Published online Jan 18, 2025. doi: 10.5312/wjo.v16.i1.102972
Revised: December 23, 2024
Accepted: January 2, 2025
Published online: January 18, 2025
Processing time: 70 Days and 23.4 Hours
This letter compares the clinical efficacy and economic feasibility of the scoliocorrector fatma-UI (SCFUI) with direct vertebral rotation (DVR) in treating adole
Core Tip: The innovative scoliocorrector fatma-UI (SCFUI), a significant advancement in the treatment of adolescent idiopathic scoliosis (AIS). It emphasizes SCFUI's efficacy in three-dimensional spinal deformity correction, comparing favorably to traditional methods. The document highlights the necessity for specialized training for surgeons in the use of SCFUI, its impact on long-term patient outcomes, and explores its cost-effectiveness. This comprehensive analysis positions SCFUI as a promising solution in AIS treatment, addressing current challenges and focusing on holistic patient care.
- Citation: Zhu JK, Li ZP, Zhou PH. Advances in 3D correction of adolescent scoliosis: The superiority of scoliocorrector fatma-UI in rotational realignment. World J Orthop 2025; 16(1): 102972
- URL: https://www.wjgnet.com/2218-5836/full/v16/i1/102972.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i1.102972
I am writing to discuss the recent article by Phedy et al[1] on the scoliocorrector fatma-UI (SCFUI) (Table 1). Before examining the technological innovations of SCFUI, it is essential to establish a clear understanding of adolescent idiopathic scoliosis (AIS), a condition that poses significant challenges in terms of its prevalence, risks, and healthcare costs.
| Section | Focus area | Importance |
| SCFUI development | Design and engineering of SCFUI | Foundational aspect of SCFUI |
| Finite element analysis | Stress and strain analysis | Ensures device safety and reliability |
| Biomechanical testing | Material strength and durability | Confirms material suitability for surgical use |
| Clinical trial design | Methodology and participant selection | Establishes trial validity and integrity |
| SCFUI vs DVR | Comparative effectiveness | Determines superiority over existing methods |
| Surgical procedure details | Step-by-step surgical application | Guides surgeons in practical application |
| Training for surgeons | Essential skills for using SCFUI | Crucial for effective use of SCFUI |
| Skill enhancement programs | Advanced training techniques | Enhances surgical proficiency |
| Patient follow-up protocols | Post-treatment monitoring | Critical for assessing treatment success |
| Long-term outcomes | Physical and health implications | Determines long-term treatment efficacy |
| Psychosocial considerations | Mental health and quality of life | Addresses patient's emotional and social needs |
| Cost-effectiveness analysis | Economic impact and healthcare resources | Evaluates financial viability and patient affordability |
AIS is a complex orthopedic condition that necessitates ongoing advancements in treatment strategies. Its three-dimensional deformity requires correction in the coronal, sagittal, and axial planes[2]. Current approaches, such as direct vertebral rotation (DVR), provide effective coronal and rotational corrections[3] but have notable limitations, including the risk of thoracic hypokyphosis[4,5] (Table 2). Addressing these shortcomings is critical for improving outcomes in AIS surgical management.
| Treatment method | Method name | Angle reduction degrees (SD) | Sample size | Average age (SD) | Average duration of treatment (week) | Outcome measures | Ref. |
| Improved | SCFUI | 3.17 (2.19) | 21 | 15.92 (0.35) | N/A | Rotational angle | |
| DVR | 1.19 (2.11) | 23 | 15.73 (1.51) | N/A | Rotational angle | [1] | |
| Conservative | Core Strength Training | 3.82 | 110 | 13.23 (2.40) | 12 | Cobb angle | |
| PSSE | 3.79 | 95 | 12.82 (1.19) | 24 | Cobb angle | ||
| Yoga | 4.60 | 32 | 18.63 (0.91) | 12 | Cobb angle | ||
| Schroth | 3.63 | 34 | 14.70 (1.30) | 24 | Cobb angle | [35] |
AIS affects a significant proportion of adolescents, presenting not only high incidence rates but also substantial healthcare costs[6,7]. Beyond spinal deformities, the condition is often complicated by risks such as neurological deficits, infections, and surgical hardware-related issues[8]. These factors exacerbate the economic burden of AIS, emphasizing the need for innovative, cost-efficient, and effective therapeutic approaches.
The SCFUI represents a promising advancement in AIS treatment, specifically designed to enhance three-dimensional correction. By overcoming the limitations of existing techniques like DVR, SCFUI has the potential to optimize surgical outcomes. The study by Phedy et al[1] highlights the development and evaluation of this innovative tool, providing valuable insights into its efficacy, safety, and functional outcomes.
The introduction of SCFUI is timely, given the pressing need for refined interventions that can achieve comprehensive correction across all planes while minimizing complications. This novel approach not only complements existing techniques but also aligns with the broader objective of reducing the healthcare burden associated with AIS.
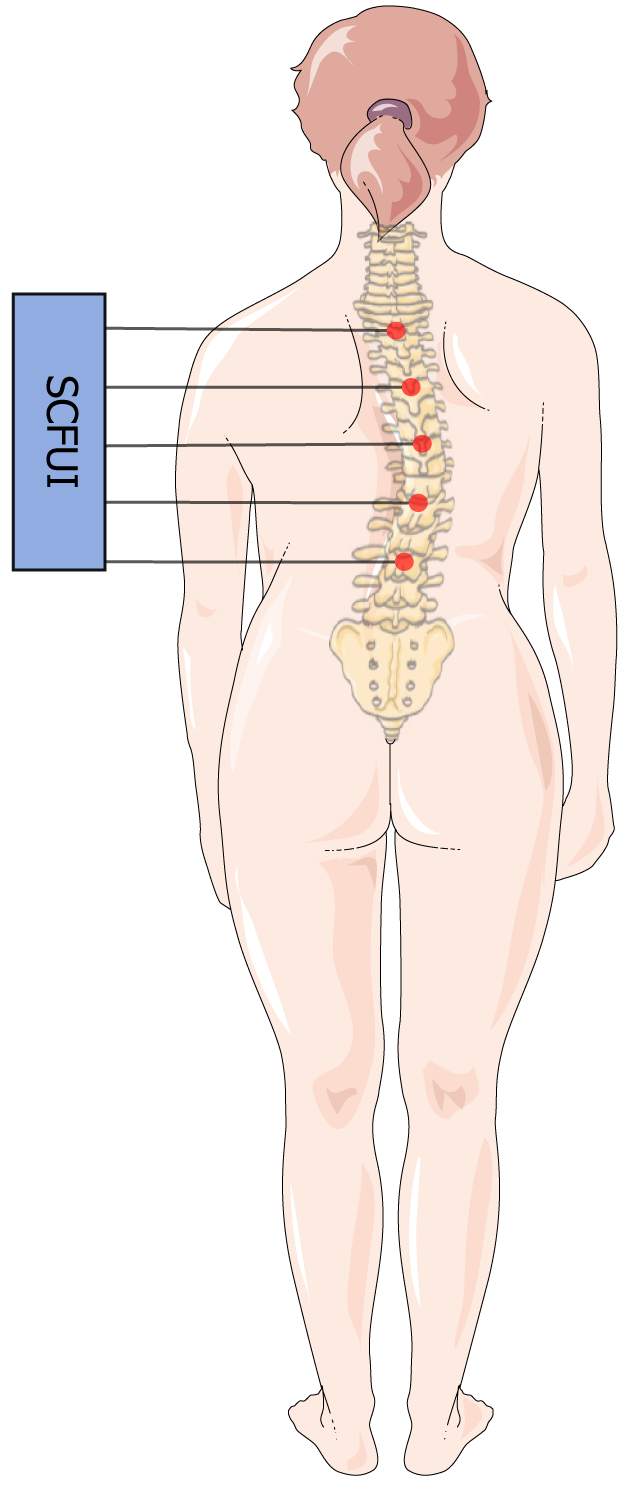
The SCFUI represents a breakthrough in the surgical management of AIS, offering a novel approach to three-dimensional spinal correction (Figure 1). Developed through extensive research involving finite element analysis and biomechanical testing, SCFUI was specifically designed to address the complex challenges of scoliosis correction. Its innovative design, incorporating pulleys, wires, and correction screws, enhances its efficacy and safety in clinical settings[1].
The SCFUI stands out in the treatment of AIS due to its superior rotational correction capability, surpassing traditional methods such as DVR[1,3,9]. Research has shown that SCFUI delivers significant improvements in axial rotational alignment, effectively reducing residual deformities while minimizing the risks of degenerative changes and biomechanical impairments. By addressing the limitations of conventional techniques, SCFUI mitigates long-term complications associated with inadequate correction. Its ability to achieve comprehensive three-dimensional spinal alignment not only enhances postoperative outcomes but also lowers the risk of complications, ultimately improving patients’ overall quality of life.
The findings from biomechanical and finite element analyses confirm the structural integrity of SCFUI, supporting its clinical application[1]. Clinical trials have further demonstrated its safety and efficacy, with patients treated using SCFUI showing improved spinal alignment without compromising neurological functions. Motor-evoked and somatosensory-evoked potentials remained stable, underscoring the tool's reliability in preserving neurological safety during surgery[1].
Furthermore, SCFUI represents a significant evolution in AIS treatment methodologies, reflecting a broader shift towards more precise, efficient, and safe surgical interventions. Its success in clinical trials and subsequent integration into surgical practice highlights the importance of continuous innovation in medical technology, particularly in orth
Despite its promising performance, further research is necessary to evaluate the long-term benefits and potential risks associated with SCFUI. Ongoing studies are essential to fully understand its implications for patient outcomes and refine its application in diverse clinical scenarios[1].
Overall, the development and implementation of SCFUI in AIS treatment mark a significant advancement in surgical technology. By addressing the limitations of existing techniques and providing a more comprehensive correction of complex spinal deformities, SCFUI exemplifies the dynamic nature of medical research and its critical role in advancing patient care in orthopedic surgery.
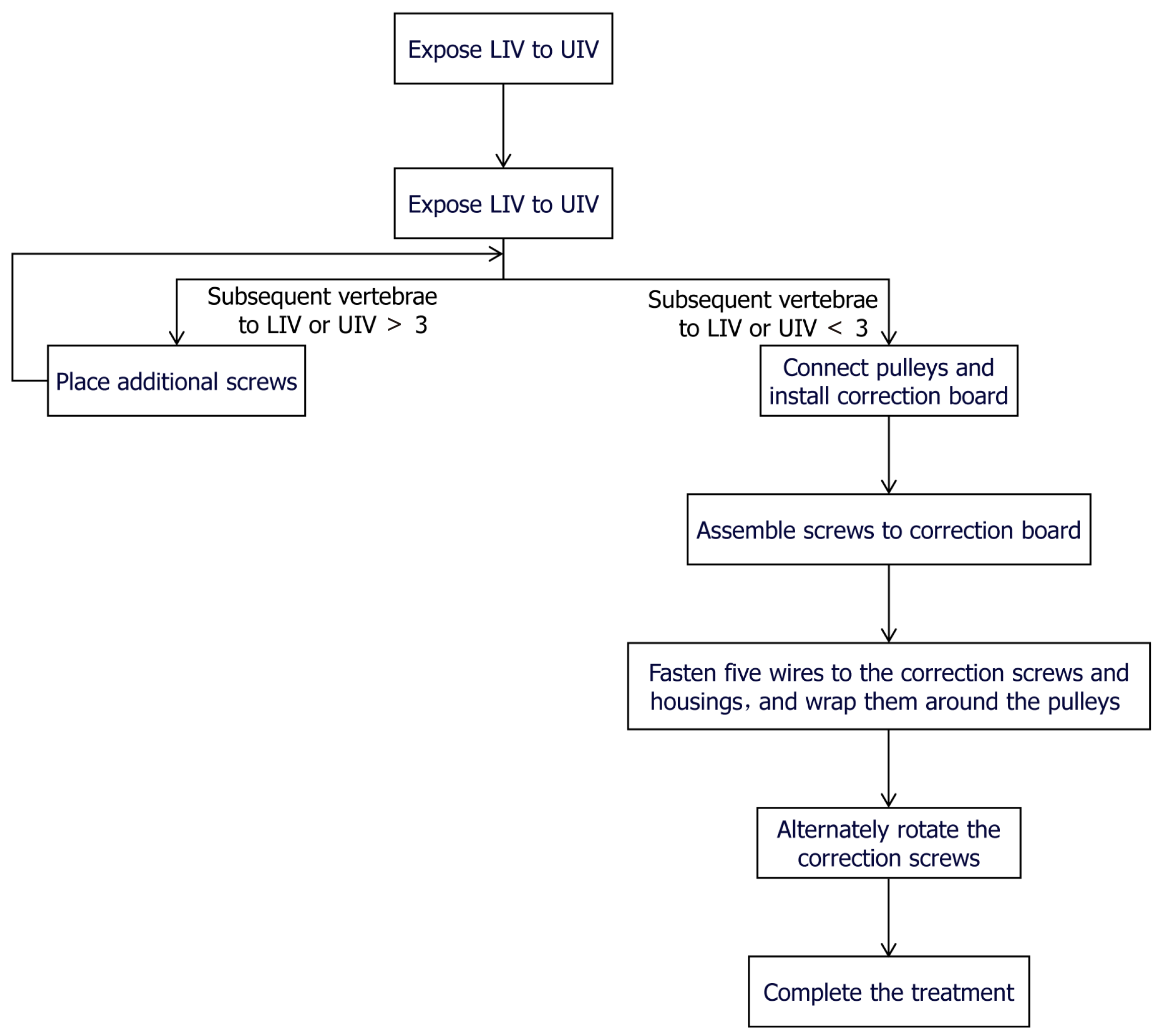
The development of the SCFUI for AIS treatment represents a significant advancement in surgical techniques. Training and skill development for surgeons using this tool is crucial, as it involves a complex procedure that requires a precise understanding of three-dimensional spinal deformities and their correction (Figure 2).
The SCFUI is designed to aid in the three-dimensional correction of scoliosis, a challenge in traditional methods[10-12]. Its development involved rigorous testing, including finite element and biomechanical analysis, to ensure its efficacy and safety in clinical applications. The device showed promising results in clinical trials, providing better rotational correction compared to DVR while maintaining similar safety and functional outcomes.
For surgeons, training in the use of SCFUI should encompass both the theoretical understanding of its design and practical skills in its application. This includes familiarization with the device's components, such as the correction board, screws, pulleys, and wires, and their proper assembly and application during surgery.
Given the complexity of AIS and the precision required in surgical interventions, simulation-based training could be highly beneficial for surgeons. This would allow them to practice the procedure in a controlled environment, minimizing the risk of complications during actual surgeries. Additionally, ongoing training and workshops could be instrumental in keeping surgeons updated on the latest developments and techniques associated with SCFUI.
Future research in this area could focus on simplifying the device for easier assembly and application, expanding its use for different types of scoliotic curves, and further evaluating its long-term outcomes compared to other surgical techniques. Such research would be invaluable in advancing the treatment of AIS and improving patient outcomes.
Long-term outcomes and patient follow-up in AIS research are crucial for understanding the impact of various treatments on patients' lives. Recent studies have provided valuable insights into these aspects (Table 2).
A systematic review and meta-analysis of randomized controlled trials and observational studies have assessed the impact of patient scoliosis-specific exercises (PSSE) on AIS outcomes. The results indicated that while PSSE led to some improvement in Cobb angle, it was not clinically significant. Moreover, the study found no substantial improvement in axial trunk rotation or SRS-22 scores, which assess scoliosis-related health quality of life[13].
Another key aspect of AIS research is the natural history and long-term health implications of the condition. Studies have shown that while AIS does not generally result in increased mortality, severe cases can lead to complications such as cardiorespiratory failure, especially in curves exceeding 110 degrees. Importantly, smaller curves (50-70° range) in adolescent-onset idiopathic scoliosis typically do not lead to such severe outcomes, especially in patients not bothered by pain or appearance concerns[14].
Additionally, an in-depth analysis comparing the long-term outcomes of conservative measures, like bracing and physical therapy, vs surgical interventions, revealed that the severity of lifelong pain correlates more with the degree of the curve rather than the type of treatment. The study also found that conservative treatment, such as bracing, can impact patients' self-image and mental health more significantly than surgical treatments[15].
Furthermore, corrective surgery for AIS, such as posterior spinal fusion, can bring several benefits including improvements in aesthetics, quality of life, disability, back pain, psychological well-being, and breathing function. However, long-term complications like neurological damage, strain on unfused vertebrae, and degenerative disc disease (DDD) also need to be considered. The outcomes after surgery showed variations, with some patients developing new DDD and others experiencing no association between the development of DDD and clinical findings like disability and pain[16].
Overall, these findings highlight the importance of considering both the physical and psychological impacts of AIS and its treatments in the long term. They also underscore the need for ongoing research to better understand the long-term effects of various treatment modalities in AIS.
The treatment costs for AIS have risen substantially over the past few decades, increasing from $55000 in 1997 to $177000 in 2012[1,6]. In response to this escalating financial burden, the development of SCFUI introduces a promising alternative for AIS management, underpinned by cost-effectiveness analysis (CEA).
CEA plays a pivotal role in AIS treatment by evaluating the economic and health outcomes of various therapeutic options. Its primary objective is to optimize the allocation of healthcare resources by comparing the costs and benefits of different interventions. This involves calculating the incremental cost-effectiveness ratio (ICER), which quantifies the additional cost required to achieve a unit of health improvement, such as extended life expectancy or enhanced functional capacity. The ICER serves as a critical metric for guiding decision-makers in selecting the most value-driven treatment strategies.
SCFUI exhibits notable cost-effectiveness advantages in clinical settings. Regarding correction outcomes, SCFUI matches the efficacy of traditional DVR techniques in the coronal and sagittal planes while demonstrating superior performance in rotational correction (11.59° ± 7.46° vs 18.23° ± 6.39°, P = 0.001). Clinical trials have further validated that the SCFUI and DVR groups share comparable safety profiles in terms of neurological function and overall outcomes. Finite element analysis reveals that the maximum stress on SCFUI components ranges between 31.2 and 252 MPa, and biomechanical testing indicates an elastic modulus of 9561324 ± 633277 MPa, underscoring the tool’s safety and reliability[1].
Economically, SCFUI offers significant advantages by streamlining surgical procedures, reducing operative time, minimizing the risk of complications, and shortening hospital stays. Its exceptional three-dimensional correction capabilities also lower the likelihood of revision surgeries, leading to substantial long-term cost savings. These benefits are particularly impactful in resource-constrained healthcare settings[1].
The introduction and application of SCFUI align seamlessly with contemporary healthcare policies focused on reducing medical expenses while ensuring high-quality treatment outcomes. By providing an innovative, cost-effective solution, SCFUI addresses the mounting financial challenges associated with AIS treatment, meeting the increasing demand for accessible and effective care.
The economic impact of AIS treatment is multifaceted. It includes direct costs like surgery, hospital stays, and ongoing medical care, and indirect costs like lost parental workdays and long-term care needs. For instance, the introduction of advanced treatments like SCFUI may initially increase direct costs due to the technology's novelty and required specialized training. However, if SCFUI leads to fewer complications and revisions, it could reduce long-term costs for families and healthcare systems.
The burden on families is not just financial. There's also an emotional and physical cost, including the stress of managing treatment schedules and the impact on family dynamics. Effective treatment strategies should consider these broader economic and familial impacts, ensuring that families are supported throughout the treatment process.
Healthcare accessibility is a significant factor in the treatment of AIS. It involves ensuring that patients have timely and effective access to the required medical services[17]. Key strategies to improve healthcare accessibility include managing appointment schedules effectively, reducing no-shows, and optimizing the utilization of healthcare resources[17].
Effective management of outpatient appointments is crucial. This can be achieved by implementing policies like open access scheduling and overlapping appointment models, which help to reduce patient wait times and improve the efficiency of healthcare providers[18]. Managing appointment cancellations and no-shows effectively, perhaps by maintaining a waiting list for same-day appointments, is also important[19]. These strategies can significantly improve patient satisfaction and treatment outcomes by ensuring timely access to care[20].
Such measures are particularly relevant in AIS treatment, where timely interventions can be critical to the success of the treatment plan[21]. Implementing these strategies can lead to better management of healthcare resources, improving access to care for AIS patients[22].
The impact of multiple systems and organs on adolescent mental health is a critical consideration in the treatment of AIS, which poses complex psychological and physical challenges. Adolescents with AIS often face diminished self-esteem, altered body image, and limitations in daily activities, contributing to psychological distress and social withdrawal[23,24]. These challenges are exacerbated by physical symptoms such as pain, discomfort, and restricted mobility, further affecting their mental well-being[25].
AIS treatments, both conservative and surgical, significantly influence patients' psychological health. Bracing, while effective in halting curve progression, is associated with increased anxiety and social challenges due to its visibility and physical discomfort[26]. Conversely, surgical interventions, though initially anxiety-inducing, often lead to substantial improvements in body image, self-esteem, and overall mental health post-operatively[27,28]. Recognizing these varied psychological impacts is crucial for developing comprehensive care strategies that address the full spectrum of AIS-related challenges.
Adolescent psychology is profoundly influenced by factors such as family dynamics, societal attitudes, and personal health perceptions, all of which play a crucial role in determining the outcomes of AIS treatment. Support from family members and healthcare providers is instrumental in shaping adolescents' attitudes toward their health and enhancing their adherence to treatment. A nurturing and supportive environment can significantly alleviate the psychological burden associated with AIS, promote resilience, and ultimately improve treatment outcomes[29].
Given these dynamics, a holistic approach to AIS treatment is essential. This involves addressing not only the physical deformities but also the psychological challenges associated with AIS[30]. Multidisciplinary treatment programs that integrate physical and mental health support are particularly effective[31,32]. Psychosocial interventions, including counseling, support groups, and educational initiatives, empower adolescents and their families to navigate the challenges of AIS treatment. These measures improve mental health outcomes, enhance quality of life, and promote treatment adherence.
By adopting a holistic, multidisciplinary approach, healthcare providers can create a supportive environment that actively involves adolescents in their care. This comprehensive strategy ensures optimal outcomes, addressing both the physical and psychological needs of patients with AIS while fostering long-term well-being and satisfaction.
Future research directions and potential developments in the field of AIS treatment are crucial for enhancing patient outcomes and advancing medical knowledge. Given the high incidence, risk, and cost associated with AIS, it is evident that innovative approaches are necessary.
One promising avenue is the refinement and assessment of cutting-edge surgical instruments and methods. A notable example is the SCFUI, as showcased in the study by Phedy et al[1] This innovative tool is designed to facilitate three-dimensional correction of scoliosis. Its demonstrated efficacy in clinical trials indicates a substantial potential for enhancing surgical results.
Future studies could focus on refining these tools for broader applicability, including different types of scoliosis curves. Additionally, exploring minimally invasive surgical techniques could reduce recovery times and complications. The integration of new materials and technology, like biocompatible implants or robotics, may also enhance precision in surgery.
Moreover, as AIS can have a substantial psychosocial impact on adolescents, future research should also explore comprehensive care approaches. This includes psychological support for patients, as well as post-operative rehabilitation strategies to improve long-term functional outcomes.
Finally, with advancements in genetics and molecular biology, research could delve into the underlying causes of AIS. Understanding the genetic components may lead to early detection methods or preventative strategies, potentially reducing the need for surgical interventions. Recent advancements in genetics and molecular biology have unveiled critical insights into the etiology and progression of AIS. Notably, variations in the LBX1 gene have been associated with increased susceptibility to AIS[33,34], highlighting the potential for genetic screening in early diagnosis and personalized treatment approaches. Furthermore, epigenetic studies have identified specific DNA methylation patterns correlated with AIS progression, suggesting that targeted epigenetic therapies could emerge as viable non-surgical interventions[35]. These genetic and epigenetic discoveries pave the way for developing predictive models and individualized treatment plans, ultimately enhancing patient outcomes and quality of life.
In summary, the future of AIS treatment lies in a multidisciplinary approach that combines surgical innovation, comprehensive patient care, and a deeper understanding of the condition's etiology. This approach not only aims at improving surgical techniques and outcomes but also at enhancing the overall quality of life for AIS patients.
This study underscores the superiority of SCFUI over DVR in rotational correction. However, limitations such as a small sample size, short follow-up period, and single-center design may affect the generalizability and comprehensiveness of the findings. The absence of patient-reported outcome measures (PROMs), such as the SRS-22 score, further limits the assessment of patients' quality of life and subjective benefits.
Future research should address these issues by increasing sample sizes, incorporating multi-center designs, extending follow-up durations, and integrating PROMs. These improvements will enhance the robustness of the evidence, providing stronger support for clinical application and decision-making.
| 1. | Phedy P, Dilogo IH, Indriatmi W, Supriadi S, Prasetyo M, Octaviana F, Noor Z. Scoliocorrector Fatma-UI for correction of adolescent idiopathic scoliosis: Development, effectivity, safety and functional outcome. World J Orthop. 2024;15:61-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (2)] |
| 2. | Peng Y, Wang SR, Qiu GX, Zhang JG, Zhuang QY. Research progress on the etiology and pathogenesis of adolescent idiopathic scoliosis. Chin Med J (Engl). 2020;133:483-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 93] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 3. | Kim GU, Yang JH, Chang DG, Suk SI, Suh SW, Song KS, Nam KY, Oh IS, Park HY, Kim SI, Kim YH, Ha KY. Effect of Direct Vertebral Rotation in Single Thoracic Adolescent Idiopathic Scoliosis: Better 3-Dimensional Deformity Correction. World Neurosurg. 2019;129:e401-e408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Urbanski W, Wolanczyk MJ, Jurasz W, Kulej M, Morasiewicz P, Dragan SL, Sasiadek M, Dragan SF. The impact of direct vertebral rotation (DVR) on radiographic outcome in surgical correction of idiopathic scoliosis. Arch Orthop Trauma Surg. 2017;137:879-885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Watanabe K, Nakamura T, Iwanami A, Hosogane N, Tsuji T, Ishii K, Nakamura M, Toyama Y, Chiba K, Matsumoto M. Vertebral derotation in adolescent idiopathic scoliosis causes hypokyphosis of the thoracic spine. BMC Musculoskelet Disord. 2012;13:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Kobayashi K, Sato K, Ando T, Imagama S. Changes in medical costs for adolescent idiopathic scoliosis over the past 15 years. Nagoya J Med Sci. 2023;85:333-342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Bozzio AE, Hu X, Lieberman IH. Cost and Clinical Outcome of Adolescent Idiopathic Scoliosis Surgeries-Experience From a Nonprofit Community Hospital. Int J Spine Surg. 2019;13:474-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Yoshihara H, Paulino C, Yoneoka D. Predictors of Increased Hospital Stay in Adolescent Idiopathic Scoliosis Patients Undergoing Posterior Spinal Fusion: Analysis of National Database. Spine Deform. 2018;6:226-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Kim HJ, Chang DG, Lenke LG, Pizones J, Castelein R, Trobisch PD, Watanabe K, Yang JH, Suh SW, Suk SI. Rotational Changes Following Use of Direct Vertebral Rotation in Adolescent Idiopathic Scoliosis: A Long-Term Radiographic and Computed Tomography Evaluation. Spine (Phila Pa 1976). 2024;49:1059-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 10. | Sikora-Klak J, Upasani VV, Ilharreborde B, Cross M, Bastrom TP, Mazda K, Yaszay B, Newton PO. Three-dimensional analysis of spinal deformity correction in adolescent idiopathic scoliosis: comparison of two distinct techniques. Childs Nerv Syst. 2021;37:555-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Almansour H, Pepke W, Bruckner T, Diebo BG, Akbar M. Three-Dimensional Analysis of Initial Brace Correction in the Setting of Adolescent Idiopathic Scoliosis. J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Mohamed RA, Yousef AM. Impact of Schroth three-dimensional vs. proprioceptive neuromuscular facilitation techniques in adolescent idiopathic scoliosis: a randomized controlled study. Eur Rev Med Pharmacol Sci. 2021;25:7717-7725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 13. | Baumann AN, Orellana K, Oleson CJ, Curtis DP, Cahill P, Flynn J, Baldwin KD. The impact of patient scoliosis-specific exercises for adolescent idiopathic scoliosis: a systematic review and meta-analysis of randomized controlled trials with subgroup analysis using observational studies. Spine Deform. 2024;12:545-559. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Asher MA, Burton DC. Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis. 2006;1:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 326] [Cited by in RCA: 344] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 15. | Pombrio R. Adolescent idiopathic scoliosis: Lifetime pain and quality of life analysis after treatment. Capstone Showcase 2022. Available from: https://scholarworks.arcadia.edu/showcase/2022/pa/4. |
| 16. | Ghandhari H, Ameri E, Nikouei F, Haji Agha Bozorgi M, Majdi S, Salehpour M. Long-term outcome of posterior spinal fusion for the correction of adolescent idiopathic scoliosis. Scoliosis Spinal Disord. 2018;13:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Zavatsky JM, Peters AJ, Nahvi FA, Bharucha NJ, Trobisch PD, Kean KE, Richard S, Bucello Y, Valdevit A, Lonner BS. Disease severity and treatment in adolescent idiopathic scoliosis: the impact of race and economic status. Spine J. 2015;15:939-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 18. | Almorsy L, Khalifa M. Improving Health Care Accessibility: Strategies and Recommendations. Stud Health Technol Inform. 2016;226:187-189. [PubMed] |
| 19. | Huang Y, Verduzco S. Appointment Template Redesign in a Women's Health Clinic Using Clinical Constraints to Improve Service Quality and Efficiency. Appl Clin Inform. 2015;6:271-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Kopach R, DeLaurentis PC, Lawley M, Muthuraman K, Ozsen L, Rardin R, Wan H, Intrevado P, Qu X, Willis D. Effects of clinical characteristics on successful open access scheduling. Health Care Manag Sci. 2007;10:111-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 101] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 21. | Creps J, Lotfi V. A dynamic approach for outpatient scheduling. J Med Econ. 2017;20:786-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Almomani I, AlSarheed A. Enhancing outpatient clinics management software by reducing patients' waiting time. J Infect Public Health. 2016;9:734-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Lee SB, Chae HW, Kwon JW, Sung S, Lee HM, Moon SH, Lee BH. Is There an Association Between Psychiatric Disorders and Adolescent Idiopathic Scoliosis? A Large-database Study. Clin Orthop Relat Res. 2021;479:1805-1812. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Rushton PR, Grevitt MP. What is the effect of surgery on the quality of life of the adolescent with adolescent idiopathic scoliosis? A review and statistical analysis of the literature. Spine (Phila Pa 1976). 2013;38:786-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 25. | Gallant JN, Morgan CD, Stoklosa JB, Gannon SR, Shannon CN, Bonfield CM. Psychosocial Difficulties in Adolescent Idiopathic Scoliosis: Body Image, Eating Behaviors, and Mood Disorders. World Neurosurg. 2018;116:421-432.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 26. | Mitsiaki I, Thirios A, Panagouli E, Bacopoulou F, Pasparakis D, Psaltopoulou T, Sergentanis TN, Tsitsika A. Adolescent Idiopathic Scoliosis and Mental Health Disorders: A Narrative Review of the Literature. Children (Basel). 2022;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 25] [Reference Citation Analysis (0)] |
| 27. | Pezham H, Babaee T, Bagheripour B, Asgari M, Jiryaei Z, Vahab Kashani R, Rahgozar M, Arazpour M. Stress level and quality of life of adolescents with idiopathic scoliosis during brace treatment. Turk J Phys Med Rehabil. 2022;68:231-237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 28. | von Soest T, Kvalem IL, Roald HE, Skolleborg KC. The effects of cosmetic surgery on body image, self-esteem, and psychological problems. J Plast Reconstr Aesthet Surg. 2009;62:1238-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 99] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 29. | Huang Y, Liu F, Gao D, Wang H. Family Functioning Affected by Adolescent Idiopathic Scoliosis in China: A Cross-Sectional Study. Front Pediatr. 2022;10:880360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 30. | Yan LI, Wong AY, Cheung JP, Zhu B, Lee KC, Liang SR, Ll JY, Ho BYW, Bressington D. Psychosocial interventions for teenagers with adolescent idiopathic scoliosis: A systematic literature review. J Pediatr Nurs. 2023;73:e586-e593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 31. | Negrini S, Carabalona R. Social acceptability of treatments for adolescent idiopathic scoliosis: a cross-sectional study. Scoliosis. 2006;1:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 32. | Luo M, Zhang Y, Huang S, Song Y. The Susceptibility and Potential Functions of the LBX1 Gene in Adolescent Idiopathic Scoliosis. Front Genet. 2020;11:614984. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Londono D, Kou I, Johnson TA, Sharma S, Ogura Y, Tsunoda T, Takahashi A, Matsumoto M, Herring JA, Lam TP, Wang X, Tam EM, Song YQ, Fan YH, Chan D, Cheah KS, Qiu X, Jiang H, Huang D; Japanese Scoliosis Clinical Research Group, TSRHC IS Clinical Group, International Consortium for Scoliosis Genetics, Su P, Sham P, Cheung KM, Luk KD, Gordon D, Qiu Y, Cheng J, Tang N, Ikegawa S, Wise CA. A meta-analysis identifies adolescent idiopathic scoliosis association with LBX1 locus in multiple ethnic groups. J Med Genet. 2014;51:401-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 34. | Neri S, Assirelli E, Manzetti M, Viroli G, Ialuna M, Traversari M, Ciaffi J, Ursini F, Faldini C, Ruffilli A. Identification of Epigenetic Biomarkers of Adolescent Idiopathic Scoliosis Progression: A Workflow to Assess Local Gene Expression. Int J Mol Sci. 2024;25. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 35. | Chen Y, Zhang Z, Zhu Q. The effect of an exercise intervention on adolescent idiopathic scoliosis: a network meta-analysis. J Orthop Surg Res. 2023;18:655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |