INTRODUCTION
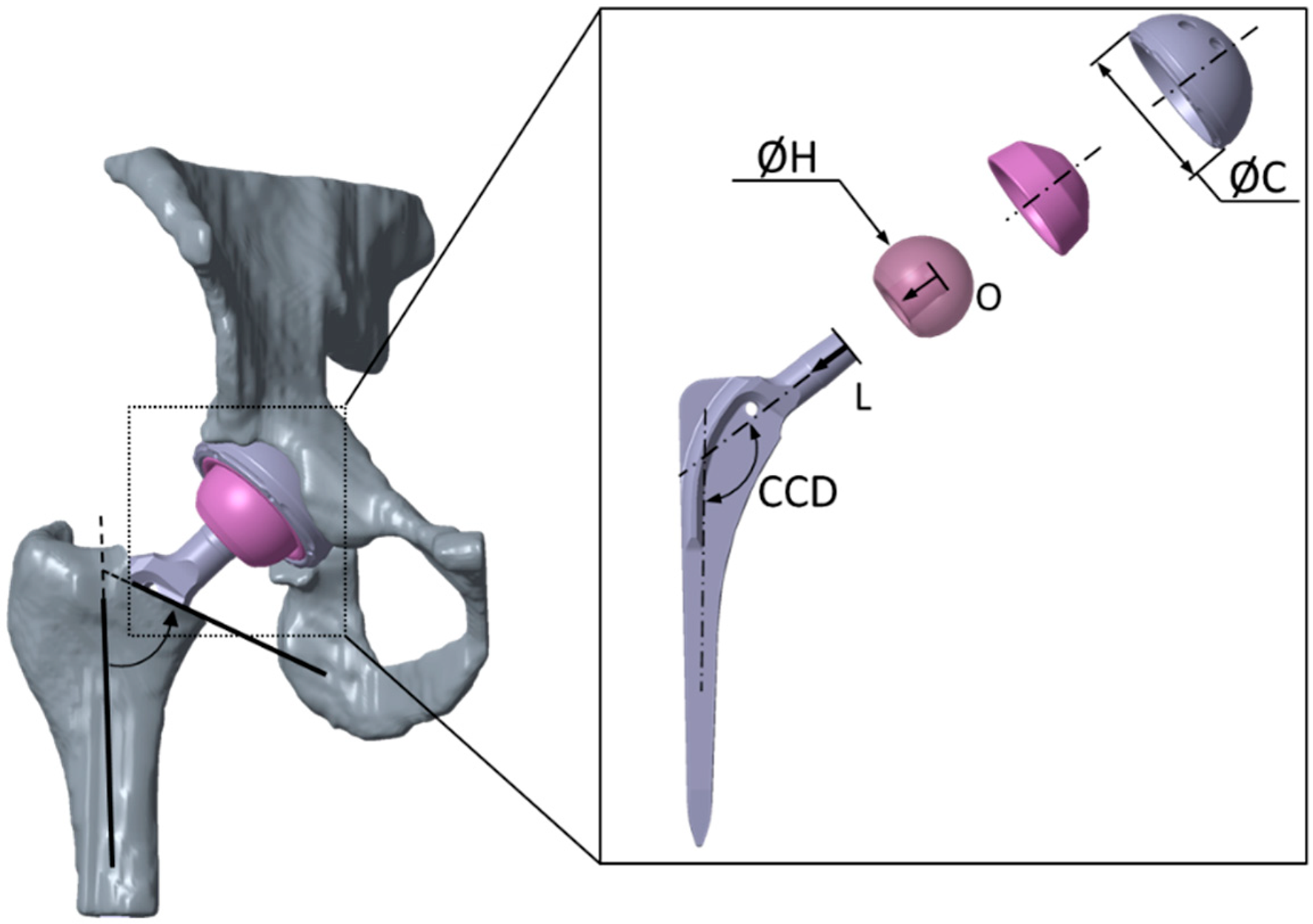
Total hip arthroplasty as presented in Figure 1 is a medical procedure that have been successfully performed worldwide. The procedure in adults with sequelae from childhood hip disorders presents unique challenges due to significant anatomical variations and complexities. These patients often suffer from limb shortening[1], limping[2], pain[3], and altered gait[4], making total hip arthroplasty particularly demanding. The paper published by Oommen et al[5] provides a detailed review of the essential considerations and strategies for managing these complex cases. This article aims to expand on these insights by exploring the integration of computational simulation, specifically finite element analysis (FEA), to enhance surgical precision and outcomes.
Figure 1 Total hip arthroplasty[6].
Citation: Kebbach M, Schulze C, Meyenburg C, Kluess D, Sungu M, Hartmann A, Günther K, Bader R. An MRI-Based Patient-Specific Computational Framework for the Calculation of Range of Motion of Total Hip Replacements. Appl Sci 2021; 11: 2852. Copyright ©The Author(s) 2021. Published by MDPI. CCD: Centrum-collum-diaphyseal.
THE ROLE OF FEA IN TOTAL HIP ARTHROPLASTY
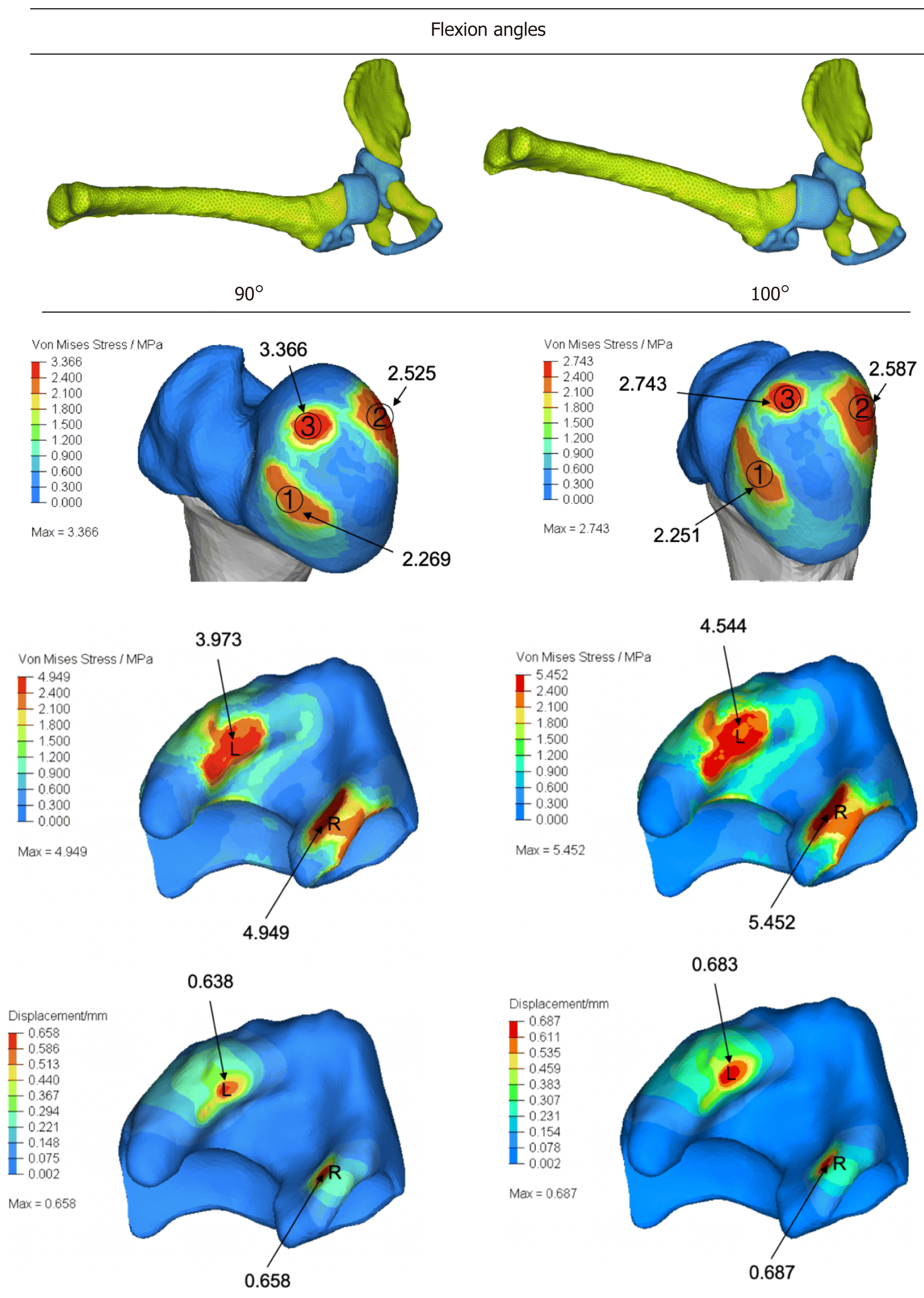
FEA is a sophisticated computational tool that models the mechanical behavior of structures[6] under various conditions, including stress[7], strain[8], and deformation[9]. This approach offers several advantages for studying total hip arthroplasty, including lower costs and faster results, when compared to clinical studies, experimental testing, and mathematical modelling[10]. In the context of orthopedic surgery, FEA provides a powerful means to gain detailed insights into the biomechanical performance of both implants and bone structures, which is crucial for enhancing surgical outcomes. In preoperative planning[11], FEA allows for the simulation of different surgical scenarios, enabling surgeons to visualize and predict the mechanical interactions between implants[12] and the patient’s unique anatomy[13]. This process helps in determining the optimal size[14], shape[15], material[16], design[17], and placement of implants[18], thereby reducing the risk of complications such as implant loosening[19] or failure[20]. Using FEA, surgeons can assess the load distribution across the hip joint[21] and ensure that the implant can withstand the physiological forces it will encounter during daily activities[22], such as studied by Zhang et al[23] that performs computational study via FEA for investigate stress distribution at human hip joint as shown in Figure 2.
Figure 2 Von Mises stress and displacement at hip joint[23].
Citation: Zhang Z, Sui D, Qin H, Li H, Zhang Z. Contact pressure distribution of the hip joint during closed reduction of developmental dysplasia of the hip: A patient-specific finite element analysis. BMC Musculoskelet Disord 2020; 21: 600. Copyright ©The Author(s) 2020. Published by BioMed Central.
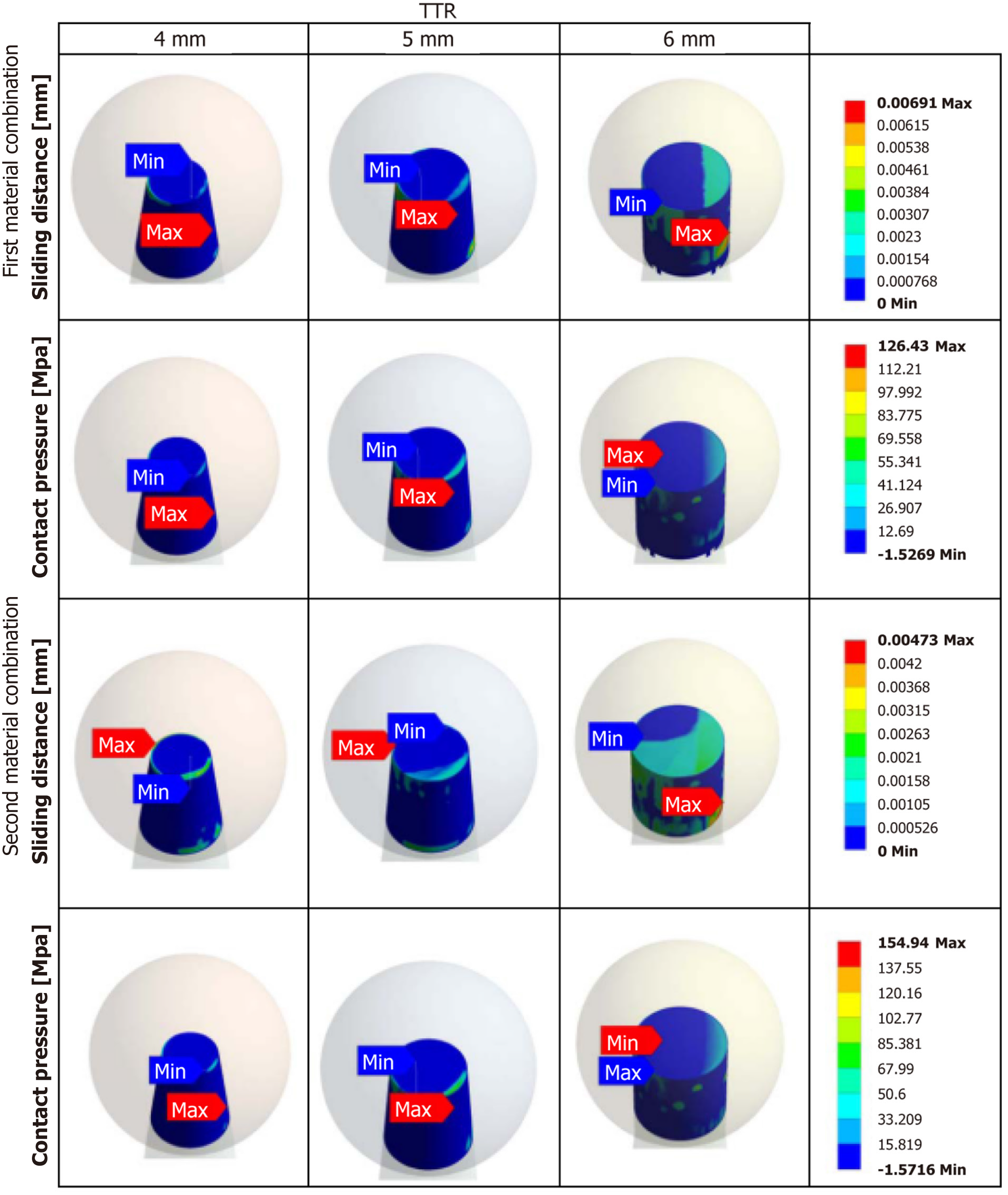
Moreover, FEA contributes significantly to implant design. For example, study by Gutmann et al[24] (Figure 3) explore wear performance of various design on total hip arthroplasty with varying chamfer geometry at the trunnion junction. Manufacturers can use FEA to test new implant materials[25] and geometries[26] under simulated conditions before clinical application. This virtual testing phase helps in identifying potential issues and refining the design to enhance durability and compatibility with the human body. For example, different alloy compositions[27] or coating materials[28] can be evaluated for their biomechanical properties, ensuring that the final product provides optimal support and longevity.
Figure 3 Contact pressure and sliding distance distribution on modified trunnion geometry of total hip arthroplasty[24].
Citation: Gutmann C, Shaikh N, Shenoy BS, Shaymasunder Bhat N, Keni LG, K N C. Wear estimation of hip implants with varying chamfer geometry at the trunnion junction: a finite element analysis. Biomed Phys Eng Express 2023; 9. Copyright ©Institute of Physics (the “Institute”) and IOP Publishing Limited. Published by IOP Publishing Limited. Max: Maximum; Min: Minimum; TTR: Taper trunnion radius.
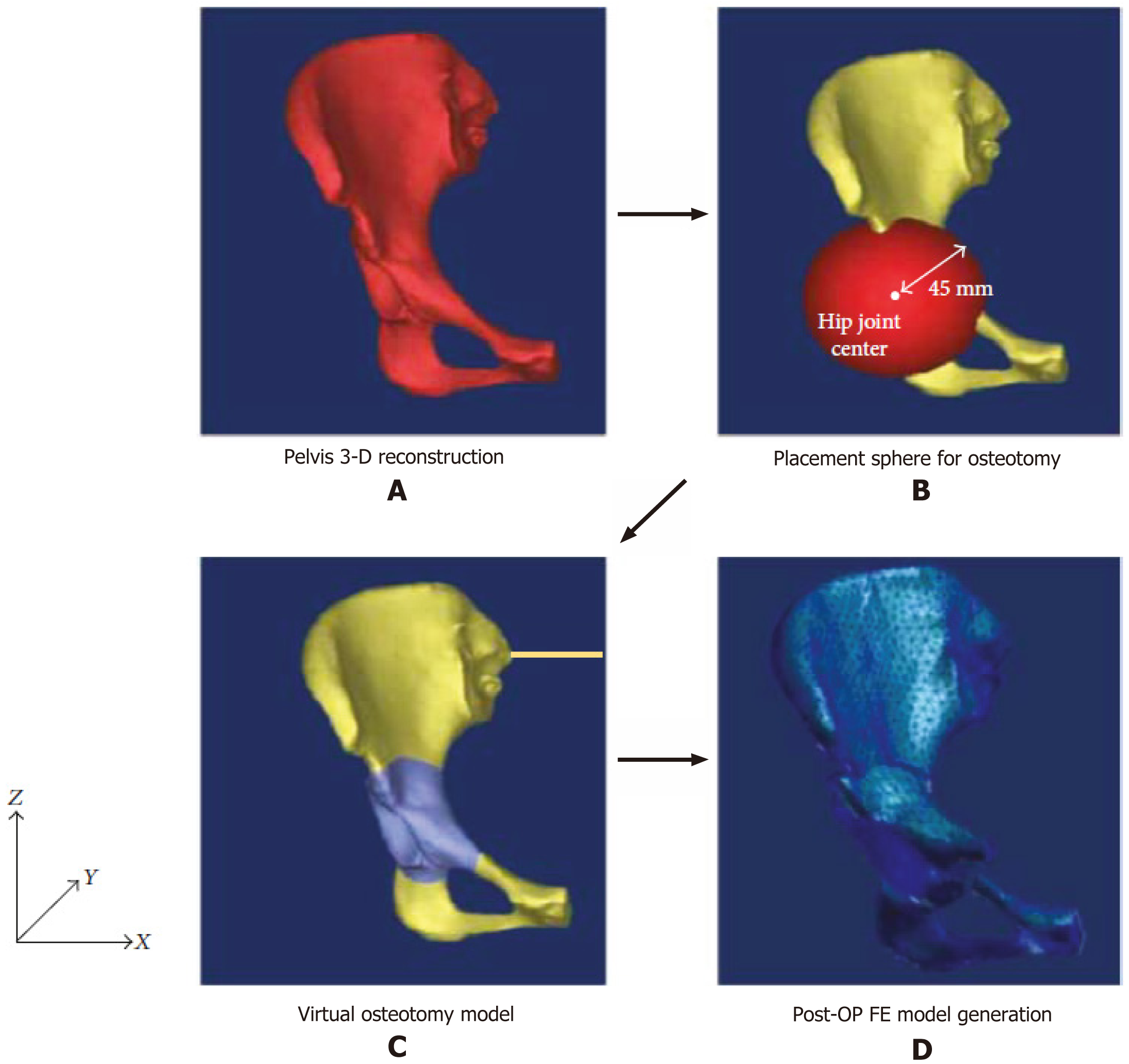
Additionally, FEA enables the customization of implants to match the specific anatomical features of each patient. For example, Park et al[29] conduct computational simulation to evaluate the optimal direction and amount of acetabular rotation in three anatomical planes (sagittal, coronal, and transverse) during periacetabular osteotomy for a patient with hip dysplasia that would contribute to implant design of patient’s anatomy-specific. This personalized approach minimizes the risk of complications and improves overall surgical outcomes. Furthermore, FEA aids in understanding the long-term behavior of implants and bone structures[30]. By simulating repetitive loading conditions over extended periods, FEA can predict how implants will perform under chronic stress[31]. This predictive capability is invaluable for assessing the long-term success of surgical interventions and making informed decisions about implant selection and surgical techniques[32]. By modeling the mechanical environment of the hip joint[33], FEA helps surgeons anticipate challenges that might arise during surgery. This includes understanding how different surgical approaches[34] or osteotomies[35] might affect the stability and alignment of the hip joint. This allows surgeons to plan precise cuts and adjustments that will restore the hip to its optimal functional position (Figure 4).
Figure 4 Finite element model using patient’s anatomy-specific[29].
Citation: Park SJ, Lee SJ, Chen WM, Park JH, Cho YS, Shin T, Kwon SY. Computer-Assisted Optimization of the Acetabular Rotation in Periacetabular Osteotomy Using Patient’s Anatomy-Specific Finite Element Analysis. Appl Bionics Biomech 2018; 2018: 9730525. Copyright ©The Author(s) 2018. Published by Hindawi Publishing Corporation. A: Pelvis 3-D reconstruction; B: Placement sphere for osteotomy; C: Virtual osteotomy model; D: Postoperative finite element model generation. Post-OP FE: Postoperative finite element.
ENHANCING PREOPERATIVE PLANNING
Preoperative planning is critical for successful total hip arthroplasty, particularly in patients with altered hip anatomy. Comprehensive assessments, such as templating and computed tomography evaluations, are essential to ensure optimal outcomes. FEA significantly enhances this process by providing detailed biomechanical insights, enabling surgeons to make informed decisions about implant selection and surgical strategies.
One key application of FEA in preoperative planning is simulating different implant configurations. FEA can model various implant sizes[36], positions[37], and orientations[38], predicting their biomechanical performance and helping surgeons choose the most suitable options. By running simulations on different configurations, surgeons can visualize how each implant interacts with the patient’s unique anatomy. This step is crucial for identifying potential issues before surgery, such as improper fit or alignment, which could lead to complications like implant loosening or instability postoperatively.
FEA also plays a vital role in predicting load distribution. By analyzing stress and strain patterns, FEA helps ensure that implants distribute loads optimally[39], thereby reducing the risk of complications such as implant loosening[40] or bone fracture[41]. Understanding how forces will be distributed across the implant and the surrounding bone allows surgeons to select and position implants that minimize stress concentrations. This enhances the longevity and stability of the prosthesis, ultimately improving patient outcomes.
Additionally, FEA assists in assessing bone quality, which is particularly important for patients with childhood hip disorder sequelae, where bone quality may be compromised. FEA can evaluate bone density and quality, aiding in planning fixation strategies and selecting appropriate implant materials[42]. This assessment ensures that the bone can adequately support the implant and identifies necessary modifications to achieve a successful surgical outcome.
OPTIMIZING IMPLANT DESIGN AND PLACEMENT
Patients with childhood hip disorder sequelae often present with significant anatomical variations, including altered acetabular and femoral structures. These deviations from typical anatomy pose challenges in restoring the anatomical hip center and achieving stable fixation. Addressing these complexities requires advanced tools and techniques, and FEA has emerged as a valuable resource in optimizing surgical strategies for such cases. One important application of FEA is modeling anatomical variations. FEA can generate detailed models of the altered acetabular floor and proximal femur, allowing surgeons to understand the unique anatomical features they will encounter[43]. These models enable a tailored surgical approach, ensuring that implants fit well within the modified anatomy and function effectively post-surgery. By providing a comprehensive understanding of the patient’s anatomy, FEA helps surgeons anticipate and address potential complications, leading to better surgical outcomes.
FEA also facilitates the customization of implants to match the patient’s specific anatomical needs. By simulating various implant designs, FEA aids in the development of customized implants that precisely fit the patient’s unique anatomy[44]. Custom implants can address specific anomalies, such as irregular bone shapes or sizes, enhancing stability and functionality. This individualized approach ensures that patients receive implants designed for their specific conditions, improving the overall effectiveness of the surgical intervention. In addition, FEA is instrumental in evaluating surgical techniques. For instance, it can simulate various approaches, such as subtrochanteric shortening osteotomy, and predict their biomechanical outcomes. By providing insights into how different techniques influence joint stability and load distribution, FEA guides surgeons in optimizing their surgical plans[45]. This level of precision minimizes risks, improves the chances of restoring normal hip function, and enhances the overall success of the procedure.
SIMULATING SUBTROCHANTERIC SHORTENING OSTEOTOMY
The paper published by Oommen et al[5] emphasizes the importance of subtrochanteric shortening osteotomy in addressing high-riding hips and significant limb shortening. This procedure is particularly complex, requiring meticulous planning and precise execution to achieve optimal outcomes. FEA offers valuable support in optimizing this surgical technique, aiding surgeons in planning and implementation. One key application of FEA in subtrochanteric shortening osteotomy is simulating the osteotomy and subsequent implant placement. By creating detailed models of the procedure, FEA can predict the mechanical outcomes of different surgical scenarios[46]. This allows surgeons to identify the optimal location and angle for the osteotomy and determine the best positioning of the implant to restore proper limb length and alignment. Such simulations help surgeons refine their surgical approach, reducing the likelihood of errors and improving the accuracy of the procedure.
FEA also plays a critical role in optimizing the alignment and stability of the femoral component after osteotomy. By analyzing the mechanical interactions between the implant and the surrounding bone, FEA ensures that the hip center is restored accurately and that the implant is securely fixed[47]. This step is essential for achieving a balanced and stable hip joint, which supports normal gait and overall function. Through these capabilities, FEA helps surgeons enhance the effectiveness of subtrochanteric shortening osteotomy, leading to improved patient outcomes and a higher quality of life.
IMPROVING POSTOPERATIVE OUTCOMES
The primary objective of integrating FEA into total hip arthroplasty planning is to improve postoperative outcomes by adjusting implants and surgical techniques to the specific needs of each patient. FEA provides detailed biomechanical insights that allow for more precise planning and execution, ultimately enhancing the overall effectiveness and safety of the procedure.
One significant benefit of using FEA in total hip arthroplasty is the enhancement of hip function. By ensuring accurate restoration of the hip center and secure fixation of the implant, FEA contributes to improved joint mechanics and reduced pain. Properly positioned and stabilized implants enable patients to regain normal mobility and experience greater comfort, leading to a more successful recovery[48]. Additionally, FEA plays a crucial role in reducing complication rates. By optimizing implant design and placement, FEA minimizes risks associated with dislocation[49], loosening[50], and wear[51]. This proactive approach reduces the likelihood of revision surgeries and increases the overall success rate of the total hip arthroplasty procedure, ensuring better outcomes for patients. Furthermore, total hip arthroplasty helps achieve better long-term outcomes by tailoring the surgical approach to the unique anatomical features of each patient. Personalized planning enhances the longevity of the implant, providing patients with a durable solution that meets their functional and anatomical needs. This individualized approach leads to higher patient satisfaction and a significantly improved quality of life.
ADDRESSING ACETABULAR AND FEMORAL CHALLENGES
The paper published by Oommen et al[5] highlighted the unique challenges associated with the acetabulum and femur in patients with childhood hip disorder sequelae, emphasizing the need for careful planning and precise surgical execution. These anatomical variations often complicate total hip arthroplasty and require advanced tools, such as FEA, to address effectively. Acetabular changes are among the most significant challenges in these patients. Alterations in the acetabular floor, distortion of the margins, and changes in version necessitate meticulous preoperative assessment and planning[52]. FEA, provides a powerful tool for simulating the optimal positioning and orientation of the acetabular component, ensuring the joint is both stable and functional. By addressing these changes before surgery, surgeons can minimize the risk of complications stemming from improper implant placement, such as instability or suboptimal load distribution.
Proximal femur variations add another layer of complexity to total hip arthroplasty in patients with childhood hip disorder sequelae. Anatomical differences, including decreased canal diameter[53], increased cortical thickness[54], changes in anteversion[55], and metaphyseal-diaphyseal mismatch[56], can make the placement of the femoral component particularly challenging. FEA, allows surgeons to model these variations and predict the most suitable implant design and placement strategy. By ensuring that the femoral component is adequately supported and aligned, FEA, reduces the risk of mechanical failure and enhances the overall stability and functionality of the implant. Through these capabilities, FEA, plays a crucial role in overcoming the challenges associated with acetabular and femoral abnormalities, improving surgical outcomes and patient satisfaction.
INCORPORATING MODULAR IMPLANTS AND CUSTOM SOLUTIONS
The use of modular implants has proven particularly advantageous in addressing the complex anatomical variations associated with childhood hip disorder sequelae. These implants provide the flexibility needed to adjust critical parameters such as neck length, offset, and anteversion during surgery, making them a valuable option for managing challenging cases. FEA plays a crucial role in optimizing the design and customization of these implants to meet the specific needs of each patient. FEA is instrumental in designing modular implants by simulating various configurations and assessing their biomechanical performance, such as performed by Luo et al[57]. Through these simulations, FEA identifies the most effective designs for restoring the hip center and achieving stable fixation. Modular implants tailored to the patient’s unique anatomy offer a more precise and effective solution, ensuring better implant stability and overall surgical outcomes. By accounting for individual anatomical differences, FEA helps refine modular implant designs, enhancing their compatibility and functionality. In addition to modular implants, FEA facilitates the development of patient-specific custom implants. These implants are designed to address unique anatomical anomalies, such as irregular bone shapes or sizes, ensuring a more accurate fit and better biomechanical integration[58]. By creating detailed models of the patient’s anatomy, FEA allows for the design of implants that conform precisely to their bone structure, improving both function and durability. This personalized approach significantly enhances surgical outcomes, providing patients with solutions that are specifically suitable to their needs.
ADVANCEMENTS IN IMAGING AND SIMULATION TECHNOLOGIES
The integration of advanced imaging techniques with FEA has the potential to significantly enhance the planning and execution of total hip arthroplasty. Techniques such as 3D printing[59], virtual reality[60], and augmented reality[61] provide detailed anatomical models and immersive simulations, which improve both preoperative planning and intraoperative navigation. These innovations enable a higher level of precision, ultimately leading to better surgical outcomes. One of the most impactful applications of advanced imaging is the creation of accurate 3D models[62]. Using advanced imaging technologies, highly detailed representations of the patient’s hip anatomy can be generated. These models can then be integrated with FEA simulations to plan implant placement and refine surgical techniques. The detailed visualization provided by 3D models allows surgeons to gain a comprehensive understanding of the patient’s unique anatomical features, enabling more precise and effective surgical planning. Additionally, virtual reality and augmented reality technologies offer transformative benefits for surgical training[63]. By creating immersive environments, these tools allow surgeons to practice complex procedures and refine their techniques in a risk-free setting. Surgeons can simulate various scenarios and develop the confidence needed to handle challenging cases. This improved training not only enhances surgical skills but also contributes to better patient outcomes by ensuring that surgeons are well-prepared for real-world procedures.
Augmented reality is particularly valuable during surgery, as it enhances intraoperative navigation[64]. By overlaying digital information onto the surgical field, augmented reality provides real-time guidance to the surgeon. This technology helps in visualizing anatomical landmarks, implant positioning, and surgical pathways, reducing the likelihood of errors. The real-time feedback augmented reality offers allows surgeons to make more informed decisions, improving the overall precision and success of the procedure. Together, these advanced imaging techniques and FEA represent a powerful combination for advancing the field of total hip arthroplasty.
FUTURE DIRECTIONS AND RESEARCH
The paper published by Oommen et al[5] highlighted current strategies for total hip arthroplasty in patients with childhood hip disorder sequelae but identifies opportunities for further research into FEA and advanced technologies to improve outcomes. Validating FEA models with clinical outcomes is crucial to ensure accuracy and reliability, enabling their broader adoption. Developing patient-specific simulations can enhance surgical planning by adapting approaches to individual anatomies, improving precision and effectiveness[65-67]. Combining FEA with advanced imaging techniques, such as 3D printing[59], virtual reality[60], and augmented reality[61] can provide detailed anatomical insights, supporting more accurate planning and navigation.
Innovations in surgical techniques informed by FEA, such as novel osteotomy methods[68] and implant designs[69], can address complex anatomical variations. Longitudinal studies on implant longevity will provide essential data on the long-term performance of implants and surgical approaches[70]. Multidisciplinary collaborations among surgeons, engineers, and scientists can drive the development of more sophisticated tools and solutions. Research into biomaterials for implants, optimizing their integration[71] and mechanical properties[72], offers potential for improved outcomes. Customized rehabilitation programs and studies quantifying the economic and quality-of-life benefits of advanced total hip arthroplasty techniques can further enhance patient care. Finally, real-time surgical guidance systems integrating FEA and robust surgeon training programs will ensure precision and the effective use of emerging technologies in clinical practice[73-75].
CONCLUSION
Total hip arthroplasty for adults who have experienced childhood hip disorders is a uniquely challenging procedure. These patients often have significantly altered anatomy and complex biomechanical demands that require careful consideration during surgery. By integrating advanced tools like FEA into the preoperative planning and execution of total hip arthroplasty, surgeons can achieve greater precision, optimize implant placement and design, and ultimately improve outcomes for these individuals. The paper published by Oommen et al[5] sheds light on effective strategies for managing these complex cases, and this editorial builds on that knowledge by exploring the transformative potential of FEA and other advanced technologies. With the detailed biomechanical insights that FEA provides, surgeons can create highly tailored approaches that address each patient’s unique needs. This not only leads to better functional recovery but also reduces the risk of complications and improves the overall quality of life for patients. As research and technology continue to advance, the integration of FEA into orthopedic surgery holds immense promise for setting new standards in the care of childhood hip disorder sequelae. To make this a reality, future efforts should focus on validating FEA models with clinical outcomes, developing patient-specific simulations, exploring cutting-edge imaging techniques, innovating surgical methods, and fostering collaboration across disciplines. By pushing these boundaries, the medical community can deliver the most effective, personalized care, helping patients regain mobility and lead fuller, healthier lives.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country of origin: Indonesia
Peer-review report’s classification
Scientific Quality: Grade C, Grade C
Novelty: Grade A, Grade B
Creativity or Innovation: Grade A, Grade B
Scientific Significance: Grade A, Grade C
P-Reviewer: Meng JH S-Editor: Bai Y L-Editor: A P-Editor: Zhang YL