Published online Jun 18, 2024. doi: 10.5312/wjo.v15.i6.570
Revised: April 14, 2024
Accepted: April 26, 2024
Published online: June 18, 2024
Processing time: 188 Days and 7.5 Hours
The preferred treatment for distal humeral intercondylar fractures is open re
To compare triceps reflecting anconeus pedicle (TRAP) and olecranon osteotomy approaches for internal fixation of distal humeral intercondylar fracture.
In total, 40 cases of Arbeitsgemeinschaft für Osteosynthesefragen/Association of the Study of Internal Fixation type C, closed, and Gustilo type I intercondylar humeral fractures were included. Patients ranged in age from 18 years to 70 years. The patients were randomized into two groups: TRAP group and olecranon ost
The mean age was 43.2 years in the TRAP group and 37.5 years in the olecranon osteotomy group. The mean operative time and mean duration of hospital stay in the TRAP group were significantly higher than in the olecranon osteotomy group (119.5 vs 111.5 min and 9.85 vs 5.45 d, respectively). The mean arc of flexion-extension, Disabilities of Arm, Shoulder and Hand score, and Mayo Elbow Performance Score were comparable without any significant difference in the groups at the 12-month follow-up (107.0 vs 106.2, 18.3 vs 15.7, and 84.2 vs 86.2, respectively). Ulnar paresthesia and superficial infections were comparable in both groups (2 cases vs 3 cases and 3 cases vs 2 cases, respectively). Hardware prominence was significantly higher in the olecranon osteotomy group, mostly due to tension band wiring.
Both approaches were equivalent, but there is a need for further study including higher numbers of subjects and longer study duration to prove the benefits of one approach over the other.
Core Tip: The classical olecranon osteotomy approach for intra-articular and extra-articular distal humerus fractures provides excellent visualization of the fracture and allows for optimal reduction and adequate fixation of the fracture fragments. However, several complications, such as nonunion and hardware backout, are associated with this approach. Therefore, an alternative approach, such as the triceps reflecting anconeus pedicle, was developed. This study determined that the triceps reflecting anconeus pedicle and olecranon osteotomy approaches are similarly efficacious for internal fixation of distal humeral intercondylar fractures. Additional studies with more patients and a longer follow-up period are needed to determine the best approach.
- Citation: Ailani R, Bhuyan SK, Prasad BK, Kumar A, Dawani N. Clinical outcomes of triceps reflecting anconeus pedicle and olecranon osteotomy approach for distal humerus intercondylar fractures. World J Orthop 2024; 15(6): 570-577
- URL: https://www.wjgnet.com/2218-5836/full/v15/i6/570.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i6.570
Distal humerus fractures are challenging injuries to treat. They constitute 2%-6% of all humeral fractures and 30% of all elbow injuries[1]. There is a bimodal age distribution with the first peak in young males caused by high-energy trauma and a second peak in elderly females over 60 caused by low-energy injuries[2]. Intercondylar fractures are intra-articular fractures that need anatomic reduction, rigid fixation, and early mobilization to achieve the optimal functional outcomes. With the advent of modern reconstructive techniques, implant design, and surgical approaches, open reduction and internal fixation with plates and screws is the preferred surgical option for most of these fractures[3].
Several posterior approaches for treating distal humerus fractures have been described in the literature. They include olecranon osteotomy, paratricipital (triceps-on), and triceps-off type approaches, such as triceps-splitting, triceps reflecting, triceps reflecting anconeus pedicle (TRAP), and the triceps tongue approach[4]. Each approach has its own advantages and disadvantages. Therefore, the selection of a particular approach depends on several factors including the degree of articular visualization, fracture characteristics, patient factors (elderly, low demand), and any associated injuries like triceps laceration or olecranon fracture[4].
Olecranon osteotomy (the MacAusland transolecranon approach) is recommended by many experts for wider exposure. However, nonunion at the osteotomy site, avascular necrosis, heterotopic ossification, failure of fixation, hardware prominence, and decreased range of motion are complications of this approach[5]. The TRAP approach, which is a combination of modified Kocher and Bryan-Morrey approaches, gives adequate exposure for fixation of these complex intercondylar fractures without compromising the anconeus innervation and posterolateral ligaments[5].
The purpose of this study was to compare clinical outcomes of the TRAP approach and the olecranon osteotomy approach to determine the best treatment for internal fixation of distal humeral intercondylar fractures.
This hospital-based prospective randomized interventional study was approved by our institutional ethics committee. In total, 46 cases of intercondylar distal humerus Arbeitsgemeinschaft für Osteosynthesefragen/Association of the Study of Internal Fixation (AO/ASIF) type C1, C2 and C3 fractures met the inclusion criteria and were initially included. Patients were included in this study if they met the following criteria: AO/ASIF type C fractures; age between 18 years to 70 years; closed and Gustilo grade I open fractures; no associated fractures in the same limb; and competent neurovascular status of the limb. Exclusion criteria included: Fractures more than 3 wk old; preexisting elbow stiffness; infected or grade II/III open fractures; pathological fractures; any associated fractures in the same limb; preexisting arthrosis or disability; psychiatric and polytrauma patients who were not able to rehabilitate in an appropriate time frame; and fractures with neurovascular injury. We recruited patients for this study from January 1, 2016 to August 30, 2020.
Patients were randomly allocated into groups based on computer-generated randomization plans. They were evenly divided into two groups: 23 patients were treated with the TRAP approach (TRAP group); and 23 patients were treated with the olecranon osteotomy approach (olecranon osteotomy group). Three patients dropped out of the olecranon osteotomy group, and two patients in the TRAP groups were lost to follow-up. One patient from the TRAP group was diagnosed with a peri-implant fracture and was excluded from the study. All operations were performed by senior surgeons and were followed up for a minimum period of 12 months.
We used 3.5 mm stainless steel (316L) nonlocking reconstruction plates contoured to fit the distal humerus and fixed in parallel configuration. The plates were different lengths in order to decrease the stress riser at the bone implant interface. Since the primary aim of the study was to compare the different approaches used for fracture fixation, the implant material, configuration, and design were standardized and fixed in both groups to remove any internal bias.
Postoperative mobilization was started on day 2 in the olecranon osteotomy group. It was started 1 wk after the removal of an anterior slab applied in full extension in the TRAP group. The patients were followed up at 6 wk, 3 months, 6 months, and 12 months, and comparison of the functional status was completed. Functional assessment was carried out using the Mayo Elbow Performance Score (MEPS) and Disability of Arm, Shoulder and Hand (DASH) score and measuring the flexion and extension range of the elbow. MEPS was described by Morrey et al[6] for evaluation of the results of treatment of elbow fractures and dislocations. It consists of assessment of pain, arc of motion, stability, and a patient rating of daily function. Pain is weighted highest. The scale ranges from 0 to 100, with a higher score indicating a better outcome. The DASH score is a 30-item, self-reported questionnaire with a total score range of 0 to 100[7]. A higher DASH score indicates greater disability.
Olecranon osteotomy approach: The patient was placed in the lateral decubitus position with the arm hanging free over a bolster. A 12-15 cm long midline posterior incision was performed with a lazy curve near the olecranon to avoid the tip of the olecranon in the incision line. The incision was carried down to the level of the deep fascia and triceps tendon. Full thickness fasciocutaneous flap was elevated extending medially and laterally to the supracondylar ridges. The ulnar nerve was identified and dissected free of its surrounding tissues, then gently retracted. Then, the bare area, which is the nonarticular portion of the greater sigmoid notch, was identified by subperiosteal dissection along the medial and lateral sides of the olecranon. An apex distal chevron osteotomy entering into the bare area was performed with the help of saw and osteotomes. After osteotomy, the olecranon fragment along with the triceps tendon and musculature was elevated from the posterior surface of the humerus. Finally, fracture reduction and fixation were performed. In our study, fixation of the osteotomy was done by tension band wiring using K-wires.
TRAP approach: The TRAP method is essentially the same as the olecranon osteotomy approach until the identification and dissection of the ulnar nerve, which is next to the deep exposure and involves combined approaches from the lateral and medial sides of the elbow. In our series, we exposed from the lateral side first, then from the medial side, but it can be started from any side. The lateral exposure was completed by making an incision about 10 cm distal to the tip of olecranon in the interval between the anconeus and extensor carpi ulnaris and extended up toward the lateral epicondyle and supracondylar ridge.
After incision in the septa between the anconeus and extensor carpi ulnaris, the anconeus was subperiosteally elevated from the ulna distally and separated from the annular ligament and lateral collateral ligament complex proximally. In the medial aspect, the exposure was completed by starting 10 cm distal to the tip of olecranon at a point corresponding to the distal most extent of the anconeus muscle attachment. An incision was made in the periosteum on the subcutaneous border of the ulna, which was continued proximally along the edge of the flexor carpi ulnaris origin. Then, the peri
Then, the triceps was released from the olecranon and reflected laterally. The critical area of triceps insertion was approximately 1 cm in diameter on the olecranon in line with the intramedullary long axis of the ulna. It was marked by a suture placed in the Sharpey fibers so that it could be reattached to the olecranon with a proper length-tension relationship. The fascial and periosteal attachments of the distal anconeus were released, and the entire triceps and anconeus pedicle was reflected proximally exposing the distal humerus. At the completion of fracture fixation, the triceps was attached to the olecranon in the critical area by heavy nonabsorbable sutures through two oblique drill holes in the ulna.
The data were analyzed using Statistical Package for Social Sciences version 22.0 (IBM Corp., Armonk, NY, United States). Categorical variables were presented as numbers and percentages. The χ2 test was used to analyze the difference between two groups for the categorical variables. The continuous variables like MEPS, DASH score, and range of motion were presented as mean and standard deviation and compared between two groups by independent t-test. A P value of ≤ 0.05 was assumed to be statistically significant.
During the study period, there were 58 cases of intercondylar fractures of the distal humerus. Of them, 12 cases were excluded from the study due to Gustilo and Anderson grade 2 or 3 open fractures in 5 cases, ipsilateral limb fractures (distal radius fractures) in 4 cases, and older age (> 70 years) in 3 cases.
The mean age of patients was 43.2 years in the TRAP group and 37.5 years in the olecranon osteotomy group. The most common mechanism of injury was fall. Most fractures were AO/ASIF type C2 with a simple articular pattern but comminution in metaphysis. The mean operative time of surgery was 119.5 min in the TRAP group and 111.3 min in the olecranon osteotomy group, showing a statistically significant difference (P = 0.0067). The mean duration of hospital stay was 9.85 d in the TRAP group and 5.45 d in the olecranon osteotomy group, which also showed a statistically significant difference (P = 0.0001; Table 1).
| Parameters | TRAP group, n = 20 | Olecranon osteotomy group, n = 20 | P value |
| Male:female ratio, n | 8:12 | 11:9 | > 0.05 |
| Age in yr, mean (range) | 43.2 (18-58) | 37.45 (21-55) | < 0.05 |
| Mechanism of injury | |||
| Fall, n (%) | 16 (80) | 14 (70) | < 0.05 |
| Road traffic accident, n (%) | 4 (20) | 6 (30) | |
| AO/ASIF fracture type | |||
| Type C1 | 7 | 7 | > 0.05 |
| Type C2 | 11 | 9 | |
| Type C3 | 3 | 3 | |
| Intraoperative time in min, mean | 119.5 | 111.45 | < 0.05 |
| Hospital stay in d, mean | 9.85 | 5.45 | < 0.05 |
| Time taken for union in wk, mean (range) | 13.05 (10-16) | 12.85 (10-15) | > 0.05 |
| Complications, n | |||
| Ulnar nerve paresthesia | 2 | 3 | > 0.05 |
| Hardware prominence | 2 | 5 | < 0.05 |
| Infection | 3 | 2 | > 0.05 |
The average time taken for union was 13.05 wk in the TRAP group and 12.85 wk in the olecranon osteotomy group, with no statistically significant difference between the two approaches (P = 0.6700). Out of 40 patients, 5 patients developed ulnar nerve paresthesia (2 in the TRAP group and 3 in the olecranon osteotomy group). All patients recovered spontaneously within a 3-month period. Three patients in the TRAP group and two patients in the olecranon osteotomy group developed superficial infections and consequently received treatment by oral antibiotics. Hardware prominence occurred more in the olecranon osteotomy group.
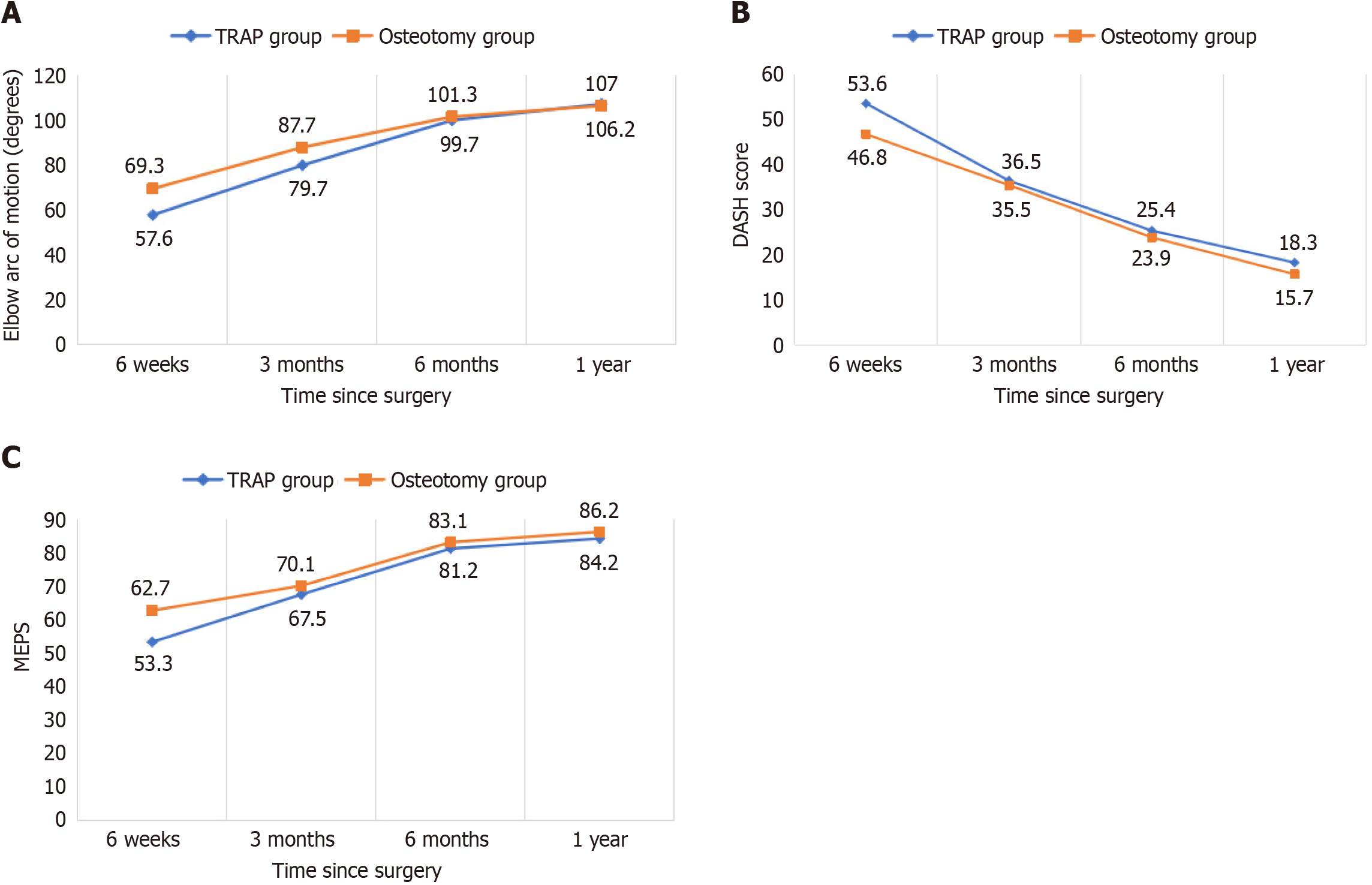
The functional outcomes were compared during the follow-up period. At 6 wk, range of motion, DASH score, and MEPS were significantly better in the olecranon osteotomy group (P < 0.05). After this 6 wk period, all parameters were comparable in both groups. At the 1-year follow-up, the mean range of flexion-extension was 11.00 to 118.00 degrees and 12.00 to 118.25 degrees (P > 0.05), mean arc of motion was 107.00 degrees and 106.25 degrees (P > 0.05), mean DASH score was 18.3 and 15.7 (P > 0.05), and MEPS was 84.2 and 86.2 (P > 0.05) in the TRAP group and the olecranon osteotomy group, respectively (Table 2). At the 1-year follow-up, 75% of the patients in the TRAP group and 85% of the patients in the olecranon osteotomy group had excellent to good outcomes (Table 3). Figure 1 demonstrate the improvement of functional outcomes at each follow-up in each group.
| Follow-up time point | TRAP group, n = 20 | Osteotomy group, n = 20 | ||||
| Arc of motion | DASH | MEPS | Arc of motion | DASH | MEPS | |
| 6 wk | 57.6 ± 3.4 | 53.6 ± 3.9 | 53.3 ± 2.9 | 69.3 ± 3.3 | 46.8 ± 4.1 | 62.7 ± 2.1 |
| 3 months | 79.7 ± 4.1 | 36.5 ± 4.2 | 67.5 ± 2.7 | 87.7 ± 3.9 | 35.5 ± 3.7 | 70.1 ± 2.8 |
| 6 months | 99.7 ± 3.7 | 25.4 ± 4.9 | 81.2 ± 3.3 | 101.3 ± 4.9 | 23.9 ± 3.8 | 83.1 ± 3.5 |
| 1 yr | 107.0 ± 3.5 | 18.3 ± 4.7 | 84.2 ± 2.9 | 106.2 ± 3.8 | 15.7 ± 3.9 | 86.2 ± 3.1 |
| MEPS | TRAP, n = 20 | Olecranon osteotomy, n = 20 | P value |
| Excellent | 14 (70) | 15 (75) | > 0.05 |
| Good | 3 (5) | 2 (10) | > 0.05 |
| Fair | 2 (10) | 2 (10) | > 0.05 |
| Poor | 1 (5) | 1 (5) | > 0.05 |
Open reduction and plate osteosynthesis through the posterior approach of the elbow is the most widely accepted treatment method for distal humerus intercondylar fractures. There are various approaches involving a posterior method for the exposure and fixation of the humeral intercondylar fractures. However, the best approach is still a matter of debate and is generally determined by surgeon’s preference and experience.
The paratricipital approach has the advantage of avoiding olecranon osteotomy and triceps reflection, but it provides limited exposure. Wilkinson et al[8] mentioned that the olecranon osteotomy approach provides the greatest exposure of the articular surface for intra-articular fractures. Patiño et al[9] concluded that the paratricipital approach allows good access to the fracture focus with no disruption of the extensor mechanism and early rehabilitation with acceptable results. However, their series of 12 patients only had 5 patients with intra-articular fractures, and no patients had an AO/ASIF type C3 fracture.
Triceps-splitting or triceps-peeling approaches have negative effects on muscle strength due to the potential for wea
We compared the functional outcomes in distal intercondylar fractures treated with either the TRAP or olecranon osteotomy approach. In our study, the mean MEPS at the 1-year follow-up was 84.2 and 86.2 in the TRAP and olecranon osteotomy groups, respectively, and there was no significant difference upon statistical analysis. Also, 75% and 85% of the patients had good to excellent outcomes according to MEPS, respectively. Azboy et al[12] retrospectively found similar mean MEPS in both groups as well (85.9 and 83.5, respectively). Those authors followed the patients for up to 3 years and found that 81.9% and 77.7% of the patients had good to excellent MEPS in the TRAP group and olecranon osteotomy group, respectively. This slight difference in results may be explained by arthritic changes in the olecranon osteotomy group that is evident only on longer follow-up.
Mishra et al[13] in 2010 and Chou et al[14] in 2016 determined that MEPS was 85 and 81 after the TRAP approach, respectively. Similarly, Chen et al[15] in 2011 and Zhang et al[16] in 2013 found that MEPS was 82.4 and 85.9 after the olecranon osteotomy approach, respectively. The DASH score in our study at the 1-year follow-up was 18.3 and 15.7 in the TRAP and olecranon osteotomy groups, respectively. Azboy et al[12] found comparable scores of 15.6 and 20.1 in their groups, respectively.
The average flexion-extension arc was also comparable in both groups at the 1-year follow-up (107.00° and 106.25° for the TRAP group and olecranon osteotomy group, respectively). Azboy et al[12], Chou et al[14], and Mishra et al[13] observed similar arc of flexion-extension (108°, 127°, and 101.5°, respectively) after the TRAP approach. Similarly, Azboy et al[12], Chen et al[15], Elmadag et al[17], Zhang et al[16], and Mckee et al[18] found that the flexion-extension arc of motion was 98.0°, 111.0°, 99.3°, 103.2°, and 102.7°, respectively, in the olecranon osteotomy group.
The mean operative time for the TRAP group (119.5 min) was significantly more than that for the olecranon osteotomy group (111.5 min) in our study. This was probably due to limited expertise with the TRAP approach in our institution and related to the higher learning curve of this approach. After a thorough literature search, we could not find any other studies mentioning the duration of surgery using the TRAP approach.
The duration of hospital stay in the TRAP group was significantly higher than that of the olecranon osteotomy group because the patients in the TRAP group were not mobilized until after 7 d after the removal of the slab. The time taken for radiological union (10-16 wk) in our study was comparable to the other studies irrespective of the approach used[5,10,19,20]. In this study, the complication rate was similar in both groups except for hardware prominence, which was significantly higher in the olecranon osteotomy group. This was mainly because of the additional implants used for the olecranon osteotomy procedure and thin subcutaneous placement of K-wires used to fix the osteotomy as compared to the TRAP group. The overall complication rate in our study was comparable to that in other studies[4,12,13].
Like any scientific study, our study had limitations. First, the sample size was relatively small. A larger sample size could be more enlightening and may be able to conclusively prove superiority of one approach over another. Second, blinding was not possible at the patient and investigator level. Third, our follow-up was of limited duration, which may have obscured the complications arising due to the effect of arthritis development at the site of olecranon osteotomy. Continued stresses on the implant due to repeated movement may lead to stress failure of the plates as well. Therefore, further development in metallurgy, implant design, and incorporation of computational simulation studies may provide us further insight into the implant stresses and thus provide novel methods to improve patient outcomes[21].
Intercondylar humerus fracture treatment demands careful preoperative planning. Open reduction and internal fixation with plate osteosynthesis through the posterior approach is the preferred method for most surgeons. TRAP and olecranon osteotomy both provide good visualization of the articular surface. Although functional outcomes significantly lag behind in the TRAP group in the initial follow-up, final outcomes are similar in both groups. In our study we found a significantly greater hardware prominence in the olecranon osteotomy approach. There is a need for further prospective randomized controlled studies for the comparison of both approaches that involve a significantly larger number of subjects for a longer duration to prove the further clinical utility of these approaches in the treatment of these fractures.
| 1. | Sharma S, John R, Dhillon MS, Kishore K. Surgical approaches for open reduction and internal fixation of intra-articular distal humerus fractures in adults: A systematic review and meta-analysis. Injury. 2018;49:1381-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Robinson CM, Hill RM, Jacobs N, Dall G, Court-Brown CM. Adult distal humeral metaphyseal fractures: epidemiology and results of treatment. J Orthop Trauma. 2003;17:38-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 222] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 3. | Zalavras CG, Papasoulis E. Intra-articular fractures of the distal humerus-a review of the current practice. Int Orthop. 2018;42:2653-2662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Athwal GS. Distal humerus fractures. In: Charles MC, James DH, Margaret MM, William MR, Paul T, editors. Rockwood and Green's Fractures in Adults. 8th ed. Philadelphia: Wolters Kluwer, 2015: 124-1286. |
| 5. | Ozer H, Solak S, Turanli S, Baltaci G, Colakoğlu T, Bolukbasí S. Intercondylar fractures of the distal humerus treated with the triceps-reflecting anconeus pedicle approach. Arch Orthop Trauma Surg. 2005;125:469-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Morrey BF, An KN, Chao EYS. Functional evaluation of the elbow. In: Morrey BF, editor. The Elbow and Its Disorders. 2nd ed. Philadelphia, PA: WB Saunders Co, 1993: 95. |
| 7. | Kennedy CA, Beaton DE, Solway S, McConnell S, Bombardier C. The DASH outcome measure user's manual. 3rd ed. Torronto: Institute for work & Health, 2011. |
| 8. | Wilkinson JM, Stanley D. Posterior surgical approaches to the elbow: a comparative anatomic study. J Shoulder Elbow Surg. 2001;10:380-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 158] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 9. | Patiño JM, Rullan Corna AF, Abdon IM, Michelini AE, Mora Pulido DA. Paratricipital approach for distal humerus fractures. Musculoskelet Surg. 2021;105:155-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 10. | Pankaj A, Mallinath G, Malhotra R, Bhan S. Surgical management of intercondylar fractures of the humerus using triceps reflecting anconeus pedicle (TRAP) approach. Indian J Orthop. 2007;41:219-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Coles CP, Barei DP, Nork SE, Taitsman LA, Hanel DP, Bradford Henley M. The olecranon osteotomy: a six-year experience in the treatment of intraarticular fractures of the distal humerus. J Orthop Trauma. 2006;20:164-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 107] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 12. | Azboy İ, Bulut M, Ancar C, Demirtaş A, Özkul E, Gem M, Karadeniz H, Arslan H. The comparison of triceps-reflecting anconeus pedicle and olecranon osteotomy approaches in the treatment of intercondylar fractures of the humerus. Ulus Travma Acil Cerrahi Derg. 2016;22:58-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Mishra P, Aggarwal A, Rajgopalan M, Dhammi I, Jain AK. Critical analysis of triceps-reflecting anconeus pedicle (TRAP) approach for operative management of intra-articular distal humerus fractures. J Clin Orthop Trauma. 2010;1:71-80. [DOI] [Full Text] |
| 14. | Chou YC, Hsu YH, Yu YH, Wu CC. Triceps-reflecting anconeus pedicle approach with double precontoured locking plate fixation is efficient in the treatment of orthopaedic trauma association type C distal humerus fracture. Injury. 2016;47:2240-2246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Chen G, Liao Q, Luo W, Li K, Zhao Y, Zhong D. Triceps-sparing versus olecranon osteotomy for ORIF: analysis of 67 cases of intercondylar fractures of the distal humerus. Injury. 2011;42:366-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Zhang C, Zhong B, Luo CF. Comparing approaches to expose type C fractures of the distal humerus for ORIF in elderly patients: six years clinical experience with both the triceps-sparing approach and olecranon osteotomy. Arch Orthop Trauma Surg. 2014;134:803-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | Elmadag M, Erdil M, Bilsel K, Acar MA, Tuncer N, Tuncay I. The olecranon osteotomy provides better outcome than the triceps-lifting approach for the treatment of distal humerus fractures. Eur J Orthop Surg Traumatol. 2014;24:43-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | McKee MD, Wilson TL, Winston L, Schemitsch EH, Richards RR. Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approach. J Bone Joint Surg Am. 2000;82:1701-1707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 148] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 19. | Tyllianakis M, Panagopoulos A, Papadopoulos AX, Kaisidis A, Zouboulis P. Functional evaluation of comminuted intra-articular fractures of the distal humerus (AO type C). Long term results in twenty-six patients. Acta Orthop Belg. 2004;70:123-130. [PubMed] |
| 20. | Huang TL, Chiu FY, Chuang TY, Chen TH. The results of open reduction and internal fixation in elderly patients with severe fractures of the distal humerus: a critical analysis of the results. J Trauma. 2005;58:62-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 102] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 21. | Farooq MU, Anwar S, Bhatti HA, Kumar MS, Ali MA, Ammarullah MI. Electric Discharge Machining of Ti6Al4V ELI in Biomedical Industry: Parametric Analysis of Surface Functionalization and Tribological Characterization. Materials (Basel). 2023;16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |