Published online Sep 18, 2024. doi: 10.5312/wjo.v15.i9.891
Revised: August 15, 2024
Accepted: August 27, 2024
Published online: September 18, 2024
Processing time: 53 Days and 23 Hours
Sport-induced injuries particularly affect young, healthy, and active individuals. Running, a popular and accessible sport, can cause a wide range of injuries, including stress fractures. Stress fractures can occur during high-intensity training or competitions, especially among well-trained amateurs and professional athletes. Adequate diagnosis can be complicated by the typically young age, unremarkable medical history, and vital condition of the patient. Stress fractures present insidiously, and this is specifically the case with stress fractures of the femoral neck. Timely intervention is crucial to prevent progressive displacement, as this can damage the blood supply to the femoral head.
A 30-year-old male runner presented to our outpatient clinic with persistent pain 3 weeks after running a marathon. X-ray showed a complete lateral fracture of the left femoral neck, which was treated surgically with a dynamic hip screw.
It is essential for healthcare providers to be vigilant for the subtle symptoms of stress fractures to ensure timely treatment. Early recognition prevents com
Core Tip: Sports-induced injuries primarily affect young, healthy, and active individuals. Stress fractures occur during high-intensity training, particularly among well-trained amateurs and professional athletes. Young age and a lack of medical history complicate the diagnosis of insidious femoral neck stress fractures. Failure to diagnose and initiate treatment leads to fracture progression, impacting vascular supply and overall outcome. Avascular necrosis requires more invasive and extensive treatment and increases the risk of complications and permanent disability.
- Citation: Oudmaijer CA, Paulino Pereira NR, Visser D, Wakker AM, Veltman ES, van Linschoten R. Lateral femoral neck stress fractures: A case report. World J Orthop 2024; 15(9): 891-901
- URL: https://www.wjgnet.com/2218-5836/full/v15/i9/891.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i9.891
Diagnosing (atypical) stress fractures of the femoral neck is complex due to their unfamiliarity and insidious presentation, often resulting in progressive displacement and delayed treatment. Timely diagnosis and intervention are crucial. In this article we discuss the diagnosis, treatment options and complications of lateral femoral neck stress fractures. Using a case from our clinic, we provide an overview of literature and the published cases of lateral femoral neck fractures.
Stress fractures are thought to occur due to repetitive loading that exceeds the bone’s regenerative capacity, most commonly affecting young, active individuals[1,2]. This condition is prevalent among marathon runners and endurance athletes, due to the repeated mechanical stress from prolonged and cumulative exertion[1,2]. While stress fractures occur in various locations—particularly in the tibia and metatarsals[2,3]—they are especially concerning when located at the femoral neck, due to the severe implications and treatment complexity. Stress fractures of the femoral neck are rare, and comprise only 2.5%-5% of all stress fractures[4]. The etiology of femoral neck stress fractures remains unclear, but the prevailing hypothesis suggests that repetitive forces on the hip joint cause micro-stress and bone fatigue, leading to a failure of structural integrity[1,2]. If undiagnosed and, therefore, untreated, these fractures can progress to a complete fracture, with consequences often exacerbated by their subtle presentation and risk of progressive displacement, potentially resulting in severe outcomes like fracture dislocation requiring prosthetic replacement.
It is important to distinguish stress fractures from acute fractures. Stress fractures develop gradually over time due to repetitive physical load or overuse, as a result of cumulative micro-damage to the bone[1,2]. Unlike acute fractures, stress fractures may initially present with mild, progressive pain during activity, which can worsen over time if not treated. Acute fractures of the hip occur suddenly due to a significant external force, such as a fall, car accident, or direct trauma[5-7]. These fractures are typically severe, immediate, and often result in a complete break of the bone. Patients usually experience intense pain and are unable to bear weight on the affected limb, requiring prompt medical intervention, often surgical, to stabilize the fracture[5-7]. These fractures predominantly affect older adults, especially those with com
Diagnosing (atypical) femoral neck stress fractures is challenging due to their insidious presentation. Patients often present with vague persistent groin or hip pain, initially mild and easily overlooked[8-10]. Pain typically worsens with physical activity and subsides with rest, often misinterpreted as muscle strain. Despite pain, walking is usually possible[8-10]. Clinical examination most often reveals full passive range of motion, with pain elicited only at extreme hip positions[10]. Active range of motion is often not complete due to the same pain. Early-stage stress fractures are frequently missed on standard radiographs, with initial sensitivity ranging from 15%-35%, which may improve to 30%-70% after 2-10 weeks[10]. Magnetic resonance imaging (MRI) is the most reliable diagnostic tool, showing bone edema at the fracture site, but MRIs are often only performed if symptoms are chronic[8]. Diagnosis is, therefore, often delayed, averaging 14 weeks[11], increasing the risk of fracture displacement, impacting blood flow to the femoral head, and subsequent avascular necrosis. Prompt and accurate diagnosis is crucial to prevent further complications, emphasizing the vital role of care providers in early detection and timely referral for additional investigation and treatment.
A 30-year-old male runner presented to our outpatient clinic at the department of Sports Medicine with persistent pain in the left groin, with the inability to fully bear weight. Initial symptoms began during a marathon, manifesting as transient muscle weakness and left groin pain after a ski trip. Symptoms progressed when he resumed his training program. As an experienced runner, he had trained regularly over the past year following a standardized program (building up to a mileage of 40-50 km a week, with 80% endurance and 20% intensive training) with no previous episodes of groin or hip pain. No recent changes in training intensity or quality were noted, aside from the skiing trip. His caloric intake was normal for his weight and activity level, with gradual intentional weight loss of 8 kg over the past 2 years. The patient had halted training and consulted a sports physician, who made the clinical diagnosis of left psoas muscle strain. During the subsequent 4 weeks, with medication for pain relief, rest, and graded training, the patient was able to resume activity without further issues or pain.
During the marathon, the patient ran pain-free for 37 km at his trained pace. At 37 km, he began experiencing progressive groin pain, becoming unable to fully bear weight on his left leg by 40 km. Despite the pain, the patient was able to finish the marathon in 4.5 hours (Figure 1). He subsequently visited his general practitioner on day 3 post-marathon due to increasing groin pain, tenderness over the greater trochanter, and inability to fully bear weight despite pain medication. The general practitioner diagnosed acute inflammation of the prior psoas muscle strain and advised increased pain medication and rest. During the following 3 weeks, the pain gradually reduced, but was still significant, and mobilization with support became possible. Due to the persistent pain, he (re-) consulted his general practitioner and a physiotherapist, eventually presenting to the outpatient clinic of the Sports Medicine department 3 weeks post-marathon.
At this point, the patient could not bear weight on his left leg without pain, although the pain had moderately improved.
The patient was not on any medication, and had an unremarkable social and occupational history.
The patient had no prior medical history.
The patient had no relevant family history regarding osteoporosis or bone disease, with only his grandmother having sustained a femoral fracture at the age of 81 after a fall.
Physical examination revealed no visible abnormalities. Passive movement of the affected side was nearly complete, with mild pain at full flexion. Active hip flexion was limited by pain from 90°, and isolated straight leg raising was impossible against resistance. Sensory, motor, and circulatory function were intact.
Not performed at the time of initial diagnosis.
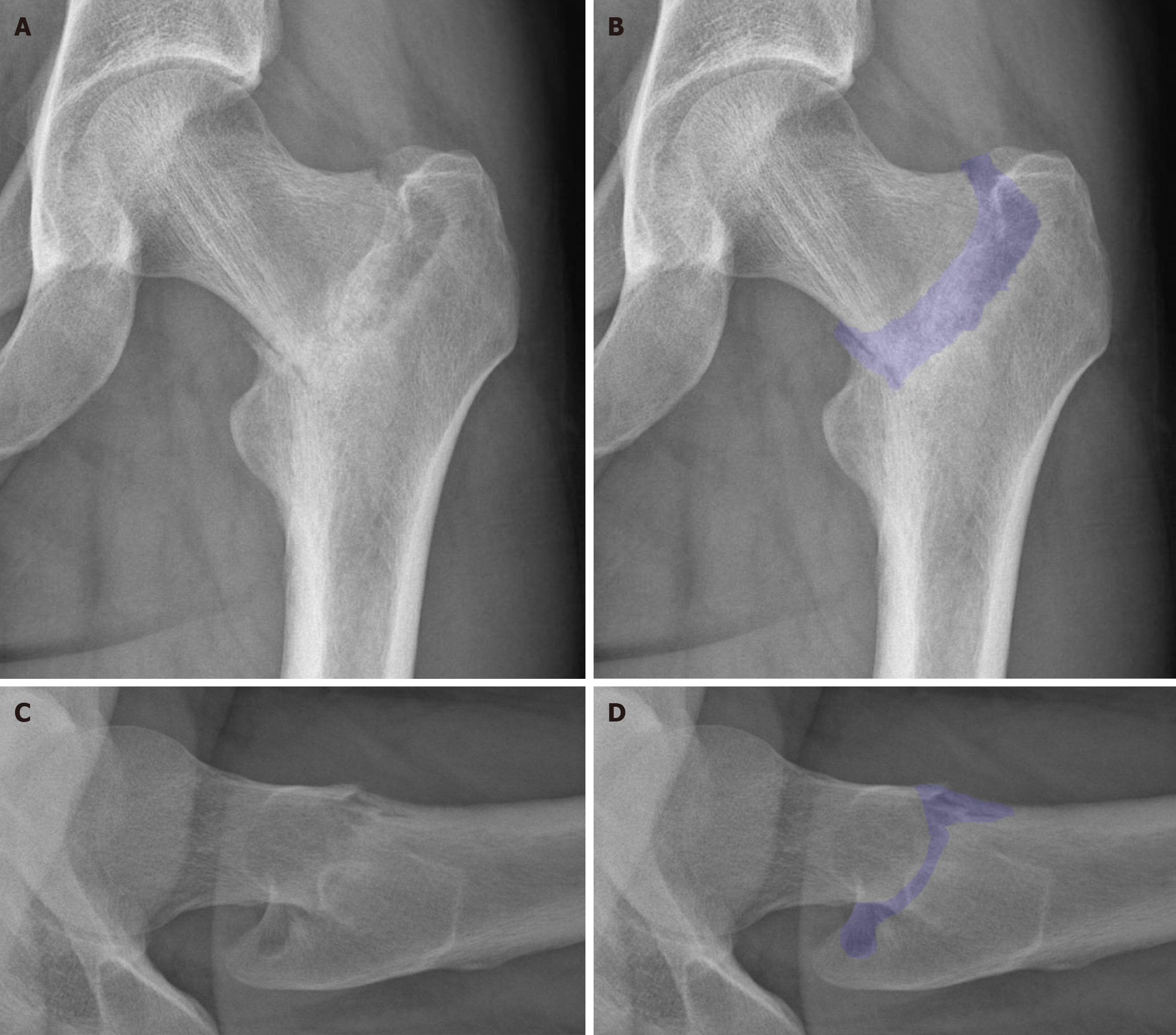
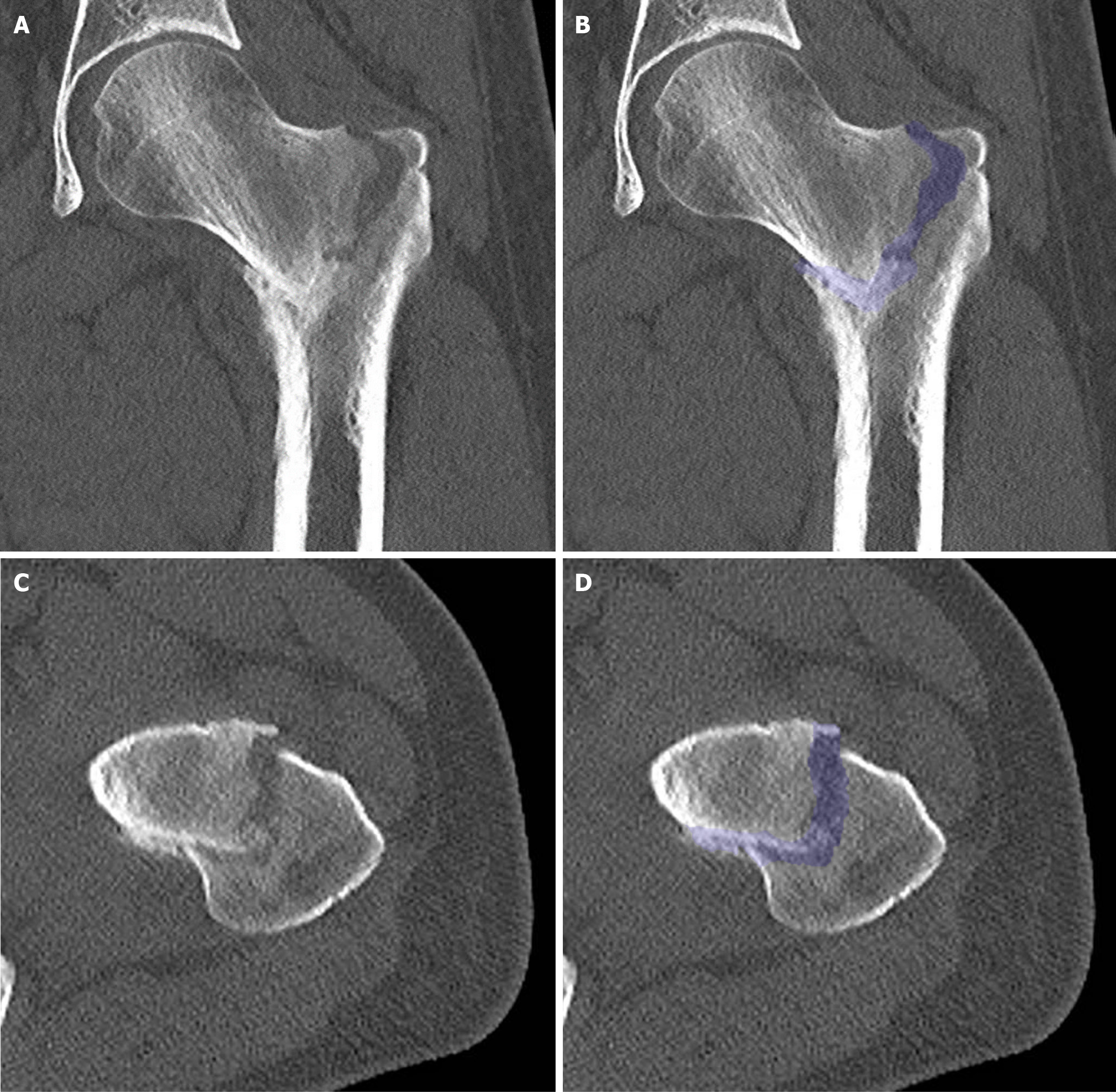
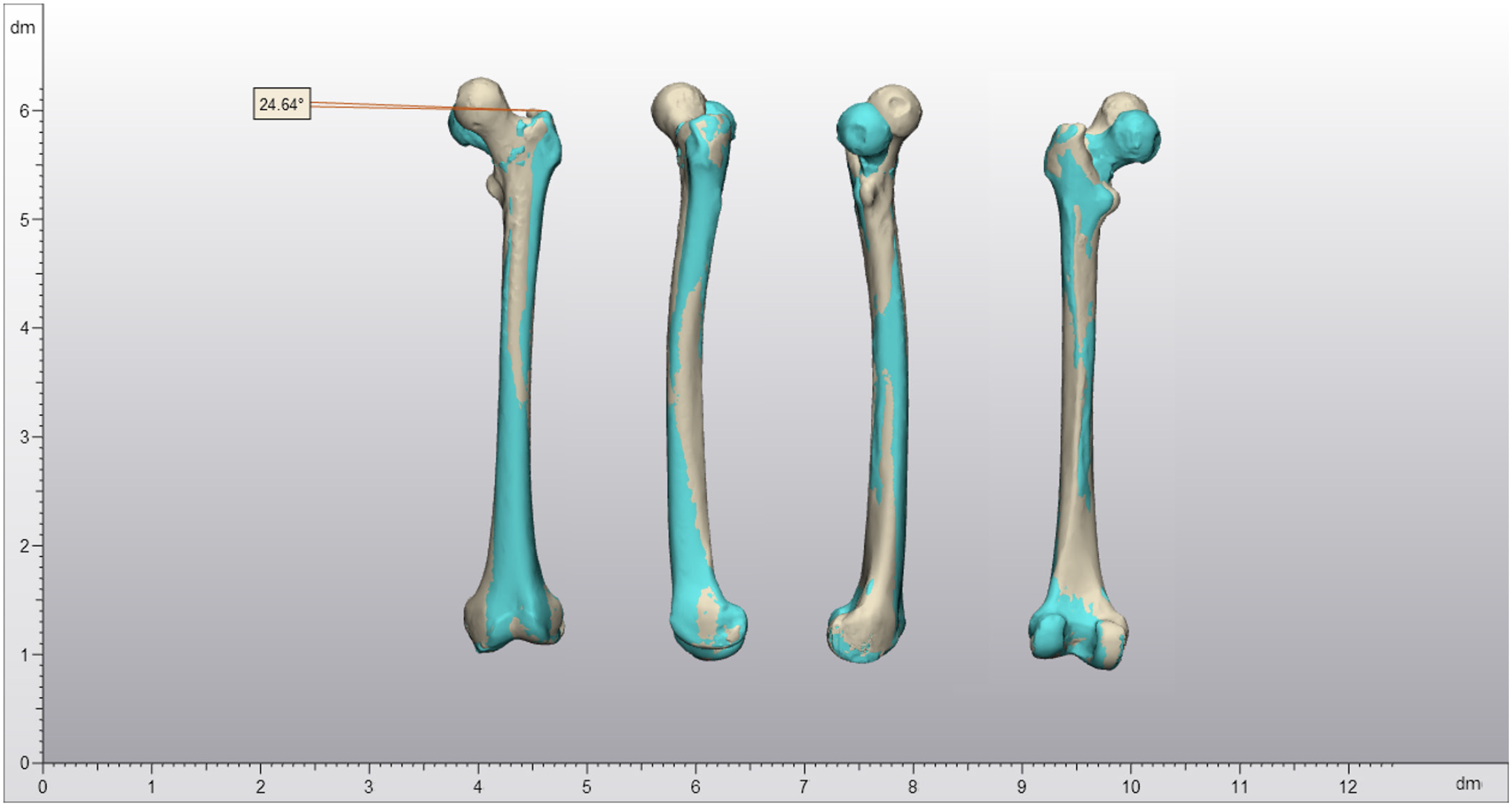
The subsequent X-ray showed a complete lateral fracture of the left femoral neck (Figure 2). A subsequent computed tomography scan (Figure 3) revealed no pre-existing bone pathology, but confirmed significant impaction and malalignment. The three-dimensional reconstruction (Figure 4) showed 24.6° external rotation and 16.0 mm shortening of the affected femur and the anatomical anteversion was neutralized due to the fracture.
Based on the duration and progression of symptoms, the hypothesis was that a stress fracture had initially healed due to rest in the 4 weeks preceding the marathon, but had progressed to a complete fracture during the marathon. However, an atypical femur fracture directly related to the marathon was a viable alternative.
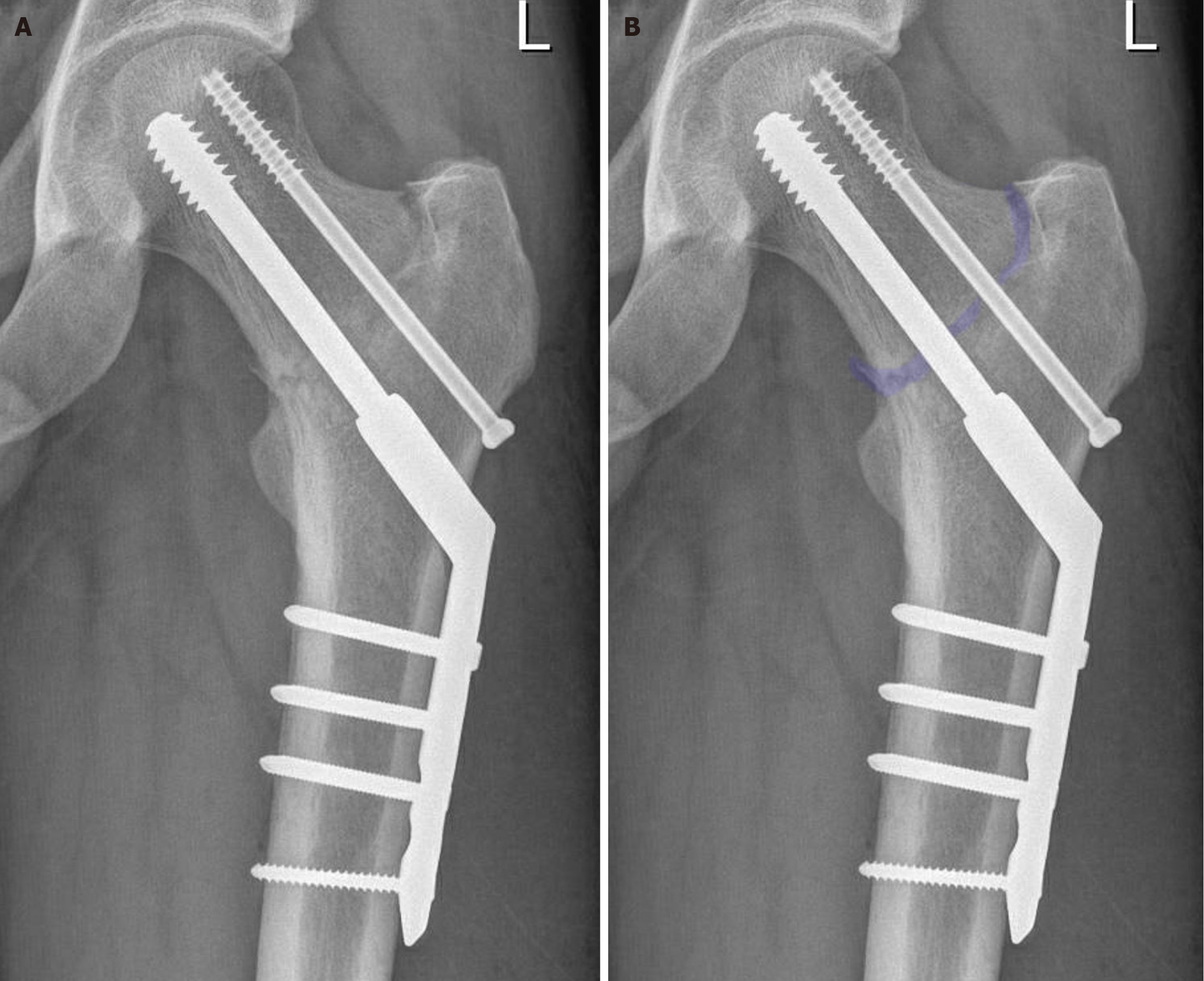
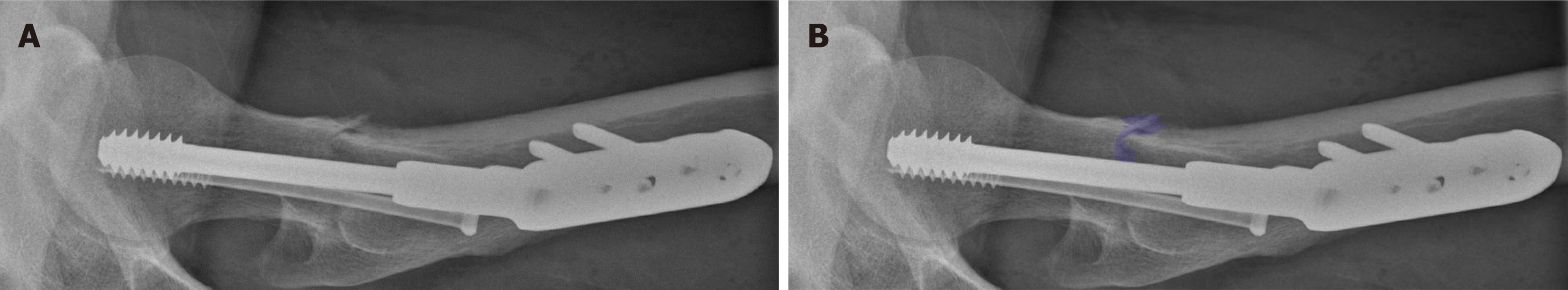
The patient underwent surgical fixation with a dynamic hip screw the day after outpatient clinic presentation. Despite the delay in presentation, anatomical alignment was successfully achieved. At the start of surgery, repositioning was acquired with traction. Afterwards, a cannulated screw (short threads were intentionally used) was placed first, to acquire more traction on the cranial side, thereby inducing more valgus alignment. The dynamic hip screw was then placed, and a four-hole plate was used due to the nature of the fracture and the unavailability of histopathology at that time. The postoperative course was uneventful, and the patient was discharged the day after surgery following initial mobilization under physiotherapy supervision and a weightbearing X-ray (Figure 5).
Given the insufficiency fracture, the atypical lateral fracture pattern, delayed presentation, and a potential underlying bone mineral pathology, partial (50%) weightbearing was advised for 6 weeks, with 10% in the first 2 weeks. Histopathology revealed no signs of bone disease or malignancy. During outpatient follow-up, the patient made satisfactory progress under physiotherapy supervision, and a 6-week radiograph showed no change in alignment (Figure 6).
After this, the patient initiated full weightbearing under supervision of a physiotherapist. He resumed work within a week post-surgery, initially working from home for 2 weeks. The endocrinologist was consulted to exclude any metabolic predisposition, finding no underlying cause for the fracture. No abnormal measurements were found for vitamin D, calcium and phosphorus metabolism, parathyroid hormone and type I procollagen carboxy terminal propeptide, and amino terminal propeptide. However, initial examination at 6 weeks post-surgery, 9 weeks post-injury, did show disuse osteopenia of the affected leg, with heightened urinary electrolyte excretion, due to excess intake, as the rest of the body was unaffected and showed normal bone mass on DEXA-examination.
At follow-up at 3 months post-surgery, our patient had improved significantly, partly due to extensive rehabilitation therapy by a specialized physical therapist, and was able to do all his daily activities, including his work as a clinical resident, without any pain or limitations. Under strict supervision, he aims to resume his physical activities, such as tennis and running (Figure 7).
Based on the cases presented in Table 1, a common theme emerges despite varying individual factors. Obviously, these atypical stress fractures typically occur following significant increases in mileage, often during marathon training or after initiation of running regimens. Predisposing factors such as medical histories or causative agents (e.g., the female athletic triad or osteoporosis) are generally absent. Absence of these predisposing factors are most likely due to publication bias, as cases where stress fractures are the result of osteoporosis, make relatively unremarkable cases. All the cases had complete fractures with varying degrees of displacement, with almost all managed surgically with a dynamic hip screw to stabilize the fracture site, after which partial weightbearing was initiated. Post-treatment outcomes show successful recovery trajectories, with patients achieving pain-free mobility and returning to physical activities gradually over weeks to months. However, there is no consistency in reporting whether patients returned to their pre-fracture level of activity, for instance long-lasting running regimens.
| Ref. | Case description | Cause of injury | Predisposing factors | Diagnosis | Treatment | Outcome |
| Biz et al[13] | 33-year-old female | Marathon training | Previous history of anorexia with amenorrhea | Left femoral lateral fracture, incomplete in the posterior-distal part | DHS + 30 days of partial weightbearing | At 12-month follow-up, she was completely pain-free and demonstrated full range of motion |
| Biz et al[13] | 48-year-old female | Initiated running | None | Complete and displaced left femoral neck base stress fracture | DHS + 30 days of no weightbearing. Subsequently increasing load over 20 days to complete load | At 3-month follow-up, she was able to walk, pain-free and had started stationary cycling and swimming |
| Cichy et al[9] | 23-year-old male marathon runner | Marathon | None | Complete, minimally displaced basicervical fracture of the right femoral neck | DHS + 6 weeks of partial weightbearing | No avascular necrosis, lights sports |
| Clough et al[10] | 55-year-old male | Marathon training | None | Displaced lateral fracture of the right femoral neck, which had collapsed into varus, with a neck-shaft angle of 110° | DHS | Not mentioned |
| Ejnisman et al[14] | 56-year-old female | No clear causative agent | None | Complete fracture of the base of the femoral neck with subtle displacement | 3x CHS | Full recovery after 6 months |
| Kerr et al[12] | 32-year-old male | Marathon | None | Lateral fracture of the femoral neck with varus displacement and a neck-shaft angle of 90° | DHS + 6 months of partial weightbearing | Full weightbearing, lights sports at 8 months |
| Scott et al[15] | 50-year-old male marathon runner | Increased his running mileage | None | Slightly displaced fracture through the base of the neck of the right proximal femur | 3x CHS + 6 weeks of partial weightbearing | Full weightbearing, light sports at 12 weeks |
Stress fractures occur when repetitive loading surpasses the body’s ability to regenerate, and are common in young and active individuals[1,2]. This condition is particularly prevalent among marathon runners and other endurance athletes due to the repeated mechanical stress from prolonged and cumulative exertion[1,2]. The hypothesis of etiology of stress fractures is that repetitive forces on the hip joint cause micro-stress and fatigue, leading to a failure of structural integrity[1,2]. If undiagnosed and untreated, these fractures can progress and displace, potentially leading to severe complications such as avascular necrosis. Diagnosing an (atypical) femoral neck stress fracture presents challenges due to its subtle onset; patients typically report persistent, vague groin or hip pain that initially is mild and often misdiagnosed[8-10]. Pain worsens with activity, but improves or resolves with rest, mimicking symptoms of muscle overuse. Initial radiographs often miss early fractures, exhibiting low sensitivity; initially ranging from 15%-35%, increasing to 30%-70% after 2-10 weeks[10]. MRI represents the current golden standard, but is often employed only after prolonged complaints and, therefore, the diagnosis is frequently delayed by an average 14-week interval[11].
Delayed diagnosis increases the risk of progressive displacement of the fracture, leading to reduced blood supply and increasing the risk of avascular necrosis[10-12]. Complications such as displacement of an initially well-aligned fracture, varus deformity, avascular necrosis, and non-union are not very common, but unfortunately delayed diagnoses are frequent[10-12]. The degree of fracture displacement is the most critical factor affecting the patient’s prognosis[11]. Regarding medial column fractures, progressive displacement leads to a 60% reduction in sports activity levels and a 30% incidence of avascular necrosis[10,11]. No information is available regarding these important predictors of long-term functioning for lateral column fractures. Therefore, a quick and accurate diagnosis is crucial to prevent further complications. General practitioners and other primary care providers play an essential role in early detection. By being alert to the symptoms of stress fractures, physicians can refer patients for further investigation and treatment in a timely manner, significantly improving the prognosis.
Femoral neck stress fractures can be treated conservatively or surgically, depending on the severity and stability of the fracture. Conservative treatment is only justifiable for an incomplete fracture on the medial side, i.e. the compression side[8]. This approach involves rest and non-weightbearing mobilization of the affected leg, followed by a gradual increase in weightbearing over 12 weeks[8]. However, if the fracture is on the lateral side, there is a high risk of progression, necessitating primary surgical treatment, most preferably with cannulated hip screws or a dynamic hip screw[8]. Surgical fixation should be considered in all cases, even for incomplete medial fractures, as it allows for immediate postoperative weightbearing. Prolonged immobilization is unacceptable for the typically young patient group[3,8].
Displaced fractures or fractures that have existed for a longer time, with a high risk of non-union and avascular necrosis, require surgical intervention[3,8]. The preferred method is surgical fixation, often by means of a dynamic hips screw or cannulated hip screws, aiming to restore anatomy and maintain adequate blood supply to the femoral head[8,11,12]. Surgical fixation of (incomplete) lateral, medial, or displaced fractures, can be performed with specific fixation methods depending on the degree of displacement, angle of the fracture, and patient-related factors. These methods vary from cannulated hip screws, dynamic hip screws, and intramedullary pens, to complete hip replacement surgery.
Recovery after surgery varies significantly depending on the duration, alignment, and severity of the fracture[8,11,12]. Conservatively treated, non-displaced fractures have a better prognosis and a shorter recovery period. Displaced fractures and cases with avascular necrosis often require long-term rehabilitation and can result in permanent limitations, both during sport and daily activities[8]. Therefore, timely and adequate treatment is vital to ensure the best possible outcome for the patient.
In our case, the initial presentation during marathon training was particularly insidious, given the rapid transient nature and absence of symptoms during other sport activities. Initial additional diagnostics would not have revealed a stress fracture, which would have only been detected by MRI as an area of bone edema[8]. During the second presentation, when there was a complete lateral fracture, timely radiographic diagnosis would have resulted in earlier surgical fixation, significantly lowering the risk of non-union, complications, and making a return to pre-existing functioning more likely[9,10,12]. However, timely detection of a femoral neck (stress) fracture is extremely challenging due to the non-specific clinical symptoms. The symptoms can be easily misinterpreted, and a prolonged diagnosis period is common[8,11,13-15], due to the low incidence of stress fractures, the vitality of young patients, and atypical symptoms, leading to muscle overuse being be more likely. Consequently, insufficient action is often taken. Increased alertness and a lower threshold for additional diagnostics in the presence of persistent and/or atypical hip or groin pain in active patients results in earlier identification and appropriate treatment.
It is essential for healthcare providers, specifically those in primary care and emergency departments, to be vigilant for the subtle symptoms of stress fractures to ensure timely diagnosis and treatment. Early recognition and intervention can prevent complications such as avascular necrosis and permanent disabilities, leading to a better prognosis with recovery to pre-existing levels of functioning.
Our thanks go out to all involved staff at the Erasmus MC.
| 1. | Neidel P, Wolfram P, Hotfiel T, Engelhardt M, Koch R, Lee G, Zwingenberger S. Cross-Sectional Investigation of Stress Fractures in German Elite Triathletes. Sports (Basel). 2019;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Rizzone KH, Ackerman KE, Roos KG, Dompier TP, Kerr ZY. The Epidemiology of Stress Fractures in Collegiate Student-Athletes, 2004-2005 Through 2013-2014 Academic Years. J Athl Train. 2017;52:966-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 131] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 3. | McInnis KC, Ramey LN. High-Risk Stress Fractures: Diagnosis and Management. PM R. 2016;8:S113-S124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 4. | Dutton RA. Stress Fractures of the Hip and Pelvis. Clin Sports Med. 2021;40:363-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (1)] |
| 5. | LeBlanc KE, Muncie HL Jr, LeBlanc LL. Hip fracture: diagnosis, treatment, and secondary prevention. Am Fam Physician. 2014;89:945-951. [PubMed] |
| 6. | Marks R, Allegrante JP, Ronald MacKenzie C, Lane JM. Hip fractures among the elderly: causes, consequences and control. Ageing Res Rev. 2003;2:57-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 171] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 7. | Schroeder JD, Turner SP, Buck E. Hip Fractures: Diagnosis and Management. Am Fam Physician. 2022;106:675-683. [PubMed] |
| 8. | Weinrich L, Dahne M, Lindner T, Stöckle U, Tsitsilonis S. Femoral Neck Stress Fracture of a Male, Healthy Marathon Runner - Case Report and Literature Review. Z Orthop Unfall. 2022;160:564-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Cichy B, Roche SJ, Wozniak A. Atypical femoral neck stress fracture in a marathon runner: a case report and literature review. Ir J Med Sci. 2012;181:427-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Clough TM. Femoral neck stress fracture: the importance of clinical suspicion and early review. Br J Sports Med. 2002;36:308-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Johansson C, Ekenman I, Törnkvist H, Eriksson E. Stress fractures of the femoral neck in athletes. The consequence of a delay in diagnosis. Am J Sports Med. 1990;18:524-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 107] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Kerr PS, Johnson DP. Displaced femoral neck stress fracture in a marathon runner. Injury. 1995;26:491-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Biz C, Berizzi A, Crimì A, Marcato C, Trovarelli G, Ruggieri P. Management and treatment of femoral neck stress fractures in recreational runners: a report of four cases and review of the literature. Acta Biomed. 2017;88:96-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 14. | Ejnisman L, Wajnsztejn A, Queiroz RD, Ejnisman B. Unusual presentation of a femoral stress fracture. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Scott MP, Finnoff JT, Davis BA. Femoral neck stress fracture presenting as gluteal pain in a marathon runner: case report. Arch Phys Med Rehabil. 1999;80:236-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |