Published online Aug 18, 2024. doi: 10.5312/wjo.v15.i8.744
Revised: May 30, 2024
Accepted: July 9, 2024
Published online: August 18, 2024
Processing time: 207 Days and 15.6 Hours
Patient reported outcome measures (PROMs) can be used to assess knee function following anterior cruciate ligament (ACL) reconstruction. Intra-operatively, femoral and tibial tunnels are created to accommodate the new ACL graft. It is postulated that there is an optimum position and orientation of these tunnels and that outcomes from this procedure are affected by their position.
To evaluate the influence of graft tunnel position on early to mid-term clinical outcomes following ACL reconstruction.
Six PROMs were collected following ACL reconstruction which included the Knee Injury and Osteoarthritis Outcome Score (KOOS), International Knee Documen
A total of 87 patients were included in the study with a mean post-operative follow-up of 2.3 years (range 1 to 7 years). Posterior position of tibial tunnel was associated with improved KOOS quality of life (rho = 0.43, P = 0.002) and EQ-5D VAS (rho = 0.36, P = 0.010). Anterior position of EndoButton femoral tunnel was associated with an improved EQ-5D index (rho = -0.38, P = 0.028). There were no other significant correlations between any of the other radiological parameters and PROM scores.
Overall, graft tunnel position had very little correlation with clinical outcomes following ACL reconstruction. A few (posterior) tibial tunnel and (anterior) EndoButton femoral tunnel measurements were associated with better PROMs.
Core Tip: This is an observational cross-sectional study investigating the effect of graft tunnel position following anterior cruciate ligament reconstruction and its association with patient reported outcome measures (PROMs). PROMs were collected before and at a minimum of 12 months following surgery. The results of these questionnaires were analysed to determine whether radiological measurements of graft tunnel position had a significant impact on early to mid-term clinical outcomes. If significance is found, it is important to determine the most optimal position for the tunnels to improve patients’ function following these procedures.
- Citation: Mann O, Al-Dadah O. Anterior cruciate ligament reconstruction: Effect of graft tunnel position on early to mid-term clinical outcomes. World J Orthop 2024; 15(8): 744-753
- URL: https://www.wjgnet.com/2218-5836/full/v15/i8/744.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i8.744
Anterior cruciate ligament (ACL) rupture is a debilitating injury for an increasing number of patients. It is estimated that between 100000 and 200000 cases of ACL rupture occur in the United States every year[1]. Consequently, the volume of ACL reconstruction surgery being performed is rising. Between 1994 and 2006 the frequency of ACL reconstruction surgery has risen by 37% in the United States[2]. The procedure requires a new graft to be fixed in place of the original ACL in order to restore knee stability. As a requirement for the graft to be fixed in place, bone tunnels must be drilled into the tibia and femur to accommodate the new graft. These tunnels must be drilled in a position that allows the new graft to have the same orientation as the native ACL, and thereby improve the functional stability of the knee joint[3-5]. It is postulated that the position and orientation of these tunnels have an effect on post-operative clinical outcomes for patients. Current national guidelines in the United Kingdom state that the femoral tunnel should be placed in an anatomical or near-anatomical position, between 9 o’clock and 11 o’clock (right knee) or between 1 o’clock and 3 o’clock (left knee) as referenced from clock face positions in the coronal plane[6]. If the position of the femoral tunnel is too anterior in the sagittal plane, there is risk of loss of full flexion of the knee and graft rupture once movement is regained following surgery[6]. If the tunnel is too posterior in the sagittal plane, there is a risk of it breaking through the posterior wall of the femur[6]. The tibial tunnel is generally placed in the middle third of the tibia, too anterior and it can lead to loss of extension due to impingement, too posterior it can impinge on the posterior cruciate ligament (PCL)[6].
Patient reported outcome measures (PROMs) are used to generate quantitative data relating to the clinical function of the knee joint. Patients complete validated questionnaires which can be used to quantify the level of disability associated with an ACL rupture and the functional improvement following surgery. They can also be used to evaluate various patient and surgical factors associated with functional outcome which can better inform clinical practice.
The aim of this study was to evaluate the influence of graft tunnel position on early to mid-term clinical outcomes following ACL reconstruction. The hypothesis is that no correlation exists between radiological parameters and post-operative PROMs.
This is an observational cross-sectional study. All the patients included in this study attended a specialist knee clinic and underwent ACL reconstruction surgery following clinical assessment and radiological investigation between October 2015 and April 2022. This study was registered with the Institution’s Clinical Effectiveness Department (registration number CA10358). This therapeutic research study constituted part the first author’s Masters dissertation. Some of the post-operative PROM data points presented in this study were also used in another longitudinal observational study which has also been submitted for publication, but all the radiological data points and the analysis itself in this study are entirely original.
Inclusion criteria consisted of patients with an ACL rupture whose symptoms where refractory to an initial period of conservative treatment (i.e., physiotherapy, activity modification, etc.) who subsequently underwent an arthroscopic primary, anatomic single bundle ACL reconstruction using either middle third bone-patella tendon-bone autograft or quadrupled hamstring tendon (gracilis and semitendinosus) autograft. Hamstring grafts were secured to the femur via suspensory fixation using EndoButton (Smith & Nephew Inc., Andover, MA, United States) and to the tibia using radiolucent polyetheretherketone (PEEK) interference screws (Smith & Nephew Inc., Andover, MA, United States) or round cannulated interference screws (Smith & Nephew Inc., Andover, MA, United States). Patella tendon grafts were secured using Softsilk interference screws (Smith & Nephew Inc., Andover, MA, United States) both in the femur and the tibia. The femoral tunnel was drilled using the transportal technique for both graft types and the tibial tunnel was drilled using a standard tibial jig set to 60 degrees for the patella tendon graft and 55 degrees for the hamstring graft. Both the femoral and tibial tunnels were centred on the native ACL footprint. Exclusion criteria consisted of PCL tear, multi-ligament reconstruction, revision ACL reconstruction and advanced osteoarthritis.
A total of 6 validated PROMs were used in this study which included the Knee Injury and Osteoarthritis Outcome Score (KOOS)[7,8], EuroQol-5 Dimension-5 level (EQ-5D-5L)[9-12], International Knee Documentation Committee (IKDC) score[13,14], Tegner score[15], Lysholm score[15], and the 12-item Short Form survey[16]. There were two patients who were under 16 years of age at the time of surgery but were aged over 16 years at the latest point of contact post-operatively at the time of conducting this study (via postal questionnaire) and therefore completed the same (adult) PROM forms as the rest of the study cohort.
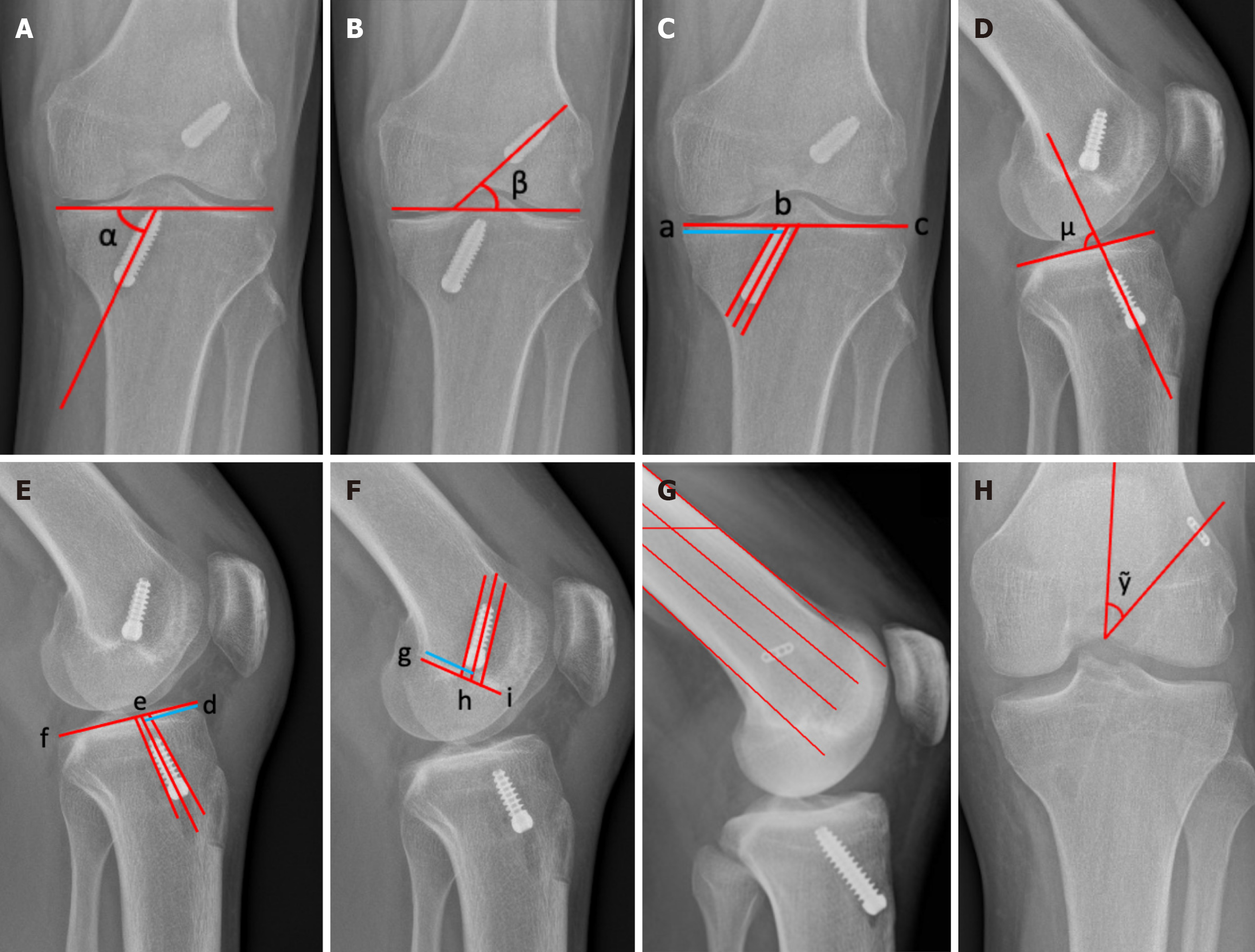
Post-operative X-rays were evaluated by the first author, after receiving appropriate training from the senior author and thereafter a proforma was devised and adhered to. Accuracy was ensured by initially repeating the evaluation on a patient sample to allow for recognition of errors in calculation and/or measurements on X-rays. The interobserver reliability of these measurements has previously been evaluated by Nema et al[17] and found to have high intraclass correlation coefficients (ranging from 0.71 to 0.96) between reviewers. The following radiological measurements were evaluated as illustrated in Figure 1.
Coronal angle of the tibial tunnel (α) (Figure 1A)[17]. This angle is found by drawing a line over the tibial plateau on an AP radiograph, intersected by a line following the course of the tibial tunnel. The angle is measured between these two lines and gives the coronal angle of the tibial tunnel[17].
Coronal angle of the femoral tunnel (β) (Figure 1B)[17]. This angle is found by drawing a line across the lowermost points of the femoral condyles on an AP radiograph, intersected by a line following the course of the femoral tunnel. The angle is measured between these two lines and gives the coronal angle of the femoral tunnel[17].
Coronal position of the tibial tunnel ab/ac (%) (Figure 1C)[17]. This is found by drawing a line across the tibial plateau on an AP radiograph, and this line is measured. A line is drawn that intersects the tibial plateau line, that runs through the centre of the tibial tunnel. The distance between the medial-most point of the tibial plateau and the point where these two lines intersect is measured and expressed as a percentage distance of the width of the tibial plateau[17].
Transplant orientation to joint angle (μ) (Figure 1D)[18]. The angle is found by drawing a line parallel to the tibial plateau on a lateral radiograph. A second line is drawn parallel to the direction of the tibial tunnel. The angle where these two lines intersect is the transplant orientation to joint angle[18].
Sagittal position of the tibial tunnel de/df (%) (Figure 1E)[17]. A line is drawn across the tibial plateau on lateral radiograph and measured. Another line is drawn through the centre of the tibial tunnel. The distance from the most anterior point of the tibial plateau to where these two lines intersect is measured and expressed as a percentage length of the tibial plateau line. This is the sagittal tibial tunnel position[17].
Position along Blumensaat’s line gh/gi (%) (Figure 1F)[17,19]. This was measured only for patients who had an interference screw in the femoral tunnel. First, the position along Blumensaat’s line was measured. Blumensaat’s line is drawn on a lateral radiograph along the roof of the intercondylar notch of the femur and measured[19]. Another line is drawn through the centre of the femoral tunnel. The distance from where these two lines intersect and the most posterior point of Blumensaat’s line is measured and expressed as a percentage of the length of Blumensaat’s line. This is the femoral tunnel position along Blumensaat’s line[17].
EndoButton position (anterior, middle, or posterior) (Figure 1G)[20]. To find this, two lines are drawn parallel to the anterior and posterior cortices of the femur on lateral radiograph. Two further lines are drawn between these two lines in a way that the three spaces between these four lines are all the same width. From this point, it can be assessed whether the EndoButton is anterior, middle, or posterior[20].
Femoral tunnel angle to femoral diaphysis (º) (Figure 1H)[21]. This is found by drawing a line parallel to the femoral diaphysis from the intercondylar notch on AP radiograph. Another line is drawn from the intercondylar notch, through the centre of the EndoButton. The angle between these lines is measured and recorded as the angle of femoral tunnel to femur[21].
Plotted histograms with fitted curve lines, box-plots, normal Q-Q plots, and the Shapiro-Wilk statistic were used to test normality of data distribution. All the radiological measurement data (continuous variables) and all the PROM data (continuous variables) displayed a skewed distribution and therefore the relevant non-parametric statistical tests were used for the data analysis. The Spearman’s Rank correlation test was used for the main correlation analysis and the Kruskal-Wallis H test was used for the comparison between EndoButton positions. The level of statistical significance was set at P < 0.05. Statistical analysis was performed using SPSS for Windows version 28.0 (IBM Corp., Armonk, NY, United States).
Table 1 shows the demographics of the patients in the study at the time of surgery, showing a mean age of 31.5, over twice as many males as females (60:27) (more males participated in at risk activities which result in ACL rupture), and a mean body mass index of 27.5.
| Item | n = 87 |
| Age (years), mean (range) | 31.5 (12.0-62.0) |
| Sex (male:female) | 60:27 |
| Laterality (left:right) | 44:43 |
| Graft type (hamstring:BTB) | 60:27 |
| Height (cm), mean ± SD | 174.3 ± 8.8 |
| Weight (kg), mean ± SD | 84.1 ± 18.0 |
| BMI (kg/m2), mean ± SD | 27.5 ± 5.4 |
Table 2 shows the measurements of the post-operative X-ray parameters as described in Figure 1. Table 3 shows the results of all the post-operative PROM data collected. The mean time between surgery and completion of post-operative PROM questionnaires was 2.3 years (range 1.0 to 7.0 years).
| Item | Median (inter-quartile range) |
| Coronal position tibial tunnel (%) | 46.3 (42.7-49.6) |
| Coronal angle tibial tunnel (º) | 70.8 (66.7-76.4) |
| Coronal angle femoral tunnel (º) | 45.7 (39.8-52.0) |
| Sagittal position tibial tunnel (%) | 44.8 (38.4-54.5) |
| Transplant orientation to joint (º) | 68.3 (60.7-72.7) |
| Position along Blumensaat’s line (%) | 47.2 (36.3-53.8) |
| Angle of femoral tunnel to femur (º) | 38.9 (35.2-43.7) |
| Item | Median (inter-quartile range) |
| KOOS pain | 89 (78-97) |
| KOOS symptom | 79 (68-86) |
| KOOS ADL | 97 (90-100) |
| KOOS sport/rec | 75 (60-85) |
| KOOS QoL | 63 (44-75) |
| KOOS overall | 81 (70-87) |
| IKDC | 75 (64-86) |
| Lysholm | 87 (76-91) |
| Tegner | 5 (4-7) |
| EQ-5D index | 0.837 (0.728-1.000) |
| EQ-5D VAS | 85 (70-90) |
| SF-12 MCS | 53 (45-58) |
| SF-12 PCS | 54 (47-57) |
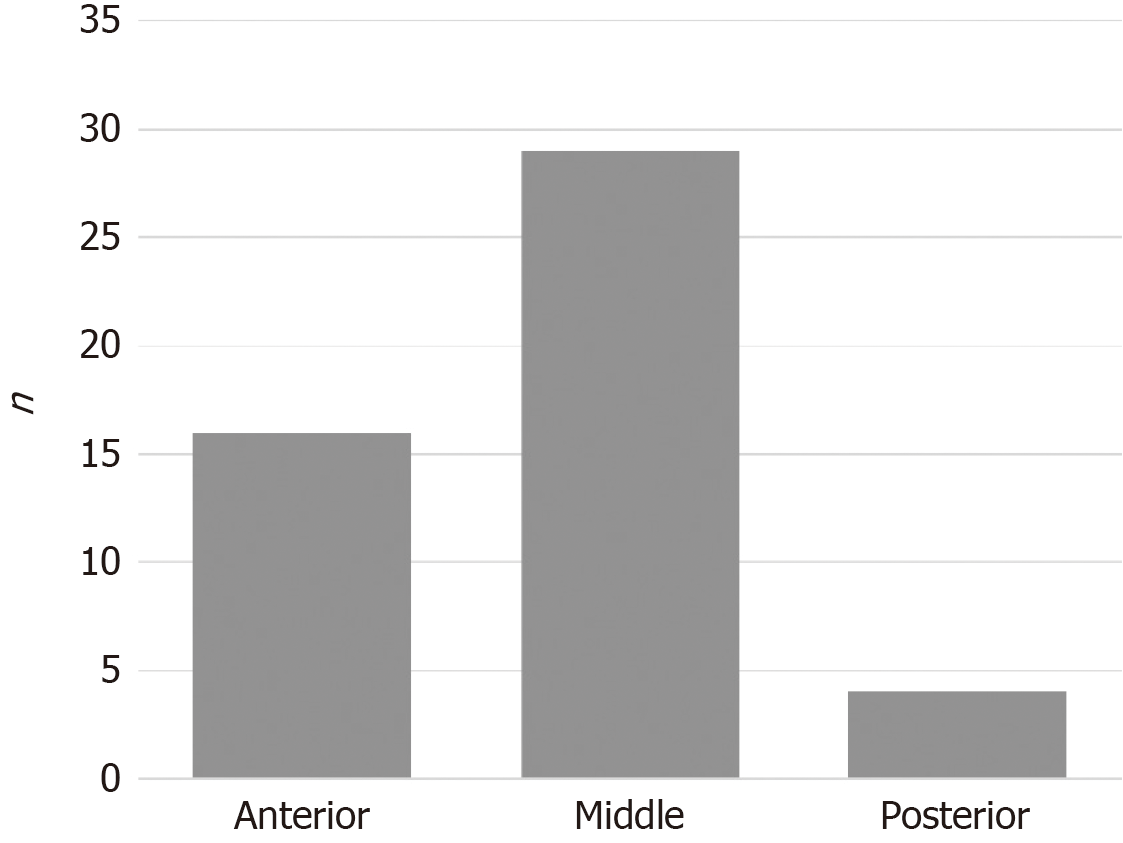
Figure 2 shows the numbers of patients in each position for EndoButton placement. The middle position was the most common for EndoButton placement which is in keeping with the anatomic ACL footprint targeted as part of the surgical technique. Table 4 shows that none of the PROM scores showed a significant difference dependent on the position of the EndoButton after ACL reconstruction using hamstring tendon autograft.
| Anterior, median (IQR) | Middle, median (IQR) | Posterior, median (IQR) | P value1 | H | |
| KOOS pain | 88 (73-97) | 85 (67-95) | 88 (82-91) | 0.748 | 0.6 |
| KOOS symptom | 79 (68-89) | 79 (57-83) | 83 (68-88) | 0.612 | 1.0 |
| KOOS ADL | 98 (87-100) | 92 (71-97) | 95 (92-96) | 0.227 | 3.0 |
| KOOS sport/rec | 78 (61-85) | 73 (45-75) | 73 (51-75) | 0.393 | 1.9 |
| KOOS QoL | 57 (25-80) | 56 (31-65) | 57 (40-69) | 0.820 | 0.4 |
| KOOS overall | 81 (64-85) | 77 (59-82) | 79 (67-83) | 0.440 | 1.6 |
| IKDC | 75 (53-77) | 69 (56-77) | 71 (64-72) | 0.664 | 0.8 |
| Lysholm | 88 (71-94) | 85 (74-89) | 83 (74-89) | 0.722 | 0.7 |
| Tegner | 5 (3-7) | 5 (3-7) | 4 (2-5) | 0.454 | 1.6 |
| EQ-5D index | 1 (0.746-1.000) | 0.750 (0.657-0.919) | 0.704 (0.668-0.810) | 0.097 | 4.7 |
| EQ-5D VAS | 74 (61-84) | 88 (64-91) | 73 (70-86) | 0.161 | 3.6 |
| SF-12 MCS | 51 (47-59) | 54 (40-59) | 54 (37-58) | 0.964 | 0.1 |
| SF-12 PCS | 55 (50-57) | 52 (35-56) | 46 (44-47) | 0.266 | 2.7 |
Table 5 shows that overall, there was no significant correlation between PROM scores and radiological parameters. The sagittal position of the tibial tunnel showed significant positive correlations with KOOS quality of life sub-score (P = 0.002), and the EQ-5D VAS sub-score (P = 0.010). Better scores were achieved in patients who had tibial tunnels placed more posteriorly. There was also a significant negative correlation between EndoButton position and the EQ-5D index sub-score (P = 0.028). Patients scored better if they have a more anterior EndoButton position.
| Coronal position TT | Coronal angle TT | Coronal angle FT | Sagittal position TT | TOJ | Position along Blumensaat’s line | Angle of FT to femur | EndoButton position | ||
| KOOS pain | rho | 0.150 | -0.160 | 0.040 | 0.200 | 0.030 | 0.370 | 0.090 | -0.090 |
| P value | 0.297 | 0.251 | 0.801 | 0.158 | 0.809 | 0.109 | 0.603 | 0.621 | |
| KOOS symptom | rho | 0.030 | -0.150 | -0.030 | 0.210 | -0.050 | -0.050 | 0.060 | -0.050 |
| P value | 0.828 | 0.285 | 0.818 | 0.127 | 0.709 | 0.823 | 0.736 | 0.778 | |
| KOOS ADL | rho | 0.093 | -0.140 | 0.190 | 0.200 | -0.060 | 0.140 | -0.150 | -0.240 |
| P value | 0.507 | 0.317 | 0.178 | 0.150 | 0.688 | 0.548 | 0.410 | 0.170 | |
| KOOS sport/rec | rho | 0.110 | -0.040 | 0.200 | 0.120 | 0.010 | 0.320 | 0.030 | -0.220 |
| P value | 0.436 | 0.771 | 0.166 | 0.410 | 0.944 | 0.190 | 0.864 | 0.220 | |
| KOOS QoL | rho | 0.230 | -0.110 | 0.200 | 0.430 | -0.200 | 0.080 | 0.010 | -0.020 |
| P value | 0.097 | 0.441 | 0.147 | 0.002a | 0.157 | 0.735 | 0.956 | 0.928 | |
| KOOS overall | rho | 0.170 | -0.040 | 0.160 | 0.250 | -0.090 | 0.230 | 0.020 | -0.140 |
| P value | 0.220 | 0.757 | 0.255 | 0.080 | 0.551 | 0.344 | 0.919 | 0.423 | |
| IKDC | rho | 0.180 | -0.100 | 0.150 | 0.260 | 0.070 | 0.260 | 0.170 | -0.160 |
| P value | 0.202 | 0.517 | 0.288 | 0.060 | 0.635 | 0.268 | 0.358 | 0.381 | |
| Lysholm | rho | 0.010 | -0.210 | -0.110 | 0.200 | -0.020 | 0.290 | 0.290 | -0.140 |
| P value | 0.921 | 0.139 | 0.446 | 0.166 | 0.898 | 0.232 | 0.105 | 0.453 | |
| Tegner | rho | -0.040 | 0.200 | -0.020 | 0.200 | 0.140 | 0.130 | 0.130 | -0.180 |
| P value | 0.766 | 0.178 | 0.913 | 0.900 | 0.333 | 0.582 | 0.500 | 0.355 | |
| EQ-5D index | rho | 0.060 | -0.150 | -0.010 | 0.260 | -0.100 | 0.310 | 0.070 | -0.380 |
| P value | 0.659 | 0.285 | 0.933 | 0.068 | 0.491 | 0.192 | 0.698 | 0.028a | |
| EQ-5D VAS | rho | 0.030 | 0.020 | -0.080 | 0.360 | -0.180 | 0.010 | 0.130 | 0.240 |
| P value | 0.820 | 0.891 | 0.566 | 0.010a | 0.213 | 0.962 | 0.461 | 0.174 | |
| SF-12 MCS | rho | 0.000 | -0.140 | -0.070 | 0.110 | -0.010 | 0.110 | 0.040 | 0.050 |
| P value | 0.999 | 0.339 | 0.650 | 0.459 | 0.956 | 0.641 | 0.822 | 0.797 | |
| SF-12 PCS | rho | 0.170 | -0.110 | 0.120 | 0.220 | -0.100 | 0.290 | -0.070 | -0.280 |
| P value | 0.244 | 0.467 | 0.405 | 0.144 | 0.524 | 0.223 | 0.732 | 0.129 |
This study has shown that overall, graft tunnel position does not correlate with post-operative clinical outcomes following ACL reconstruction.
Although there were no significant differences between median post-operative PROM scores with EndoButton position, there was a significant correlation between anterior EndoButton position and improved EQ-5D index sub-score. Conversely, Kazemi et al[22] found that improved clinical outcomes were associated with a more posteriorly placed EndoButton. Post-operative X-rays demonstrated that the EndoButton was most frequently positioned in the middle of the femur which is consistent with the anatomic surgical technique which targeted the centre of the ACL footprint. The post-operative PROM results showed no significant differences between the three EndoButton positions (anterior, middle, and posterior). This implies that EndoButton position has minimal effect on clinical outcomes, a finding supported by Gunaydin et al[20].
Graft tunnel position was not shown to effect PROMs to a significant extent, but the sagittal position of the tibial tunnel showed significant correlations with two of the outcome measures, higher scores being associated with a more posteriorly placed tibial tunnel. The more posterior the tibial tunnel, the greater scores were reported in KOOS quality of life and EQ-5D VAS sub-scores. However, Pinczewski et al[23] found that a more posteriorly placed tibial tunnel had greater association with re-rupture, and a more vertical inclination of the tibial tunnel was associated with persistent rotational instability following surgery[23]. Other studies evaluating graft tunnel position also suggested that a more posteriorly placed tibial tunnel was associated with worse outcomes and a greater degree of rotational instability[24,25]. One study looked at the effect of graft tunnel position on clinical outcomes, using IKDC, and graft failure rates[26]. They found that position of the tunnels had no effect on IKDC scores, a finding supported in the present study[26]. However, they concluded that a more anteriorly placed femoral tunnel was associated with an increased graft failure rate. This is an outcome that was not evaluated in the present study due to the very small number of re-ruptures. Larger studies would be required to investigate this association further. Kazemi et al[22] also found a correlation between a smaller coronal angle of the femoral tunnel (less vertical, more horizontal) and improved clinical outcomes, which was not found in the present study.
Opinion is varied when discussing optimal positioning of drilled tunnels for single bundle ACL reconstruction[27], however there are some well-established pitfalls within the literature. A tibial tunnel that is too anterior increases the risk of intercondylar notch roof impingement, which can lead to a higher rate of graft failure[28]. Roof impingement can present clinically as loss of full extension and an increase in laxity post-operatively[28]. The risk of roof impingement is potentially reduced if the tunnels are drilled within the original footprints of the native ACL[28]. The present study showed significantly improved PROMs for patients with a more posteriorly placed tibial tunnel, supporting this theory.
Another type of impingement that can occur is impingement on the PCL. This is most likely to occur whilst in flexion when the new graft lies on top of the PCL[28]. Again, drilling the tunnels within the footprints of the native ACL has the potential to reduce this risk, along with drilling the femoral tunnel at a 60º angle in the coronal plane[28,29]. On the other hand, one study found that depending on femoral footprint position, certain individuals may be over 50 times as likely to suffer from an ACL rupture[30]. They found that people that had suffered from an ACL rupture had significantly different femoral footprints than those who did not, those with a more posterior footprint and one that is more proximal to the flexion-extension axis of the knee are at greater risk[30]. This could lead to the formulation of the question, if people who rupture their ACL have an abnormal femoral footprint that predisposes them to ACL rupture, why is anatomical reconstruction seen as the most optimal reconstruction method for these patients?
When discussing the femoral tunnel, the clock face method is the most often referenced. The United Kingdom national guidelines state that optimal positioning for the femoral tunnel is between 9 o’clock and 11 o’clock (right knee) or between 1 o’clock and 3 o’clock (left knee)[6]. However, there are many different descriptions of the clock face method that exist and using different methods causes significant variations in tunnel position[31,32]. For this reason, a number of authors have recommended against using this method[31,32].
Allografts, although not routinely recommended for primary ACL reconstruction in younger, active patients, are often indicated for revision ACL reconstructions[33]. The tunnel placements recommended for allograft tissue are the same as for autograft tissue, described as “anatomical positioning”[33]. This requires the tunnels accommodating the new graft to be within the native ACL “footprint”, to achieve similar position and orientation as the native ACL[24]. However, Borque et al[24] also state that anatomical positioning alone is not optimal for any ACL reconstruction, as the footprint of the native ACL is often larger than the new graft size. As a result, it is recommended that the tibial tunnel aperture is drilled in the most anterior position of the native footprint, without causing graft impingement in the notch[24]. As for the femoral tunnel, the isometric anteromedial position of the tunnel aperture within the native footprint is recommended[24].
Despite finding an association that is opposite to previous studies[23-25], a particular strength of the present study was the wide variety of PROM instruments that were used. Previous studies have either only used IKDC[23,26] or Lysholm scores in isolation[22]. The main limitation of this study was the additional number of patients that were lost to follow-up as otherwise a greater total number of patients could have been included in this study. This was a pragmatic clinical study of real time clinical practice and as such is subject to the variables which effect every day clinical practice. Patients who undergo ACL reconstruction are generally young patients who often move away from the hospital from which they had their original surgery for work purposes (i.e., university students graduating and moving to another city, etc.). All the radiological parameters were measured by one reviewer only (the first author) which may present a potential limitation of this study. However, to mitigate this factor, sufficient training was delivered by the senior author and a proforma was devised and adhered to throughout the data collection process. Intra- and inter-observer reliability was not the focus of this study as this has already been evaluated by other published studies[17] and could also inform suggestions for future researchers[17].
Overall, graft tunnel position, as evaluated by radiological parameters from post-operative X-rays, had very little correlation with clinical outcomes following ACL reconstruction. A few tibial tunnel measurements (posteriorly placed) and EndoButton femoral tunnel measurement (anteriorly placed) were associated with better PROM scores.
| 1. | Evans J, Mabrouk A, Nielson JL. Anterior Cruciate Ligament Knee Injury. 2023 Nov 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 2. | Buller LT, Best MJ, Baraga MG, Kaplan LD. Trends in Anterior Cruciate Ligament Reconstruction in the United States. Orthop J Sports Med. 2015;3:2325967114563664. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 145] [Cited by in RCA: 222] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 3. | Miller MD, Cole BJ, Cosgarea AJ, Sekiya JK. Operative techniques: sports knee surgery. Philadelphia: Saunders/Elsevier, 2008. |
| 4. | Frank RM, Hamamoto JT, Bernardoni E, Cvetanovich G, Bach BR Jr, Verma NN, Bush-Joseph CA. ACL Reconstruction Basics: Quadruple (4-Strand) Hamstring Autograft Harvest. Arthrosc Tech. 2017;6:e1309-e1313. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Wilding CSR, Cruz CCA, Mannino LBJ, Deal CJB, Wake CJ, Bottoni CR. Bone-Tendon-Autograft Anterior Cruciate Ligament Reconstruction: A New Anterior Cruciate Ligament Graft Option. Arthrosc Tech. 2020;9:e1525-e1530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | British Orthopaedic Association. Best Practice for Management ofAnterior Cruciate Ligament (ACL) Injuries. September 2023. [cited 29 May 2024]. Available from: https://www.boa.ac.uk/static/88a4c3e3-df3e-4e51-a92e7d2f86d7d82a/Best-Practice-Book-for-management-of-Anterior-Cruciate-Ligament-injuries.pdf. |
| 7. | Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1182] [Cited by in RCA: 1674] [Article Influence: 76.1] [Reference Citation Analysis (0)] |
| 8. | Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2362] [Cited by in RCA: 2817] [Article Influence: 104.3] [Reference Citation Analysis (0)] |
| 9. | Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3986] [Cited by in RCA: 4412] [Article Influence: 152.1] [Reference Citation Analysis (0)] |
| 10. | EuroQol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10083] [Cited by in RCA: 11533] [Article Influence: 329.5] [Reference Citation Analysis (0)] |
| 11. | Bilbao A, García-Pérez L, Arenaza JC, García I, Ariza-Cardiel G, Trujillo-Martín E, Forjaz MJ, Martín-Fernández J. Psychometric properties of the EQ-5D-5L in patients with hip or knee osteoarthritis: reliability, validity and responsiveness. Qual Life Res. 2018;27:2897-2908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 145] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 12. | Greiner W, Weijnen T, Nieuwenhuizen M, Oppe S, Badia X, Busschbach J, Buxton M, Dolan P, Kind P, Krabbe P, Ohinmaa A, Parkin D, Roset M, Sintonen H, Tsuchiya A, de Charro F. A single European currency for EQ-5D health states. Results from a six-country study. Eur J Health Econ. 2003;4:222-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 370] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 13. | Irrgang JJ, Anderson AF. Development and validation of health-related quality of life measures for the knee. Clin Orthop Relat Res. 2002;95-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 100] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1375] [Cited by in RCA: 1592] [Article Influence: 66.3] [Reference Citation Analysis (0)] |
| 15. | Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;43-49. [PubMed] |
| 16. | Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11319] [Cited by in RCA: 12818] [Article Influence: 442.0] [Reference Citation Analysis (0)] |
| 17. | Nema SK, Balaji G, Akkilagunta S, Menon J, Poduval M, Patro D. Radiologic assessment of femoral and tibial tunnel placement based on anatomic landmarks in arthroscopic single bundle anterior cruciate ligament reconstruction. Indian J Orthop. 2017;51:286-291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Laux CJ, Ulbrich EJ, Andreisek G, Marcon M, Fischer MA, Mehra T, Ciritsis BD. Impact of graft and tunnel orientation on patient-reported outcome in anterior cruciate ligament reconstruction using bone-patellar tendon-bone autografts. J Orthop Surg Res. 2018;13:245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Skandhan A, Goel A. Blumensaat line. 2013. [cited 29 May 2024]. Available from: https://radiopaedia.org/articles/blumensaat-line-1. |
| 20. | Gunaydin B, Sever C, Cetin MU, Sari A, Dincel YM, Sener B, Varol R, Heybeli N. Does radiological evaluation of endobutton positioning in the sagittal plane affect clinical functional results in single-bundle anterior cruciate ligament reconstruction? Arch Orthop Trauma Surg. 2021;141:977-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Kim M, Choi YS, Kim H, Choi NH. Postoperative Evaluation after Anterior Cruciate Ligament Reconstruction: Measurements and Abnormalities on Radiographic and CT Imaging. Korean J Radiol. 2016;17:919-930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Kazemi SM, Abbasian MR, Esmailijah AA, Zafari A, Shahrbabaki ZS, Keshavarz AH, Esmaeilijah N, Safdari F. Comparison of Clinical Outcomes between Different Femoral Tunnel Positions after Anterior Cruciate Ligament Reconstruction Surgery. Arch Bone Jt Surg. 2017;5:419-425. [PubMed] |
| 23. | Pinczewski LA, Salmon LJ, Jackson WF, von Bormann RB, Haslam PG, Tashiro S. Radiological landmarks for placement of the tunnels in single-bundle reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2008;90:172-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 113] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 24. | Borque KA, Laughlin MS, Pinheiro VH, Jones M, Williams A. Rebranding the ‘anatomic’ ACL reconstruction: Current concepts. J ISAKOS. 2023;8:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 25. | McGuire DA, Hendricks SD. Improper posterior tibial tunnel graft placement. Arthroscopy. 2008;24:1084-5; author reply 1085. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | de Mees TTCR, Reijman M, Waarsing JH, Meuffels DE. Posteriorly positioned femoral grafts decrease long-term failure in anterior cruciate ligament reconstruction, femoral and tibial graft positions did not affect long-term reported outcome. Knee Surg Sports Traumatol Arthrosc. 2022;30:2003-2013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | McConkey MO, Amendola A, Ramme AJ, Dunn WR, Flanigan DC, Britton CL; MOON Knee Group, Wolf BR, Spindler KP, Carey JL, Cox CL, Kaeding CC, Wright RW, Matava MJ, Brophy RH, Smith MV, McCarty EC, Vida AF, Wolcott M, Marx RG, Parker RD, Andrish JF, Jones MH. Arthroscopic agreement among surgeons on anterior cruciate ligament tunnel placement. Am J Sports Med. 2012;40:2737-2746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Paschos NK, Howell SM. Anterior cruciate ligament reconstruction: principles of treatment. EFORT Open Rev. 2016;1:398-408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 99] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 29. | Simmons R, Howell SM, Hull ML. Effect of the angle of the femoral and tibial tunnels in the coronal plane and incremental excision of the posterior cruciate ligament on tension of an anterior cruciate ligament graft: an in vitro study. J Bone Joint Surg Am. 2003;85:1018-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 144] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 30. | Dimitriou D, Wang Z, Zou D, Tsai TY, Helmy N. The Femoral Footprint Position of the Anterior Cruciate Ligament Might Be a Predisposing Factor to a Noncontact Anterior Cruciate Ligament Rupture. Am J Sports Med. 2019;47:3365-3372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Kraeutler MJ, Patel KV, Hosseini A, Li G, Gill TJ, Bravman JT. Variability in the Clock Face View Description of Femoral Tunnel Placement in ACL Reconstruction Using MRI-Based Bony Models. J Knee Surg. 2018;31:965-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 32. | Han Y, Hart A, Martineau PA. Is the clock face an accurate, precise, and reliable measuring tool for anterior cruciate ligament reconstruction? Arthroscopy. 2014;30:849-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 33. | Vyas D, Rabuck SJ, Harner CD. Allograft anterior cruciate ligament reconstruction: indications, techniques, and outcomes. J Orthop Sports Phys Ther. 2012;42:196-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |