Published online Apr 18, 2024. doi: 10.5312/wjo.v15.i4.379
Revised: February 7, 2027
Accepted: April 2, 2024
Published online: April 18, 2024
Processing time: 140 Days and 7 Hours
De-Quervain’s tenosynovitis is a disorder arising from the compression and irritation of the first dorsal extensor compartment of the wrist. Patients who fail conservative treatment modalities are candidates for surgical release. However, risks with surgery include damage to the superficial radial nerve and an incom
To describe the location of the first dorsal compartment in relation to bony surface landmarks to create replicable surgical incisions.
Six cadaveric forearms, including four left and two right forearm specimens were dissected. Dissections were performed by a single fellowship trained upper extremity orthopaedic surgeon. Distance of the first dorsal compartment from landmarks such as Lister’s tubercle, the wrist crease, and the radial styloid were calculated. Other variables studied included the presence of the superficial radial nerve overlying the first dorsal compartment, additional compartment sub-sheaths, number of abductor pollicis longus (APL) tendon slips, and the presence of a pseudo-retinaculum.
Distance from the radial most aspect of the wrist crease to the extensor retin
An incision that measures 3 mm proximal from the radial styloid, 2 cm radial from Lister’s tubercle, and 5 mm proximal from the radial wrist crease will safely place surgeons at the first dorsal compartment.
Core Tip: Surgical release of the first extensor compartment at the level of the wrist has been well documented with multiple different techniques. Injury to the superficial radial nerve, decompressing the incorrect compartment, tendon injury, and incomplete release of the compartment leads to patient morbidity. We describe the precise anatomic location of the first dorsal compartment in relation to bony surface landmarks to create replicable surgical incisions. We demonstrate the location of the superficial radial nerve and document the variances in the first compartment sub-sheaths. In doing so, we have created a surgical protocol that will ensure a complete first compartment release.
- Citation: Thandoni A, Yetter WN, Regal SM. Anatomic location of the first dorsal extensor compartment for surgical De-Quervain’s tenosynovitis release: A cadaveric study. World J Orthop 2024; 15(4): 379-385
- URL: https://www.wjgnet.com/2218-5836/full/v15/i4/379.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i4.379
De-Quervain’s tenosynovitis is a common pathology of the wrist resulting in thickening of the synovial sheath and extensor retinaculum containing the first dorsal extensor compartment[1]. Subsequent irritation of the first dorsal compartment, containing the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons, leads to radial sided wrist pain and inflammation[2]. Repetitive grasping and twisting motions of the hand and wrist leads to increased inflammation along with decreased functional use of the wrist. Initial non-operative management of De-Quervain’s tenosynovitis includes the use of over-the-counter anti-inflammatory medications, supportive thumb spica bracing, and corticosteroid injections[3,4]. Failure of these conservative measures warrants surgical intervention[2-4].
Surgical release of the first extensor compartment is the standard of care following failure of conservative treatment modalities. Various surgical techniques have been described in the literature to ensure a complete release of the com
Interestingly, multiple anatomic variants and sub-sheaths within the compartment itself can hinder a complete surgical release and resolution of clinical symptoms. Cadaveric studies have documented varying numbers of tendons and tendon slips of the APL in the first dorsal compartment[16-18]. Differing numbers of subsheaths and septi between tendons were found once the compartment was exposed, requiring further dissection to ensure a complete release of all constricting factors on the tendon sheath[18-20].
However, there is currently a paucity of literature that accurately demonstrates the exact anatomic location of the first dorsal compartment at the level of the wrist[21,22]. The inability to accurately replicate a reliable surgical incision into the first compartment places the superficial radial nerve at risk and may lead to inadequate releases based on sub-sheath vari
The aim of this study is to determine the precise anatomic location of the first dorsal compartment in relation to bony surface landmarks in order to create reliable and replicable surgical incisions. Secondary aims of this project are to document the location of the superficial radial nerve and to document the variances in the first compartment sub-sheaths. In doing so, our aim is to create a surgical protocol that will ensure a complete first compartment release without injury to the surrounding neurovascular structures when treating De-Quervain’s tenosynovitis.
Six cadaveric forearms were obtained to perform this study including four left and two right forearm specimens. All specimens included the entire forearm and hand from the proximal ulna to the fingertips. In total, four cadavers were male and two were female. All cadaver specimens were obtained from different individuals. Cadaver specifications included age ranges from thirty to sixty years of age. The two right forearm specimens were from a sixty-year-old male and a thirty-seven-year-old female specimen. Of the four left forearm specimens, three were from male cadavers while one forearm was from a female cadaver. The age ranges for the left forearm cadavers included a fifty-five-year-old male, fifty-eight-year-old male, thirty-three-year-old male, and a thirty-two-year-old female.
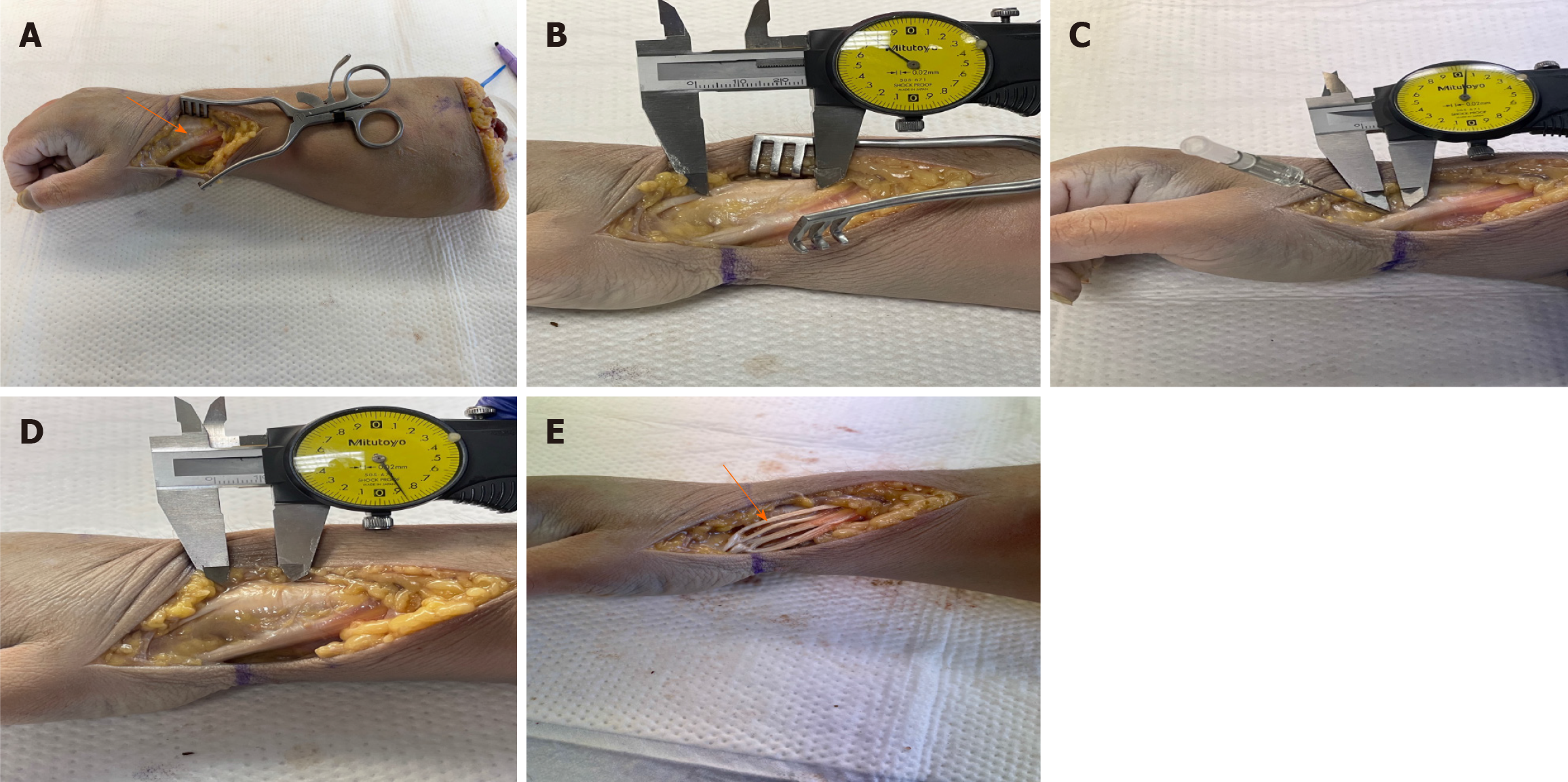
Inclusion criteria for our study included cadaver models within age ranges of 30-60 with no prior trauma history or surgical intervention to the wrist and hand region that would otherwise confound results from a soft tissue standpoint. Exclusion criteria included cadavers with prior history of wrist or hand surgical intervention. Cadavers with a history of surgical history including retained hardware, prior fractures, history of skin grafting, or soft tissue or bony trauma were excluded. All specimens included the entire forearm and hand from the proximal ulna to the fingertips. Any specimens with evidence of prior amputations related to trauma or vascular disease were excluded. Fresh frozen cadaveric forearms were thawed only once at which time all surgical dissections were undertaken (Figure 1). The cadaveric forearms were purchased using institutional research funding.
All cadaveric dissections and data measurements were performed by a single fellowship trained hand and upper ext
Various data points were obtained to maximize a reproducible surgical site incision over the first dorsal compartment. The length of the distal phalanx of the thumb and the distance from the thumb distal interphalangeal joint to the tip of the digit were two topographical data points that were collected. Creating an incision centered over the first dorsal compartment based on those two measurements was analyzed to determine the proximity of those values to the extensor retinaculum. The overall length of the extensor retinaculum was obtained and served as a key measurement that allowed comparison measurements from other landmarks (Figure 2A). Other landmarks of interest included Lister’s tubercle, the wrist crease, and the radial styloid. Obtaining distances from each of these landmarks to the extensor retinaculum were obtained to determine which data points reliably placed our incision over the first dorsal compartment (Figure 2B-D). Important other parameters that were documented included the presence or absence of the superficial radial nerve overlying the first dorsal compartment, additional compartment sub-sheaths, number of APL tendon slips, and the presence of a pseudoretinaculum (Figure 2E). All measurements were obtained using the same methodology in each cadaveric forearm.
Cadaveric measurement data were analyzed using descriptive statistics. The mean, standard deviation and standard error values were calculated manually using standard equations. Confidence intervals were then computed manually using standard formulas prior to the creation of the data figures and tables. Statistical review of the study was performed by a biomedical statistical team at our home institution.
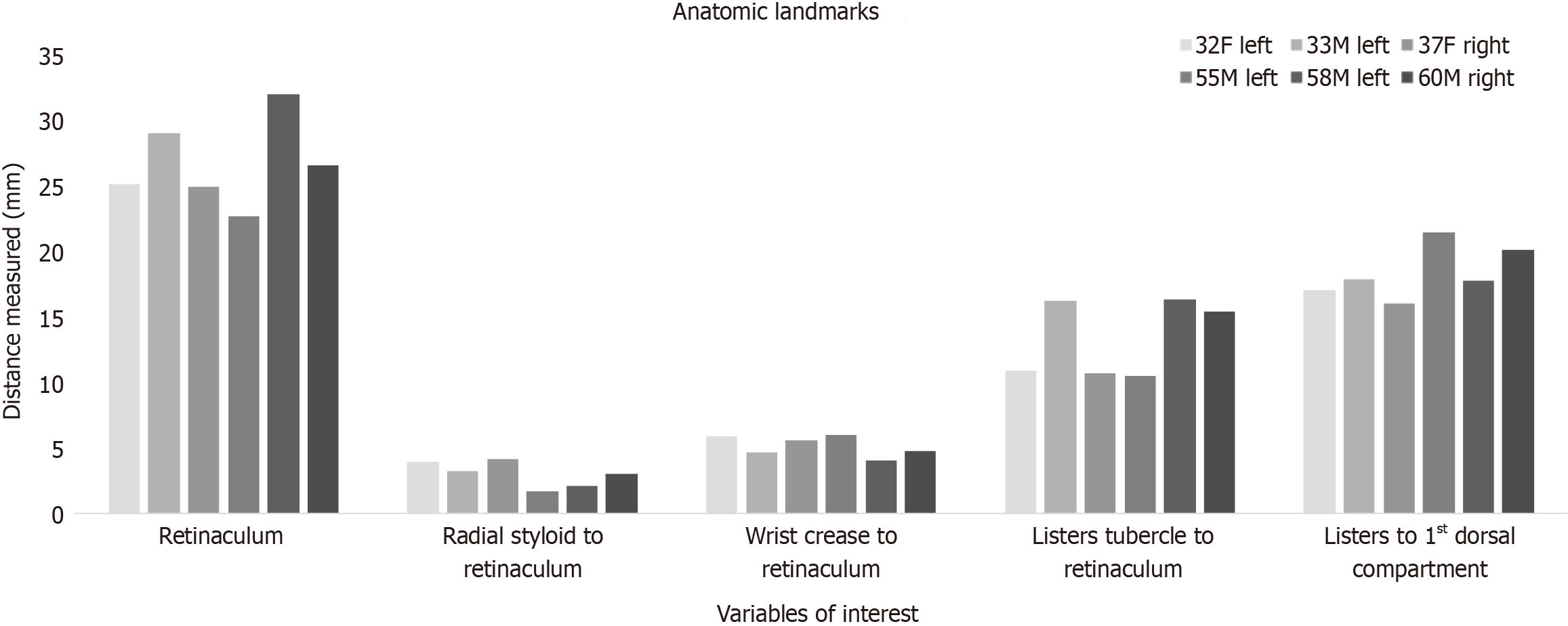
Data points from all six cadavers were analyzed to determine the overall distribution of each variable of interest (Figure 1). Data gathered remained in proximity within each variable analyzed as no significant outliers were seen after histogram analysis (Figure 1). All measurements from the six cadavers were also averaged prior to comparison amongst the other data points. The average length of the thumb distal phalanx was 30.11 mm ± 3.39 mm while the average length of the distal phalanx crease to the tip of the digit was 30.70 mm ± 3.74 mm. The average length of the extensor retinaculum from its proximal to its distal length was 26.82 mm ± 3.34 mm. Therefore, the length from the thumb interphalangeal joint to the thumb tip gives a reasonable estimate of about 3 mm and can be used as a measurement to determine the overall length of the extensor retinaculum. The distance from the radial most aspect of the wrist crease to the retinaculum was 5.14 mm ± 0.80 mm. The distance from Lister’s tubercle to the proximal aspect of the retinaculum measured 13.37 mm ± 2.94 mm while distance from Lister’s tubercle to the start of the first dorsal compartment was 18.43 mm ± 2.01 mm. The length from the radial styloid to the initial aspect of the extensor retinaculum measured 2.98 mm ± 0.99 mm (Table 1).
| Anatomic landmarks | Mean (mm) | SD | N | SE | 95%CI |
| Distal phalanx | 30.11 | 3.39 | 6 | 1.38 | (27.40-32.82) |
| Distal phalanx crease to tip of finger | 30.70 | 3.74 | 6 | 1.52 | (27.71-33.68) |
| Retinaculum | 26.82 | 3.34 | 6 | 1.37 | (24.14-29.49) |
| Radial styloid to retinaculum | 2.98 | 0.99 | 6 | 0.40 | (2.18-3.77) |
| Superficial radial nerve crossing proximal to retinaculum | 10.20 | 4.48 | 2 | 3.17 | (3.99-16.40) |
| Wrist crease to retinaculum | 5.14 | 0.80 | 6 | 0.33 | (4.50-5.78) |
| Listers tubercle to retinaculum | 13.37 | 2.94 | 6 | 1.20 | (11.02-15.73) |
| Listers tubercle to 1st dorsal compartment | 18.43 | 2.01 | 6 | 0.82 | (16.82-20.04) |
| Separate EPB compartment | 0.66 | N/A | 6 | N/A | |
| Number of APL slips | 3.00 | 0.63 | 6 | 0.26 | (2.49-3.51) |
| Pseudo-retinaculum | N/A | N/A | 4 | N/A |
Only two cadavers had a superficial radial nerve that crossed over the first dorsal compartment. In two cadaver spec
De-Quervain’s tenosynovitis warrants surgical intervention in patients who continue to suffer from significant wrist pain and decreased function after failing conservative modalities including physical therapy, anti-inflammatory medications, and corticosteroid injections. Surgical release of the first extensor compartment at the level of the wrist has been well documented with multiple different techniques implementing either longitudinal or transverse incisions. Risk of iatrogenic injury to the superficial radial nerve, decompressing the incorrect compartment, tendon injury, and incomplete release of the compartment can lead to significant patient morbidity. Currently, there has not been a documented repro
Wilhelmi et al[23] demonstrated that the distance from the palmar digital crease to the proximal interphalangeal crease (mean, 2.42 cm ± 0.03 cm) correlated to the distance of the proximal edge of the A1 pulley from the digital palmar crease (mean, 2.45 cm ± 0.03 cm). They determined that surface landmark ratios can be a reliable and reproducible tool that can lead to successful A1 pulley release without complication in trigger finger surgery[23]. Hazani et al[21] performed a bony landmark cadaveric study that mapped out and demonstrated that the radial styloid is 0.32 cm ± 0.57 cm from the distal edge of the extensor retinaculum.
Our study demonstrated that the radial styloid was similarly only 2.98 mm ± 0.99 mm from the distal aspect of the retinaculum. Notably, we also noted that Lister’s tubercle is only 13.37 mm ± 2.94 mm from the proximal aspect of the retinaculum and 18.43 mm ± 2.01 mm from the first compartment itself. The most radial aspect of the wrist crease is only about 5 mm distal to the retinaculum as well. The length from the thumb interphalangeal joint to the thumb tip provides an estimate of about 3 mm for the entire distance from the radial styloid to the end of the retinaculum. Thus, any incision extending 3 cm distal to the radial styloid will place the surgeon at end of the retinaculum, establishing a complete release. Ultimately, placing an incision 3 mm from the radial styloid, 2 cm from Lister’s tubercle, and 5 mm from the radial wrist crease can be used to safely place the incision at the level of the first dorsal compartment.
Matzon et al[24] demonstrated the common presence of multiple APL slips in 78% of patients and found that 55% of patients had two subsheaths while 8% had three subsheaths. Kulthanan and Chareonwat[25] re-affirmed those results and demonstrated in contrast that the EPB had a single tendon in 98% of cases. Their study demonstrated that the APL had multiple slips in 89% of cases (P < 0.001)[25]. Our cadaver forearms had a mean of 3 separate APL slips, with mul
Importantly, Samarakoon et al[12] found that the superficial radial nerve branches 5.1 cm proximal to the radial styloid. They also found that the superficial radial nerve can branch 0.4 cm from the center of the first dorsal compartment and 1.6 cm from Lister’s tubercle[12]. Gurses et al[11] found that the lateral dorsal digital branch to the thumb, off of the superficial radial nerve, coursed directly over the first dorsal compartment in 8 out of 20 cadavers. In our study, we found the superficial radial nerve present in close proximity in only 2 out of the 6 cadavers (7.03 mm and 13.36 mm proximal to the retinaculum). The other four dissections did not demonstrate a clear superficial radial nerve nearby our surgical site. However, if the superficial bony landmark measurements stated above are followed, we anticipate that the superficial radial nerve will not be encountered as unnecessary dissection will not be undertaken.
The main limitation of our study includes the small sample size. We were only able to perform six cadaveric diss
Superficial landmarks are a reliable way to create a reproducible incision over the first dorsal compartment in order to obtain a complete release and protect the superficial radial nerve. Creating an incision that measures 3 mm proximal from the radial styloid, 2 cm proximal from Lister’s tubercle, and 5 mm radial from the radial wrist crease will safely place surgeons at the level of the first dorsal compartment. Extending the incision 3 cm proximal to the radial styloid will fully encompass the extensor retinaculum and allow for a complete release. The APL tendon does reliably have multiple slips and the EPB does contain multiple sub-sheaths in the majority of cases, which are important anatomic variants to be cognizant of intra-operatively.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gocmen-Mas N, Turkey S-Editor: Luo ML L-Editor: A P-Editor: Zhao YQ
| 2. | Goel R, Abzug JM. de Quervain's tenosynovitis: a review of the rehabilitative options. Hand (N Y). 2015;10:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Ilyas AM, Ast M, Schaffer AA, Thoder J. De quervain tenosynovitis of the wrist. J Am Acad Orthop Surg. 2007;15:757-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 128] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 4. | Oh JK, Messing S, Hyrien O, Hammert WC. Effectiveness of Corticosteroid Injections for Treatment of de Quervain's Tenosynovitis. Hand (N Y). 2017;12:357-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Gundes H, Tosun B. Longitudinal incision in surgical release of De Quervain disease. Tech Hand Up Extrem Surg. 2005;9:149-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Ostric SA, Martin WJ, Derman GH. Intersecting the intersection: a reliable incision for the treatment of de Quervain's and second dorsal compartment tenosynovitis. Plast Reconstr Surg. 2007;119:2341-2342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Abrisham SJ, Karbasi MH, Zare J, Behnamfar Z, Tafti AD, Shishesaz B. De qeurvian tenosynovitis: clinical outcomes of surgical treatment with longitudinal and transverse incision. Oman Med J. 2011;26:91-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Poublon AR, Kleinrensink GJ, Kerver A, Coert JH, Walbeehm ET. Optimal surgical approach for the treatment of Quervains disease: A surgical-anatomical study. World J Orthop. 2018;9:7-13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Croutzet P, Guinand R, Mares O, Apard T, Candelier G, David I. Ultrasound-Guided de Quervain's Tendon Release, Feasibility, and First Outcomes. J Wrist Surg. 2019;8:513-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Güleç A, Türkmen F, Toker S, Acar MA. Percutaneous Release of the First Dorsal Extensor Compartment: A Cadaver Study. Plast Reconstr Surg Glob Open. 2016;4:e1022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Gurses IA, Coskun O, Gayretli O, Kale A, Ozturk A. The relationship of the superficial radial nerve and its branch to the thumb to the first extensor compartment. J Hand Surg Am. 2014;39:480-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 12. | Samarakoon LB, Lakmal KC, Thillainathan S, Bataduwaarachchi VR, Anthony DJ, Jayasekara RW. Anatomical relations of the superficial sensory branches of the radial nerve: a cadaveric study with clinical implications. Patient Saf Surg. 2011;5:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Suresh SS, Zaki H. De quervain disease: Ibri technique to avoid superficial radial nerve injury. Tech Hand Up Extrem Surg. 2009;13:113-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Robson AJ, See MS, Ellis H. Applied anatomy of the superficial branch of the radial nerve. Clin Anat. 2008;21:38-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 74] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | Ikiz ZA, Uçerler H. Anatomic characteristics and clinical importance of the superficial branch of the radial nerve. Surg Radiol Anat. 2004;26:453-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Shiraishi N, Matsumura G. Anatomical variations of the extensor pollicis brevis tendon and abductor pollicis longus tendon--relation to tenosynovectomy. Okajimas Folia Anat Jpn. 2005;82:25-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Nam YS, Doh G, Hong KY, Lim S, Eo S. Anatomical study of the first dorsal extensor compartment for the treatment of de Quervain's disease. Ann Anat. 2018;218:250-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Sugiura S, Matsuura Y, Kuniyoshi K, Nishikawa S, Toyooka T, Mori C, Suzuki T. Anatomic study of the first extensor compartment and the relationship between the extensor tendon width and its distal insertion. Surg Radiol Anat. 2017;39:1223-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Xu H, Wu JX, Wang Q, Gao ZY. Anatomical variations in the first extensor compartment: a cadaver study. ANZ J Surg. 2018;88:913-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Lee ZH, Stranix JT, Anzai L, Sharma S. Surgical anatomy of the first extensor compartment: A systematic review and comparison of normal cadavers vs. De Quervain syndrome patients. J Plast Reconstr Aesthet Surg. 2017;70:127-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 21. | Hazani R, Engineer NJ, Cooney D, Wilhelmi BJ. Anatomic landmarks for the first dorsal compartment. Eplasty. 2008;8:e53. [PubMed] |
| 22. | Rousset P, Vuillemin-Bodaghi V, Laredo JD, Parlier-Cuau C. Anatomic variations in the first extensor compartment of the wrist: accuracy of US. Radiology. 2010;257:427-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 23. | Wilhelmi BJ, Snyder N 4th, Verbesey JE, Ganchi PA, Lee WP. Trigger finger release with hand surface landmark ratios: an anatomic and clinical study. Plast Reconstr Surg. 2001;108:908-915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Matzon JL, Graham JG, Lutsky KF, Takei TR, Gallant GG, Beredjiklian PK. A Prospective Evaluation of the Anatomy of the First Dorsal Compartment in Patients Requiring Surgery for De Quervain's Tenosynovitis. J Wrist Surg. 2019;8:380-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Kulthanan T, Chareonwat B. Variations in abductor pollicis longus and extensor pollicis brevis tendons in the Quervain syndrome: a surgical and anatomical study. Scand J Plast Reconstr Surg Hand Surg. 2007;41:36-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |