Published online Aug 18, 2024. doi: 10.5312/wjo.v15.i8.820
Revised: July 19, 2024
Accepted: July 29, 2024
Published online: August 18, 2024
Processing time: 51 Days and 18.8 Hours
Acute injuries to the tibiofibular syndesmosis, often associated with high ankle sprains or malleolar fractures, require precise diagnosis and treatment to prevent long-term complications. This case report explores the use of needle arthroscopy as a minimally invasive technique for the repair of tibiofibular syndesmosis injuries.
We report on a 40-year-old male patient who presented with a trimalleolar fracture and ankle subluxation following a high ankle sprain. Due to significant swelling and poor soft tissue quality, initial management involved external stabilization. Subsequently, needle arthroscopy was employed to assess and treat the tibiofibular syndesmosis injury. The procedure, performed under spinal anest
This technique may enhance clinical outcomes and reduce recovery times, war
Core Tip: Needle arthroscopy demonstrates significant potential as a minimally invasive technique for the repair of acute tibiofibular syndesmosis injuries, offering enhanced visualization and diagnostic accuracy over traditional methods. In a case study of a 40-year-old male with a trimalleolar fracture, this method resulted in substantial improvements in pain, range of motion, and functional outcomes, achieving full recovery within 26 weeks. These findings suggest that needle arthroscopy could become a preferred approach in managing such injuries, promoting faster recovery and reducing the risk of complications. Further research is warranted to confirm these benefits.
- Citation: Wojtowicz BG, Domzalski M, Lesman J. Needle arthroscopic-assisted repair of tibio-fibular syndesmosis acute injury: A case report. World J Orthop 2024; 15(8): 820-827
- URL: https://www.wjgnet.com/2218-5836/full/v15/i8/820.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i8.820
The tibiofibular syndesmosis comprises four ligaments: The interosseous ligament, the anterior inferior tibiofibular ligament, the posterior inferior tibiofibular ligament, and the transverse tibiofibular ligament. These ligaments are frequently injured during high ankle sprains or malleolar fractures.
According to the study by McCollum et al[1], the most accurate examination for assessing isolated injury to the tibiofibular syndesmosis is computed tomography of the bilateral ankle joints, where a difference in syndesmosis width exceeding 2 mm is indicative[1]. In malleolar fractures, evidence shows that in the AO41-B variant, Weber type B, the syndesmosis is injured in 50% of cases, while in the AO41-C variant, Weber type C, it is almost always injured[2,3]. Advancements in functional outcomes following ankle fractures over the last five decades have underscored the importance of achieving anatomical realignment of the fracture and restoring the integrity of the articular surface[4]. Despite these advancements, complications such as chronic pain, arthrofibrosis, recurrent swelling, and perceived instability remain common after ankle fractures. These issues may arise due to suboptimal alignment of the articular surface and additional damage to the articular cartilage, which may not be diagnosed in standard imaging tests[5,6].
Arthroscopy has provided a safe and effective means of addressing various pathological conditions involving the tibiotalar joint. Ankle arthroscopy serves both diagnostic and therapeutic purposes. In 1993, Ferkel and Orwin[7] highlighted the value of ankle arthroscopy in the evaluation and management of ankle fractures.
In acute injuries, ankle arthroscopy allows for comprehensive examination of the cartilage surfaces of the talus, tibia, and fibula, as well as the intra-articular ligaments. and the tibiofibular syndesmosis.
In recent years, needle arthroscopy has been gaining popularity as a less invasive procedure than standard arthros
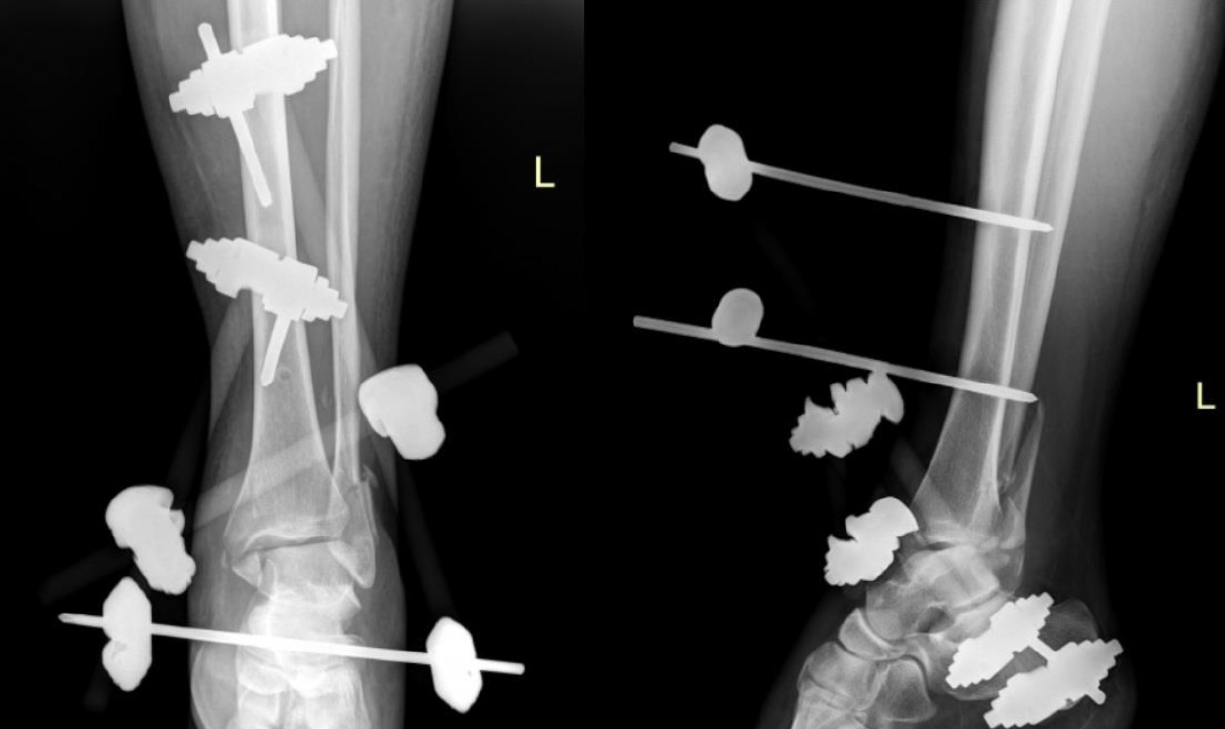
A 40-year-old man was brought to our emergency care unit due to increasing swelling of the lower limb approximately 3 days after a sprain injury of the ankle joint. X-rays revealed trimalleolar fracture with ankle subluxation (Figure 1). Due to significant swelling around the ankle joint and poor soft tissue quality, primary closed reduction with external stabilization (DePuy Synthes, West Chester, PA, United States) was performed (Figure 2). The external fixator was removed 27 days later due to swelling and poor skin condition, and the fracture was converted to internal fixation.
Given the expected fibrosis inside the tibiofibular syndesmosis during preoperative planning, nanoscopy was indicated to assess the mobility of the tibiofibular syndesmosis and potentially refresh it to prevent interference with anatomical repositioning. The patient was placed supine under spinal anesthesia. A tourniquet was used, and the procedure was performed under fluoroscopic control. The fibula was anatomically reduced, and the fracture was stabilized using a dedicated plate and locking screws (Arthrex, Naples, FL, United States).
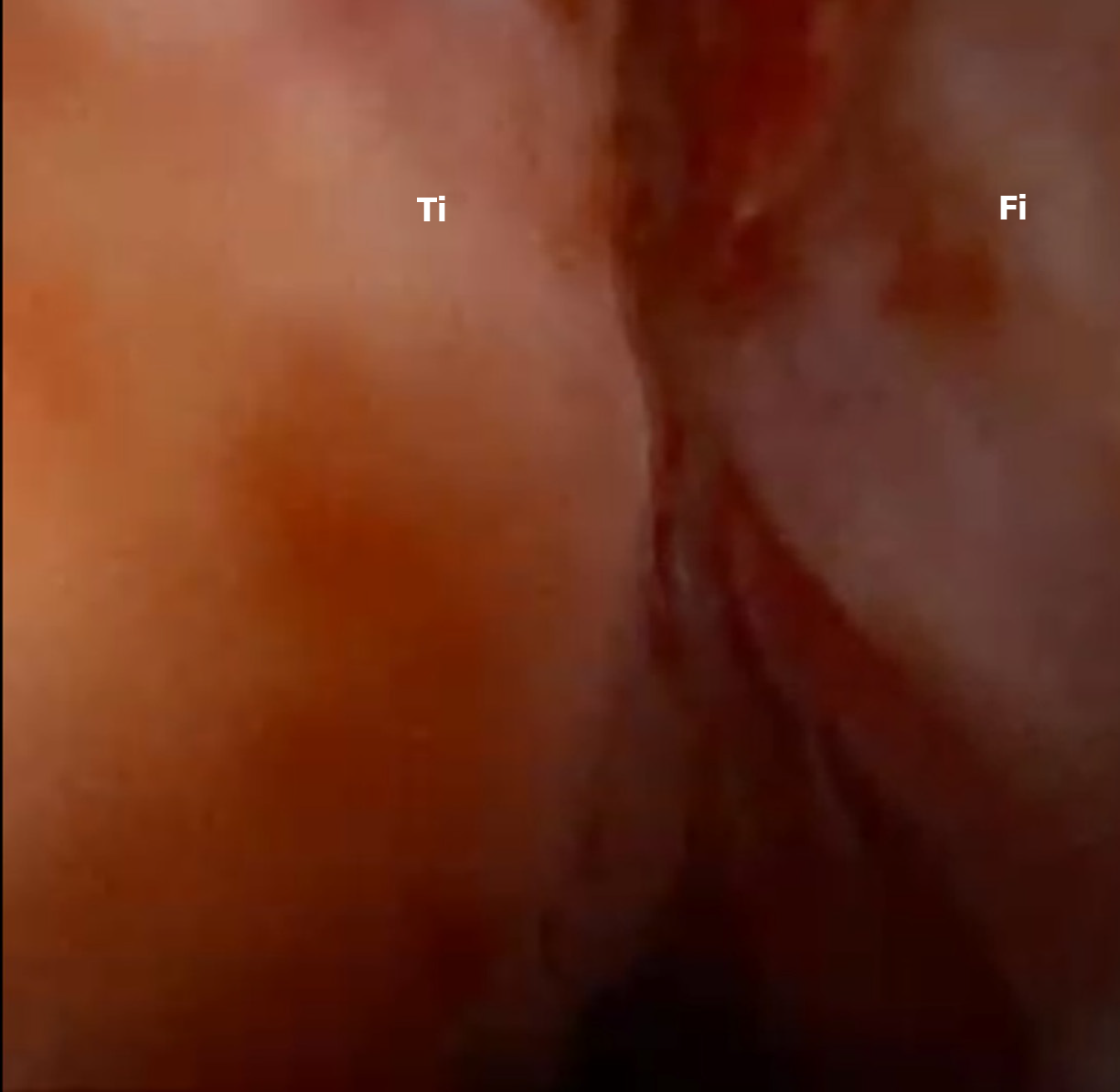
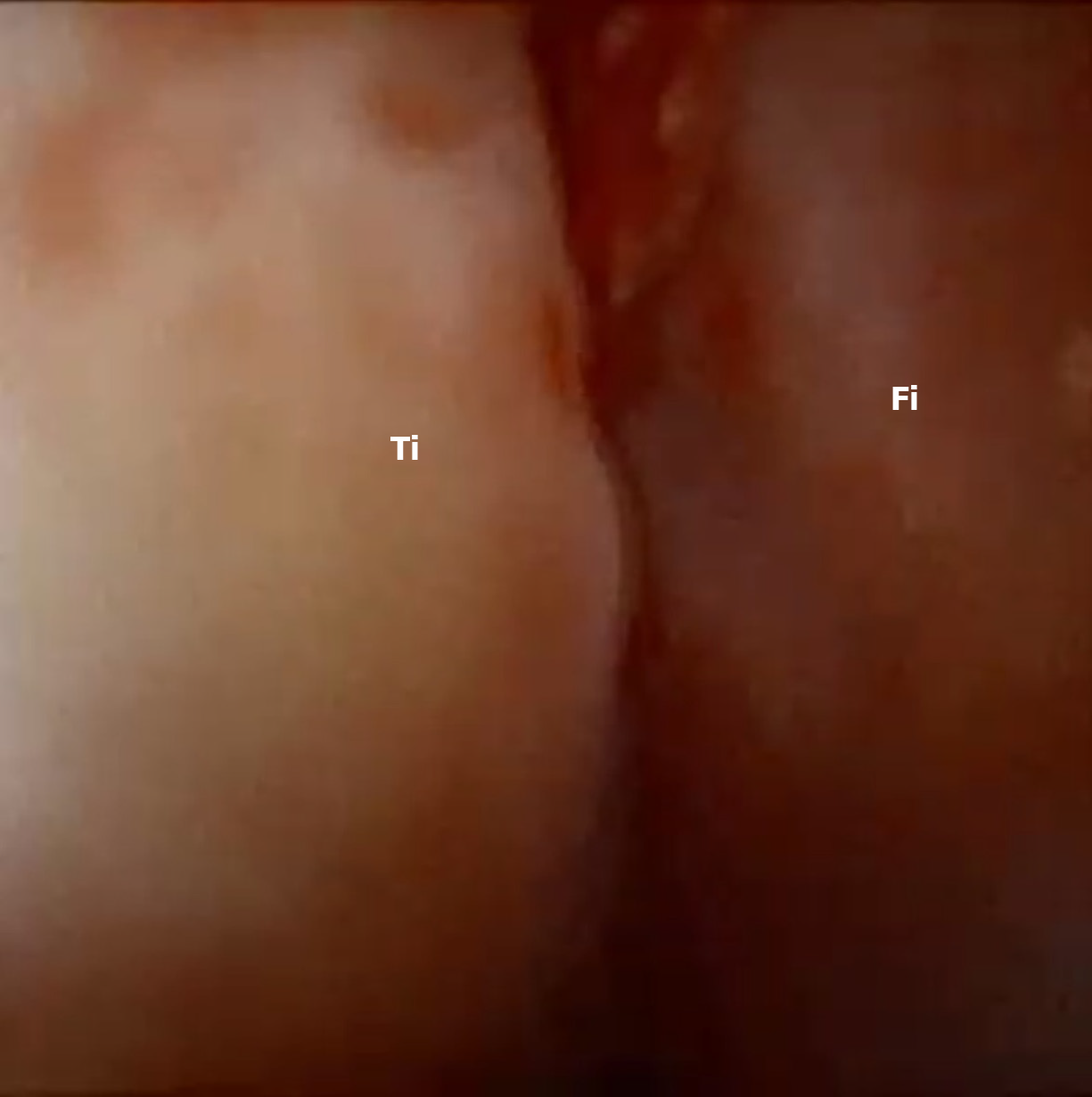
Nanoscopy of the ankle joint was performed with NanoScope (Arthrex, Naples, FL, United States). The injury and hypermobility of the syndesmosis were visualized (Figure 3). Under nanoscopic control, the tibiofibular syndesmosis was reduced and stabilized using a suture button (TightRope, Arthrex, Naples, FL, United States) (Figure 4). The medial malleolus was then fixed using two screws (Arthrex, Naples, FL, United States) (Figure 5).
Follow-up visits were conducted at 2, 6, 10, 16, 22, and 26 weeks post-procedure. Initially, the patient was non-weight-bearing on the involved limb for six weeks and used a CAM-Walker brace (DonJoy, Vista, CA, United States). After six weeks, the pain-Visual Analog Scale (VAS) score was 5, with a range of motion of 10 degrees of plantar flexion and 0 degrees of dorsiflexion. The Ankle-Hindfoot score (AOFAS) was 49. The patient then underwent a standard rehabilitation protocol focusing on reducing swelling and increasing the range of motion. After 16 weeks, there was an improvement in the range of motion: Dorsiflexion was 15 degrees, plantar flexion was 45 degrees, and the pain VAS score was reduced to 3. The patient started returning to a more active lifestyle, with an AOFAS score of 85. At 26 weeks post-procedure, the patient achieved a full range of motion and was pain-free, with a VAS score of 0 and an AOFAS score of 95, with only minor limitations during recreational activities and on uneven terrain, thus completing the orthopedic treatment.
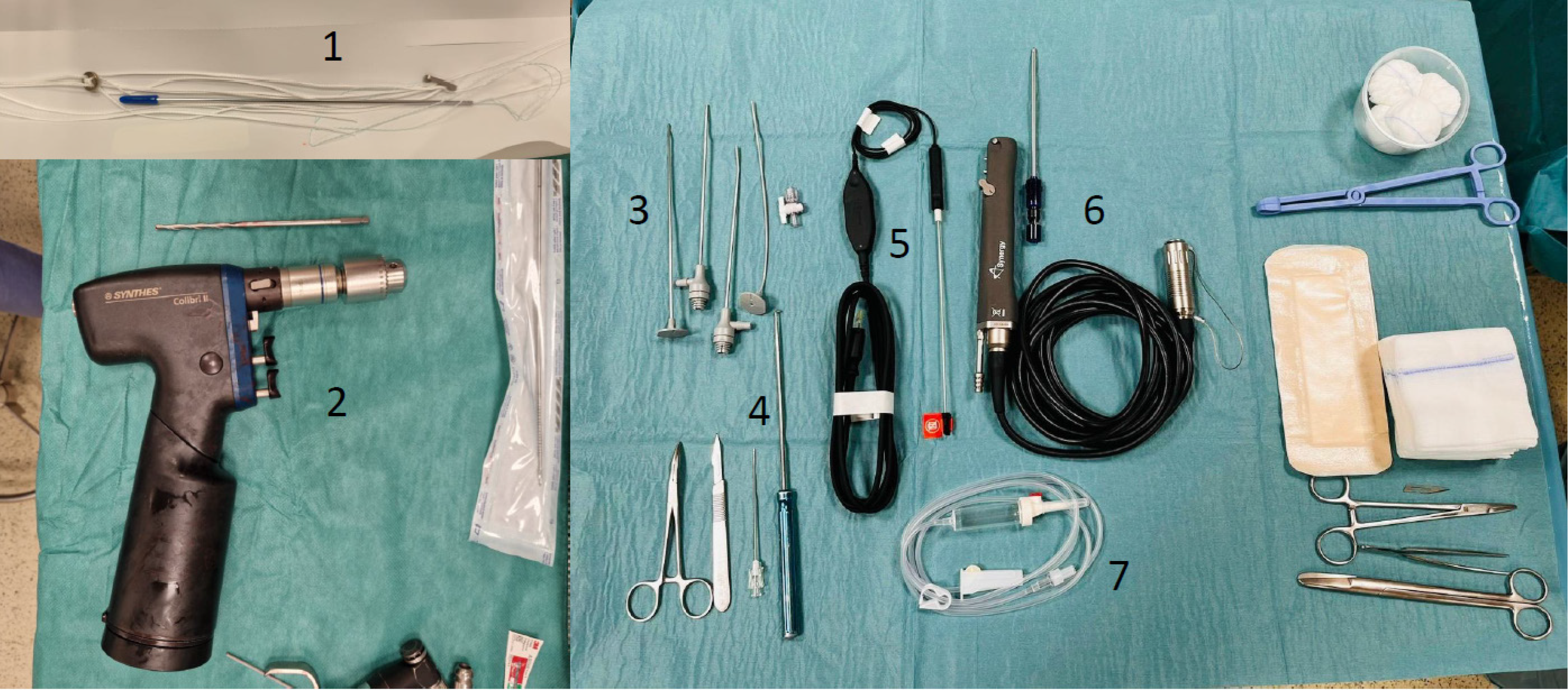
Nanoscopy is a video system comprising a handheld device with an integrated light source, packaged in a single-use kit, and connected to a 13-inch portable console. The handheld device, with a diameter of 1.9 mm, houses a light-emitting diode (LED) light and features image and video recording capabilities. It is inserted into a trocar with a diameter of 2.4 mm, connected to water, which significantly reduces the invasive area by 84% compared to a traditional arthroscope. The Nano needle scope tip offers a non-tilted viewing angle of 120°. Additionally, the needle arthroscope comes in three length variants: 125 mm, 180 mm, and 250 mm. The overall characteristics of the nanoscope are comparable to those of standard arthroscopes used in procedures. A dedicated shaver with a diameter of 2.8 mm is also available for nanoscopy (Figure 6).
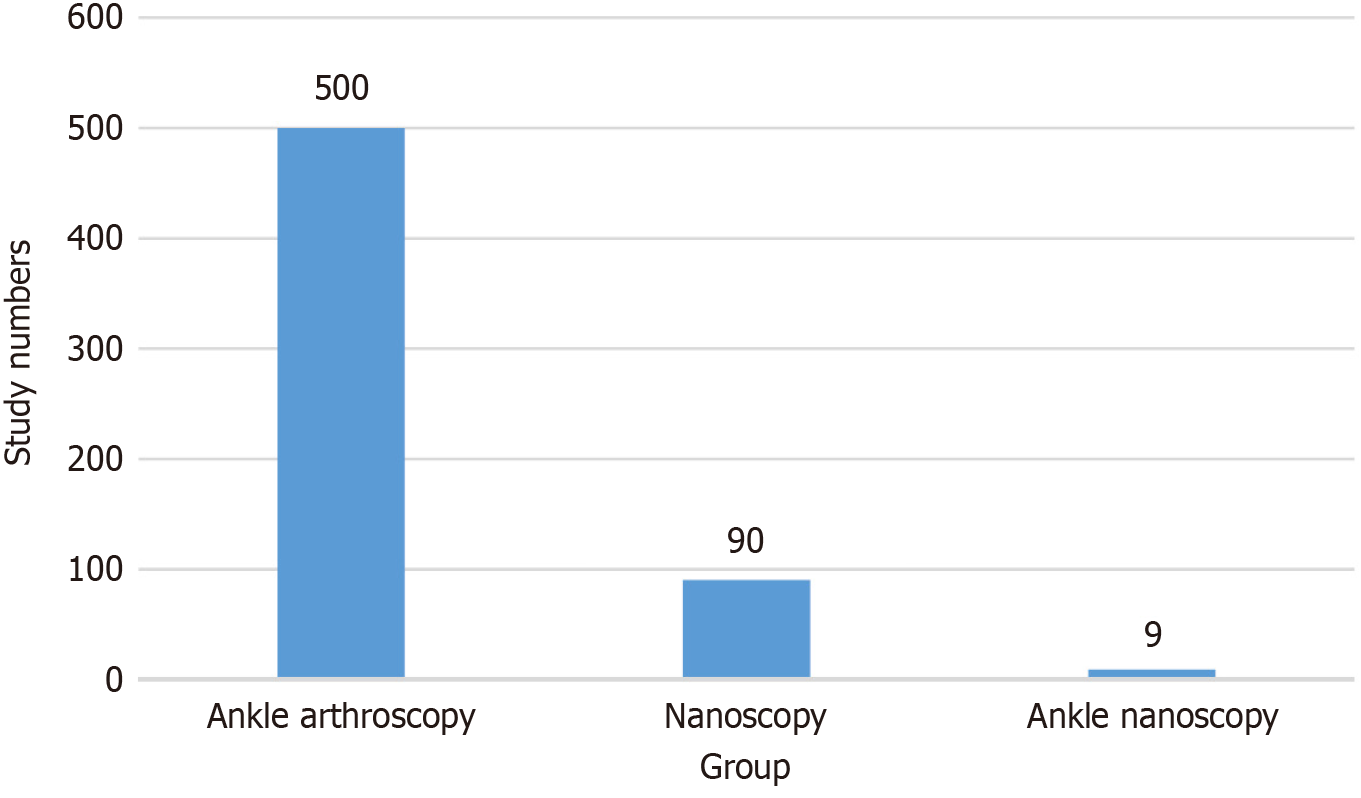
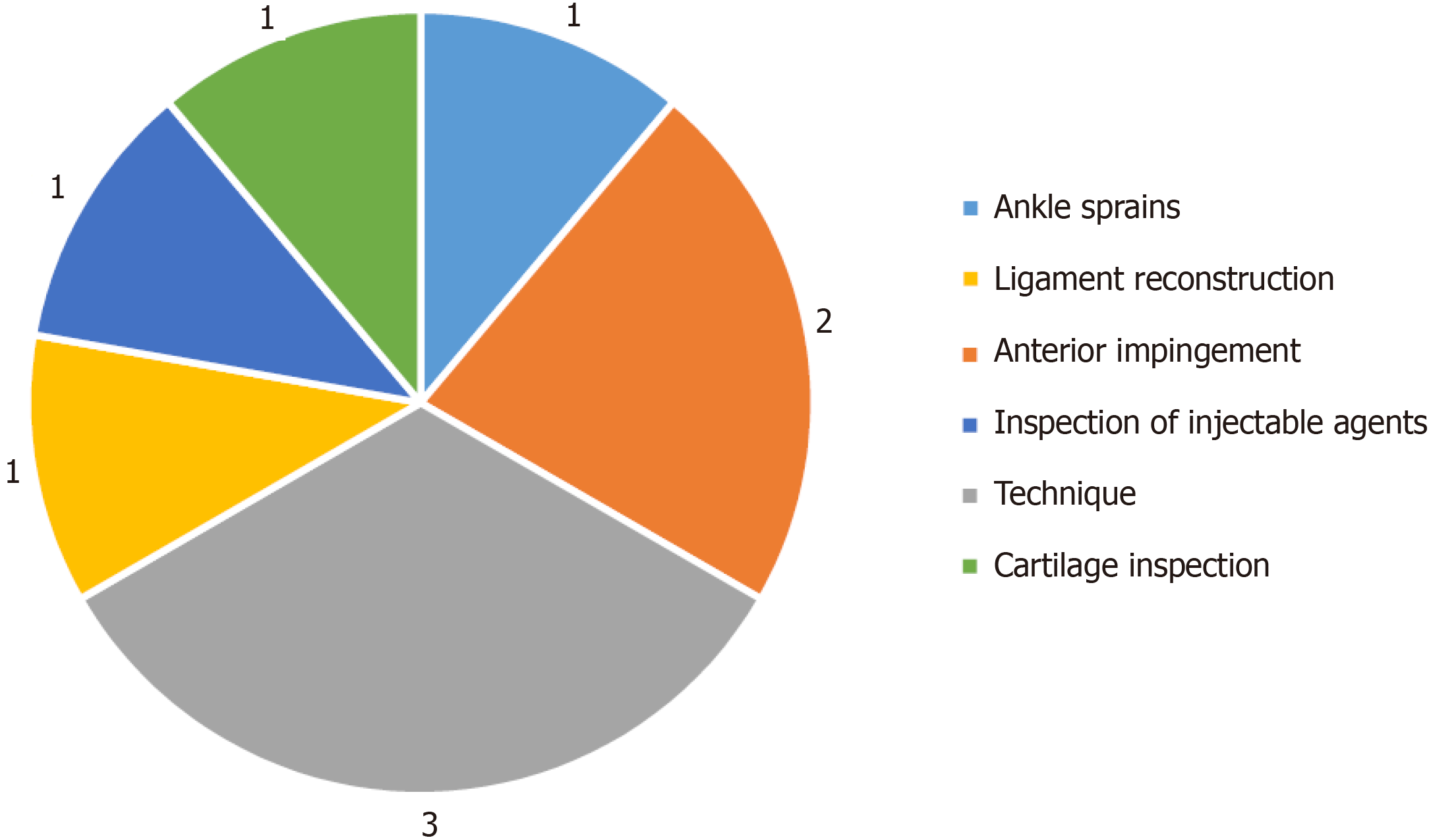
Over the past 25 years, around 500 studies have been conducted on ankle joint arthroscopy. In the same period, approximately 90 studies have focused on needle arthroscopy, with 9 of these specifically addressing ankle joint nanoscopy (Figure 7). These studies cover various topics, including: Ankle sprain (1 study)[9], anterior impingement of the ankle joint (2 studies)[10,11], technique of needle arthroscopy (3 studies)[12-14], ligament reconstruction (1 study)[8], inspection of injectable agents (1 study)[15], and cartilage inspection (1 study)[16] (Figure 8).
The findings suggest that needle arthroscopy could be a promising tool for treating ankle joints. In a 2024 study, Walinga et al[16] demonstrated that needle arthroscopy facilitates visualization of the tibiofibular syndesmosis and the surrounding cartilage. Additionally, this procedure can be performed with minimal pain under local anesthesia[17]. Colasanti et al[11] research indicates that patients are highly interested in the procedure and find the experience of watching the camera feed to be positive.
Over the past decade, several reviews and meta-analyses have addressed the fixation of lower leg fractures using arthroscopy. However, none of these studies have focused on needle arthroscopy. Recent research consistently suggests improved postoperative outcomes in patients undergoing arthroscopy-guided malleoli osteosynthesis.
In his 2016 study, Chan and Liu[17] emphasized the utility of ankle arthroscopy in visualizing the intricacies of acute ankle injuries. By directly visualizing the joint, arthroscopy aids in identifying and evaluating intra-articular fractures, tibiofibular syndesmosis injuries, associated osteochondral injury, and ligament injuries.
Liu et al[18] in a 2020 study, argued that fracture reduction through arthroscopy yields superior short-term results, although this advantage may diminish over the medium term.
Smith et al[19] in a 2020 study, demonstrated that ankle arthroscopy during open reduction and internal fixation significantly enhances patient outcomes for Weber B fibular fractures and ankle dislocations, without increasing complication rates. Despite extending the procedure by an average of 10 minutes, arthroscopy led to statistically significant improvements.
In a 2021 study, Aziz et al[20] illustrated that ankle arthroscopy serves as a crucial diagnostic and prognostic tool, effectively managing acute intra-articular injuries without substantial cost increases or serious adverse events.
However, Lee et al’s review underscores the need for further investigation into complications, additional costs, and procedural duration[21]. Similarly, Williams et al[22] in 2021, advocates for more research on the potential benefits of integrating ankle arthroscopy into the treatment of the ankle fractures before considering its routine application in all cases.
These conclusions are not surprising, given that over the last 25 years, only three randomized controlled trials have been conducted, involving a total of 159 patients, which examined the impact of arthroscopic intervention in lower leg ankle fractures on patient recovery time, healing duration, and accurate diagnosis of additional ankle joint injuries[23-25].
The presented case report validates the practical application of the mentioned conclusions. In essence, the needle arthroscope in this study offered ergonomic advantages, a smaller diameter, and flexible optics, potentially reducing the risk of iatrogenic injury. However, its limitations included the absence of camera tilt and lower resolution. Needle arthroscopy is positioned as an alternative to magnetic resonanse imaging and diagnostic arthroscopy. Assessing the tibiofibular syndesmosis was notably easier compared to traditional arthroscopy. Moreover, ergonomics play a significant role in ankle arthroscopy. The smaller size of the needle arthroscope facilitates ease of use, but achieving three-plane stabilization becomes more challenging, particularly for surgeons accustomed to standard arthroscopy. A nanoscope takes up much less space than a full arthroscopic tower and is portable, so using it during a procedure takes less time and it can always be ready. Additionally, mastering the use of a nanoscope requires additional time, thereby increasing the learning curve.
Ankle joint nanoscopy, characterized by its minimally invasive nature, emerges as a valuable diagnostic and therapeutic option for chronic and acute ankle injuries. Offering imaging and interventional capabilities within the ankle joint, it presents several advantages over conventional arthroscopy. Nonetheless, it is crucial not to view the needle arthroscope merely as a miniature version of traditional arthroscopy. Rather, it represents a novel tool, necessitating a reevaluation and delineation of innovative procedures tailored to maximize its utility and advantages.
| 1. | McCollum GA, van den Bekerom MP, Kerkhoffs GM, Calder JD, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21:1328-1337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 103] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Du Plessis GN, Griesel LD, Lourens D, Grabe RP. Incidence of syndesmotic injuries in all different types of ankle fractures. SA orthop J. 2008;7:28-33. |
| 3. | Vosseller JT, Karl JW, Greisberg JK. Incidence of syndesmotic injury. Orthopedics. 2014;37:e226-e229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Hughes JL, Weber H, Willenegger H, Kuner EH. Evaluation of ankle fractures: non-operative and operative treatment. Clin Orthop Relat Res. 1979;111-119. [PubMed] |
| 5. | Renstrom PA. Persistently Painful Sprained Ankle. J Am Acad Orthop Surg. 1994;2:270-280. [PubMed] [DOI] [Full Text] |
| 6. | Stone JW. Osteochondral Lesions of the Talar Dome. J Am Acad Orthop Surg. 1996;4:63-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 64] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Ferkel RD, Orwin JF. Ankle Arthroscopy: A new tool for treating acute and chronic ankle fractures. Arthroscopy. 1993;9:352-353. [DOI] [Full Text] |
| 8. | Lopes R, Noailles T, Padiolleau G, Bouguennec N, Vieira TD. Needle arthroscopy in anatomical reconstruction of the lateral ankle: a report of three cases with a parallel comparison to the standard arthroscopy procedure. J Exp Orthop. 2022;9:75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Butler JJ, Brash AI, Azam MT, DeClouette B, Kennedy JG. The Role of Needle Arthroscopy in the Assessment and Treatment of Ankle Sprains. Foot Ankle Clin. 2023;28:345-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 10. | Colasanti CA, Mercer NP, Garcia JV, Kerkhoffs GMMJ, Kennedy JG. In-Office Needle Arthroscopy for the Treatment of Anterior Ankle Impingement Yields High Patient Satisfaction With High Rates of Return to Work and Sport. Arthroscopy. 2022;38:1302-1311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 40] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 11. | Colasanti CA, Kaplan DJ, Chen JS, Kanakamedala A, Dankert JF, Hurley ET, Mercer NP, Stone JW, Kennedy JG. In-Office Needle Arthroscopy for Anterior Ankle Impingement. Arthrosc Tech. 2022;11:e327-e331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 12. | Stornebrink T, Walinga AB, Stufkens SAS, Kerkhoffs GMMJ. Wide-Awake Needle Arthroscopy of the Anterior Ankle: A Standardized Approach. Arthrosc Tech. 2024;13:102901. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Inoue J, Yasui Y, Sasahara J, Takenaga T, Ha M, Miyamoto W, Kawano H, Murakami H, Yoshida M. Comparison of visibility in needle arthroscopy of the ankle according to surgical experience: A cadaveric study. Foot Ankle Surg. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 14. | Duenes ML, Azam MT, Butler JJ, Weiss MB, Kennedy JG. In-Office Needle Arthroscopy for the Foot and Ankle. Arthroscopy. 2023;39:1129-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Stornebrink T, Stufkens SAS, Mercer NP, Kennedy JG, Kerkhoffs GMMJ. Can bedside needle arthroscopy of the ankle be an accurate option for intra-articular delivery of injectable agents? World J Orthop. 2022;13:78-86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Walinga AB, Dahmen J, Stornebrink T, Emanuel KS, Kerkhoffs GMMJ. Fifteen out of 16 elite athletes showed concomitant low-grade cartilage lesions of the ankle with unstable syndesmotic injuries: concerns from a prospective case series. BMJ Open Sport Exerc Med. 2024;10:e001879. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 17. | Chan KB, Lui TH. Role of Ankle Arthroscopy in Management of Acute Ankle Fracture. Arthroscopy. 2016;32:2373-2380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Liu C, You JX, Yang J, Zhu HF, Yu HJ, Fan SW, Li HY. Arthroscopy-Assisted Reduction in the Management of Isolated Medial Malleolar Fracture. Arthroscopy. 2020;36:1714-1721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Smith KS, Drexelius K, Challa S, Moon DK, Metzl JA, Hunt KJ. Outcomes Following Ankle Fracture Fixation With or Without Ankle Arthroscopy. Foot Ankle Orthop. 2020;5:2473011420904046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Aziz H, Amirian A, Dabash S, Dunn WR, Bloome D. Ankle Arthroscopy as an Adjunct to the Management of Ankle Fractures. Foot Ankle Orthop. 2021;6:24730114211002165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 21. | Lee KM, Ahmed S, Park MS, Sung KH, Lee SY, Koo S. Effectiveness of arthroscopically assisted surgery for ankle fractures: A meta-analysis. Injury. 2017;48:2318-2322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Williams CE, Joo P, Oh I, Miller C, Kwon JY. Arthroscopically Assisted Internal Fixation of Foot and Ankle Fractures: A Systematic Review. Foot Ankle Orthop. 2021;6:2473011420950214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 23. | Ge T, Chen M, Zheng MQ, Wang XL, Wang JW, Zhang GM. Preliminary effect of posterolateral ankle arthroscopy for ankle fractures in elderly patients. Int J Clin Exp Med. 2017;10:9740-9745. |
| 24. | Takao M, Ochi M, Oae K, Naito K, Uchio Y. Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br. 2003;85:324-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 188] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 25. | Thordarson DB, Bains R, Shepherd LE. The role of ankle arthroscopy on the surgical management of ankle fractures. Foot Ankle Int. 2001;22:123-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 65] [Article Influence: 2.7] [Reference Citation Analysis (0)] |