Published online Jun 18, 2024. doi: 10.5312/wjo.v15.i6.585
Revised: March 10, 2024
Accepted: May 7, 2024
Published online: June 18, 2024
Processing time: 147 Days and 11.7 Hours
Cheilectomy of the 1st metatarsophalangeal joint (MTPJ) is one of the most common procedures for the management of hallux rigidus. However, there is no consensus regarding outcomes following minimally invasive dorsal cheilectomy (MIDC) for the management of hallux rigidus.
To evaluate outcomes following MIDC for the management of hallux rigidus.
During November 2023, the PubMed, EMBASE and Cochrane Library databases were systematically reviewed to identify clinical studies examining outcomes following MIDC for the management of hallux rigidus.
Six studies were included. In total, 348 patients (370 feet) underwent MIDC for hallux rigidus at a weighted mean follow-up of 37.9 ± 16.5 months. The distribution of patients by Coughlin and Shurna's classification was recorded in 4 studies as follows: I (58 patients, 27.1%), II (112 patients, 52.3%), III (44 patients, 20.6%). Three studies performed an additional 1st MTPJ arthroscopy and debridement following MIDC. Retained intra-articular bone debris was observed in 100% of patients in 1 study. The weighted mean American orthopedic foot and ankle society score improved from a preoperative score of 68.9 ± 3.2 to a postoperative score of 87.1. The complication rate was 8.4%, the most common of which was persistent joint pain and stiffness. Thirty-two failures (8.7%) were observed. Thirty-three secondary procedures (8.9%) were performed at a weighted mean time of 8.6 ± 3.2 months following the index procedure.
This systematic review demonstrated improvements in subjective clinical outcomes together with a moderate complication rate following MIDC for the management of hallux rigidus at short-term follow-up. A moderate re-operation rate at short-term follow-up was recorded. The marked heterogeneity between included studies and paucity of high quality comparative studies limits the generation of any robust conclusions.
Core Tip: This systematic review found improvements in patient reported outcome measurements together with a moderate complication rate following minimally invasive dorsal cheilectomy (MIDC) for the management of hallux rigidus at short-term follow-up. A moderate re-operation rate at short-term follow-up was recorded. The marked heterogeneity between included studies and dearth of high quality comparative studies limits the generation of any robust conclusions. This current systematic review demonstrates that MIDC may be a safe, efficacious procedure in the setting of low-to-moderate grade hallux rigidus.
- Citation: Esser K, Butler JJ, Roof M, Mercer NP, Harrington MC, Samsonov AP, Rosenbaum AJ, Kennedy JG. Outcomes following minimally invasive dorsal cheilectomy for hallux rigidus: A systematic review. World J Orthop 2024; 15(6): 585-592
- URL: https://www.wjgnet.com/2218-5836/full/v15/i6/585.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i6.585
Osteoarthritis of the first metatarsophalangeal joint (MTPJ) is the most common arthritic condition of the foot, affecting 2.5% of patients over 50 years old[1]. Classic presentation entails 1st MTPJ pain and progressive stiffness exacerbated on toe-off[1]. For patients with low-to-moderate grade hallux rigidus as graded by the Coughlin and Shurnas’ classification[2], initial management entails the use of nonsteroidal anti-inflammatory drugs, intra-articular corticosteroid injections, physical therapy, and shoe wear modification[1]. For patients with mild-to-moderate recalcitrant hallux rigidus, operative management using a dorsal metatarsal cheilectomy is often recommended[3]. DuVries first described the open dorsal cheilectomy in 1959, which involves resection of dorsal osteophytes from the metatarsal head and proximal phalanx and debridement of pathological synovitis. This procedure has produced satisfactory outcomes in the short-term and is considered the gold standard treatment option for moderate hallux rigidus[3].
Minimally invasive dorsal cheilectomy (MIDC) is a joint-preserving procedure that has become an increasingly popular alternative to an open approach[4-9]. The approach involves a dorsomedial stab incision and percutaneous insertion of instrumentation, with the dorsal osteophyte resected with a burr under fluoroscopic guidance[5]. Several recent studies have reported numerous benefits to this approach: smaller incisions, reduced soft-tissue disruption, reduced postoperative morbidity, accelerated recovery time, and improved aesthetics post-procedure[8,9]. Despite reports of good postoperative outcomes, there is no consensus regarding subjective clinical outcomes, radiographic outcomes, complication rates, and recurrence rates following MIDC for hallux rigidus.
To our knowledge, no systematic review examining outcomes following MIDC for hallux rigidus has been performed at present. The purpose of this systematic review was to assess the clinical, functional and radiographic outcomes following MIDC. In addition, the level of evidence (LOE) and quality of evidence of the included studies were analysed.
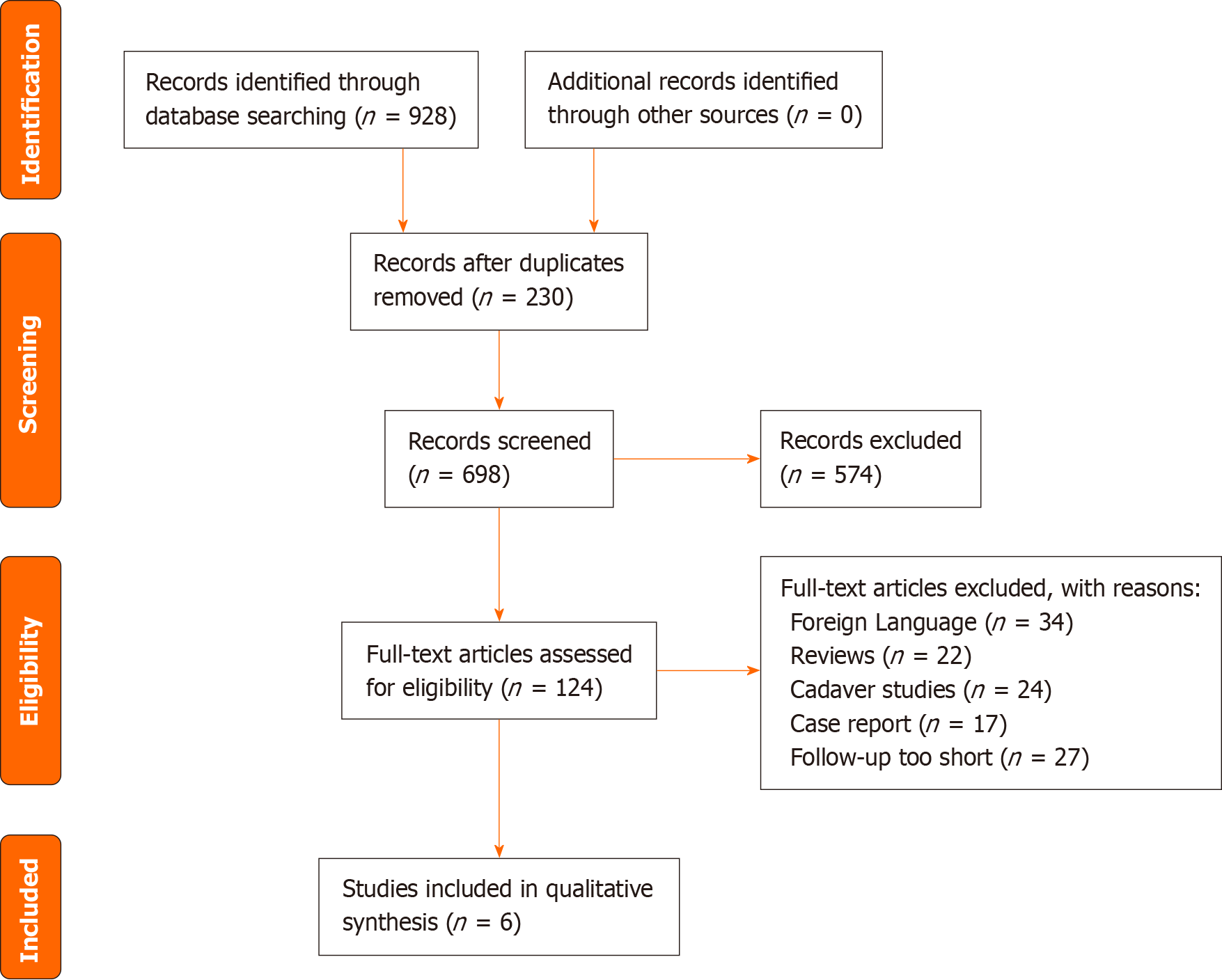
In November 2023, a systematic review of the MEDLINE, EMBASE and Cochrane Library databases was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines[10]. The following search terms were used: [(hallux and rigidus) or (metatarsophalangeal joint) and (cheilectomy)]. Table 1 displays the inclusion and exclusion criteria. Following retrieval of the data, the titles, abstracts and full text articles were screened by 2 independent reviewers of all searched studies by applying the aforementioned criteria. A senior author was consulted to arbitrate any disagreements that arose.
| Inclusion criteria | Exclusion criteria |
| Clinical studies reporting outcomes after minimally invasion cheilectomy (arthroscopic or mini-open) for hallux rigidus | Review articles |
| Follow up ≥ 12 months | Case reports |
| Published in a peer-reviewed journal | Cadaveric studies |
| Article written in English | Fewer than 5 patients per cohort |
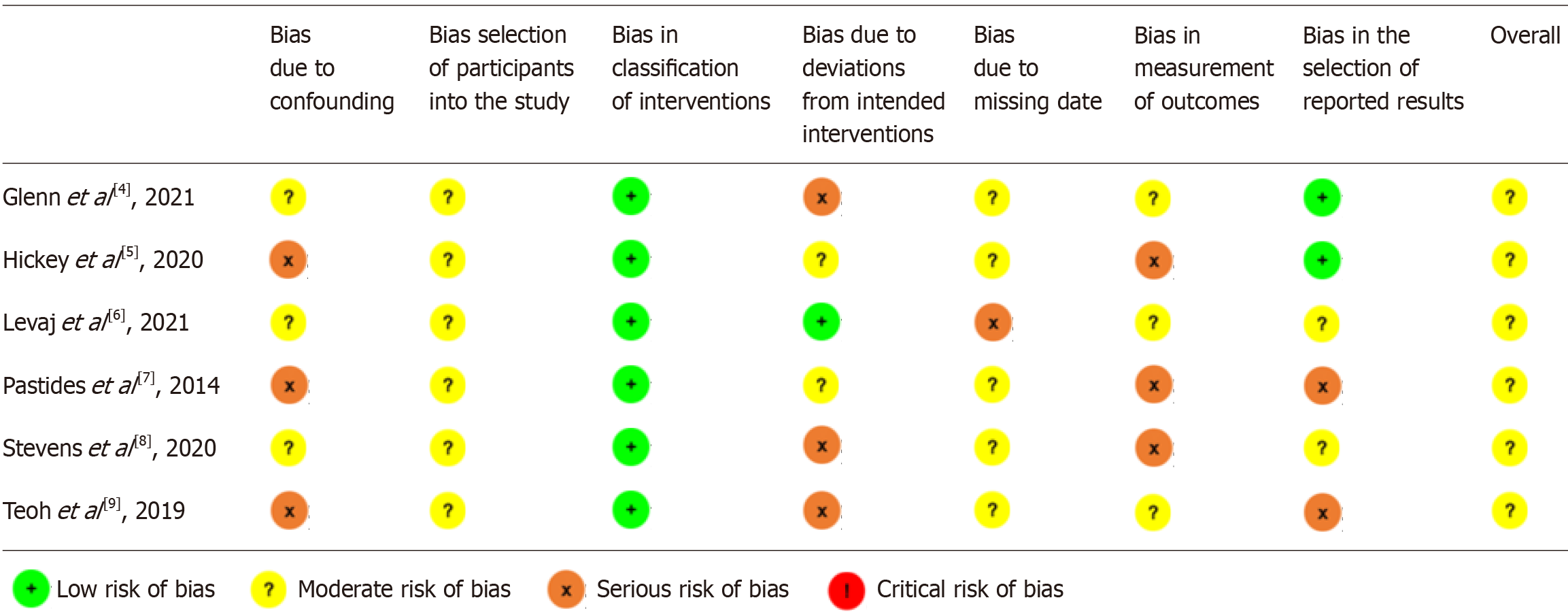
The LOE was assessed using previously accepted criteria. The risk of bias and methodological quality of clinical evidence for non-randomised studies was assessed using the Risk Of Bias In Non-randomised Studies-of Interventions tool by 2 independent reviewers[11]. The options for a domain-level risk-of-bias judgement are ‘low’, ‘moderate’, ‘serious’ or ‘critical’ risk of bias, with an additional option of ‘no information’. Discrepancies were ameliorated by a senior author who assessed the data until a consensus was found.
Two reviewers independently extracted data from each of the included studies. Data regarding patient demographics and the characteristics of the surgical procedure were collected. Objective and subjective outcomes, 1st MTPJ range of motion, postoperative imaging, complications, failures, and reoperations were evaluated.
SAS software version 9.3 (SAS Institute, Inc., Cary, NC, United States) was used to complete statistical analyses. Descriptive statistics were calculated for all continuous and categorical variables. Continuous variables were reported as weighted mean and standard deviation, whereas categorical variables were reported as frequencies with associated percentages.
The search generated 928 studies. Of these, 6 met the inclusion and exclusion criteria (Figure 1). The 6 studies were published between 2014 and 2021.
Study characteristics and patient demographic data are listed in Table 2. One study was LOE III[8] and 5 studies were LOE IV[4-7,9]. All studies were moderate risk of bias (Figure 2). In total, there were 348 patients (370 feet) that underwent minimally invasive cheilectomy for hallux rigidus with a weighted mean age of 51.1 ± 5.4 years (range: 41.8-54). There were 66 males (30.7%) and 149 females (69.3%). The weighted mean postoperative follow up time was 37.9 ± 16.5 months (range: 17-56.4 months). Fifty-eight feet (27.1%) were classified as Grade I, 112 feet (52.3%) classified as Grade II, and 44 feet (20.6%) classified as Grade III.
| Ref. | LOE | Patients (n) | Feet (n) | Mean follow-up (months) | Mean age (yr) | Sex (M/F) | Coughlin and Shurna's grade |
| Glenn et al[4], 2021 | 4 | 20 | 20 | 16.5 | 52 | M = 6; F = 14 | |
| Hickey et al[5], 2020 | 4 | 36 | 36 | 56.4 | 50 | M = 10; F = 26 | I = 5; II = 27; III = 1 |
| Levaj et al[6], 2021 | 4 | 29 | 29 | 31.2 | 41.8 | M = 19; F = 10 | I = 11; II = 12; III = 6 |
| Pastides et al[7], 2014 | 4 | 41 | 54 | 17 | 43 | M = 6; F = 35 | I = 9; II = 19; III = 26 |
| Stevens et al[8], 2020 | 3 | 133 | 133 | 36 | 54 | ||
| Teoh et al[9], 2019 | 4 | 89 | 98 | 50 | 54 | M = 25; F = 64 | I = 33; II = 54; III = 11 |
All 6 studies described using a stab incision at the dorsomedial aspect of the first MTPJ, followed by debridement of osteophytes with a burr to complete cheilectomy. Five studies reported using a 3.1 mm burr[4,5,7-9], while the remaining study did not report burr size[6]. Three studies performed 1st MTPJ arthroscopic evaluation and debridement following resection of the dorsal osteophyte[4-6]. One study reported arthroscopic findings and found that 100% of patients had bone debris within the 1st MTPJ despite irrigation following resection of the osteophyte[4]. In addition, the authors reported that 100% of patients had evidence of synovitis, 10% had loose bodies within the 1st MTPJ, and 30% had a loose cartilage flap identified on arthroscopic evaluation.
Table 3 summarises the clinical and functional outcomes. Four different subjective clinical scoring tools were recorded across the 6 studies. The most commonly utilized patient reported outcome measure (PROM) was the American Or
| Ref. | Patients (n) | Feet (n) | PROM | Score | 1st MTPJ ROM (°) | Complications | Failures | Secondary surgical procedures | ||
| Preop | Postop | Preop | Postop | |||||||
| Glenn et al[4], 2021 | 20 | 20 | VAS | 7.1 | 0.8 | 47 | 67 | 0 | 0 | 0 |
| Hickey et al[5], 2020 | 36 | 36 | AOFAS | 66.6 | n/r | 31.9 | 72.7 | EHL rupture = 1, neuropathic pain = 3, joint stiffness = 1 | 0 | Repeat arthroscopic cheilectomy = 1, manipulation under anaesthetic = 3 |
| Levaj et al[6], 2021 | 29 | 29 | n/r | 0 | 0 | Joint stiffness = 1 | 1 | Open revision = 1 | ||
| Pastides et al[7], 2014 | 41 | 54 | AOFAS | 71.1 | 87.1 | 39 | 48 | Neuropathic pain = 2 | 2 | MTPJ fusion = 2 |
| Stevens et al[8], 2020 | 133 | 133 | n/r | 0 | 0 | EHL rupture = 1, neuropathic pain = 3, superficial wound problems = 2, joint stiffness/pain = 7, ectopic bone in wound = 2 | 17 | MTPJ arthrodesis = 9, open cheilectomy = 3, MIS cheilectomy-2, interposition arthroplasty = 1, hallux valgus correction = 2 | ||
| Teoh et al[9], 2019 | 89 | 98 | VAS | 8 | 3 | 11.3 | 69.1 | Neuropathic pain = 4, superficial wound problems = 2, wound infection = 2 | 12 | Repeat cheilectomy = 4, open removal of loose bone = 1, 1st MTPJ arthrodesis = 7 |
Postoperative range of motion (ROM) of the 1st MTPJ joint was reported in 4 studies[4,5,7,9]. The weighted preoperative mean 1st MTPJ ROM was 21.5° ± 20.5° (range, 11.3°-47°). The weighted postoperative mean 1st MTPJ ROM was 42.8° ± 34.2° (range, 48°-72.7°). Four studies reported dorsiflexion[4,5,7,9]. The weighted mean dorsiflexion preoperatively was 26.8 ± 10.3 (range, 11.3-32), compared to 57.2 ± 16.3 (range, 39-72.7) postoperatively. Two studies reported plantarflexion[4,5]. The weighted preoperative mean plantarflexion was 11 ± 5.07 (range, 7-15), compared to post
Return to sport was recorded in 1 study[7]. The authors demonstrated that 73% of patients had returned to sporting activity by 6 wk after the procedure.
Radiographic data was not reported in any of the 6 studies.
Data regarding complications, secondary procedures, and failures is listed in Table 3. Complications in total, 31 complications (8.4%) were observed in the patient cohort. Complications included numbness and neuropathic pain, extensor hallucis longus tendon rupture, joint stiffness, ectopic bone in wound, superficial wound infection, and deep wound infection. The most common complication was neuropathic pain (3.2%). In total, 33 patients (8.9%) required secondary procedures at a weighted mean time of 8.6 ± 3.2 months following the index procedure. These included arthroscopic cheilectomy, steroid injection, open revision, arthrodesis, interposition arthroplasty, hallux valgus correction, and open removal of loose bone. The most common secondary surgical procedure was first MTPJ arthrodesis (6.9%). In total, there were 32 failures (8.7%) recorded at final follow-up.
This current systematic review found that MIDC produces improvements in subjective clinical outcomes and high patient satisfaction rates together with moderate complication rates (8.4%) at short-term follow up. Notably, a moderate reo
Hallux rigidus is a debilitating pathology which results in progressively worsening of 1st MTPJ pain, decreased ROM and reduced quality of life[1]. The progressive, relentless nature of the degenerative changes at the 1st MTPJ renders conservative treatment modalities ineffective in the long term. Thus, following failure of nonoperative management, surgical intervention is warranted. Joint sparing procedures including cheilectomy and interpositional arthroplasty are indicated in mild-to-moderate disease while joint sacrificing procedures such as 1st MTPJ arthrodesis are indicated in more severe pathology[3]. Open cheilectomy is the most commonly utilized joint sparing procedure for the management of mild-to-moderate hallux rigidus, with good clinical outcomes and excellent survivorship reported at short-term follow-up in the literature[12]. Cetinkaya et al[12] conducted a retrospective review of 29 patients who underwent open che
All studies included in this current review performed MIDC using a 3 mm dorsomedial stab incision followed by resection of any dorsal osteophyte using a 3.1 mm conical or wedge burr under fluoroscopic guidance. Furthermore, in 3 studies, the joint was accessed with a 2.7 mm arthroscope following resection of the dorsal osteophytes, and any identified synovitis, loose bodies, scar tissue, cartilage flaps and/or osteochondral lesions was treated as appropriate[4-6]. This systematic review found significant improvements in functional outcomes following MIDC, as evidenced by an increase in 1st MTPJ ROM from preoperative ROM of 21.5° to postoperative ROM of 42.8°, which is comparable to prior case series for open cheilectomy. This indicates that despite the less aggressive surgical approach, MIDC leads to noninferior restoration of 1st MTPJ range of motion in comparison to open cheilectomy. Furthermore, the use of the arthroscope provides excellent visualization of the joint and can identify any intra-articular pathology. Glenn et al[4] utilized an arthroscope during their procedures and found that 100% of their cases had intra-articular synovitis, 30% had large cartilage flaps contributing to 1st MTPJ impingement and 10% had loose bodies, all of which were treated concurrently at the time of the procedure, underpinning both the diagnostic and therapeutic benefits of 1st MTPJ arthroscopy during minimally invasive surgery cheilectomy[4].
Although open cheilectomy results in excellent functional outcomes, there is concern regarding postoperative morbidity, with particular attention paid to postoperative wound complication rates which are reported to range from 3.5%-9.1%[13,15]. MIDC mitigates against the morbidity associated with open cheilectomy due to the minimal soft tissue disruption afforded by smaller stab incisions in comparison to the standard 5-6 cm incision performed during open cheilectomy[4,12]. Overall, the postoperative wound complication rate in the MIDC cohort was 1.6% with no cases of deep infections nor wound dehiscence, reinforcing that MIDC is a safe, effective surgical technique with low incisional morbidity. MIDC may be a particularly useful strategy in patients predisposed to wound complications including pat
MIDC is not without limitations, however. The most common complication observed in this systematic review was iatrogenic nerve injury, which was found in 3.2% of patients who primarily reported altered sensation in the distribution of the dorsal medial cutaneous nerve (DMCN). The stab incision during MIDC is typically placed over the dorsomedial aspect of the 1st metatarsal just proximal to the medial eminence[9]. In comparison to a mid-medial incision, a dors
This current systematic review found a moderate secondary surgical procedure rate (8.9%) following MIDC in the short-term period. Teoh et al[9] postulated that a substantial proportion of the reoperations in their cohort could be attributed to the “learning curve” associated with MIDC, as 42% of their reoperations were due to a lack of technical proficiency, illustrated by the high rates of inadequate osteophyte resection[9]. Interestingly, the reoperation rate was higher in the studies that did not perform 1st MTPJ arthroscopy (10.9%) compared to the studies that did perform 1st MTPJ arthroscopy (2.4%). Glenn et al[4] found that, despite copious irrigation following resection of the osteophyte, 100% of patients had retained bone debris within the joint as visualized on arthroscopic examination of the 1st MTPJ[4]. The large quantities of retained bone debris may not be sufficiently expelled through the small incisions and can lead to persistent 1st MTPJ stiffness and pain, requiring further intra-articular injections and inevitable repeat cheilectomies and/or joint sacrificing procedures. The authors performed 1st MTPJ arthroscopic debridement of any identified bone debris in their patient cohort, and reported no reoperations at final follow-up, reinforcing that 1st MTPJ arthroscopy is crucial following MIDC to ensure adequate clearance of any debris from the joint to reduce the risk of symptomatic recurrence[4].
This systematic review is influenced by numerous limitations and/or biases. There was significant inconsistency in the reporting of data between studies, limiting the generation of robust conclusions. The search criterion was limited to the MEDLINE, EMBASE and Cochrane Library Database articles that were published exclusively in English. The included studies have a LOE that was graded as low with poor methodological quality, with no adequate control group included in any of these studies. The follow-up was short, thus the long-term longevity of MIDC could not be determined. Finally, the data extraction was not performed blindly, but was carried out by two independent reviewers and later confirmed by the lead author
This systematic review demonstrated improvements in subjective clinical outcomes together with a low complication rate following minimally invasive cheilectomy for the management of hallux rigidus at short-term follow-up. A moderate re-operation rate at short-term follow-up was recorded. However, the marked heterogeneity between included studies and paucity of high quality comparative studies limits the generation of any robust conclusions. Further research with a longer follow-up is warranted to determine the precise role for minimally invasive cheilectomy in the management of hallux rigidus.
| 1. | Ho B, Baumhauer J. Hallux rigidus. EFORT Open Rev. 2017;2:13-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 2. | Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003;85:2072-2088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 361] [Article Influence: 17.2] [Reference Citation Analysis (1)] |
| 3. | Galois L, Hemmer J, Ray V, Sirveaux F. Surgical options for hallux rigidus: state of the art and review of the literature. Eur J Orthop Surg Traumatol. 2020;30:57-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 4. | Glenn RL, Gonzalez TA, Peterson AB, Kaplan J. Minimally Invasive Dorsal Cheilectomy and Hallux Metatarsal Phalangeal Joint Arthroscopy for the Treatment of Hallux Rigidus. Foot Ankle Orthop. 2021;6:2473011421993103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 5. | Hickey BA, Siew D, Nambiar M, Bedi HS. Intermediate-term results of isolated minimally invasive arthroscopic cheilectomy in the treatment of hallux rigidus. Eur J Orthop Surg Traumatol. 2020;30:1277-1283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Levaj I, Knežević I, Dimnjaković D, Smoljanović T, Bojanić I. First Metatarsophalangeal Joint Arthroscopy of 36 Consecutive Cases. Acta Chir Orthop Traumatol Cech. 2021;88:211-216. [PubMed] [DOI] [Full Text] |
| 7. | Pastides PS, El-Sallakh S, Charalambides C. Minimally Invasive Cheilectomy for the Treatment of Grade I to III Hallux Rigidus: A Prospective Study Reporting on Early Patient Outcome. Tech Foot Ankle Surg. 2014;13:98. [DOI] [Full Text] |
| 8. | Stevens R, Bursnall M, Chadwick C, Davies H, Flowers M, Blundell C, Davies M. Comparison of Complication and Reoperation Rates for Minimally Invasive Versus Open Cheilectomy of the First Metatarsophalangeal Joint. Foot Ankle Int. 2020;41:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Teoh KH, Tan WT, Atiyah Z, Ahmad A, Tanaka H, Hariharan K. Clinical Outcomes Following Minimally Invasive Dorsal Cheilectomy for Hallux Rigidus. Foot Ankle Int. 2019;40:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 10. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13930] [Cited by in RCA: 13343] [Article Influence: 833.9] [Reference Citation Analysis (0)] |
| 11. | Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7683] [Cited by in RCA: 10833] [Article Influence: 1203.7] [Reference Citation Analysis (2)] |
| 12. | Cetinkaya E, Yalcinkaya M, Sokucu S, Polat A, Ozkaya U, Parmaksizoglu AS. Cheilectomy as a First-Line Surgical Treatment Option Yields Good Functional Results in Grade III Hallux Rigidus. J Am Podiatr Med Assoc. 2016;106:22-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Waizy H, Czardybon MA, Stukenborg-Colsman C, Wingenfeld C, Wellmann M, Windhagen H, Frank D. Mid- and long-term results of the joint preserving therapy of hallux rigidus. Arch Orthop Trauma Surg. 2010;130:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Hogan MV, Mani SB, Chan JY, Do H, Deland JT, Ellis SJ. Validation of the Foot and Ankle Outcome Score for Hallux Rigidus. HSS J. 2016;12:44-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Easley ME, Davis WH, Anderson RB. Intermediate to long-term follow-up of medial-approach dorsal cheilectomy for hallux rigidus. Foot Ankle Int. 1999;20:147-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 109] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Fisichella L, Fenga D, Rosa MA. Surgical Site Infection In Orthopaedic Surgery: Correlation Between Age, Diabetes, Smoke And Surgical Risk. Folia Med (Plovdiv). 2014;56:259-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Lai Q, Cai K, Lin T, Zhou C, Chen Z, Zhang Q. Prior Intra-articular Corticosteroid Injection Within 3 Months May Increase the Risk of Deep Infection in Subsequent Joint Arthroplasty: A Meta-analysis. Clin Orthop Relat Res. 2022;480:971-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 18. | Solan MC, Lemon M, Bendall SP. The surgical anatomy of the dorsomedial cutaneous nerve of the hallux. J Bone Joint Surg Br. 2001;83:250-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |