Published online Aug 18, 2024. doi: 10.5312/wjo.v15.i8.683
Revised: June 13, 2024
Accepted: July 5, 2024
Published online: August 18, 2024
Processing time: 225 Days and 22.7 Hours
Adults requiring total hip arthroplasty (THA) for childhood disorder sequelae present with shortening, limp, pain, and altered gait. THA, which can be particularly challenging due to altered anatomy, requires careful planning, assessment, and computed tomography evaluation. Preoperative templating is essential to establish the appropriate acetabular and femoral size. Information regarding neck length and offset is needed to ensure the proper options are available at THA. Hip centre restoration must be planned preoperatively and achieved intraoperatively with appropriate exposure, identification, and stable fixation with optimum-size components. Identifying the actual acetabular floor is essential as changes include altered anatomy, distortion of the margins and version changes. Proximal femur changes include anatomical variation, decreased canal diameter, cortical thick
Core Tip: Total hip arthroplasty for childhood disorders in adulthood requires careful planning and awareness regarding the acetabular and femoral anatomic variations. Preoperative planning must include templating to understand acetabular and femoral sizing, offset, and neck length requirements, while modularity may be needed to address any meta-diaphyseal changes. Small acetabular and femoral components are commonly required in these hips to achieve good fixation. Preoperative assessment of the shortening pattern would help plan for a femoral shortening osteotomy, which may be necessary in patients with high-riding hips. Adequate exposure, extensive soft-tissue release, and restoration of the hip centre, leg length and offset are required to achieve favourable long-term outcomes.
- Citation: Oommen AT. Total hip arthroplasty for sequelae of childhood hip disorders: Current review of management to achieve hip centre restoration. World J Orthop 2024; 15(8): 683-695
- URL: https://www.wjgnet.com/2218-5836/full/v15/i8/683.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i8.683
Total hip arthroplasty (THA) for sequelae of childhood disorders could be challenging, with distortion of normal anatomy, poor development, and limb length discrepancy[1-3]. The presentation at THA is associated with shortening, pain, and functional limitations. Planning, templating, intraoperative soft tissue releases, identification of true ace
A clinical hip examination with detailed neuromuscular assessment is required before performing THA. Radiological examination with proper anteroposterior (AP) and lateral views, including the entire femur and the limb, would be essential to identify the presence of proximal femoral anatomic variations (e.g., femoral bowing) and to quantify the degree of limb length discrepancy. Computed tomography (CT) can be used as an adjunct to assess bony abnormalities and acetabular and femoral version.
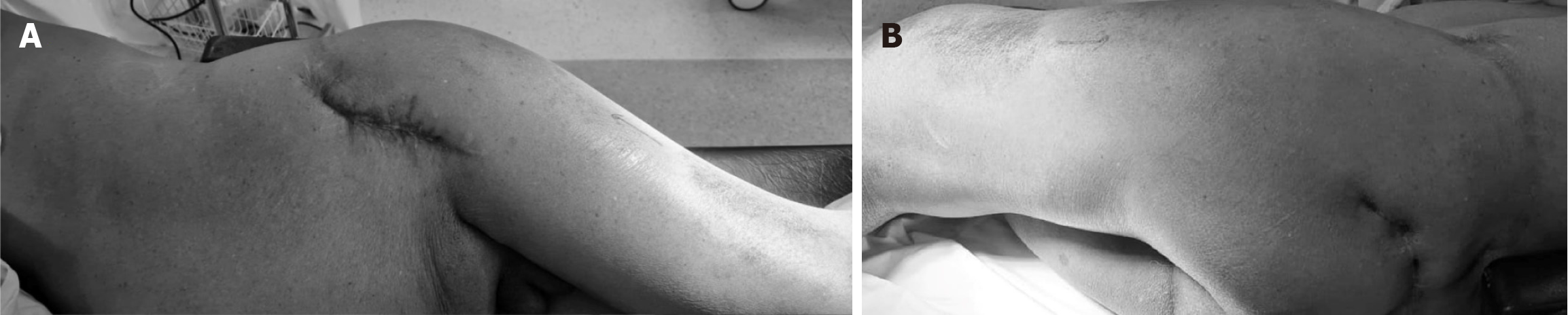
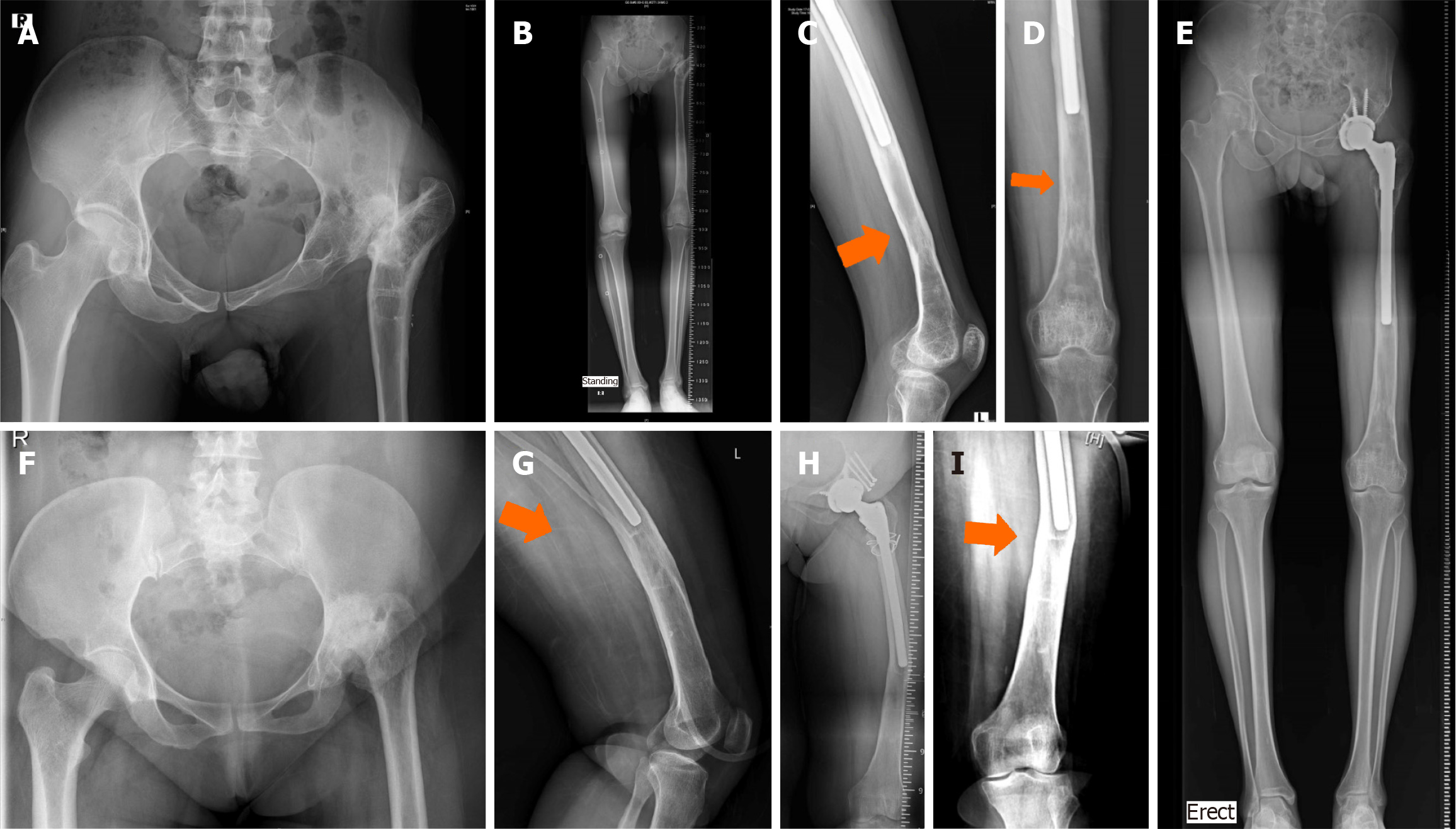
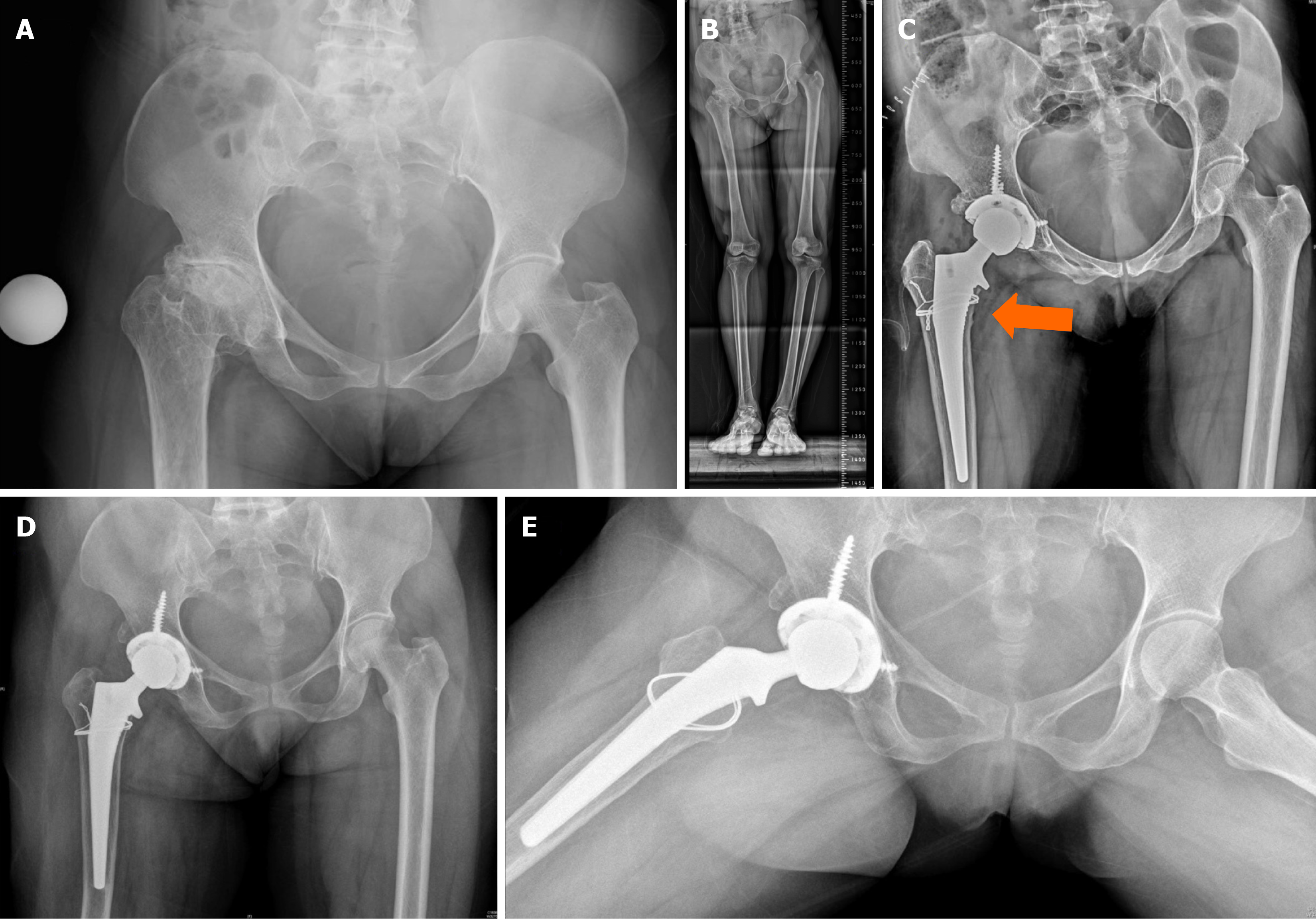
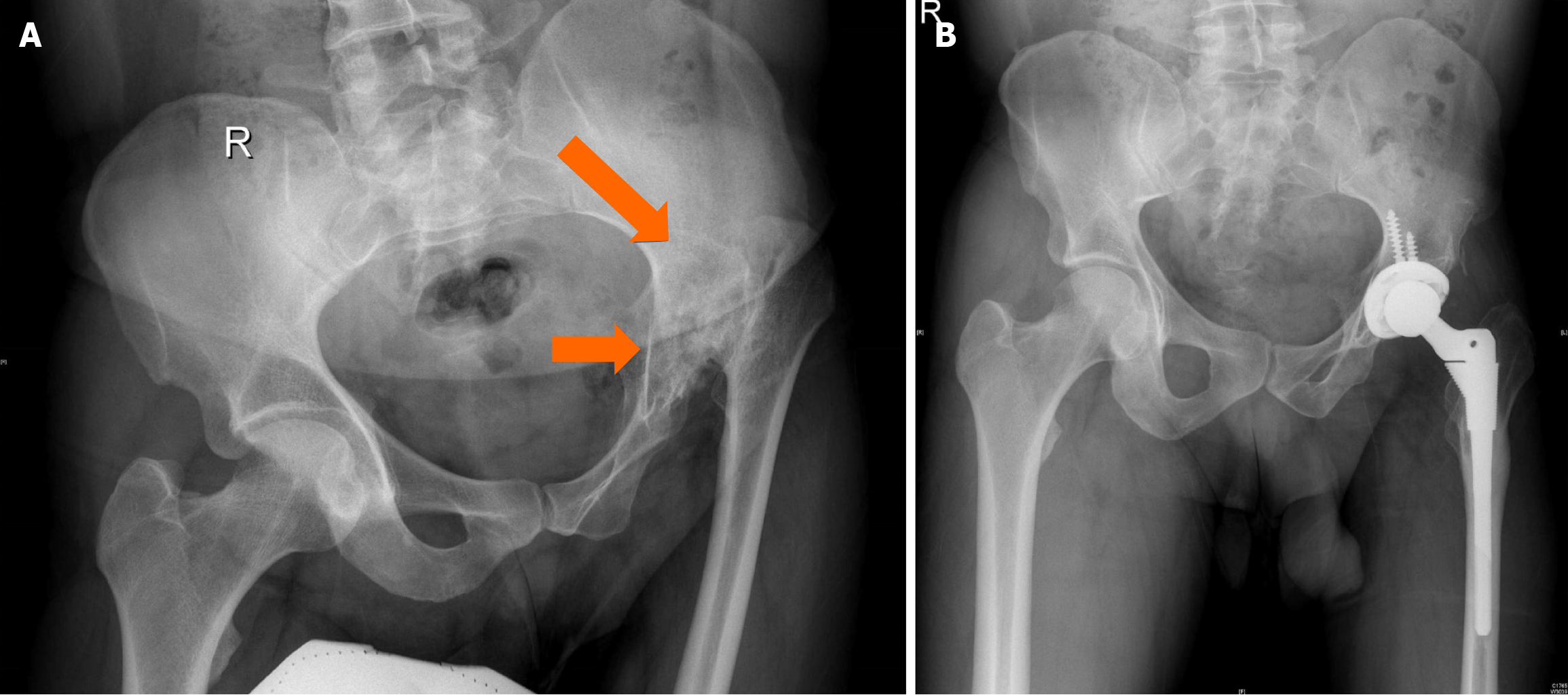
Preoperative examination and assessment need to be meticulous as there is often a history of several prior surgeries, multiple incisions, and significant soft tissue/skin scarring (Figure 1).
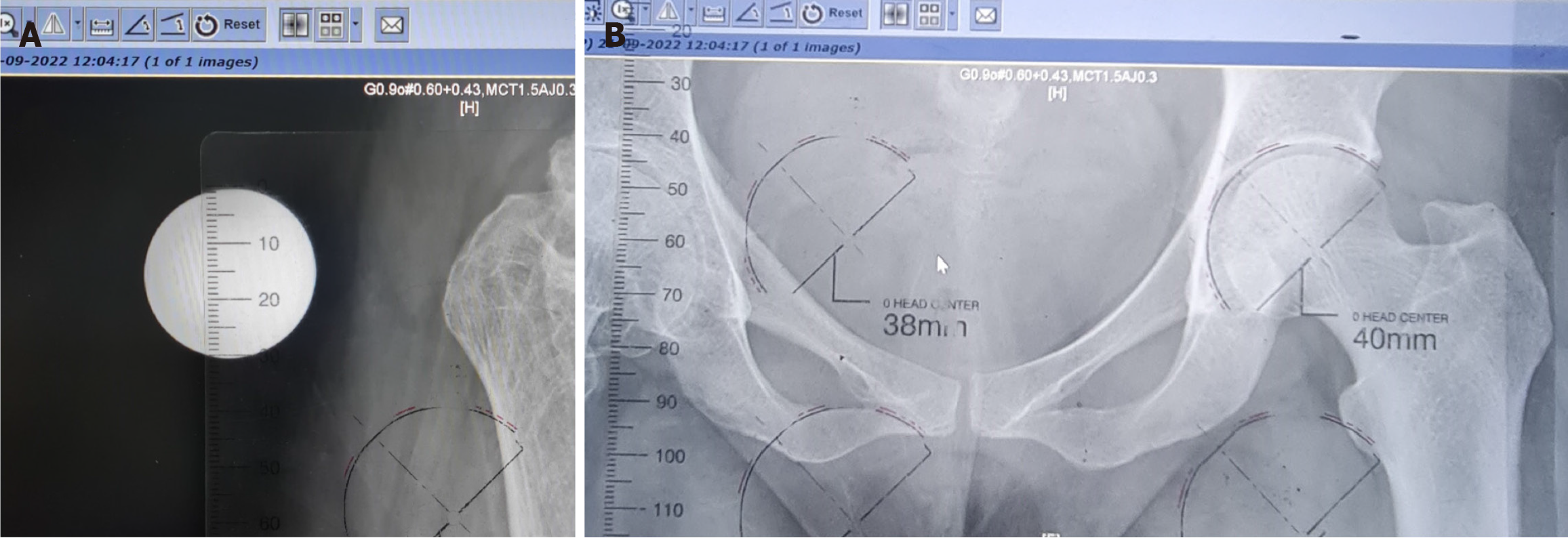
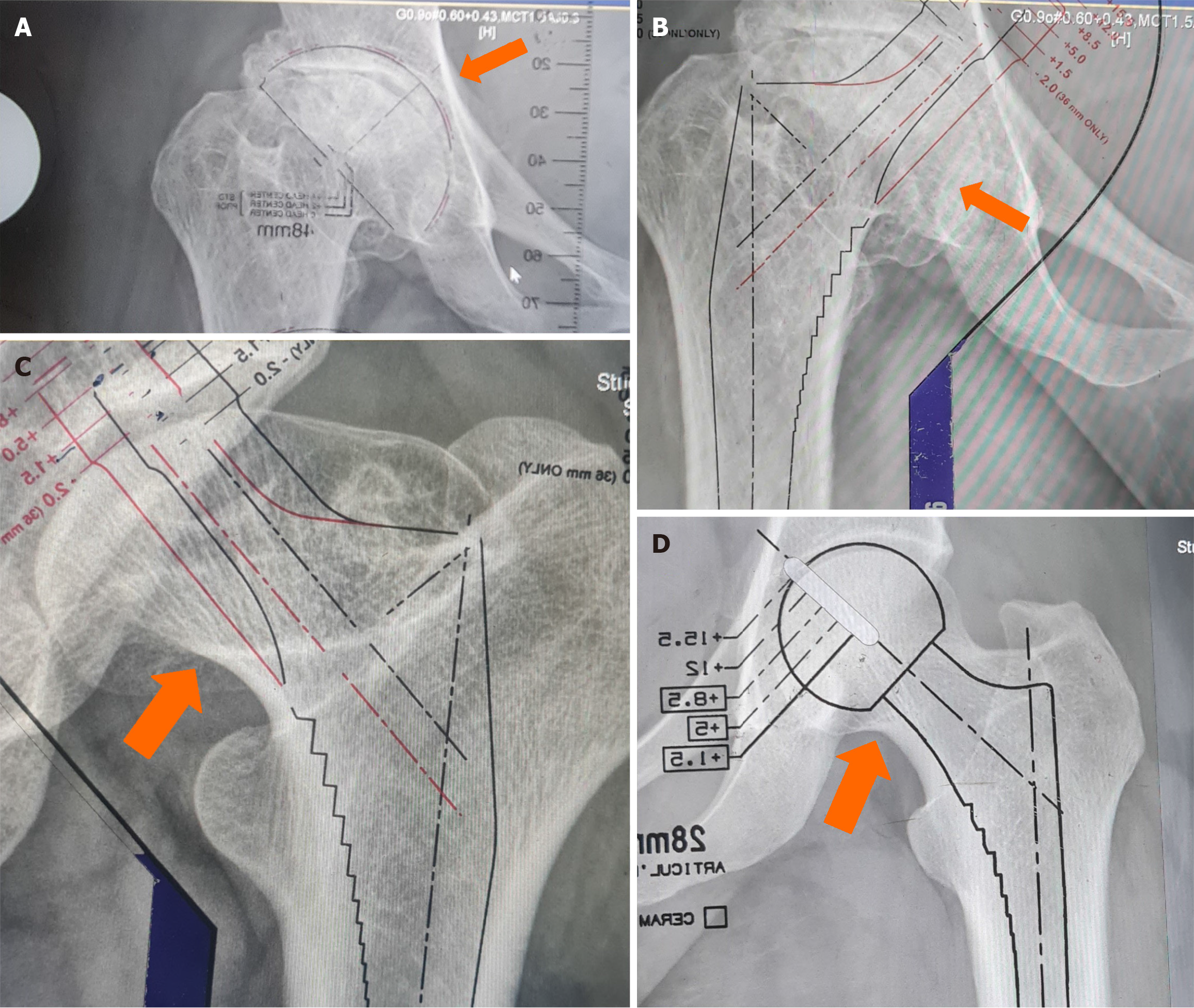
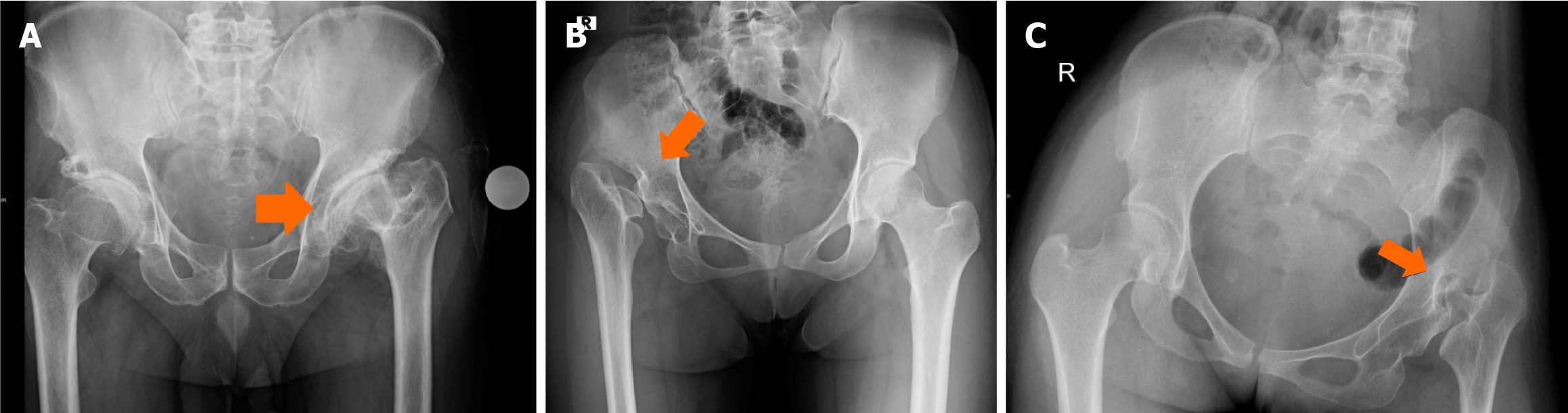
Templating provides essential information regarding the possible component sizes for the acetabulum and the femur. The horizontal offset and limb length discrepancy must be assessed to plan for various offset and neck length options for the proposed THA (Figures 2 and 3)[7,8]. Preoperative templating could be done using the magnification adjustments on any computer with digital X-ray viewing software[8]. Preoperative templating must be corroborated with intraoperative findings as most centres lack the availability of navigation or robotic technology.
Childhood disorders lead to improper development of the acetabular cavity, hemipelvis, and femoral canal[3,6]. Acetabular changes include small hypoplastic and ill-defined shallow cavities with thin anterior and posterior walls and possibly deficient AP and/or posteroinferior columns; the ilium itself is often also poorly developed. The acetabulum must be carefully templated and planned as the cup size may be small in diameter. Intraoperatively, the true acetabulum must be identified, which is done by placing a retractor in the obturator foramen. Intraoperative imaging is a powerful adjunct to confirm positioning before beginning to ream[1,3,6,9,10]. Reaming and preparation must be done judiciously after identifying the true acetabulum and assessing the anterosuperior and posteroinferior columns. The acetabular component needs careful sizing for the best fit, small component, and maximum preservation of bone stock. The acetabular shell should be secured with screws for immediate mechanical stability of the construct.
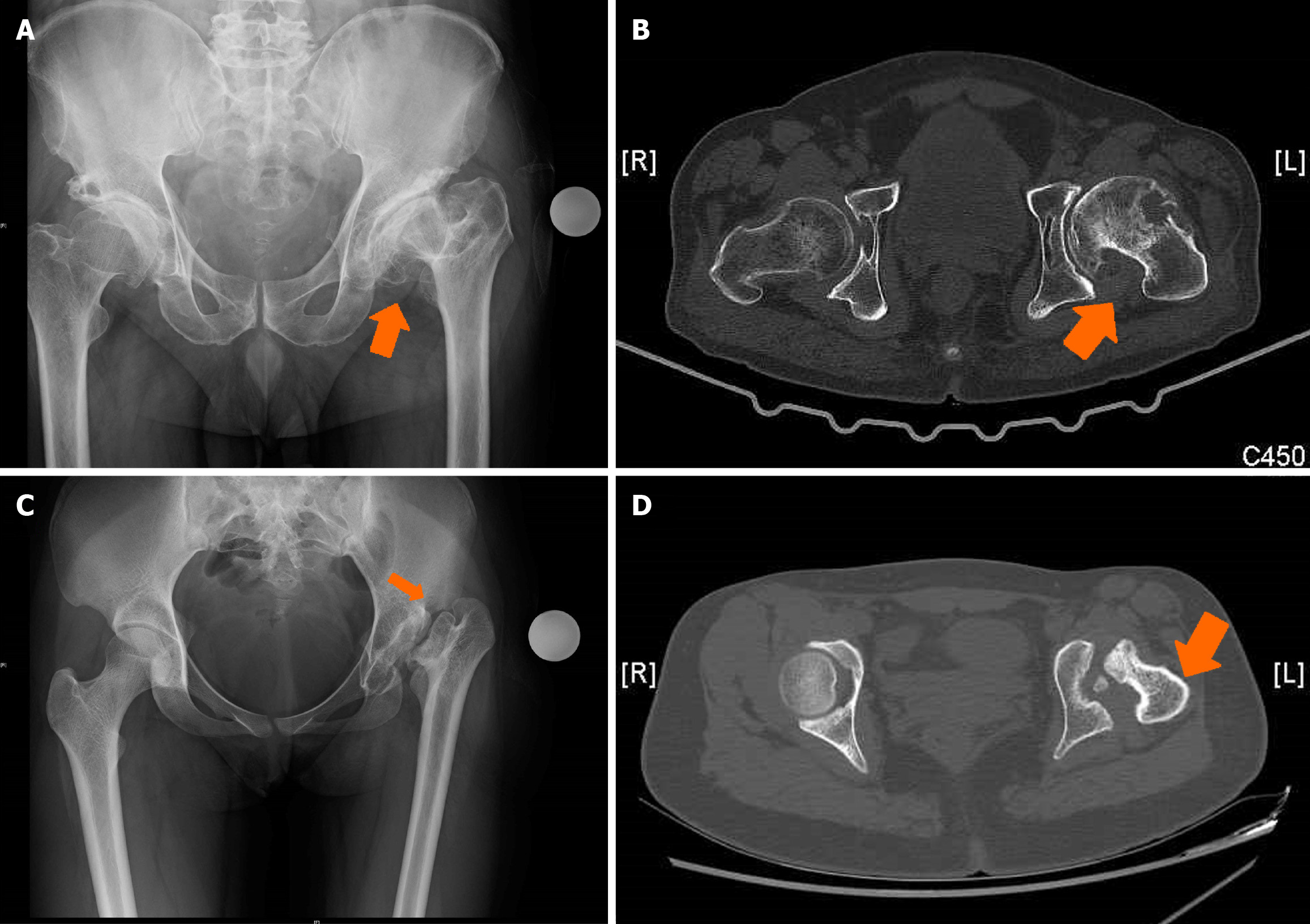
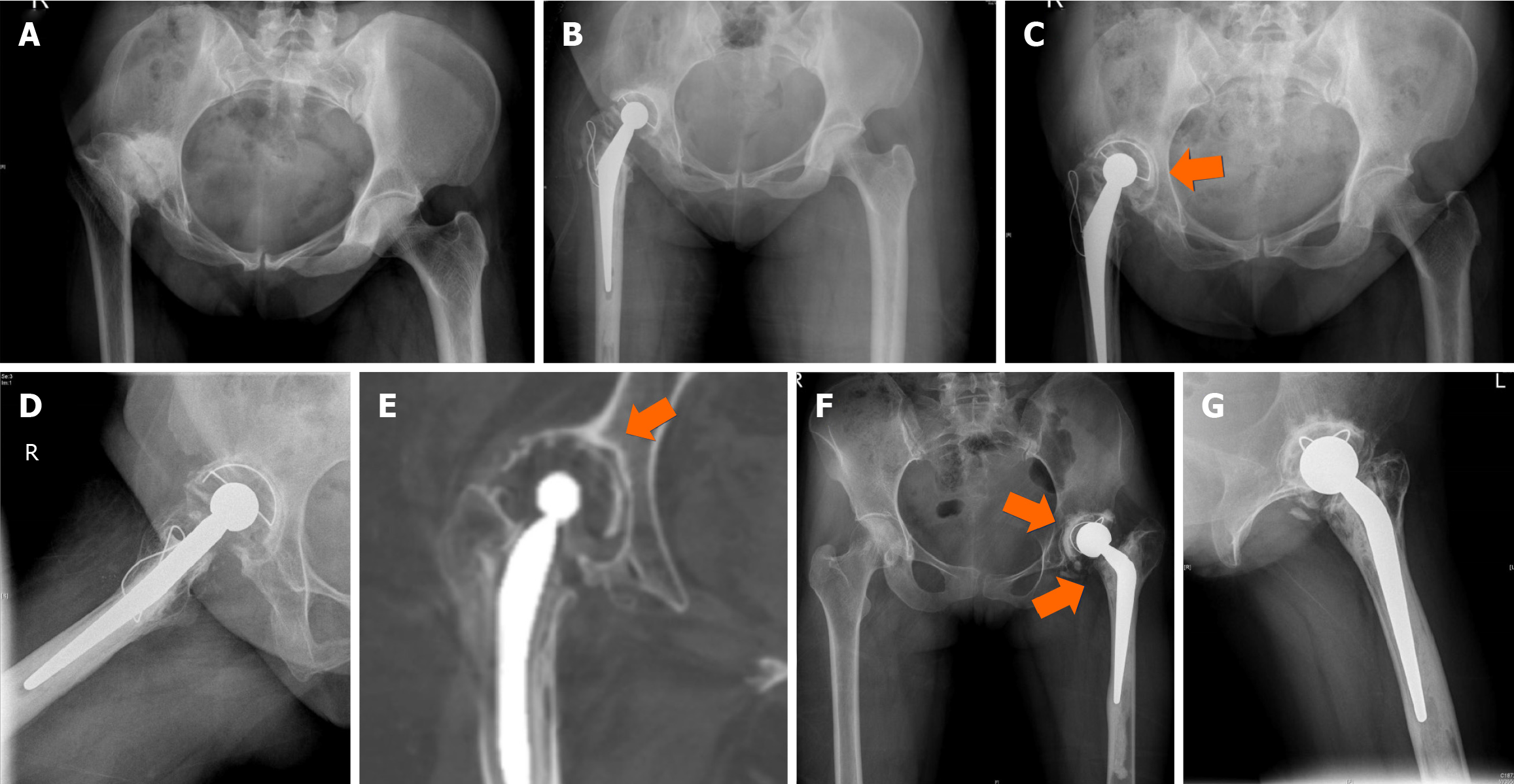
The femoral anatomical variations are changes in the femoral head, abnormalities in the neck, femoral anteversion (Figure 4), and metaphyseal changes with a meta-diaphyseal mismatch. The canal itself could be narrow with variable degrees of anterior and lateral bowing[6,9]. Prior childhood femoral lengthening procedures could pose challenges with femoral canal preparation, and reaming must be done with care for optimal size assessment (Figure 5).
The main components of the standard soft-tissue hip envelope are the iliofemoral ligament, which limits external rotation and extension; pubofemoral ligament, which limits abduction and external rotation; ischiofemoral ligament, restricting flexion, adduction and internal rotation; and the annular ligaments, contributes to stability in hip flexion and extension[7].
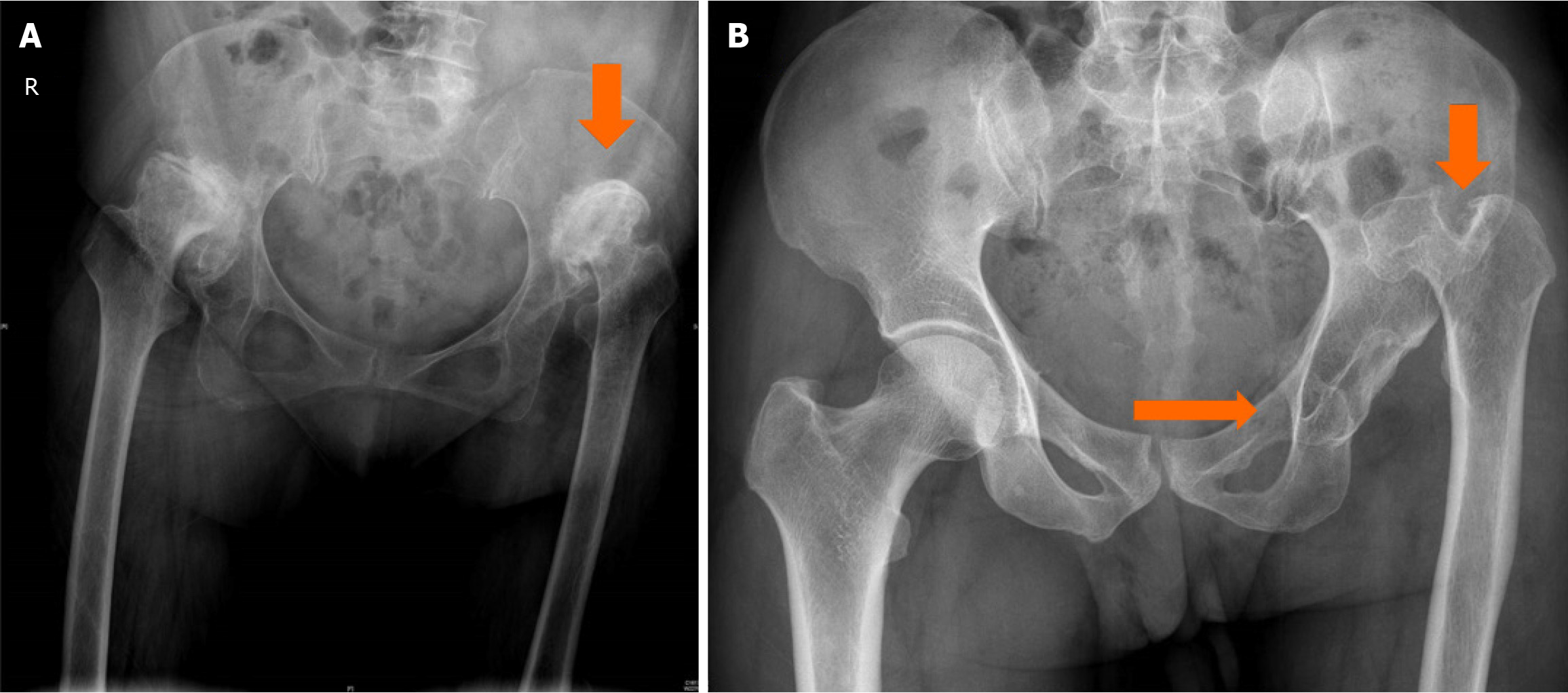
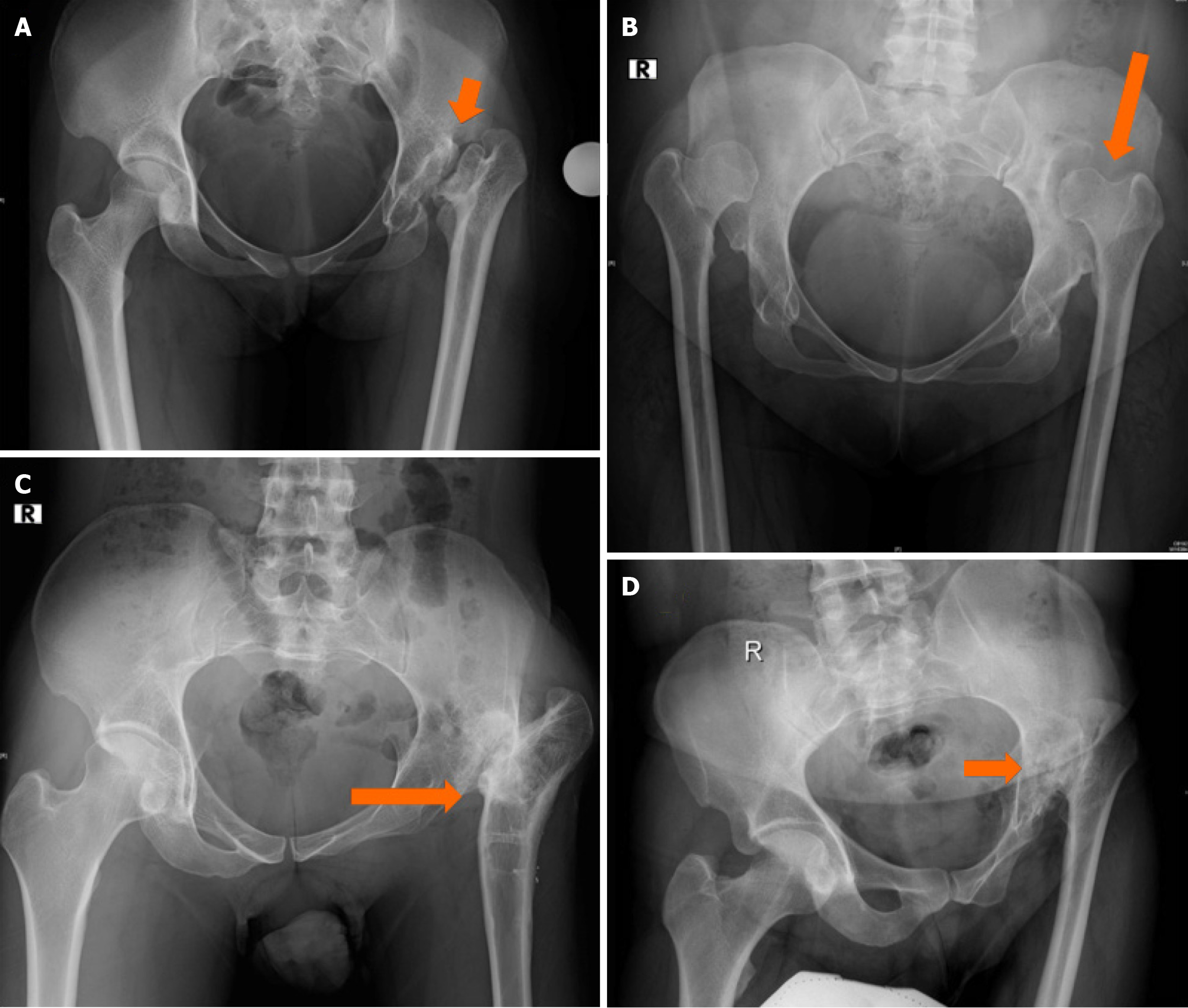
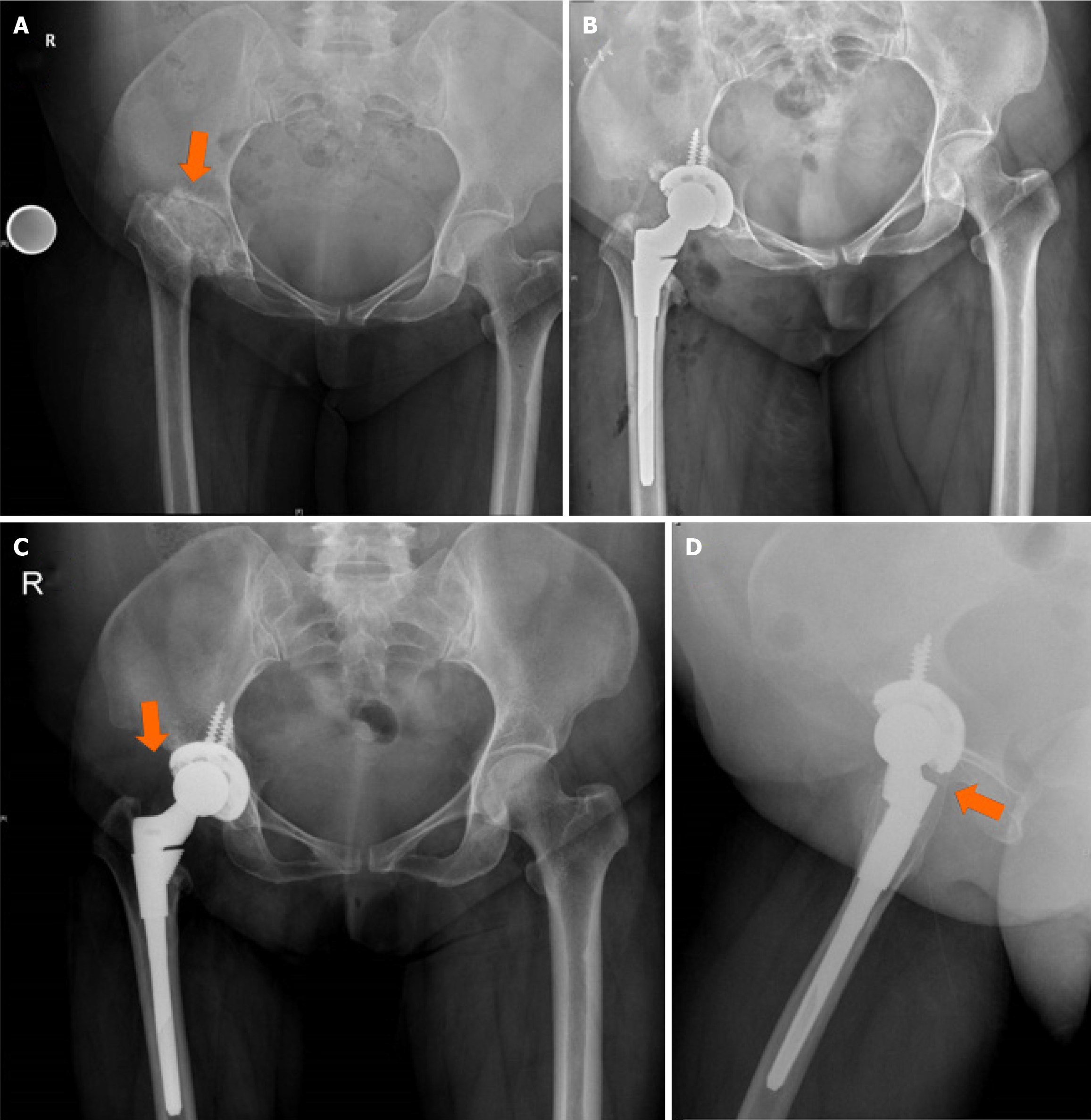
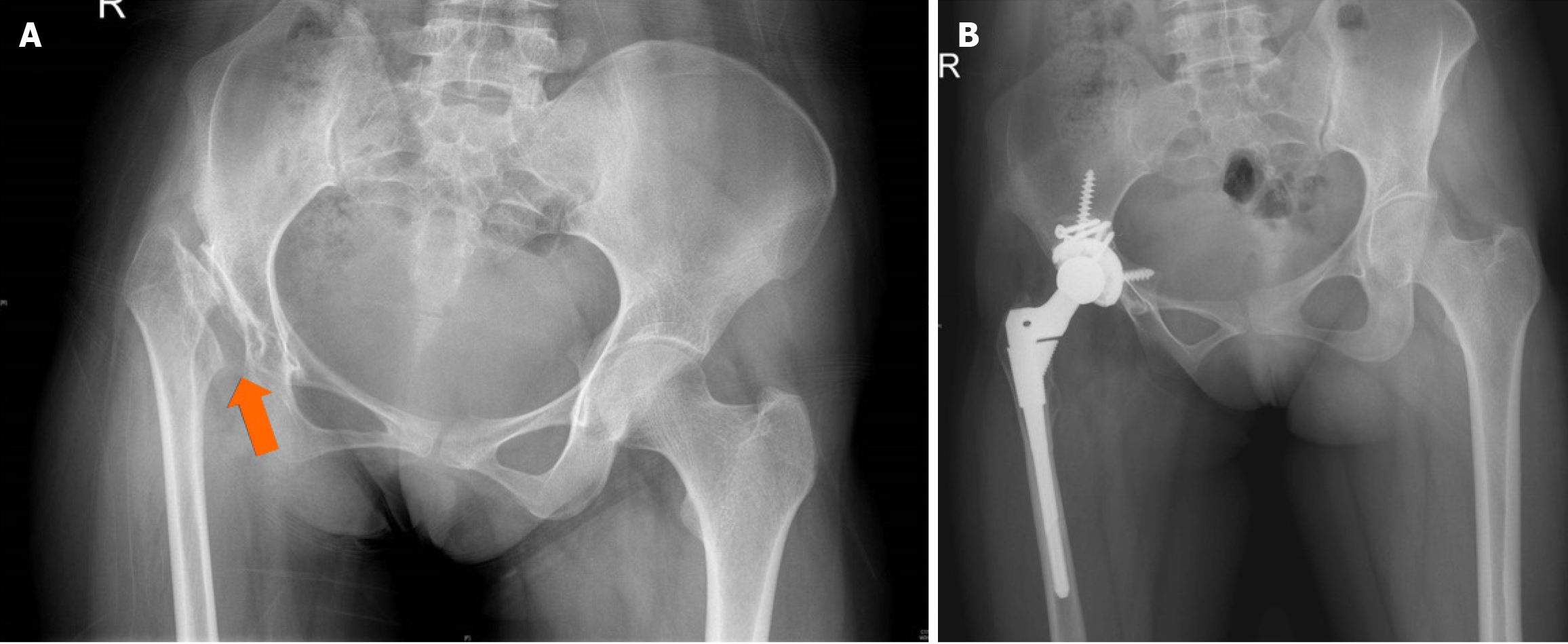
Planning for soft-tissue and capsular releases should be based on a thorough preoperative physical examination and radiographic assessment. Identifying and understanding the type of preoperative hip shortening is also critical in determining the probability of requiring a subtrochanteric shortening osteotomy. Shortening could be supratrochanteric, with the femoral head centre below the level of the greater trochanter and the lesser trochanter at the level of the inferior aspect of the teardrop (Figure 6)[7]. Shortening is described as infratrochanteric, with the relationship between the greater trochanter and the femoral head centre maintained while the lesser trochanter is above the level of the teardrop (Figure 7). Combined supratrochanteric and infratrochanteric shortening may also exist (Figure 8). Supratrochanteric shortening would require a low neck cut and concomitant soft-tissue releases with a short-neck stem with a low amount of femoral offset. A subtrochanteric shortening osteotomy is more commonly needed for infratrochanteric shortening and in cases with combined shortening[7].
The proximal migration of the femur would require extensive soft tissue and capsular release on the acetabular and femoral aspects to achieve restoration of the horizontal offset. Stable reduction with the restoration of the hip centre of rotation (COR) is usually achieved with a 360 release of the soft tissue and capsule, sparing the abductors. Subtro
Stability and optimal fixation of the osteotomy are ideally achieved with a modular stem. Modularity in the femoral component would be suitable for version adjustment, addressing the meta diaphyseal mismatch, and obtaining good proximal and distal fixation[9]. This will ensure optimal load distribution over the proximal and distal femur and prevent stress shielding.
Preparation and reaming of the femur must be done sequentially with caution as there is a high risk for calcar fractures or distal fractures due to osteoporosis, anatomic deformities and small calibre femoral canals. Fractures encountered intraoperatively require additional stabilisation with wiring or plate osteosynthesis and are progressed slowly with limi
Anatomical COR restoration is ideal to restore limb length, horizontal offset, and correct limb length discrepancy. The shortening and altered gait pattern with back pain are the common complaints on presentation in adulthood at THA.
Femoral shortening with modular stem fixation would necessitate protected weight bearing till complete union of the osteotomy.
The gait pattern would take a few months to stabilise, and these individuals are satisfied with restoring limb length and hip stability.
THA in childhood disorders ideally requires anatomical hip centre restoration to reproduce biomechanics, limb length, offset and increased survivorship. The risk of dislocation or instability in these hips would be low, particularly with anatomical hip centre restoration. High hip centre with lateralisation could lead to early symptomatic loosening requiring revision. Although hip centre elevation up to 1 cm has shown good long-term survivorship, it would be ideal to attempt native anatomic hip centre restoration in these hips[11,12].
Sequelae of developmental dysplasia of the hip (DDH) are among the most common childhood disorders requiring THA in adulthood. The initial retroversion of the femur neck during early development gradually leads to varying degrees of excessive anteversion in these hips. Coxa valga with narrowing of the medullary canal at the isthmus and reduction of the external medullary diameter are typical of the dysplastic hip[6]. The medullary flare is lost with poor femur development, a narrow medullary canal, and decreased canal size. Awareness regarding the mismatch of the diaphysis and metaphysis is essential and would necessitate using modular stems for optimal stability, fit, and long-term survivorship[9]. The Crowe classification would help preoperative planning for soft tissue release and implant option requirements for THA[10,13,14] (Table 1).
| Crowe type | Description |
| Type 1 | < 50% of the vertical diameter of the femoral head; < 10% of the height of the pelvis |
| Type 2 | 50%–75% of the vertical diameter of the femoral head; 10%–15% of the height of the pelvis |
| Type 3 | 75%–100% of the vertical diameter of the femoral head; 15%–20% of the height of the pelvis |
| Type 4 | > 100% of the vertical diameter of the femoral head; 20% of the height of the pelvis |
Acetabular changes vary from malposition due to superolateral translation, version, size variation and incongruity[6]. The distortion could occur in both AP and transverse planes, with the changes well seen in preoperative CT evaluation.
The high hip centre has been advocated for Crowe 2 or 3 hips; however, restoration of the anatomical hip centre would be preferred for restoration of normal biomechanics and good long-term outcome (Figure 10)[11,12].
Soft tissue contractures would be significant, especially with high-riding hips and considerable shortening. Careful soft tissue balancing combined with subtrochanteric shortening to restore the hip centre would reduce the risk of neurological injury in these high hips with combined supra and infra trochanteric shortening (Figure 11)[6,7].
Perthes disease is characterised by femoral head distortion, gradual deformation, and collapse with limb shortening. Limb length discrepancy is not as significant as seen with DDH. Adults present with decreased movement and increasing pain with functional disability.
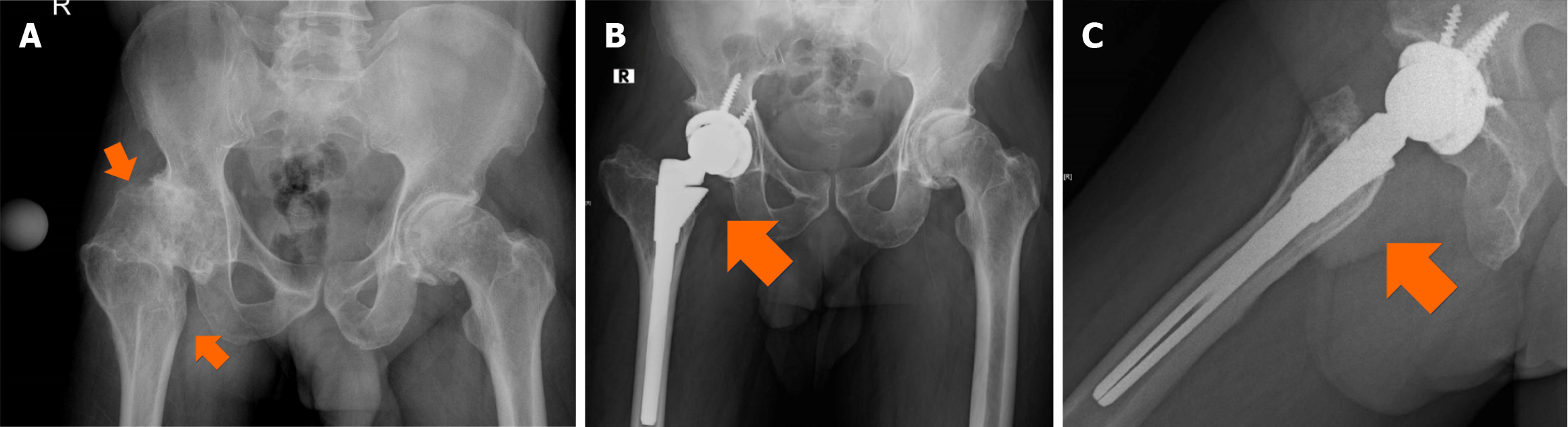
The common abnormalities in Perthes sequelae include a large femoral head, often below the level of the greater trochanter and an oblong acetabulum (Figure 12)[6]. Version changes in the femur are expected and must be identified[1,5,15].
Approach and surgical exposure should consider soft tissue releases to fully visualise the acetabulum before initiating reaming to restore the hip COR. Judicious reaming is ensured to avoid eccentric reaming of the walls and correct medialisation after removal of the medial osteophyte. Gradual sequential reaming is advocated for good column capture of the acetabular component. Care is taken not to oversize the acetabular component using pre-operative templating as a guide. The osteophytes are removed around the margins of the acetabulum to prevent impingement after the actual implant is stabilised with screws if required.
The femur is carefully prepared to ensure cortical contact and recognition of any meta-diaphyseal mismatch that could be encountered in Perthes disease. Femoral components could be monobloc or modular as the femoral and acetabular version must be carefully adjusted. Primary femur implants are available with short, standard, and high offset options, and the short neck option is often required in these hips to reproduce the native offset assessed in the contralateral normal hip.
Care is taken to achieve optimal fit and stability. The limb length, offset, and combined anteversion are checked after trial reduction, considering the preoperative and intraoperative templating. Femoral version assessment and restoration is essential, and this has been achieved well with standard or short stems[2,5,15]. Hip resurfacing has been described in Perthes, where distortion is not significant[16]. The direct anterior approach has also achieved promising results in hips with Perthes disease[17].
Slipped capital femoral epiphysis sequelae present in adulthood with distortion of the femoral head may be compli
High riding hips due to postseptic sequelae in childhood present for THA in the fourth or fifth decade with pain, shortening, and a persistent limp. The challenges include soft-tissue scarring, shortening and poorly developed acetabulum[4]. Distal reattachment of the greater trochanter with the abductor has been described earlier to optimise abductor length and function. The high-riding hips would require extensive soft-tissue release and restoration of the COR. Subtrochanteric shortening osteotomy for these high-riding hips with combined supratrochanteric and infra
Containment procedures for the hip are standard practice for dysplastic hips with femoral and acetabular procedures. Femoral correction includes varus derotation osteotomy, valgus osteotomy, and femoral lengthening, which could distort the distal femoral canal. Proximal femur preparation would have to be done with care in hips with altered anatomy due to prior osteotomies (Figures 4 and 12).
Previous acetabular procedures like Chiari osteotomy have improved bone stock for THA. Literature regarding THA after acetabular procedures for childhood hip disorders is limited; however, 5-year survivorship seems good[6].
Restoration of native hip centre and limb length would be ideal. High hip centre with lateralisation can lead to sympto
Femoral nerve palsy (1 out of 20) and dislocation (2 out of 20) have been reported following THA with femoral shortening in severely dysplastic hips[4]. Femoral palsy had recovered, and dislocations were treated by closed reduction with no recurrence[4].
Intraoperative fractures have been reported due to abnormal anatomy (11%–17%) and neurological injury in 3% in a review of literature for THA in Perthes disease[5].
Cemented THA revision rates in dysplastic hips seem to have a slightly increased revision rate (3.3% higher than other groups, with a failure rate of 40% at 25 years)[6]. Acetabular loosening seems to be the leading cause for revision, probably due to the altered anatomy in the dysplastic hips[6]. THA survivorship for high hips has been reported to be 78% at 20 years follow-up[4]. Dislocation rates appear low in these high-riding hips after THA, probably due to hip centre restoration. An overall revision rate of 7% at 7.5 years due to aseptic loosening has been documented for THA in Perthes disease sequelae[5]. Survivorship of 90%–95% has been reported for cementless THA in Perthes disease[2]. An average follow-up of 3.3 years (0.7–10 years) reported good outcomes in another small series with 10 patients who underwent THA for childhood arthritis sequelae[20]. Heterotopic ossification and infection are complications that do occur, with excellent survivorship in THA for postseptic sequelae[13,18]. Recent data suggest good outcomes and survival[3].
THA for sequelae to childhood disorders is challenging. Anatomical variations in the acetabulum and femur need careful assessment to plan and restore the anatomical hip COR. Scarring and bony changes from childhood infection or previous surgical procedures must be considered during exposure and reconstruction. Distortion in the anatomy and preservation of native bone stock must be considered during preoperative templating. Having a high suspicion for need of a subtrochanteric shorterning osteotomy allows for more efficient intraoperative execution of the preoperative plan. Adequate exposure, soft-tissue releases, and implant option availability for offset and neck length are needed to restore the hip COR and recreate native hip biomechanics.
| 1. | Anthony CA, Wasko MK, Pashos GE, Barrack RL, Nunley RM, Clohisy JC. Total Hip Arthroplasty in Patients With Osteoarthritis Associated With Legg-Calve-Perthes Disease: Perioperative Complications and Patient-Reported Outcomes. J Arthroplasty. 2021;36:2518-2522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Baghdadi YM, Larson AN, Stans AA, Mabry TM. Total hip arthroplasty for the sequelae of Legg-Calvé-Perthes disease. Clin Orthop Relat Res. 2013;471:2980-2986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Te Velde JP, Buijs GS, Schafroth MU, Saouti R, Kerkhoffs GMMJ, Kievit AJ. Total Hip Arthroplasty in Teenagers: A Systematic Literature Review. J Pediatr Orthop. 2024;44:e115-e123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Park KS, Yoon TR, Song EK, Seon JK, Lee KB. Total hip arthroplasty in high dislocated and severely dysplastic septic hip sequelae. J Arthroplasty. 2012;27:1331-1336.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Hanna SA, Sarraf KM, Ramachandran M, Achan P. Systematic review of the outcome of total hip arthroplasty in patients with sequelae of Legg-Calvé-Perthes disease. Arch Orthop Trauma Surg. 2017;137:1149-1154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Gent E, Clarke NM. Joint replacement for sequelae of childhood hip disorders. J Pediatr Orthop. 2004;24:235-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 7. | Boe RA, Selemon NA, Eachempati KK, Paprosky WG, Sheth NP. Soft-Tissue Balancing in Total Hip Arthroplasty. JBJS Rev. 2021;9:e20.00116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Krishnamoorthy VP, Perumal R, Daniel AJ, Poonnoose PM. Accuracy of templating the acetabular cup size in Total Hip Replacement using conventional acetate templates on digital radiographs. J Clin Orthop Trauma. 2015;6:215-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Christie M, Brinson MF. Proximal/distal mismatch: type A and C femurs. Orthopedics. 2005;28:s1033-s1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15-23. [PubMed] |
| 11. | Nawabi DH, Meftah M, Nam D, Ranawat AS, Ranawat CS. Durable fixation achieved with medialized, high hip center cementless THAs for Crowe II and III dysplasia. Clin Orthop Relat Res. 2014;472:630-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Kannan A, Madurawe C, Pierrepont J, McMahon S. Does total hip arthroplasty with high hip centre in dysplasia compromise acetabular bone stock? Hip Int. 2023;33:518-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Qian Z, Mamtimin A, Zhang X, Xu B, Mu W, Cao L. Mid-Term Outcomes of Cementless Total Hip Arthroplasty in Adult Patients with Childhood Hip Infection. Med Sci Monit. 2021;27:e930760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Jawad MU, Scully SP. In brief: Crowe's classification: arthroplasty in developmental dysplasia of the hip. Clin Orthop Relat Res. 2011;469:306-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Lee KH, Jo WL, Ha YC, Lee YK, Goodman SB, Koo KH. Total hip arthroplasty using a monobloc cementless femoral stem for patients with childhood Perthes' disease. Bone Joint J. 2017;99-B:440-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Su EP, Morgenstern R, Khan I, Gaillard MD, Gross TP. Hip resurfacing arthroplasty for end-stage arthritis caused by childhood hip disease. Hip Int. 2020;30:572-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Hasler J, Flury A, Hoch A, Cornaz F, Zingg PO, Rahm S. Total hip arthroplasty through the direct anterior approach for sequelae of Legg-Calvé-Perthes disease. Arch Orthop Trauma Surg. 2023;143:5935-5944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 18. | Malhotra R, Batra S, Sugumar PA, Gautam D. Clinical outcome in total hip arthroplasty for septic sequelae in childhood: a retrospective study. Bone Jt Open. 2022;3:314-320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 19. | Oommen AT, Chandy VJ, Jeyaraj C, Kandagaddala M, Hariharan TD, Arun Shankar A, Poonnoose PM, Korula RJ. Subtrochanteric femoral shortening for hip centre restoration in complex total hip arthroplasty with functional outcome. Bone Jt Open. 2020;1:152-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Luceri F, Morelli I, Sinicato CM, Della Grazia A, Verdoni F, Maffulli N, Peretti GM, Curci D. Medium-term outcomes of total hip arthroplasty in juvenile patients. J Orthop Surg Res. 2020;15:476. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |