Published online Aug 18, 2024. doi: 10.5312/wjo.v15.i8.796
Revised: June 23, 2024
Accepted: July 19, 2024
Published online: August 18, 2024
Processing time: 82 Days and 16.1 Hours
Among the most frequent hip fractures are trochanteric fractures, which usually occur from low-energy trauma like minor falls, especially in older people with osteoporotic bones.
To evaluate the treatment efficacy of dynamic condylar screws (DCS) and proximal femoral nails (PFN) for unstable intertrochanteric fractures.
To find pertinent randomized controlled trials and retrospective observational studies comparing PFN with DCS for the management of unstable femoral inter
This study included six articles, comprising a total of 173 patients. Compared to the DCS, the PFN had a shorter operation time [mean difference (MD): -41.7 min, 95% confidence interval (95%CI): -63.04 to -20.35, P = 0.0001], higher success rates with closed reduction techniques [risk ratio (RR): 34.05, 95%CI: 11.12-104.31, P < 0.00001], and required less intraoperative blood transfusion (MD:
Compared to DCS, PFN offers shorter operative times, reduces the blood transfusions requirements, achieves higher closed reduction success, enables faster fracture healing, and lowers reoperation incidence.
Core Tip: The management of unstable intertrochanteric fractures frequently utilizes both proximal femoral nails and dynamic condylar screws. This meta-analysis critically examined the effectiveness thereof, aiming to identify the superior treatment option. These findings are pivotal to refine surgical strategies, ultimately aiming to improve patient outcomes in managing these challenging orthopedic injuries.
- Citation: Yousif Mohamed AM, Salih M, Abdulgadir M, Abbas AE, Lutfi Turjuman D. Comparative efficacy of proximal femoral nail vs dynamic condylar screw in treating unstable intertrochanteric fractures. World J Orthop 2024; 15(8): 796-806
- URL: https://www.wjgnet.com/2218-5836/full/v15/i8/796.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i8.796
One of the most frequent hip fractures, especially in older people with osteoporotic bones, is the trochanteric fracture, which usually results from low-energy trauma such as simple falls[1]. Fractures in the proximal femur area that run from the extracapsular basilar neck to the lesser trochanter and proximal to the medullary canal are referred to as trochanteric fractures[2]. This type of fracture is prevalent among elderly individuals[3], a trend which is likely influenced by in
Unstable fracture patterns involve fracture lines extending into the subtrochanteric area, lateral wall blowout, com
Trochanteric fractures, regardless of their geometric configuration, typically undergo operative intervention unless there are present contraindications, such as severe comorbidities posing risks during the intraoperative or perioperative period. However, managing unstable trochanteric fracture patterns presents a significant challenge, often resulting in high postoperative complication rates, including mortality.
Modern treatment options include intramedullary fixation techniques like cephalomedullary nails and intramedullary hip screws, as well as extramedullary techniques like dynamic hip screw (DHS), compression hip screw, dynamic cond
According to several studies, extramedullary devices are less effective than intramedullary devices in treating unstable trochanteric femur fractures. The use of extramedullary fixation techniques should be performed with caution because of the increased risk of complications and lower functional results.
For stable trochanteric fractures, the most recent study by the American Academy of Orthopedic Surgeons[7] suggests DHS. For AO/OTA 31-A3 fractures, the DCS system featuring a 95° lag screw has been the commonly preferred trea
This study aimed to perform a comprehensive evaluation of available treatment options for unstable intertrochanteric fractures, specifically comparing the efficacy of PFN vs DCS in managing such fractures. A comprehensive evaluation of clinical outcomes, such as surgical time, type of reduction, need for blood transfusions, length of hospitalization, rates of postoperative infection, complications related to implants, and rates of reoperation, were the aims of this study. We hypothesized that PFN would show better results than DCS in the treatment of unstable intertrochanteric fractures.
The protocol was registered using regular reporting methods[12] and assigned PROSPERO number CRD42024537426.
This study conducted a meta-analysis using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline. The Google database, PubMed, EMBASE, Scopus, Cochrane Library, and Web of Science were all searched without regard to location or type of publication. The following Medical Subject Heading (MeSH) keywords and their combinations were used in the search: (((“Femoral Fractures”[MeSH]) OR (“Hip Fractures”[MeSH])) OR ((((((((((in
This search was modified to contain publications spanning from 1 January 1996 to 5 April 2024. There were no other filters used in this search. The year 1996 was chosen because the PFN evolved during this time[11].
This study looked for relevant studies involving adult humans in the reference lists of related reviews and original articles. Every language was considered. Since the data for this meta-analysis was gathered from published articles, ethical approval was not required for this study (Supplementary material).
Using the Population, Intervention, Comparator and Outcomes paradigm, two authors independently screened each title and abstract. The populations were people with unstable intertrochanteric fractures; the intervention was fixation with a PFN; the comparison was fixation with a DCS; the outcomes included operation time, reduction type, blood transfusion, length of hospital stay, fracture consolidation, implant-related complications, reoperation, and infection rates.
All studies, both prospective randomized controlled trials (RCTs) and retrospective, which compared the efficacy of PFN and DCS in managing intertrochanteric fractures among patients aged 18 years and above, with fractures cate
Data selection for this study was carried out independently by two authors. Initially, titles of articles were manually sc
Two authors (AMYM and DLT), independently extracted data from the eligible studies using pre-prepared data extra
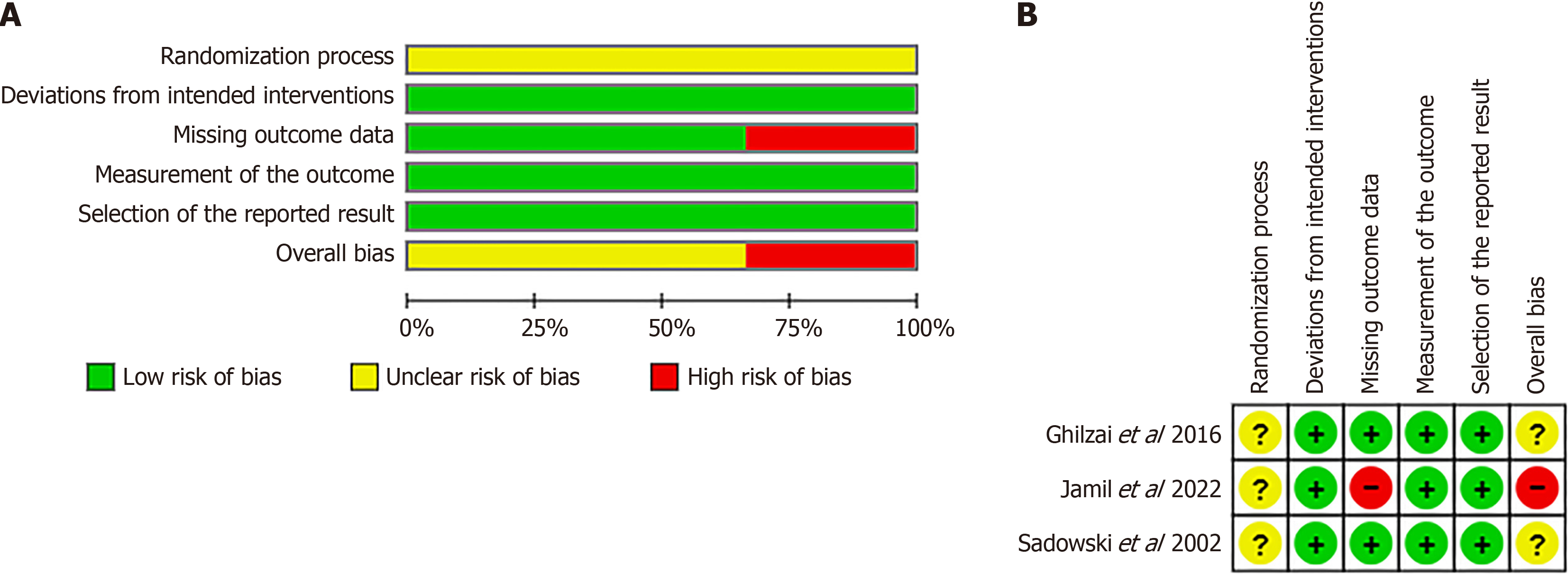
This study used the revised Cochrane risk-of-bias tool for randomized trials (ROB-2)[13] to assess the quality of RCTs[14-16] and the Newcastle–Ottawa Scale[17] to assess the quality of observational studies[18-20]. The overall assessment of ROB-2 showed that Ghilzai et al[15] and Sadowski et al[16] were of some concern, while Jamil et al[14] was of high co
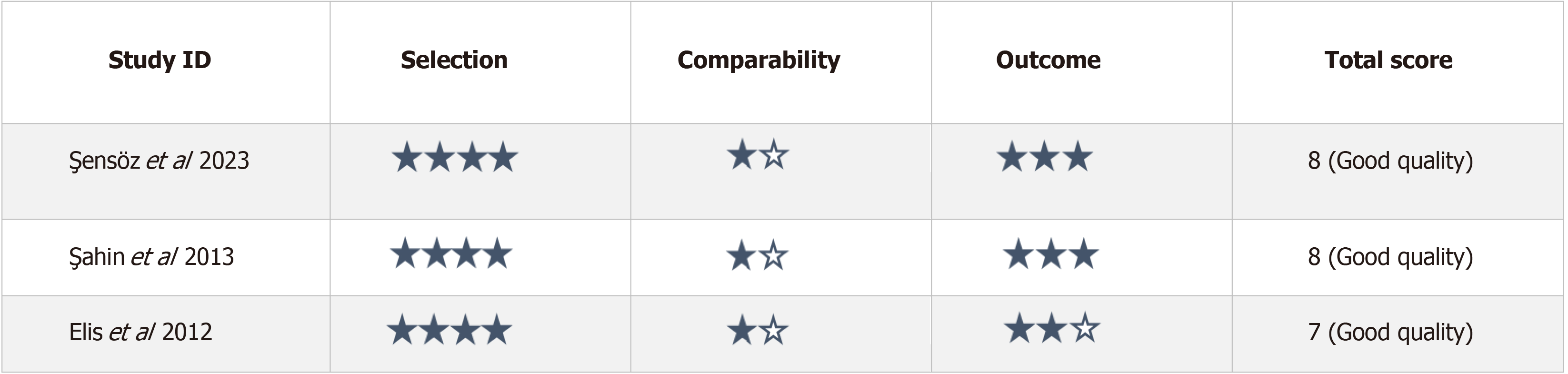
The evaluation of quality for the observational studies, as presented in Figure 3, indicated that they were of high quality. Specifically, two studies achieved a score of 8[18,19], while Elis et al[20] received a score of 7. Across all studies, there was a loss of a quality point in the Comparability domain, with Elis et al[20] experiencing an additional deduction in the adequacy of follow-up domain.
The stated outcome measures’ mean, SD, and range were noted. In cases where SD was not provided, it was calculated using the range[21].
The Comprehensive Meta-Analysis program was used to conduct the meta-analysis. A random-effects model was used for pooling as half of the studies used a retrospective cohort design. The effect sizes were represented as MD or risk ratio (RR), with their corresponding 95% confidence intervals (95%CI) based on the measurement scale (continuous[22] and binary[23]) outcomes, respectively. P < 0.05, I² > 50% was defined as high heterogeneity; and P ≥ 0.05, I² < 50% was defined as moderate heterogeneity. P = 0.05 was used as the statistical significance criterion.
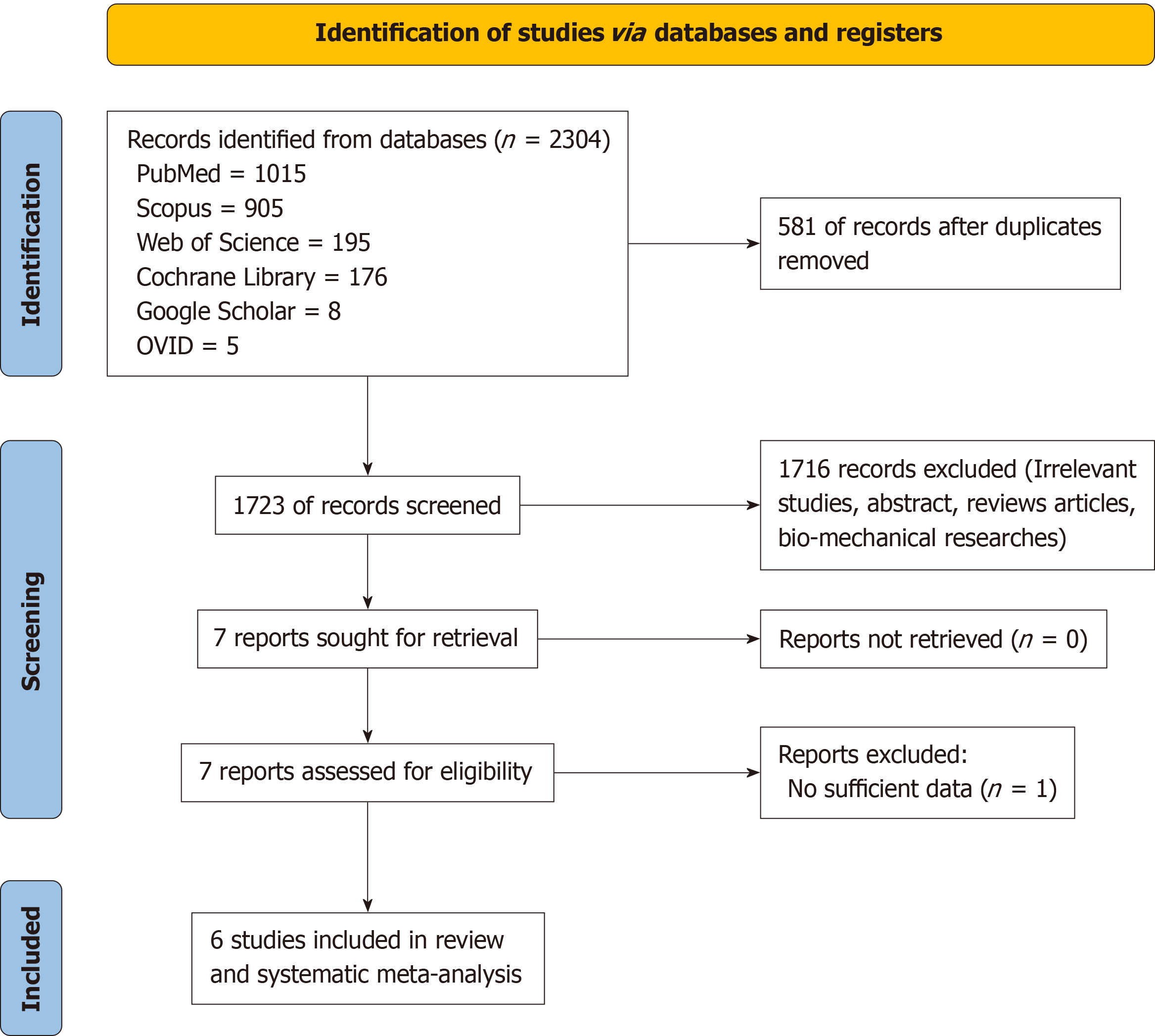
A thorough computerized search used many databases and yielded a total of 2304 items. Prominent sources including PubMed (n = 1015), Scopus (n = 905), Web of Science (n = 195), Cochrane Library (n = 176), Google Scholar (n = 8), and OVID (n = 5) were included in this search. Following the initial screening phase, which involved the removal of articles based on titles and the elimination of duplicates, 1723 articles remained for further evaluation. Subsequently, after scrutinizing the abstracts, 1716 articles were excluded, with one additional article being discarded due to insufficient data, focusing solely on one outcome measure. Following this rigorous screening process, a total of six studies[15-20] met the inclusion criteria for conducting a meta-analysis. The details of the selection method are summarized in a flow chart (Figure 1).
A total of six studies, which compared the use of PFN with DHS with patients with unstable trochanteric fractures, were included in this review. Among the studies identified, there were three randomized controlled trials[15-17] involving a total of 173 patients. Within this subgroup, 97 patients were assigned to the PFN group and 76 to the DCS group. Addi
All studies were conducted between 2002 and 2023. All included studies were conducted in various countries, except for Şensöz et al[18] and Sahin et al[19], both of which were conducted in Türkiye. Although all studies utilized plate fi
| Ref. | Study type | Center | Study period | Follow-up in mo | Number of patients | Average age in yr | Sex as male/female | Fracture type and n | Conclusion | |||
| PFN | DCS | PFN | DCS | PFN | DCS | |||||||
| Şensöz et al[18], 2023 | Retrospective cohort | Dr. Lutfi Kirdar Kartal City Hospital, Istanbul, Turky | Between 2013 and 2018 | At least 2 yr | 36 | 25 | 65.52 | 59.36 | 15/21 | 13/12 | A2.3 61 | DCS was superior to PFN in early fracture union time. However, it showed a higher nonunion rate. PFN showed shorter hospital stay time than DCS and is recommended to be applied in that fracture type |
| Jamil et al[14], 2022 | RCT | Jawaharlal Nehru Medical College and Hospital, Aligarh Muslim University, Aligarh, India | Between November 2019 to December 2021 | NA | 15 | 11 | 54.20 | 59.82 | 4/11 | 6/5 | A2.2 16/A2.3 10 | PFN showed better results than DCS regarding operative time, union rate, duration for fracture union, and rate of complications |
| Ghilzai et al[15], 2016 | RCT | Liaquat National Hospital, Karachi, Pakistan | February 2012 to August 2013 | NA | 21 | 19 | 80.00 | 77.00 | NA | NA | A2.2 21/A2.3 19 | PFN is superior to DCS in the treatment of proximal femur fractures type 31A3 |
| Sahin et al[19], 2014 | Retrospective cohort | Izmir Tepecik Education and Research Hospital, Izmir, Türkiye | Between January 2007 and December 2010 | At least 1 yr | 42 | 37 | 51.75 | 57.50 | 17/25 | 18/19 | A2.2 44/A2.3 35 | PFN is superior to DCS in the treatment of unstable peritrochanteric fractures, owing to its effect in reducing operative blood loss, and biological fixation achievement |
| Elis et al[20], 2012 | Retrospective cohort | Tel Aviv Sourasky Medical Center, Tel Aviv, Israel | Between January 2006 and July 2009 | At least 1 yr | 19 | 14 | 51.75 | 57.50 | 3/16 | 3/11 | A2.2 19/A2.3 14 | EPFN was as effective as DCS devices for the treatment of reverse oblique hip fractures |
| Sadowski et al[16], 2002 | RCT | University Hospital of Geneva, Geneva, Switzerland | Between March 1998 and June 1999 | At least 1 yr | 20 | 19 | 88.00 | 77.00 | 7/13 | 4/14 | A2.2 20/A2.3 19 | The results support the use of PFN rather than DCS for the treatment of reverse oblique and transverse intertrochanteric fractures |
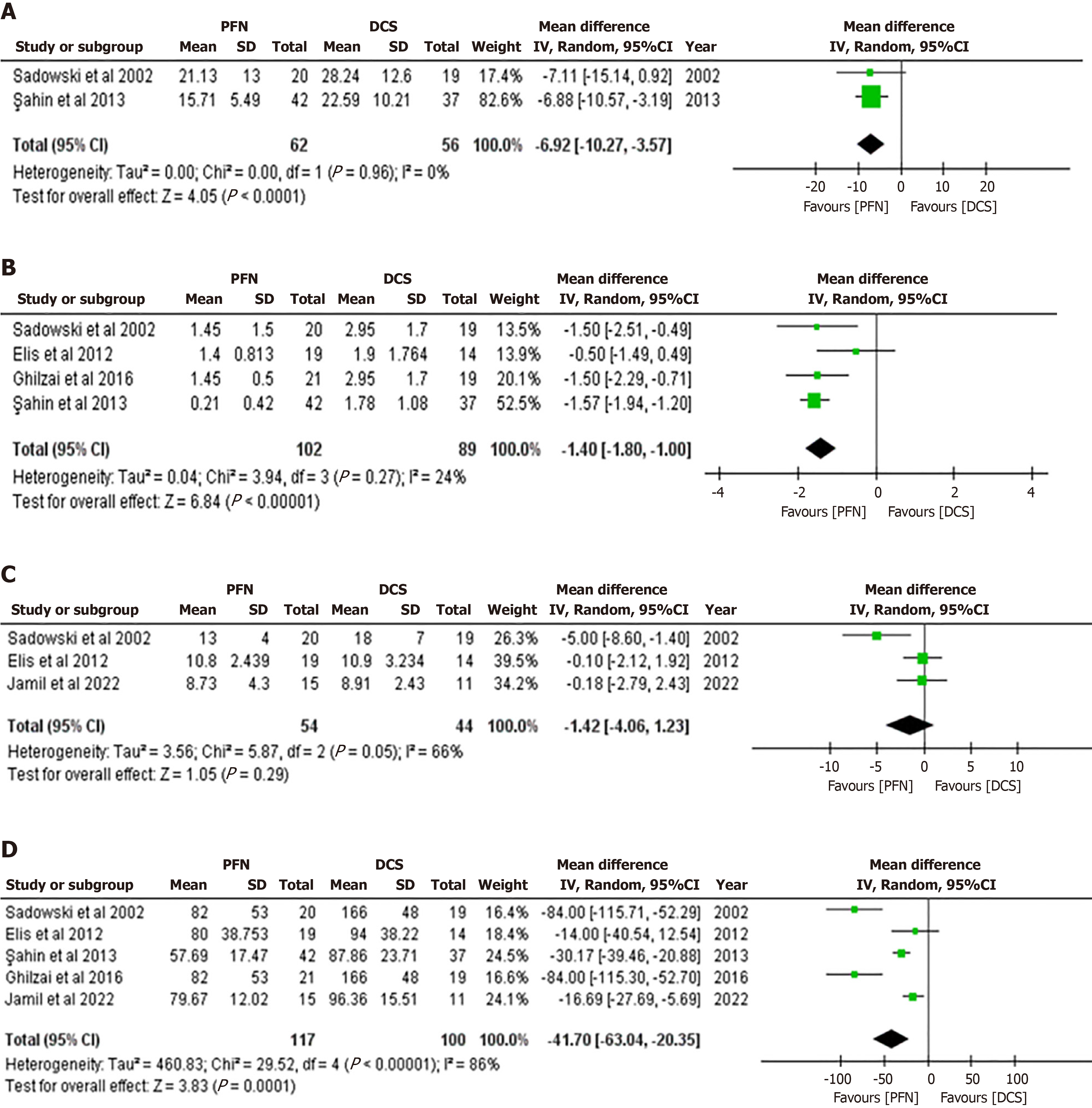
Fracture union time, a pivotal endpoint in assessing surgical outcomes, was meticulously evaluated by only two studies: Sadowski et al[16] and Sahin et al[19]. The results showed that the PFN group had significantly reduced fracture union time more than the DCS group and the results showed heterogeneity (MD: -6.92, 95%CI: -10.27 to -3.57, P < 0.0001; I2 = 0%, P = 0.96) (Figure 4A). Moreover, the impact of surgical intervention on blood transfusion requirements, a critical consideration in orthopedic procedures, was rigorously examined across four studies[16,17,19,20]. The pooled analysis favored the PFN group over the DCS group, revealing a significant difference in favor of PFN, albeit with low heterogeneity (MD: -1.40, 95%CI: -1.80 to -1.00, P < 0.00001; I2 = 24%, P = 0.27) (Figure 4B). Furthermore, hospital stay duration, a crucial indicator of postoperative recovery, was meticulously documented in three studies[15,17,20]. There was no significant distinction between the groups, according to the analysis (MD: -1.42, 95%CI: -4.06-1.23, P = 0.29), with high heterogeneity noted (I2 = 66%, P = 0.05) (Figure 4C).
All studies, except for Şensöz et al[18], provided comprehensive data on operation duration. The PFN group exhibited a significant reduction in operation time compared to the DCS group with the results indicating high heterogeneity (MD: -41.7, 95%CI: -63.04 to -20.35, P = 0.0001; I2 = 86%, P < 0.00001) (Figure 4D).
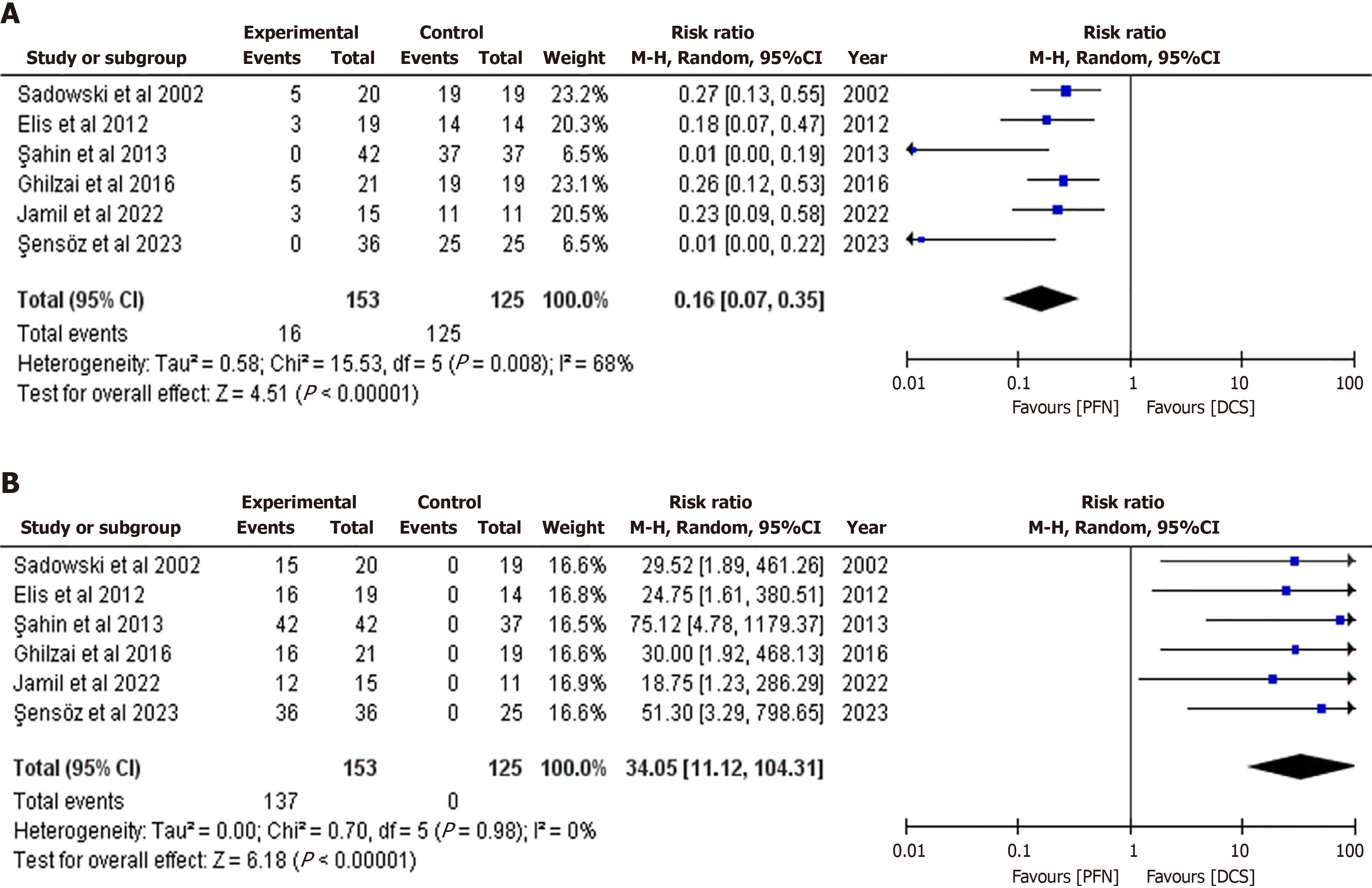
Interestingly, the type of reduction, a crucial aspect of surgical technique, was meticulously documented in all studies, except Sahin et al[19]. Specifically, open reduction was notably less prevalent in the PFN group than in the DCS group (RR: 0.16, 95%CI: 0.07 to 0.35, P < 0.00001), showcasing a trend toward a less invasive approach, with high heterogeneity noted among the studies (I2 = 68%, P = 0.008) (Figure 5A). Conversely, closed reduction, indicating a less invasive surgical technique, was substantially more frequent in the PFN group than in the DCS group (RR: 34.05, 95%CI: 11.12 to 104.31, P < 0.00001), highlighting a potential advantage of the PFN approach, with minimal/no heterogeneity observed (I2 = 0%, P = 0.980) (Figure 5B).
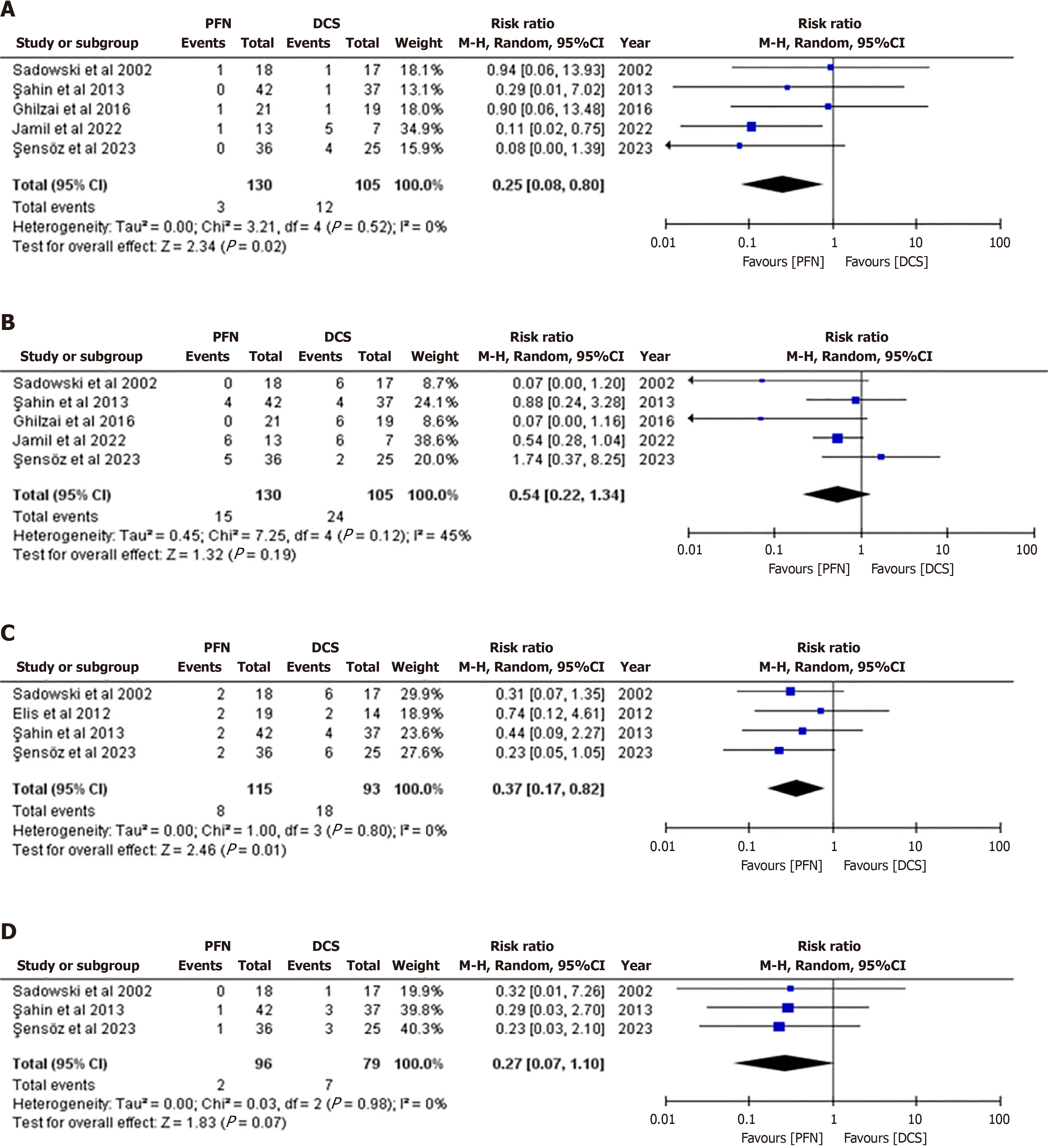
Notable variations in postoperative complications were observed between the PFN and DCS groups. PFN demonstrated notably lower rates of nonunion fractures compared to DCS, as evidenced by findings from five studies[15-19] (RR: 0.25, 95%CI: 0.08-0.80, P = 0.02). Notably, these results showed no heterogeneity across studies (I² = 0%, P = 0.52) (Figure 6A). However, while implant-related complications trended lower in the PFN group across all studies[15-20] (RR: 0.54, 95%CI: 0.22-1.34, P = 0.19), statistical significance was not attained, with moderate heterogeneity noted across studies (I² = 45%, P = 0.120) (Figure 6B).
Moreover, PFN demonstrated a significant reduction in reoperation rates compared to DCS, with findings consistent across four studies[17-20] (RR: 0.37, 95%CI: 0.17-0.82, P = 0.01; I2 = 0%, P = 0.80) (Figure 6C). Furthermore, infection rates were lower in the PFN group across three studies[18-20] (RR: 0.27, 95%CI: 0.07-1.10, P = 0.07), although statistical sig
An increased risk of osteoporotic intertrochanteric fractures is seen in elderly people. Hip joint functional exercises in conjunction with prompt surgery for these fractures may reduce complications, including pressure ulcers, deep vein thrombosis, and stiffness in the joints[24]. Because the PFN has a smaller distal shaft diameter and less concentrated stress at the tip, it is useful in preventing femoral shaft fractures. Surgeons can reduce surgical trauma, blood loss, infection, and wound complications by using intramedullary fixation to minimize soft tissue dissection[25,26].
Technical benefits of the DCS include stability in the sagittal plane[19]. However, significant disadvantages of the DCS include the possibility of devascularization of fracture fragments as a result of thorough dissection, which may result in infection, nonunion, or delayed union[27,28].
The findings suggest that the PFN offers several intraoperative advantages compared to the DCS. Specifically, PFN was linked to a notably shorter operation time and a greater success rate in closed reduction techniques, indicating a less invasive procedure. This is crucial because less invasive methods are generally associated with quicker recovery periods and shorter hospital stays. To protect the fracture hematoma, which is essential to the healing process, closed reduction entails aligning the ends of a fracture by manipulating its fragments without surgically exposing the surrounding tissues[29]. This study found that the rate of successful closed reductions was significantly higher in the PFN group than in the DCS group.
On the other hand, the length of hospital stay did not significantly differ between the two groups in this study. Addi
The shorter operating duration highlights PFN’s effectiveness in treating these fractures surgically, which may be because of the smaller incision and reduced muscle damage. While DCS necessitates a wider incision, PFN implants are generally placed using a minimally invasive procedure without accessing the fracture site[30].
PFN also appears to outperform DCS regarding certain postoperative outcomes. The data has revealed that PFN has a lower incidence of nonunion fractures and implant-related complications, though the latter did not reach statistical sig
However, it is essential to note that infection rates, while lower in the PFN group, did not show a statistically signi
A significant finding from this study is the reduced fracture union time observed with PFN. This outcome is especially important for older patients, as prolonged immobility can cause additional complications such deep vein thrombosis, pressure ulcers, and lung problems. PFN has been associated with a faster fracture union time, which may indicate a more effective healing process, allowing for earlier mobilization and a reduction in the total demand on healthcare resources.
This study had a number of advantages, and was the first meta-analysis to compare PFN with DCS. Moreover, the inclusion of solely comparative studies reduced the possibility of matching and operative bias. Furthermore, the selection procedure demonstrated a high degree of selectivity, which reduced the study’s heterogeneity and the possibility of bias.
However, the study also had some limitations. First, there were few comparable studies in the literature that could be included. Furthermore, this study was unable to conduct subgroup analyses to investigate possible sources of heterogeneity, because of the small number of included papers (three RCTs and three retrospective studies). Second, subgroup analysis is a valuable tool in meta-analysis to assess the consistency of findings across different study designs, popu
The results of this study show that PFN is a reliable implant that, when used in unstable intertrochanteric fractures, provides acceptable functional and radiological outcomes. Notably, PFN typically improves the healing process for fractures and minimizes the blood transfusions requirements and operating durations, as well as decreases the incidence of reoperation, and achieves higher closed reduction success.
The authors wish to thank Dr. Mohamed Mahmoud of Egypt, who performed the statistical analysis for this meta-analysis. His expertise and commitment significantly improved our research. Additionally, we thank Stephen Pinder, a native-speaking medical English specialist from the Department of Clinical Epidemiology and Biostatistics, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Thailand for English language review and editing.
| 1. | Dimon JH, Hughston JC. Unstable intertrochanteric fractures of the hip. J Bone Joint Surg Am. 1967;49:440-450. [PubMed] |
| 2. | Court-Brown CM, Heckman JD, McQueen M, Ricci W, Tornetta P III, McKee M. Rockwood and Green’s fractures in adults. 8th ed. Wolters Kluwer, 2015: 2075-2083. |
| 3. | Kumar GN, Sharma G, Khatri K, Farooque K, Lakhotia D, Sharma V, Meena S. Treatment of Unstable Intertrochanteric Fractureswith Proximal Femoral Nail Antirotation II: Our Experience in Indian Patients. Open Orthop J. 2015;9:456-459. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1996] [Cited by in RCA: 1941] [Article Influence: 58.8] [Reference Citation Analysis (0)] |
| 5. | Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1375] [Cited by in RCA: 1489] [Article Influence: 53.2] [Reference Citation Analysis (0)] |
| 6. | Schipper IB, Marti RK, van der Werken C. Unstable trochanteric femoral fractures: extramedullary or intramedullary fixation. Review of literature. Injury. 2004;35:142-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 103] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | American Academy of Orthopaedic Surgeons. Management of Hip Fractures in Older Adults EvidenceBased Clinical Practice Guideline. December 3, 2021. [cited 25 June 2024]. Available from: https://www.aaos.org/hipfxcpg. |
| 8. | Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am. 2001;83:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 219] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 9. | Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997;79:969-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 151] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Sanders R, Regazzoni P. Treatment of subtrochanteric femur fractures using the dynamic condylar screw. J Orthop Trauma. 1989;3:206-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 51] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Boldin C, Seibert FJ, Fankhauser F, Peicha G, Grechenig W, Szyszkowitz R. The proximal femoral nail (PFN)--a minimal invasive treatment of unstable proximal femoral fractures: a prospective study of 55 patients with a follow-up of 15 months. Acta Orthop Scand. 2003;74:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 110] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18665] [Cited by in RCA: 17544] [Article Influence: 1096.5] [Reference Citation Analysis (1)] |
| 13. | Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6581] [Cited by in RCA: 15288] [Article Influence: 2548.0] [Reference Citation Analysis (0)] |
| 14. | Jamil MF, Mohd J, Abbas M, Siddiqui YS, Khan MJ. A comparative study of Proximal Femoral Nail (PFN) versus Dynamic Condylar Screw (DCS) in management of unstable trochanteric fractures. Int J Burns Trauma. 2022;12:83-92. [PubMed] |
| 15. | Ghilzai AK, Idrees Z, Khan MA, Kazim M, Najjad R. Comparison of proximal femur nail and dynamic condylar screw in treating proximal femoral fractures. 6th Annual Research Day; 2015; Karachi, Pakistan. 2016; 32: 100-103. |
| 16. | Sadowski C, Lübbeke A, Saudan M, Riand N, Stern R, Hoffmeyer P. Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study. J Bone Joint Surg Am. 2002;84:372-381. [PubMed] |
| 17. | Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. [cited 20 June 2024]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. |
| 18. | Şensöz E, Ergun S, Kayaalp ME, Eceviz E. The Comparison of Dynamic Condylar Screw Plate to Proximal Femoral Nail in Reverse Oblique and Transverse Intertrochanteric Fractures: A Retrospective Study on 61 Patients. Cureus. 2023;15:e36397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Sahin EK, Imerci A, Kınık H, Karapınar L, Canbek U, Savran A. Comparison of proximal femoral nail antirotation (PFNA) with AO dynamic condylar screws (DCS) for the treatment for unstable peritrochanteric femoral fractures. Eur J Orthop Surg Traumatol. 2014;24:347-352. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Elis J, Chechik O, Maman E, Steinberg EL. Expandable proximal femoral nails versus 95° dynamic condylar screw-plates for the treatment of reverse oblique intertrochanteric fractures. Injury. 2012;43:1313-1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Walter SD, Yao X. Effect sizes can be calculated for studies reporting ranges for outcome variables in systematic reviews. J Clin Epidemiol. 2007;60:849-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 161] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 22. | Guyatt GH, Thorlund K, Oxman AD, Walter SD, Patrick D, Furukawa TA, Johnston BC, Karanicolas P, Akl EA, Vist G, Kunz R, Brozek J, Kupper LL, Martin SL, Meerpohl JJ, Alonso-Coello P, Christensen R, Schunemann HJ. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles-continuous outcomes. J Clin Epidemiol. 2013;66:173-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 525] [Article Influence: 40.4] [Reference Citation Analysis (0)] |
| 23. | Guyatt GH, Oxman AD, Santesso N, Helfand M, Vist G, Kunz R, Brozek J, Norris S, Meerpohl J, Djulbegovic B, Alonso-Coello P, Post PN, Busse JW, Glasziou P, Christensen R, Schünemann HJ. GRADE guidelines: 12. Preparing summary of findings tables-binary outcomes. J Clin Epidemiol. 2013;66:158-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 490] [Cited by in RCA: 620] [Article Influence: 47.7] [Reference Citation Analysis (0)] |
| 24. | Haidukewych GJ. Intertrochanteric fractures: ten tips to improve results. Instr Course Lect. 2010;59:503-509. [PubMed] |
| 25. | Radford PJ, Needoff M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg Br. 1993;75:789-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 209] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 26. | Leung KS, So WS, Shen WY, Hui PW. Gamma nails and dynamic hip screws for peritrochanteric fractures. A randomised prospective study in elderly patients. J Bone Joint Surg Br. 1992;74:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 229] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 27. | Konstantinidis L, Papaioannou C, Mehlhorn A, Hirschmüller A, Südkamp NP, Helwig P. Salvage procedures for trochanteric femoral fractures after internal fixation failure: biomechanical comparison of a plate fixator and the dynamic condylar screw. Proc Inst Mech Eng H. 2011;225:710-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Neogi DS, Trikha V, Mishra KK, Rohilla N, Yadav CS. Biological plate fixation of comminuted subtrochanteric fractures with the Dynamic Condylar Screw: a clinical study. Acta Orthop Belg. 2009;75:497-503. [PubMed] |
| 29. | McKibbin B. The biology of fracture healing in long bones. J Bone Joint Surg Br. 1978;60-B:150-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 776] [Cited by in RCA: 659] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 30. | Huang SG, Chen B, Zhang Y, Nie FF, Ju L, Li M, Zhang YH. Comparison of the Clinical Effectiveness of PFNA, PFLCP, and DHS in Treatment of Unstable Intertrochanteric Femoral Fracture. Am J Ther. 2017;24:e659-e666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 31. | Simmermacher RK, Bosch AM, Van der Werken C. The AO/ASIF-proximal femoral nail (PFN): a new device for the treatment of unstable proximal femoral fractures. Injury. 1999;30:327-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 139] [Article Influence: 5.3] [Reference Citation Analysis (0)] |