Published online Jul 18, 2024. doi: 10.5312/wjo.v15.i7.635
Revised: May 30, 2024
Accepted: June 18, 2024
Published online: July 18, 2024
Processing time: 127 Days and 16.2 Hours
Clubfoot, or congenital talipes equinovarus, is a widely recognized cause of disability and congenital deformity worldwide, which significantly impacts the quality of life. Effective management of clubfoot requires long-term, multidisciplinary intervention. It is important to understand how common this condition is in order to assess its impact on the population. Unfortunately, few studies have investigated the prevalence of clubfoot in Saudi Arabia.
To determine the prevalence of clubfoot in Saudi Arabia via the patient population at King Fahad University Hospital (KFUH).
This was a retrospective study conducted at one of the largest hospitals in the country and located in one of the most densely populated of the administrative regions.
Of the 7792 births between 2015 to 2023 that were included in the analysis, 42 patients were diagnosed with clubfoot, resulting in a prevalence of 5.3 per 1000 live births at KFUH.
The observed prevalence of clubfoot was significantly higher than both global and local estimates, indicating a substantial burden in the study population.
Core Tip: Clubfoot, or congenital talipes equinovarus, is a congenital deformity with global impact, but comprehensive prevalence data for Saudi Arabia are lacking. This study at King Fahad University Hospital aimed to address this gap by analyzing 7792 births that occurred between 2015 and 2023. The analysis revealed a prevalence of 5.3 per 1000 live births, which is higher than global estimates and indicates a substantial burden. The findings emphasize the urgency of targeted interventions to address clubfoot in the Eastern Province of Saudi Arabia.
- Citation: Alomran AK, Alzahrani BA, Alanazi BS, Alharbi MA, Bojubara LM, Alyaseen EM. Prevalence and associated factors of clubfoot in the eastern province of Saudi Arabia: A hospital-based study. World J Orthop 2024; 15(7): 635-641
- URL: https://www.wjgnet.com/2218-5836/full/v15/i7/635.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i7.635
Congenital talipes equinovarus (CTEV), often called clubfoot, is a congenital condition characterized by cavus, adductus, varus, and equinus deformities of the leg. CTEV was first observed by Hippocrates in 300 BC[1]. It is one of the most frequently encountered foot abnormalities, and it can be seen immediately after birth[2]. CTEV patients have been known to have certain tibial and tarsal bone anatomical abnormalities, including mispositioned tarsal bones that result in high metatarsal bone flexion, increased planter arch curvature, equines foot with inverted, adducted calcaneus due to posteromedial foot ligament contracture, calf muscle atrophy, and foot shortening. There are no histologic or electric abnormalities[3,4]. In 80% of cases, it presents by itself as an isolated malformation. It may present as syndromic CTEV secondary to other congenital anomalies such as spina bifida (myelomeningocele), arthrogryposis, or dystrophic dwarfism. That increases the risk of morbidity, mortality, and resistance to treatment[5,6].
CTEV can be a bilateral or unilateral deformity, with the right leg more commonly affected[2]. Despite extensive epidemiological, clinical, and basic science research, the etiology of club foot remains unclear. Most of investigations suggest a genetic component is involved, but that is inconsistent with the Mendelian inheritance pattern. Several studies have observed that CTEV was associated with deletion of CASP10, an apoptosis regulatory gene on chromosome 2 (2q31-33)[7]. Other suggested causes include abnormalities of joint and/or bone formation, uterine restriction (oligohydramnios), and neurological and vascular abnormalities that occur in the second trimester of pregnancy[1,8]. Numerous studies have reported male sex, maternal age, maternal smoking, maternal marital status, maternal education, and maternal diabetes as associated with increased risk of CTEV[9].
Classification of CTEV is essential to score the severity of CTEV at birth and to assess the outcome of treatment. While several classification systems have been developed in the last 50 years[10], the Dimeglio scale and Pirani score are the most commonly used clinical systems to assess the severity of CTEV[11]. Prognosis depends on associated conditions but is generally excellent for cases of isolated CTEV[12]. Conservative nonsurgical treatments include manipulation and casting. Surgical techniques include soft tissue release and bone procedures[11]. However, conservative management is widely accepted due to the high risk of post-surgical complications[12]. Conservative treatments include the Kite method, physiotherapy, and the Ponseti method. The Ponseti method has recently been recognized as the most effective treatment with minimal complications in both isolated and syndromic cases, including idiopathic or syndromic comorbidities[6,11]. Inadequate treatment of CTEV can lead to lifelong disabilities, chronic pain, and limited opportunities for education and employment[13], King Faisal street[14].
The incidence and prevalence of CTEV vary with race and ethnicity. Globally, there are 0.6-1.5 cases of CTEV per 1000 live births per year, with a total of 150000 infants being affected annually. CTEV is thus one of the most common birth defects in children. Bilateral CTEV occurs in approximately 50% of cases, with a male-to-female ratio of 2:1[4,15,16]. Kruse et al[17] described the sex difference as the Carter effect, with girls having more predisposing genes than boys and the ability to transmit them to their offspring. About 80% of CTEV cases have been reported in low-middle income countries[2] and CTEV is estimated to affect 2.3/1000 (0.23%) of Saudis visiting King Saud Medical City[18]. In order to understand the impact and burden of CTEV on the population, it is important to determine its prevalence. Unfortunately, few studies have been conducted on the prevalence of CTEV in Saudi Arabia.
This study investigated the prevalence of CTEV in the Eastern Province of Saudi Arabia, with a specific focus on King Fahad University Hospital (KFUH). The goal was to better understand the prevalence of this condition in this country. The findings of the study increase the understanding of CTEV and can help guide future interventions and healthcare planning.
Data was collected from patient medical profiles in the QuadraMed system (QuadraMed Corp., Plano, TX, United States) and the database at the KFUH Orthopedic Department.
The research was carried out at KFUH. With a capacity of 540 beds, it is the largest university hospital in the Eastern Province of Saudi Arabia. Saudi patients of both sexes who were diagnosed with CTEV between 2015 and 2023, had medical records with complete diagnostic and patient information, and were 0-5 years of age, were eligible to participate in this study. We conducted a comprehensive evaluation that included all instances of isolated CTEV as well as those accompanied by additional idiopathic or syndromic comorbidities.
This was a retrospective, descriptive, cross-sectional study. This design was chosen because its analytical data capabilities suit the purpose of this study.
The sample was assessed by examining medical files included in a list provided by the orthopedic department’s database and the QuadraMed program at KFUH. There were 42 cases of CTEV, 38 of which had been born in the hospital. Four cases had been born in the Maternal and Child Hospital, which is a part of the University Hospital and is located near the main building. Thirty-nine of the cases were diagnosed clinically by physical examination and three were identified by prenatal ultrasonography. The diagnosis was primarily by physical examination that identified CTEV deformities including midfoot cavus, forefoot adduction, and hindfoot equinus and valgus.
Following approval by the hospital’s Institutional Review Board, the required data were obtained from medical files by a medical student who was supervised by two orthopedic physicians from KFUH.
The study results were reported as frequencies and percentages and the analysis were performed with Statistical Package for the Social Sciences version 20 (IBM Corp., Armonk, NY, United States).
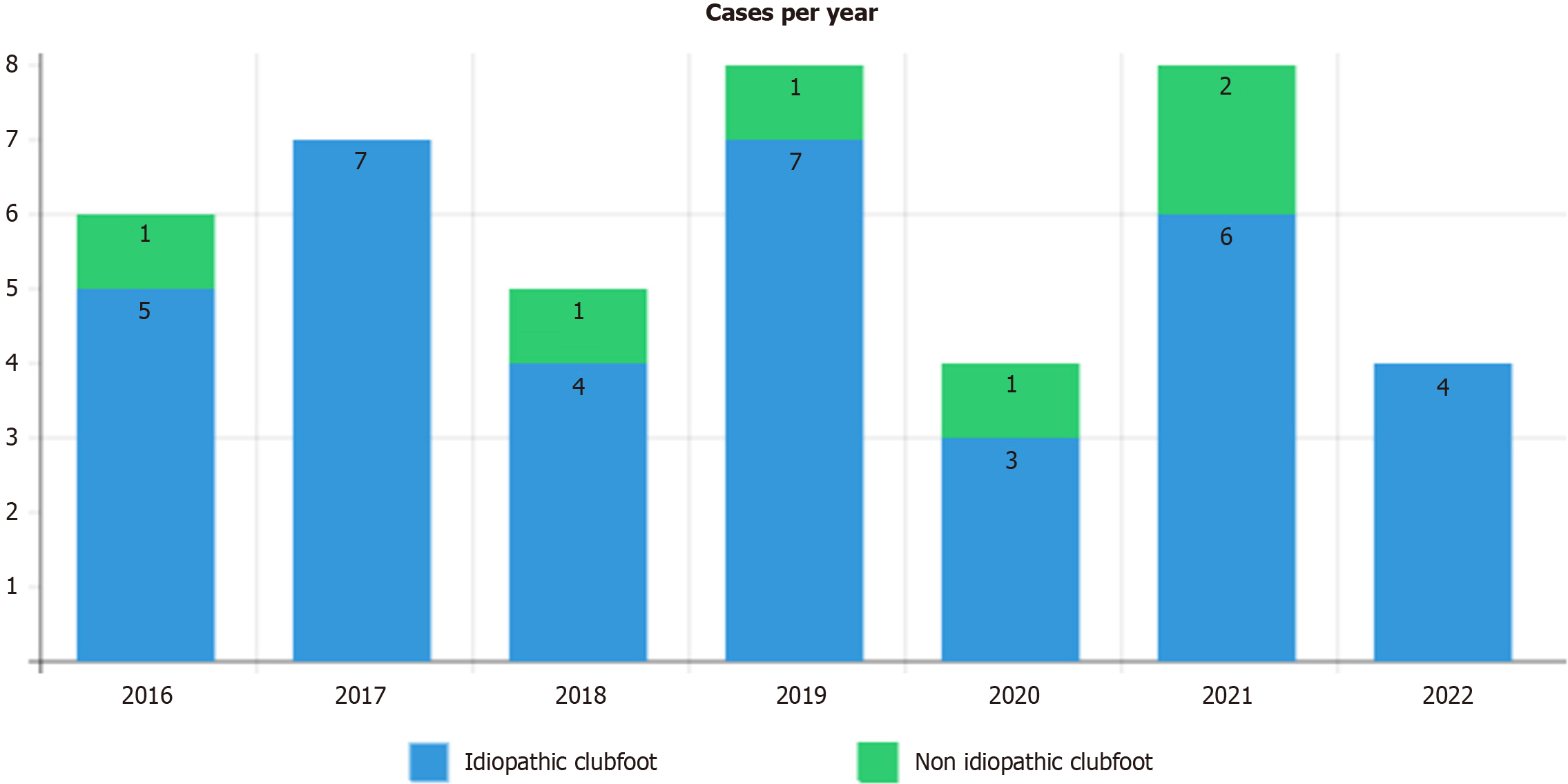
A total of 7792 births at KFUH between 2015 and 2023 were included in the analysis. CTEV was diagnosed in 42 children, resulting in a prevalence of 5.3 per 1000 live births. The male-to-female ratio was 2.23:1.00 with 69% male and 31% female patients. The epidemiological description of CTEV was obtained from data on these 42 cases that was collected by the Orthopedics Department at KFUH. Table 1 describes the characteristics of the patients and Table 2 lists the associated medical conditions. Stacked bar charts in Figure 1 were used to outline the frequencies of idiopathic and non-idiopathic CTEV from 2016 to 2022. There were no cases in 2015 and 2023.
| Characteristic | Total, n = 42 |
| Sex | |
| Male | 29 (69.0) |
| Female | 13 (31.0) |
| Clubfoot | |
| Bilateral | 27 (64.3) |
| Unilateral | 15 (35.7) |
| Right | 8 (19.0) |
| Left | 7 (16.7) |
| Developmental dysplasia of the hip | |
| Yes | 4 (9.5) |
| No | 38 (90.5) |
| Maternal history of chronic disease | |
| Diabetes mellitus | 1 (2.4) |
| None | 41 (97.6) |
| Associated medical condition | Total, n = 42 |
| Arthrogryposis | 3 (7) |
| Hydrocephalus | 3 (7) |
| Myelomeningocele | 3 (7) |
| Undescended testicle | 2 (4) |
| Sacrococcygeal teratoma | 1 (2) |
| Spina bifida | 1 (2) |
| Congenital insensitivity to pain syndrome | 1 (2) |
| None | 28 (67) |
A multiple regression analysis was conducted to examine the association of various demographic and clinical parameters and the occurrence of CTEV. The outcomes revealed several significant predictors. Initially, the presence of maternal chronic illness (β coefficient = 0.02 and P = 0.45) and familial predisposition to CTEV (β coefficient = 0.08 and P = 0.29) were not significantly predictive. Developmental dysplasia of the hip (DDH) (β coefficient = 0.31 and P < 0.001) was significantly predictive of CTEV. In particular, CTEV occurrence was estimated to be 2.5-fold more likely in individuals with DDH than in those without DDH. Regarding the sidedness of CTEV, bilateral manifestation was significantly associated with the presence of DDH (β coefficient = 0.22 and P = 0.003). In addition, DDH was significantly associated with unilateral CTEV (β coefficient = 0.18 and P = 0.012). In the cohort presenting with associated ailments, arthrogryposis, hydrocephalus, myelomeningocele, undescended testicle, sacrococcygeal teratoma, spina bifida, and congenital insensitivity to pain syndrome, all emerged as noteworthy and significant prognosticators of CTEV onset, with varying β-coefficients and corresponding P values. Furthermore, the collective presence of these associated maladies explained a substantial proportion of the variance observed in CTEV occurrence (R2 = 0.45, F8,33 = 12.54, P < 0.001).
CTEV, or clubfoot, is one of the most common causes of disability and congenital deformity worldwide, and it significantly impacts quality of life. CTEV management requires long-term multidisciplinary intervention. Determining the prevalence of this condition is crucial for assessing the impact of CTEV in Saudi Arabia. The prevalence of CTEV in this birth cohort at KFUH in Saudi Arabia’s Eastern Province was 5-times higher than the global estimate. KFUH is one of the largest hospitals in one of the five most densely populated of the 13 administrative regions in Saudi Arabia.
As shown in this study, the prevalence of CTEV among 7792 births at KFUH was 5.3 per 1000 live births. This result is considerably different from findings of global and local studies. Of the 42 CTEV patients, 7 required surgical intervention owing to a late diagnosis, which is often made after the 1st year of life. At the 5-year follow-up, both the surgically treated and conservatively treated cohorts had similar functional outcomes, including walking age, walking distance, athletic participation, stair climbing ability, and foot pain complaints. Table 3 presents a detailed comparison of the clinical results between patients with clubfoot who underwent surgical intervention and those who underwent conservative treatment. The analysis did identify significant risk factors within the cohort. Parental consanguinity was present in 36 cases. Prolonged labor, exceeding the standard duration of 24 hours, was noted in 33 cases. Breech presentation occurred in 17 cases. Additionally, 28 cases had associated neuromuscular syndromes, as previously detailed. Table 4 highlights these risk factors and their significance. A 2017 estimate of the average global prevalence of CTEV in children less than 5 years of age was 0.9 per 1000 live births, or 675061 cases in a population of 675100000 children[13]. Asia had the highest CTEV prevalence[13]. A study of the prevalence of CTEV in Europe in 2019 estimated that it was 1.13 per 1000 live births[18]. Our study findings revealed a prevalence approximately 5-times higher than the global estimate. A previous study in Saudi Arabia also reported that the overall rates and incidence of congenital disease and malformation were above average compared to the other parts of the world[19]. The high incidence of CTEV is probably related to the high rate of consanguineous marriage, which others have shown to contribute to the prevalence and risk of CTEV. A previous study found that in 31% of the CTEV cases, the parents were related (i.e., first- or second-degree cousins)[15]. In Turkey, where consanguineous marriages are frequent, studies have demonstrated that children born to first-cousin parents had a significantly increased prevalence of CTEV, with a risk of idiopathic CTEV that was over 4-times higher than the average[20,21]. However, a study conducted in China, where consanguinity is uncommon, found a prevalence of 4.27-7.00 per 1000 live births[22]. A hospital-based study conducted in Riyadh, Saudi Arabia with a sample size of 18515 births found a prevalence of 2.2 per 1000 live births[15]. Studies in China and the United States reported prevalences of congenital CTEV in male and female babies of 5.31 and 4.30 per 10000 births, respectively[22,23]. In our study the male-to-female ratio of 2.23:1.00 indicated that male sex was associated with the risk of CTEV in this birth cohort.
| Clinical outcome | Surgical treatment (mean ± SD) | Conservative treatment (mean ± SD) | P value |
| Walking age (months) | 15 ± 3 | 16 ± 4 | 0.01 |
| Walking distance (meters) | 500 ± 50 | 480 ± 70 | 0.02 |
| Athletic participation | 80% | 75% | 0.02 |
| Stair climbing ability | Good | Good | 0.01 |
| Foot pain complaint | 30% | 27% | 0.02 |
| Risk factor | Number of cases | SD | P value |
| Parental consanguinity | 36 | 4.2 | 0.045 |
| Prolonged labor (> 24 hours) | 33 | 3.9 | 0.021 |
| Breech presentation | 17 | 2.8 | 0.072 |
| Presence of neuromuscular conditions | 28 | 4.0 | 0.032 |
Various factors that may contribute to an increased risk of developing CTEV have been identified. These include maternal and paternal smoking, family history, exposure to amniocentesis and selective serotonin reuptake inhibitors, gestational diabetes, nulliparity, and male sex. A comprehensive meta-analysis and systematic review of 42 studies (28 case-control, 10 cohort, and 4 randomized trial) comprising 31844 CTEV cases and 6604013 controls that was conducted in 2018 confirmed the significance of previously identified risk factors[24]. In it, 10% of the mothers had chronic diseases, with asthma, hypertension, and diabetes mellitus accounting for 5%, 3%, and 2%, respectively. In addition, a family history of CTEV was present in 5% of the cases, a relatively low rate compared to both local and global studies[5,18]. Such a low percentage could have been the consequence of a small sample size, as in a single-hospital based study.
Several associated conditions have been observed among CTEV cases, including asthma, speech difficulties, undescended testis, and DDH. However, all these conditions occur in an insignificant number of CTEV cases, representing only 2% for each[25,26]. First, asthma is among the most common chronic diseases in Saudi Arabia, with an estimated prevalence of 14.3%[21]. Consequently, asthma and CTEV have a weak association, as shown in this study, based on the relatively small sample. Second, speech difficulties and undescended testis also comprised an insignificant percentage. These points should be further investigated in a larger sample to give a well-determined strength of association.
DDH is one of the most critical anomalies associated with CTEV. In a prospective study of 101 cases, 16 were associated with mild DDH and 1 case met the acetabular index criteria of severe DDH (i.e., Tönnis angle)[27]. Moreover, an observational study including 119 cases found that 9 were diagnosed with DDH[26]. In this study, the incidence of DDH was relatively high compared to other studies in which 7% of the cases were diagnosed with DDH. However, another local study showed nearly double this percentage[25]. This study found a significant difference in the laterality of the condition, with 68% of the patients affected bilaterally and 38% unilaterally. The right foot was involved in 19% of the unilateral cases and the left foot was involved in 17%. This difference was not significant in other studies[26,27].
This study has potential limitations. First, it was conducted at a single hospital, focused on a specific region in Saudi Arabia, and may not be represent the entire population. Therefore, caution should be exercised in generalizing the findings to the broader Saudi population. Second, the past medical history of mothers was not adequately documented, which could affect the reliability of the reported chronic diseases. Further study is needed to explore associated conditions and their prevalence in greater detail, using larger sample sizes and more diverse settings.
This study provides valuable insights into the prevalence of CTEV in Saudi Arabia, specifically in the Eastern Province. The study population had a significant burden of CTEV, with a higher prevalence than both global and local statistics. Comprehensive interventions and healthcare planning are needed to manage and address the associated conditions of CTEV in Saudi Arabia. More study is needed to better understand the prevalence of CTEV and associated factors in Saudi Arabia.
| 1. | Naveed A, Fatima SA, Riaz S, Awan SS, Waqas MS, Aslam S. Prevalence of leg pain and knee contractures in children having clubfoot. Rawal Med J. 2021;46:587-588. |
| 2. | Cady R, Hennessey TA, Schwend RM. Diagnosis and Treatment of Idiopathic Congenital Clubfoot. Pediatrics. 2022;149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 31] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 3. | Mustari MN, Faruk M, Bausat A, Fikry A. Congenital talipes equinovarus: A literature review. Ann Med Surg (Lond). 2022;81:104394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Rendy G, Dwi Winanto I, Ilham Abdullah Irsyam O. The effect of socioeconomic fac-tors on the first visit of a clubfoot to a health facility. IJRP. 2022;101. [DOI] [Full Text] |
| 5. | Panza R, Albano F, Casto A, Del Vecchio C, Laforgia N, Dibello D. Incidence and prevalence of congenital clubfoot in Apulia: a regional model for future prospective national studies. Ital J Pediatr. 2023;49:151. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Pavone V, Chisari E, Vescio A, Lucenti L, Sessa G, Testa G. The etiology of idiopathic congenital talipes equinovarus: a systematic review. J Orthop Surg Res. 2018;13:206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 64] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 7. | Yolaçan H, Güler S, Özmanevra R. Clubfoot from past to the present: A bibliometric analysis with global productivity and research trends. Medicine (Baltimore). 2023;102:e32803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Maghfuri HB, Alshareef AA. The Efficacy of the Ponseti Method in the Management of Clubfoot: A Systematic Review. Cureus. 2024;16:e52482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Smythe T, Rotenberg S, Lavy C. The global birth prevalence of clubfoot: a systematic review and meta-analysis. EClinicalMedicine. 2023;63:102178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 10. | Arianto HF, Faesal A Maodah, Yunus Abdul Bari. Talipes Equinovarus (TEV) and VACTREL Associated Anomalies: Narrative Literature Review. Bioscmed. 2022;6:2014-2022. [DOI] [Full Text] |
| 11. | Van Schelven H, Moerman S, Van der Steen M, Besselaar AT, Greve C. Prognostic factors for recurrent idiopathic clubfoot deformity: a systematic literature review and meta-analysis. Acta Orthop. 2022;93:11-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Society for Maternal-Fetal Medicine, McKinney J, Rac MWF, Gandhi M. Congenital talipes equinovarus (clubfoot). Am J Obstet Gynecol. 2019;221:B10-B12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Dave M, Rankin J, Pearce M, Foster HE. Global prevalence estimates of three chronic musculoskeletal conditions: club foot, juvenile idiopathic arthritis and juvenile systemic lupus erythematosus. Pediatr Rheumatol Online J. 2020;18:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 14. | Alosaimi MA, Jawhari AM, Amin OA, Alzahrani ES, Alomar MO, Nouri MT, Altalhi MJ, Marzogi AA. Community Awareness of Congenital Talipes Equinovarus (Clubfoot) in Makkah Region, Saudi Arabia: A Cross-Sectional Study. Cureus. 2022;14:e30602. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Fakeeha JH, Alessa AE, Alkhaldi MS, Alshathri MH, Althunayyan AN. Prevalence and epidemiological description of clubfoot at King Saud Medical City, Riyadh, Saudi Arabia. JMSR. 2021;5:246-249. [DOI] [Full Text] |
| 16. | Stoll C, Alembick Y, Dott B, Roth MP. Associated anomalies in cases with congenital clubfoot. Am J Med Genet A. 2020;182:2027-2036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 17. | Kruse LM, Dobbs MB, Gurnett CA. Polygenic threshold model with sex dimorphism in clubfoot inheritance: the Carter effect. J Bone Joint Surg Am. 2008;90:2688-2694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Wang H, Barisic I, Loane M, Addor MC, Bailey LM, Gatt M, Klungsoyr K, Mokoroa O, Nelen V, Neville AJ, O'Mahony M, Pierini A, Rissmann A, Verellen-Dumoulin C, de Walle HEK, Wiesel A, Wisniewska K, de Jong-van den Berg LTW, Dolk H, Khoshnood B, Garne E. Congenital clubfoot in Europe: A population-based study. Am J Med Genet A. 2019;179:595-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 19. | Fida NM, Al-Aama J, Nichols W, Nichols W, Alqahtani M. A prospective study of congenital malformations among live born neonates at a University Hospital in Western Saudi Arabia. Saudi Med J. 2007;28:1367-1373. [PubMed] |
| 20. | Sahin O, Yildirim C, Akgun RC, Haberal B, Yazici AC, Tuncay IC. Consanguineous marriage and increased risk of idiopathic congenital talipes equinovarus: a case-control study in a rural area. J Pediatr Orthop. 2013;33:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Kurdi AM, Majeed-Saidan MA, Al Rakaf MS, AlHashem AM, Botto LD, Baaqeel HS, Ammari AN. Congenital anomalies and associated risk factors in a Saudi population: a cohort study from pregnancy to age 2 years. BMJ Open. 2019;9:e026351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 22. | Yi L, Zhou GX, Dai L, Li KS, Zhu J, Wang Y. [An descriptive epidemiological study on congenital clubfoot in China during 2001 to 2010]. Sichuan Da Xue Xue Bao Yi Xue Ban. 2013;44:606-609. [PubMed] |
| 23. | Parker SE, Mai CT, Strickland MJ, Olney RS, Rickard R, Marengo L, Wang Y, Hashmi SS, Meyer RE; National Birth Defects Prevention Network. Multistate study of the epidemiology of clubfoot. Birth Defects Res A Clin Mol Teratol. 2009;85:897-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Chen C, Kaushal N, Scher DM, Doyle SM, Blanco JS, Dodwell ER. Clubfoot Etiology: A Meta-Analysis and Systematic Review of Observational and Randomized Trials. J Pediatr Orthop. 2018;38:e462-e469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 25. | Al-Moamary MS, Alhaider SA, Alangari AA, Idrees MM, Zeitouni MO, Al Ghobain MO, Alanazi AF, Al-Harbi AS, Yousef AA, Alorainy HS, Al-Hajjaj MS. The Saudi Initiative for Asthma - 2021 Update: Guidelines for the diagnosis and management of asthma in adults and children. Ann Thorac Med. 2021;16:4-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 26. | Håberg Ø, Foss OA, Lian ØB, Holen KJ. Is foot deformity associated with developmental dysplasia of the hip? Bone Joint J. 2020;102-B:1582-1586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Chou DTs, Ramachandran M. Prevalence of developmental dysplasia of the hip in children with clubfoot. J Child Orthop. 2013;7:263-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |