joint and Referred Pain: A Systematic Review of the Literature. Pain Med. 2021;22:1149-1157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 5. | Pereira TV, Saadat P, Bobos P, Iskander SM, Bodmer NS, Rudnicki M, Dan Kiyomoto H, Montezuma T, Almeida MO, Bansal R, Cheng PS, Busse JW, Sutton AJ, Tugwell P, Hawker GA, Jüni P, da Costa BR. Effectiveness and safety of intra-articular interventions for knee and hip osteoarthritis based on large randomized trials: A systematic review and network meta-analysis. Osteoarthritis Cartilage. 2024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 6. | McLenon J, Rogers MAM. The fear of needles: A systematic review and meta-analysis. J Adv Nurs. 2019;75:30-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 333] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 7. | Perrot S, Laroche F, Poncet C, Marie P, Payen-Champenois C. Are joint and soft tissue injections painful? Results of a national French cross-sectional study of procedural pain in rheumatological practice. BMC Musculoskelet Disord. 2010;11:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Tafti D, Schultz D. Hip Joint Injection. 2023 Jul 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. [PubMed] |
| 9. | Wagner RD, Kilmartin C, Behar BJ, Chhabra AB, Freilich AM, DeGeorge BR Jr. Is This Going to Hurt, Doc? Predicting Pain with Corticosteroid Injections for Upper Extremity Conditions. Plast Reconstr Surg Glob Open. 2023;11:e5017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Hamilton JG. Needle phobia: a neglected diagnosis. J Fam Pract. 1995;41:169-175. [PubMed] |
| 11. | Masoud MA, Said HG. Intra-articular hip injection using anatomic surface landmarks. Arthrosc Tech. 2013;2:e147-e149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Heller GZ, Manuguerra M, Chow R. How to analyze the Visual Analogue Scale: Myths, truths and clinical relevance. Scand J Pain. 2016;13:67-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 355] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 13. | Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S467-S472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 846] [Cited by in RCA: 1093] [Article Influence: 84.1] [Reference Citation Analysis (0)] |
| 14. | Nir Y, Paz A, Sabo E, Potasman I. Fear of injections in young adults: prevalence and associations. Am J Trop Med Hyg. 2003;68:341-344. [PubMed] |
| 15. | Giordano BD. Comparison of Two Injection Techniques for Intra-articular Hip Injections. J Ultrasound Med. 2016;35:1259-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 16. | Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:69-71. [PubMed] |
| 17. | Saxler G, Löer F, Skumavc M, Pförtner J, Hanesch U. Localization of SP- and CGRP-immunopositive nerve fibers in the hip joint of patients with painful osteoarthritis and of patients with painless failed total hip arthroplasties. Eur J Pain. 2007;11:67-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 87] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 18. | Hiermeier UM, Mofrad L. Feasibility of one-session treatment for specific needle phobia in an adult IAPT service – a case series. Cogn Beh Ther. 2020;13:e51. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Love AS, Love RJ. Considering Needle Phobia among Adult Patients During Mass COVID-19 Vaccinations. J Prim Care Community Health. 2021;12:21501327211007393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 20. | Wright S, Yelland M, Heathcote K, Ng SK, Wright G. Fear of needles--nature and prevalence in general practice. Aust Fam Physician. 2009;38:172-176. [PubMed] |
| 21. | Taddio A, Chambers CT, Halperin SA, Ipp M, Lockett D, Rieder MJ, Shah V. Inadequate pain management during routine childhood immunizations: the nerve of it. Clin Ther. 2009;31 Suppl 2:S152-S167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 175] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 22. | Vika M, Skaret E, Raadal M, Ost LG, Kvale G. Fear of blood, injury, and injections, and its relationship to dental anxiety and probability of avoiding dental treatment among 18-year-olds in Norway. Int J Paediatr Dent. 2008;18:163-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Zambanini A, Newson RB, Maisey M, Feher MD. Injection related anxiety in insulin-treated diabetes. Diabetes Res Clin Pract. 1999;46:239-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 199] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 24. | Paller CJ, Campbell CM, Edwards RR, Dobs AS. Sex-based differences in pain perception and treatment. Pain Med. 2009;10:289-299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 279] [Cited by in RCA: 282] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 25. | Chen Q, Zhang W, Sadana N, Chen X. Estrogen receptors in pain modulation: cellular signaling. Biol Sex Differ. 2021;12:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 64] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 26. | Zubieta JK, Smith YR, Bueller JA, Xu Y, Kilbourn MR, Jewett DM, Meyer CR, Koeppe RA, Stohler CS. mu-opioid receptor-mediated antinociceptive responses differ in men and women. J Neurosci. 2002;22:5100-5107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 235] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 27. | Miller ET, Abu-Alhaija DM. Cultural Influences on Pain Perception and Management. Pain Manag Nurs. 2019;20:183-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |