Published online Jun 18, 2024. doi: 10.5312/wjo.v15.i6.578
Revised: March 14, 2024
Accepted: April 29, 2024
Published online: June 18, 2024
Processing time: 165 Days and 8.5 Hours
Elderly patients maintaining functional independence can now be candidates for primary wrist hemiarthroplasty to manage acute irreparable distal radius fra
To review the literature on the outcomes of distal radius hemiarthroplasty with available implants to assess its viability as a treatment option.
A comprehensive review of the literature was conducted using electronic da
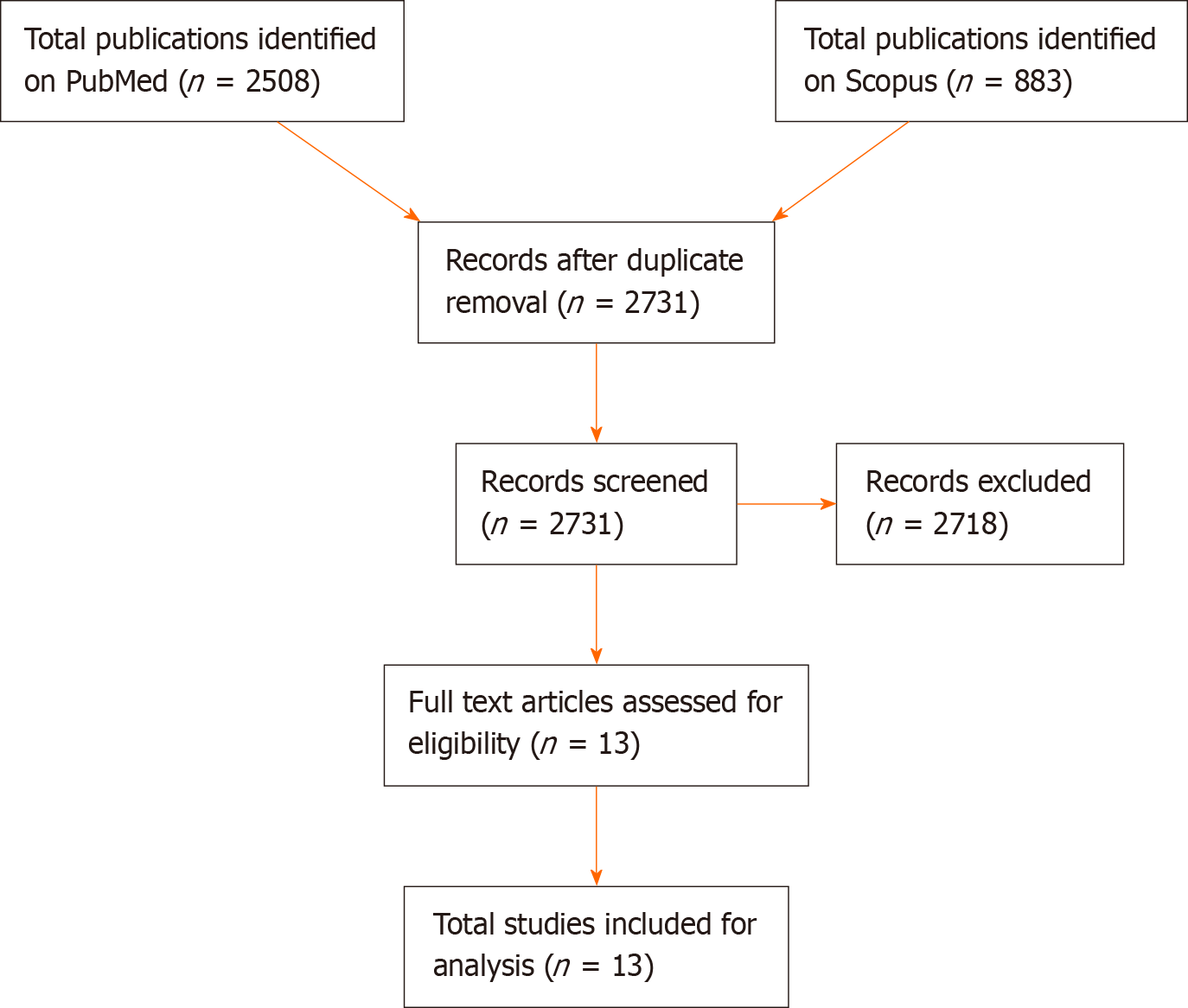
A total of 2508 articles from PubMed and 883 from Scopus were identified ini
Hemiarthroplasty is a promising treatment for irreparable DRF in the elderly. Long-term outcomes and complications require further study.
Core Tip: Distal radius fractures in elderly individuals often present challenges for stable fixation. Hemiarthroplasty has emerged as a treatment option, but definitive guidelines are lacking. This review aimed to clarify the circumstances warranting hemiarthroplasty in distal radius fractures.
- Citation: Cannella A, Caruso L, Sassara GM, Taccardo G, Passiatore M, Marescalchi M, De Vitis R. Hemiarthroplasty for irreparable distal radius fractures in the elderly: A comprehensive review. World J Orthop 2024; 15(6): 578-584
- URL: https://www.wjgnet.com/2218-5836/full/v15/i6/578.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i6.578
Distal radius fractures (DRFs) represent 12%-17% of all fractures[1-5]. DRFs have a bimodal distribution in the population because they occur after a high-energy trauma in young adults and after low-energy trauma in elderly adults, particularly in females. This kind of fracture is so common that it has been estimated that DRFs in the elderly are second only to proximal femur fractures. Approximately 10% of 65-year-old White females will experience a DRF in their remaining life span[6]. Orbay and Fernandez[7] determined that 33% of DRFs in the elderly were classified as type C3 according to the AO classification.
Martinez-Mendez et al[8] concluded that the use of volar plating should be preferred to other treatments even though complications such as loss of reduction, intraarticular screw penetration leading to malunion, osteoarthritis, and clinical failure do occur[9,10]. Due to these complications, Roux[11], inspired by hip and shoulder hemiarthroplasty, was the first to propose the implementation of radius hemiarthroplasty to minimize hospitalization and facilitate an early recovery and return to daily activities. Moreover, Herzberg et al[12] suggested a list of at least six criteria to proceed with a distal radius replacement[12,13]. The criteria included patient characteristics, energy of the accident, characteristics of the fracture chart (e.g., AO type C complete intraarticular fracture, high extraarticular and intraarticular displacement scores exceeding 6/12, main fracture line distal to the watershed line, impaction, and circumferential comminution), and trauma occurring in an active and autonomous patient.
The objective of this review was to gather, condense, and contrast findings reported in the literature regarding the efficacy of various implants in distal radius hemiarthroplasty as a potential treatment approach for elderly patients with DRFs.
The literature review encompassed studies accessible through the electronic databases PubMed and Scopus. Searches were conducted using logical operators such as "AND" and "OR" in combination with keywords including "wrist arthroplasty" , "wrist hemiarthroplasty" , "wrist replacement" , "wrist prosthesis" , "wrist hemiprosthesis" , "wrist fracture" , and "distal radius fracture" . Articles were restricted to those available in French, English, Italian, or Spanish and were confined to those published until December 1, 2023.
Initially, a total of 2508 articles were identified from PubMed and 883 from Scopus. Following the elimination of duplicates, full-text articles from indexed journals were screened by the authors based on abstracts, specifically focusing on studies where hemiarthroplasty was employed as the primary treatment for DRF. Exclusion criteria were applied to eliminate studies involving total wrist prostheses or those with indications not pertinent to DRF, such as primary or secondary wrist arthrosis (Figure 1).
Ultimately, 13 articles meeting the selection criteria were deemed eligible for inclusion in the review. All 13 articles were clinical retrospective studies, with 2 among them being case reports.
High variability was found between the 13 studies, which did not allow for a comparative statistical analysis. However, some features were consistent between the papers, allowing a descriptive analysis. As shown in Table 1, all 13 studies had a mean age at surgery of at least 73-years-old. Most patients were female, as there were only 7 males (4.2%) out of a total of 165 patients. With the exception of Apard et al[14] (a case report), all studies had a follow-up period of at least 18 months with a mean of 34.3 months.
| Ref. | Patient number | Sex | Mean age | Prosthesis indication | AO classification | Follow-up in mo | VAS | DASH | Lyon score, % | PRWE | Grip strength | Flexion | Extension | Forearm rotation arc | Ulnar deviation | Radial deviation | Cemented | Non cemented | ||||||||
| M | F | Fracture | Mal union | Tumor | OTF | C | C1 | C2 | C3 | A3 | ||||||||||||||||
| Cobra, Benedikt et al[17], 2022 | 13 | 1 | 12 | 73.5 | 13 | 0 | 0 | 0 | 0 | 0 | 0 | 13 | 0 | 31.2 | 1.1 | 39.1 | 63.3 | 36.2 | 78.3% | 22° | 46° | 136° | 29° | 17° | 7 | 5 |
| Cobra, Anger et al[16], 2019 | 11 | 0 | 11 | 80 | 11 | 0 | 0 | 0 | 0 | 0 | 2 | 9 | 0 | 18.3 | 3.8 | 59.0 | 50.0 | 72.0 | 44.0% | 36° | 27° | 164° | 26° | 15° | 8 | 3 |
| Cobra, Apard et al[14], 2022 | 1 | 0 | 1 | 83 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 6.0 | 1.0 | ND | 80.0 | ND | ND | ND | 70° | ND | ND | ND | 0 | 1 |
| EMIReMotion, Holzbauer et al[25], 2022 | 1 | 0 | 1 | 73 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 78.0 | 0 | 38.0 | ND | ND | 28 kg | 35° | 35° | 180° | 20° | 15° | 0 | 1 |
| SOPHIA, Roux et al[11], 2009 | 12 | 1 | 11 | 73 | 4 | 1 | 1 | 0 | NA | NA | NA | NA | NA | 27.0 | 1.5 | 27.2 | ND | ND | 80.0% | 30° | 65° | 110° | 20° | 20° | 6 | 0 |
| SOPHIA, Roux et al[15], 2011 | 12 | 1 | 11 | 75 | 6 | 5 | 1 | 0 | NA | NA | NA | NA | NA | 29.0 | ND | ND | ND | ND | 72.0% | 36° | 60° | 128° | 26° | 21° | 12 | 0 |
| SOPHIA, Vergnenègre et al[26], 2015 | 8 | 0 | 8 | 80 | 8 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 25.0 | 2.0 | 18.0 | ND | ND | 92.0% | 46° | 44° | 160° | 25° | 25° | 8 | 0 |
| ReMotion/Cobra, Herzberg et al[18], 2023 | 26 | 1 | 25 | 79 | 28 | 0 | 0 | 0 | 28 | 0 | 0 | 0 | 0 | 32.0 | 1.0 | ND | 75.0 | ND | 68.0% | 25° | 35° | 148° | ND | ND | 2 C§ | 10 R2; 16 C1 |
| ReMotion/Cobra, Herzberg et al[22], 2017 | 15 | 0 | 11 | 74 | 12 | 0 | 0 | 0 | 12 | 0 | 0 | 0 | 0 | 32.0 | 1.0 | 25.0 | 75.0 | 22.0 | 69.0% | 27° | 35° | 149° | ND | ND | 0 | 12/12 |
| 0 | 4 | 78 | 1 | 3 | 0 | 0 | NA | NA | NA | NA | NA | 24.0 | 2.3 | 31.0 | 67.0 | 39.3 | 59.3% | 25° | 41° | 146° | ND | ND | 0 | 4/4 | ||
| ReMotion/Cobra, Herzberg et al[19], 2018 | 25 | 1 | 24 | 77 | 19 | 5 | 0 | 3 | NA | NA | NA | NA | NA | 32.0 | 1.0 | 26.0 | 74.0 | 25.0 | 68.0% | 24° | 36° | 150° | ND | ND | 2/27 | 25/27 |
| ReMotion/Cobra, Herzberg et al[21], 2015 | 11 | 0 | 11 | 76 | 12 | 0 | 0 | 0 | 12 | 0 | 0 | 0 | 0 | 30.0 | 1.0 | 32.0 | 73.0 | 24.0 | 64.0% | 26° | 34° | 151° | ND | ND | 9 R2; 2 C1 | 0 |
| Prosthelast, Ichihara et al[23], 2015 | 12 | 0 | 12 | 76 | 11 | 0 | 0 | 1 | 0 | 1 | 6 | 3 | 2 | 32.0 | 2.8 | 37.4 | ND | ND | 49.9% | 40° | 52° | 138° | ND | ND | 0 | 12 |
| Prosthelast, Martins et al[20], 2020 | 24 | 2 | 22 | 78 | 24 | 0 | 0 | 0 | 0 | 0 | 7 | 15 | 0 | 55.0 | 2.1 | 39.8 | ND | 42.7 | 65.5% | 39° | 49° | 142° | ND | ND | 0 | 24 |
All fractures were defined as irreparable with complete intraarticular fracture with high extraarticular and intraarticular displacement, main fracture line distal to the watershed line, impaction, and circumferential comminution[12,13]. Furthermore, only 10 studies classified them as type C according to the AO classification, and 3 studies did not specify whether they were C1, C2, or C3. An evaluation of the pain perceived at the last follow-up was reported with the visual analog scale (VAS) in all the studies except that by Roux[15]. The pain at last follow-up did not exceed 3. The highest pain of almost 4 was observed by Anger et al[16].
The Disability of the Arm, Shoulder, and Hand (DASH) and Lyon scores were the most utilized functional outcome measurements. DASH was reported in 10 studies, ranging from 18 to 59 points, and the Lyon score was calculated in 7 studies, ranging from 50%-80%. The Patient Rated Wrist Evaluation (PRWE) was reported in six studies, ranging from 72 to 18. All authors provided grip strength, flexion and extension degrees, and pronosupination arc measurements. However, only six studies provided measurements for ulnar and radial deviation degrees.
The use of cement was specified in every study. All SOPHIA prostheses were cemented, and the Prosthelast protheses were not cemented. When the Cobra or the proximal component of the ReMotion prostheses were used, cement was used in 7 out of 13 patients by Benedikt et al[17], in 8 out of 11 patients by Anger et al[16], and in 2 out of 28 patients and 2 out of 27patients by the Cobra inventor Herzberg et al[18,19].
Major complications were reported with acceptable rates. There were no reports of any form of infection even in minimally exposed fractures. The most frequently reported complication was complex pain regional syndrome (15 cases). Less frequent complications included 1 case of extensor pollicis longus rupture, 2 cases of extensors tenosynovitis, 5 cases of ulnar head resections for distal radio-ulnar joint conflict, 3 cases of implant revision secondary in 2 cases to implant loosening and in 1 case to a post-traumatic fracture, and 8 cases of asymptomatic radial head perforation.
Due to several factors including the variety of implants (SOPHIA, ReMotion, Cobra, Prosthelast), the different follow-up periods, and the absence of detailed results for single patients, we were not able to conduct a statistical analysis. Nevertheless, some general conclusions can be drawn for all studies except for Anger et al[16]. In this study, the follow-up period was much shorter compared to the other studies. However, even with this limit, those other investigators observed satisfactory VAS scores in their elderly patients.
The SOPHIA implant showed a DASH score < 30 points when all studies were considered. A DASH score of < 40 points was reported in the two studies using the Prosthelast implant. This result is promising because the data comes from the study of Martins et al[20]. Those authors reported a DASH score of 39.8 and had the longest mean follow-up period (55 months). They also reported that all prostheses were primary implants in fractures. It was more difficult to establish a DASH score for the Cobra and ReMotion prostheses because four[18,19,21,22] of the six studies were from the same group and presented the two prostheses together. Excepting of the report of DASH score of 59 by Anger et al[16], the collective reported DASH scores obtained by Cobra and ReMotion are < 40 and comparable to those obtained with Prosthelast[20,23]. Other functional scores, such as the Lyon score and the PRWE, were measured only in the Cobra and ReMotion studies and in the Prosthelast work by Martins et al[20] and were consistent with the DASH scores.
Almost all the studies reported the grip strength at the last follow-up. They compared the grip strength with the contralateral hand and observed the highest percentages in patients with the SOPHIA implant, followed by Cobra, ReMotion, and finally Prosthelast. All studies also reported forearm rotation arc and flexion-extension arc. Studies on Prosthelast and SOPHIA reported a flexion-extension arc of approximately 90°, while the studies on ReMotion and Cobra reported a flexion-extension arc that ranged from 60° to 70°. The forearm rotation arc was satisfactory in all the studies, ranging from 164° in the study by Anger et al[16] to 100° in the studies by Roux[11,15]. The lower forearm rotation arc reported by Roux[11,15] was justified by the higher dimension of the SOPHIA implant and the use of the ulnar head to gain implant stability, which can lead to distal radioulnar impingement or limitation on forearm rotation.
All SOPHIA implants were cemented since it has a relatively short stem in comparison to the prosthesis dimensions. All Prosthelast implants were cementless since the absence of implant subsidence should be granted by the intramedullary Kirschner. The rotation is controlled by the stem design, and the distal radius periosteal flaps are isolated and sutured above the implant. The ReMotion implant was never cemented. The Cobra implants were only cemented in two studies by Herzberg et al[18,22]. Benedikt et al[17] and Anger et al[16] were less confident in the osteointegration, especially in highly osteoporotic patients. Therefore, they cemented 7 of 13 prostheses and 8 of 11 prostheses, respectively.
Although most complications were resolved with a secondary procedure and ultimately a good recovery was achieved for all the patients, it is important to note that the complication rate in 7 of 11 retrospective studies was around 25% when excluding complex regional pain syndrome cases that improved without consequences. Nevertheless, the absence of a prolonged period of hospitalization, which is necessary in less invasive treatments, prevents the development of a major complication as described by Diaz-Garcia et al[24].
Although most studies had a relatively short follow-up period and small sample size, we believe that distal radius hemiarthroplasty should be considered as a treatment option for elderly patients with DRF. Distal radius hemiarthroplasty in carefully selected patients is an excellent option due to the short recovery time and low complication rate.
| 1. | Solgaard S, Petersen VS. Epidemiology of distal radius fractures. Acta Orthop Scand. 1985;56:391-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 85] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | O'Neill TW, Cooper C, Finn JD, Lunt M, Purdie D, Reid DM, Rowe R, Woolf AD, Wallace WA; UK Colles' Fracture Study Group. Incidence of distal forearm fracture in British men and women. Osteoporos Int. 2001;12:555-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 203] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 3. | Owen RA, Melton LJ 3rd, Johnson KA, Ilstrup DM, Riggs BL. Incidence of Colles' fracture in a North American community. Am J Public Health. 1982;72:605-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 182] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Singer BR, McLauchlan GJ, Robinson CM, Christie J. Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg Br. 1998;80:243-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 322] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 5. | LIDSTROM A. Fractures of the distal end of the radius. A clinical and statistical study of end results. Acta Orthop Scand Suppl. 1959;41:1-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 143] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 6. | Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles', or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149:2445-2448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 69] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29:96-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 310] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 8. | Martinez-Mendez D, Lizaur-Utrilla A, de-Juan-Herrero J. Intra-articular distal radius fractures in elderly patients: a randomized prospective study of casting versus volar plating. J Hand Surg Eur Vol. 2018;43:142-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 85] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 9. | Quadlbauer S, Pezzei C, Jurkowitsch J, Rosenauer R, Pichler A, Schättin S, Hausner T, Leixnering M. Early complications and radiological outcome after distal radius fractures stabilized by volar angular stable locking plate. Arch Orthop Trauma Surg. 2018;138:1773-1782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 10. | Rosenauer R, Pezzei C, Quadlbauer S, Keuchel T, Jurkowitsch J, Hausner T, Leixnering M. Complications after operatively treated distal radius fractures. Arch Orthop Trauma Surg. 2020;140:665-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 11. | Roux JL. [Replacement and resurfacing prosthesis of the distal radius: a new therapeutic concept]. Chir Main. 2009;28:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Herzberg G, Izem Y, Al Saati M, Plotard F. "PAF" analysis of acute distal radius fractures in adults. Preliminary results. Chir Main. 2010;29:231-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Herzberg G. Acute Distal Radius Fracture: PAF Analysis. J Wrist Surg. 2013;2:95-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Apard T, Odoemene M, Descamps J. Wrist Hemiarthroplasty of Irreparable Distal Radius Fracture under Wide-Awake Local Anesthetic and No Tourniquet. Life (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Roux JL. Traitement des fractures intra-articulaires du radius distal par remplacement et resurfaçage prothétique. RCO. 2011;97:S46-S53. [DOI] [Full Text] |
| 16. | Anger F, Legré R, Nguyen MK. Results of wrist hemiarthroplasty for comminuted distal radius fractures in independent elderly people: A retrospective study on eleven patients. Hand Surg Rehabil. 2019;38:150-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Benedikt S, Kaiser P, Schmidle G, Kastenberger T, Stock K, Arora R. Lessons learned with the Cobra prosthesis in elderly patients with complex distal radius fractures-a retrospective follow-up study. Arch Orthop Trauma Surg. 2022;142:343-353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Herzberg G, Burnier M, Ly L. Role for Wrist Hemiarthroplasty in Acute Irreparable Distal Radius Fracture in the Elderly. Hand Clin. 2023;39:545-550. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Herzberg G, Walch A, Burnier M. Wrist hemiarthroplasty for irreparable DRF in the elderly. Eur J Orthop Surg Traumatol. 2018;28:1499-1503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Martins A, Lazarus P, Facca S, Gouzou S, Meyer N, Liverneaux P. Isoelastic resurfacing prosthesis for distal radius fractures: Outcomes in 24 cases with at least 2 years' follow-up. Orthop Traumatol Surg Res. 2020;106:1613-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Herzberg G, Burnier M, Marc A, Izem Y. Primary Wrist Hemiarthroplasty for Irreparable Distal Radius Fracture in the Independent Elderly. J Wrist Surg. 2015;4:156-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Herzberg G, Merlini L, Burnier M. Hemi-arthroplasty for distal radius fracture in the independent elderly. Orthop Traumatol Surg Res. 2017;103:915-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Ichihara S, Díaz JJ, Peterson B, Facca S, Bodin F, Liverneaux P. Distal Radius Isoelastic Resurfacing Prosthesis: A Preliminary Report. J Wrist Surg. 2015;4:150-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Diaz-Garcia RJ, Oda T, Shauver MJ, Chung KC. A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. J Hand Surg Am. 2011;36:824-35.e2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 293] [Cited by in RCA: 263] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 25. | Holzbauer M, Bodell LS, Froschauer SM. Wrist Hemiarthroplasty for Complex Intraarticular Distal Radius Fracture in a Patient with Manifest Osteoporosis. Life (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 26. | Vergnenègre G, Hardy J, Mabit C, Charissoux JL, Marcheix PS. Hemiarthroplasty for Complex Distal Radius Fractures in Elderly Patients. J Wrist Surg. 2015;4:169-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |