Published online Mar 18, 2024. doi: 10.5312/wjo.v15.i3.293
Peer-review started: December 14, 2023
First decision: December 23, 2023
Revised: December 26, 2023
Accepted: February 8, 2024
Article in press: February 8, 2024
Published online: March 18, 2024
Processing time: 90 Days and 15.3 Hours
Knee and hip osteoarthritis affects millions of people around the world and is expected to rise even more in frequency as the population ages. Joint arthroplasty is the surgical management of choice in these articulations. Heterotopic ossi
To compare pulsed lavage to standard lavage in joint arthroplasty.
PubMed, Cochrane, and Google Scholar (page 1-20) were searched till December 2023. Only comparative studies were included. The clinical outcomes evaluated were the heterotopic ossification formation in hip replacements, radiolucent lines formation, and functional knee scores in knee replacements.
Four studies met the inclusion criteria and were included in this meta-analysis. Pulsed lavage was shown to reduce the formation of radiolucent lines (P = 0.001). However, no difference was seen in the remaining outcomes
Pulsed lavage reduced the formation of radiolucent lines in knee replacements. No difference was seen in the remaining outcomes. Furthermore, the clinical significance of these radiolucent lines is poorly understood. Better conducted randomized controlled studies and cost-effectivity studies are needed to reinforce these findings.
Core Tip: Pulsed lavage may be important in total knee arthroplasty but has no added benefit in total hip arthroplasty.
- Citation: Daher M, Haykal G, Aoun M, Moussallem M, Ghoul A, Tarchichi J, Sebaaly A. Pulsed lavage in joint arthroplasty: A systematic review and meta-analysis. World J Orthop 2024; 15(3): 293-301
- URL: https://www.wjgnet.com/2218-5836/full/v15/i3/293.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i3.293
With the advancements in medicine, people's average life expectancies are rising[1]. Between 2000 and 2050, there will be a 135% increase in the population above the age of 65[2]. The World Health Organization has identified four chronic musculoskeletal illnesses as conditions whose prevalence will increase as the population ages. Two of these conditions are osteoarthritis (OA) and rheumatoid arthritis (RA), which both affect millions of individuals worldwide[3]. When conservative treatment for RA and OA has failed and a person's overall quality of life is continuing to decline, total hip arthroplasty (THA) and total knee arthroplasty (TKA) is the surgical management of choice[4-10]. In fact, Joint arthroplasty is as an effective intervention to relieve pain and improve joint function[11-13]. Furthermore, gait is the most common activity to be affected in patients prior to undergoing joint replacement surgery[14-18]. Different prosthetic materials can be used in joint replacement which can also impact the gait and functional outcomes post-operatively, and can be assessed by computational simulation[19-23]. The By 2030, it is predicted that the United States would undertake over 3.5 million primary TKA procedures yearly and close to 600000 main THA procedures[1].
The lifespan of the implants depends on improvements in cement penetration and implant stability in hip and knee arthroplasty[24]. Pulsed lavage (PL) can be used to achieve this[24]. Radiolucent lines are a common observation at the cement-bone interface in TKA[25]. However, the clinical outcome does not appear to be impacted by the radiolucent lines, though[26]. The majority of radiolucent lines are 1 mm wide and have a radioopaque sclerotic border. Pathological radiolucent lines, on the other hand, are larger than 2 mm and have ill-defined edges[27]. Another problem in THA is the formation of heterotopic ossification (HO). PL may stop HO development by removing the nascent mesenchymal cells from the hip joint and gluteal muscles[28].
Despite numerous publications about the efficacy of PL in the field of surgery, there is no meta-analysis about its effectiveness in Joint Arthroplasty (JA). Therefore, this meta-analysis is designed to compare PL to standard lavage (SL) in JA.
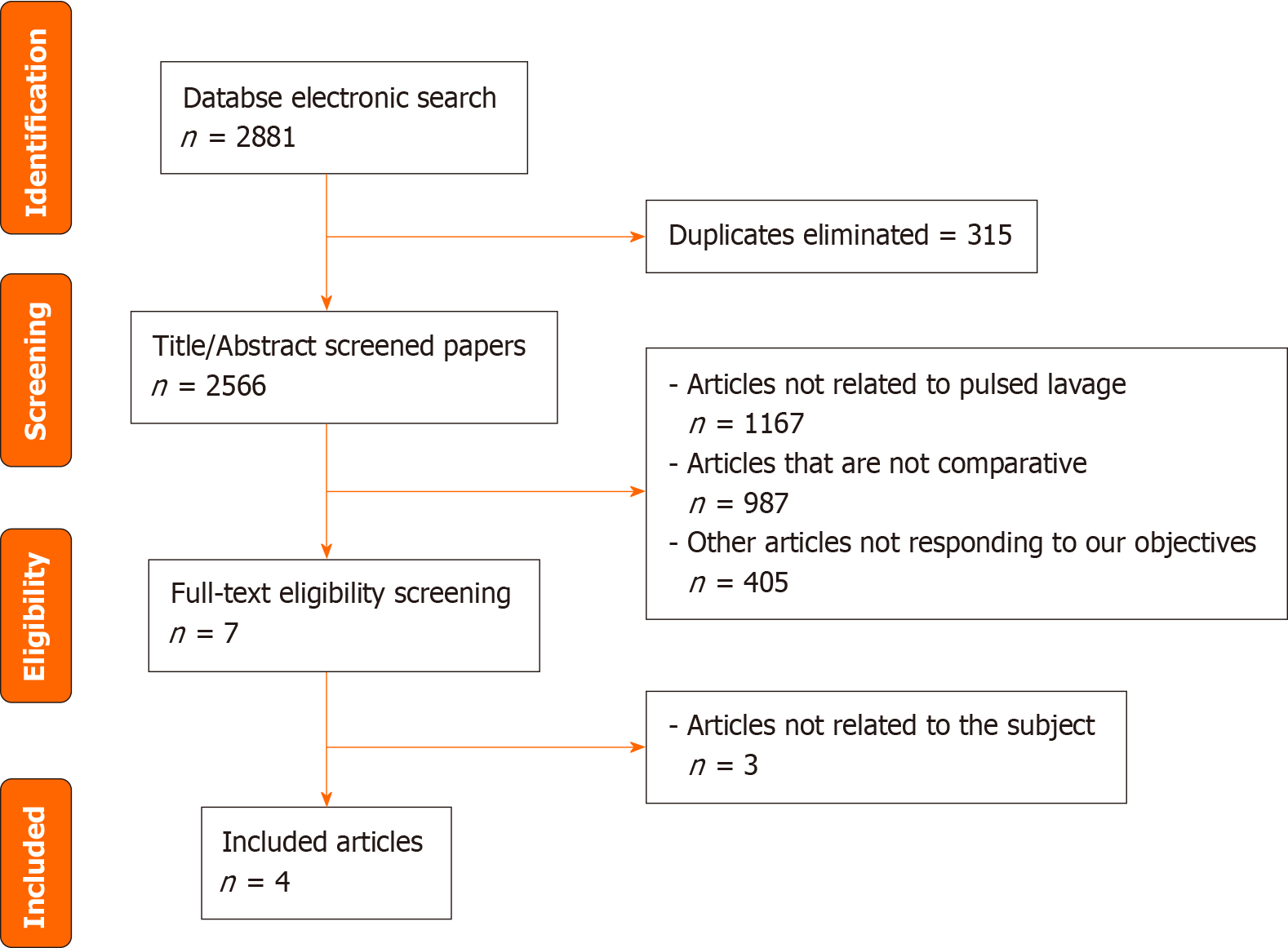
This study followed the PRISMA guidelines. PubMed, Cochrane, and Google Scholar (page 1-20) were searched updated to December 2023 for the qualified studies in order to study the efficacy of PL in JA using the following keywords and Boolean operators “puls*” AND “knee” OR “hip”. Literature was also identified by tracking reference lists from papers and Internet searches. One investigator (MD) extracted the data, and another investigator (AS) confirmed the choice of the articles. The process is summarized in the PRISMA flowchart (Figure 1).
Inclusion criteria were: (1) Comparative studies: randomized controlled trails, retrospective comparative studies, prospective clinical trials; (2) patients operated with a total or partial knee or hip replacement; and (3) Pulsed lavage was used in the first group compared to standard lavage in another group. The studies with the following characteristics were excluded from this study: (1) Case reports, narrative or systematic reviews, theoretical research, conference report, meta-analysis, expert comment, and economic analysis; and (2) non-relevant outcomes.
Two reviewers determined the eligibility of the studies independently. Extraction of the analyzed data was made from the included studies and it consisted of two parts. The first part consisted of the basic information containing the name of the authors, the title, the publication year, the journal, the volume, the issue, the pages, the study design, the sample size along with the size of each group of management, and the different types of bias suspected in each study. The second part consisted of the clinical outcomes the formation of HO, radiolucent lines formation, and functional knee scores. Any arising difference between the investigators was resolved by discussion.
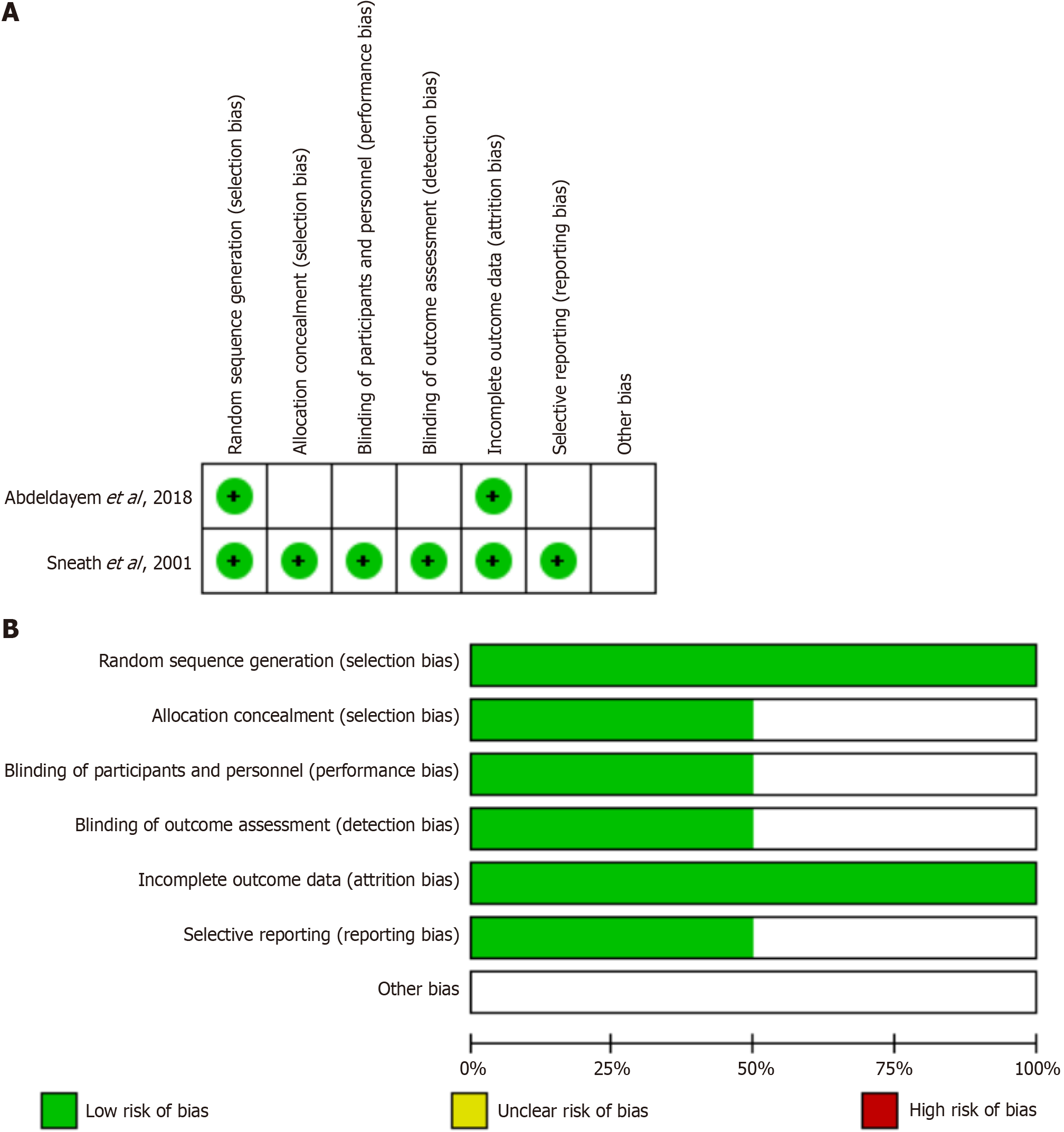
The Cochrane risk-of-bias tool was used by two writers (MD and AS) to independently assess the risk of bias. The following factors were taken into consideration when determining whether a trial had a high, low, or unclear risk of bias: Random sequence generation, allocation concealment, blinding of participants and study workers to the research procedure, blinding of outcome assessment, inadequate outcome data, and selective reporting (Figure 2A and B). Trials that had a high risk of bias for more than one key domain were deemed to have a high risk of bias, while those that had a low risk of bias for every key domain were deemed to have a low risk of bias. If neither of these conditions were met, the trials were deemed to have an unclear risk of bias. For non-randomized studies, the ROBINS-I tool for assessing risk of bias in non-randomized studies of interventions was used[29]. Studies that had a critical risk of bias were excluded.
The statistical analysis was performed using Review Manager 5.4 (The Cochrane Collaboration, 2020). For continuous data, 95% confidence intervals (CI) and standardized mean differences were utilized, while risk ratio with 95%CI was used for dichotomous data. Q tests and I2 statistics were used to evaluate heterogeneity indicating considerable heterogeneity if P ≤ 0.10 or I2 > 50%. High levels of variability were handled by the use of the random-effects model. On the other hand, the fixed-effect model was chosen if P > 0.10 or I2 < 50%. Statistical significance threshold was chosen at P = 0.05.
Four studies[24,28,30,31] met the inclusion criteria and were included in the meta-analysis with 2 randomized controlled trials and 1 prospective non-randomized study, and 1 retrospective comparative study. It involved 185 subjects in the PL group and 182 subjects in the SL group. The main characteristics of the included studies are summarized in Table 1.
| Ref. | Methods | Participants | Mean age (SD) | Measured outcomes | Follow-up time | ||
| PL | SL | PL | SL | ||||
| Abdeldayem et al[24], 2018 | Prospective randomized comparison | 44 | 42 | 64, NA | 64, NA | Knee society score, knee function score, radiolucent lines | 12 months |
| Clarius et al[30], 2009 | Prospective non-randomized comparison | 54 | 46 | 63, NA | 68, NA | Knee society score, knee function score, Oxford knee score, radiolucent lines | 22 months |
| Mellema et al[28], 2011 | Retrospective comparison | 39 | 48 | 62; 9 | 55; 10 | Rate of heterotopic ossification | 14 months |
| Sneath et al[31], 2001 | Prospective randomized comparison | 48 | 46 | 71, NA | 73, NA | Rate of heterotopic ossification | 12 months |
The risk of bias assessment is presented in Figure 2A and B and Table 2. There were no high bias risks, they were either low, moderate, or unclear.
| Studies | Confounding bias | Selection bias | Classification bias | Bias due to deviation from interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of reported results | Results |
| Clarius et al[30], 2009 | Low risk | Low risk | Low risk | Low risk | Low risk | Moderate risk | Low risk | Moderate risk |
| Mellema et al[28], 2011 | Low risk | Low risk | Low risk | Low risk | Low risk | low risk | Low risk | Low risk |
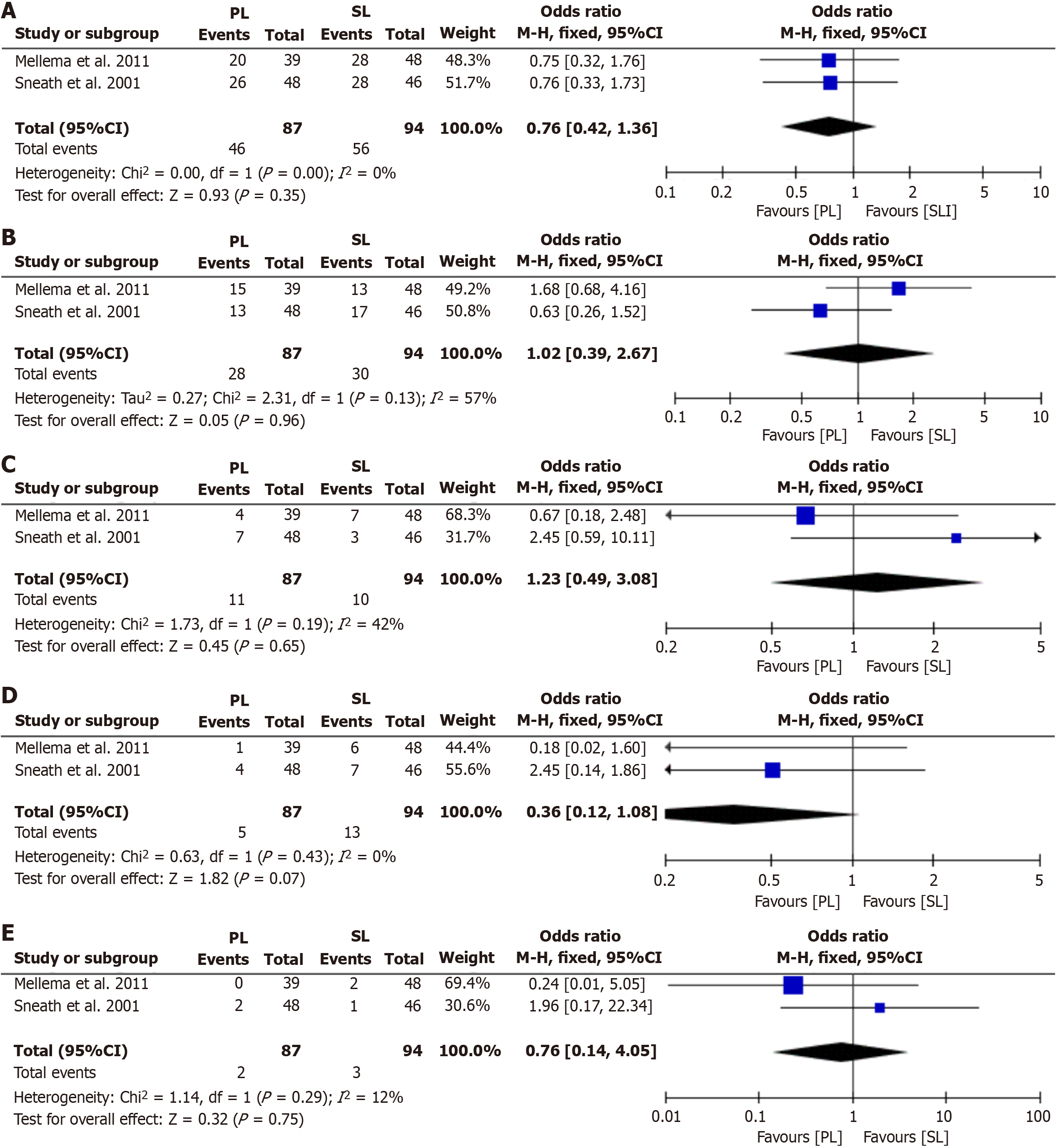
Two studies on 181 subjects (87 PL vs 94 SL) reported data on post-operative HO formation. The results showed no differences between PL and SL in overall HO formation (Odds ratio = 0.76; 95%CI = 0.42–1.36, P = 0.35, Figure 3A), Brooker grade 1 HO formation (Odds ratio = 1.02; 95%CI = 0.39–2.67, P = 0.96, Figure 3B), Brooker grade 2 HO formation (Odds ratio = 1.23; 95%CI = 0.49–3.08, P = 0.65, Figure 3C), Brooker grade 3 HO formation (Odds ratio = 0.36; 95%CI = 0.12–1.08, P = 0.07, Figure 3D), and Brooker grade 4 HO formation (Odds ratio = 0.76; 95%CI = 0.14–4.05, P = 0.75, Figure 3E).
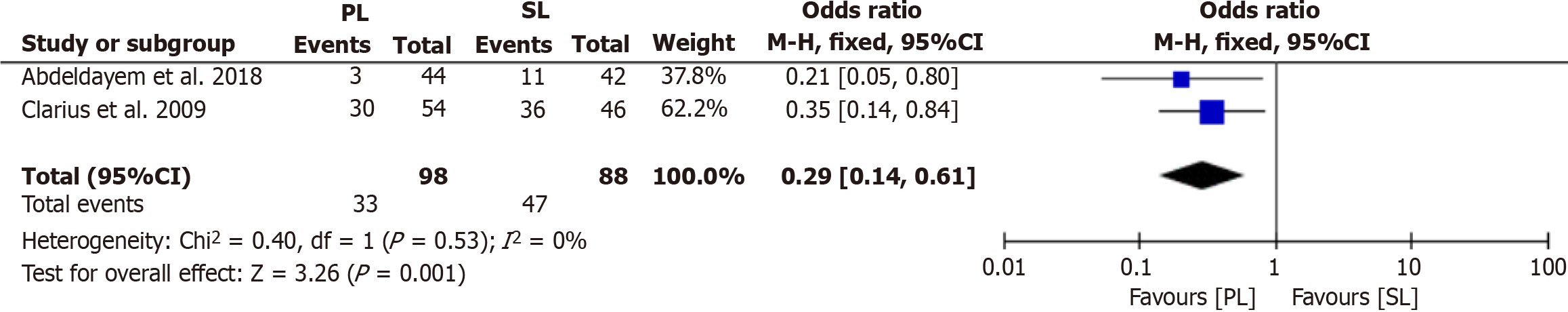
Two studies on 186 (98 PL vs 88 SL) subjects reported data on radiolucent lines formation. The results showed that when compared to SL, PL significantly reduces the formation of radiolucent lines (Odds ratio = 0.29; 95%CI = 0.14–0.61, P = 0.001, Figure 4).
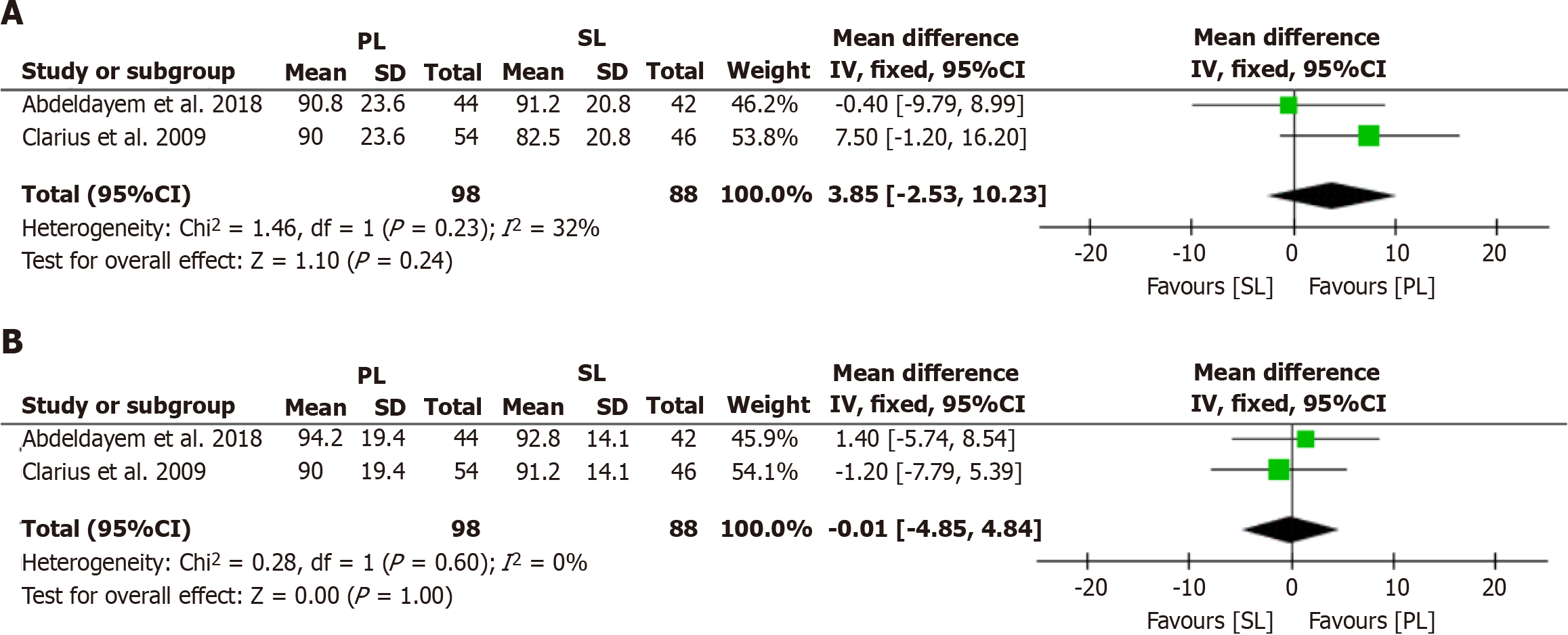
Two studies on 186 subjects (98 PL vs 88 SL) reported data on knee functional scores. The results showed no difference between PL and SL in knee society score (Mean difference= -0.01; 95%CI = -4.85–4.84, P = 1.0, Figure 5A) and knee function score (Mean difference = 3.85; 95%CI -2.53–10.23, P = 0.24, Figure 5B).
Total joint arthroplasties are expected to increase over time due to the aging population and obesity. A commonly faced adverse events in such procedures is the formation of HO in hip replacements and radiolucent lines formation in knee replacements. The efficacy of PL and preventing such problems has been studied in JA. However, this is the first meta-analysis assessing the efficacy of PL in both knee and hip replacements. The outcomes of this meta-analysis can be divided into three section: HO formation, radiolucent lines, and knee functional scores. Pulsed Lavage reduced the formation of radiolucent lines. However, no differences were seen in the remaining outcomes.
Our results showed no difference in HO formation between PL and SL. A study by Mellema et al[28] showed a beneficial effect of PL in preventing Brooker grade 3-4 HO however this may be limited by the low numbers in such high HO grades. The etiology of this pathology is still unclear. It is said that it might be from the mesenchymal pluripotential stem cells that are released by the bone during the surgery acting as a stimulus[32,33]. If that was the case, then PL should have a beneficial effect on HO formation. The lack of correlation between HO formation and PL suggests another mechanism. Pellegrini et al[34] showed that a pre-operative radiotherapy directed at the soft tissue around the hip reduced the rate of HO formation which may draw the conclusion that the osteogenic precursors responsible of HO are derived from the soft tissue and not the bone debris.
No difference in knee functional scores were seen between SL and PL, however the latter reduced the formation of radiolucent lines in knee replacement. After cemented TKA, there are two types of tibial radiolucency that can be found. In the first year post-operatively, physiological radiolucency is a frequent but common observation[24]. It does not progress or compromise the stability of the implant. Physiologic radiolucency has a sclerotic border and a thickness of no more than 1 mm on radiographs. On the other hand, pathological radiolucency typically has edges that are not sclerotic and is thicker than 2mm. These radiolucent lines are signs of septic or aseptic loosening and influence implant stability because they progress over time[24]. Abdeldayem et al[24] and Clarius et al[30] showed that the cement penetration was deeper in the PL group which could explain the lower rate of radiolucency observed when PL was used. This can be explained by the cancellous bone becoming more porous following jet lavage and then becoming much more thoroughly penetrated by bone cement[24]. However, the clinical significance of these radiolucent lines is still poorly understood[26]. In fact, radiolucency is present in all loose knee implants, but not all implants that have radiolucency are loose[26]. And seeing that there are no differences in the functional scores, one might wonder about the benefit of using PL in knee replacement.
This study has several strengths: It is the first meta-analysis comparing PL to SL in JA. Moreover, only comparative studies were included reducing the risk of operative and matching bias. Finally, the selection process was more selective. This makes the study less heterogenous and decreases the risk of bias. However, this study had also limitations: There weren’t that many comparative studies in the literature to include; Inclusion and exclusion criteria for patients were different; the number of included studies is limited and the data used for analysis was pooled and individual patients’ data were unavailable, and this could limit more comprehensive analyses.
This is the first meta-analysis comparing pulsed lavage to standard lavage in partial or total knee and hip arthroplasty. It showed that pulsed lavage reduced the formation of radiolucent lines in knee replacement. No difference was seen in the remaining outcomes when compared to standard lavage. The decrease in radiolucent lines formation may be associated to a better cement penetration however, the clinical significance of these lines is still questionable. Nevertheless, more randomized controlled studies and cost-effectivity studies are needed to confirm the benefits of this lavage technique.
Many studies compared pulse lavage to standard lavage in the setting of joint replacement but no meta-analysis is present to assess the overall utility of pulse lavage.
This study will be the first to assess the utility of pulse lavage in the setting of total hip and total knee replacements.
In the setting of hip replacement, we assessed the formation of heterotopic ossification whereas in knee replacement, we assessed the formation of radiolucent lines and functional outcomes.
PubMed, Cochrane, and Google Scholar (page 1-20) were searched till December 2023 including only comparative studies comparing pulsed lavage to standard lavage in total knee or total hip replacements.
We found no difference in heterotopic ossification in hip replacement and no difference in functional outcomes in knee replacement. However, we found a reduction in the formation of radiolucent lines in total knee replacement.
We conclude that pulsed lavage may be beneficial in the setting of total knee replacement but has no added benefit in total hip replacement.
Future research should assess the costs/benefits of pulsed lavage in the setting of total joint replacement.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Lebanon
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ammarullah MI, Indonesia S-Editor: Liu JH L-Editor: A P-Editor: Zhao YQ
| 1. | Masaracchio M, Hanney WJ, Liu X, Kolber M, Kirker K. Timing of rehabilitation on length of stay and cost in patients with hip or knee joint arthroplasty: A systematic review with meta-analysis. PLoS One. 2017;12:e0178295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 96] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Wiener JM, Tilly J. Population ageing in the United States of America: implications for public programmes. Int J Epidemiol. 2002;31:776-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 144] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81:646-656. [PubMed] |
| 4. | Bruyère O, Ethgen O, Neuprez A, Zégels B, Gillet P, Huskin JP, Reginster JY. Health-related quality of life after total knee or hip replacement for osteoarthritis: a 7-year prospective study. Arch Orthop Trauma Surg. 2012;132:1583-1587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Dailiana ZH, Papakostidou I, Varitimidis S, Liaropoulos L, Zintzaras E, Karachalios T, Michelinakis E, Malizos KN. Patient-reported quality of life after primary major joint arthroplasty: a prospective comparison of hip and knee arthroplasty. BMC Musculoskelet Disord. 2015;16:366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 6. | Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, Phillips C, Partridge AJ, Bélisle P, Fossel AH, Mahomed N, Sledge CB, Katz JN. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42:1722-1728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001;161:454-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 299] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 8. | Pearl A, Ismail A, Alsadi T, Crespi Z, Daher M, Saleh K. Frailty and Pre-Frailty in the Setting of Total Joint Arthroplasty: A Narrative Review. Geriatr Orthop Surg Rehabil. 2023;14:21514593231188864. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 9. | Aouad D, Daher M, Darwish M, Saidy E, Rassi L El, Rassi G El. Use of tranexamic acid in simultaneous bilateral total knee arthroplasty: a comparative study. Egypt Orthop J. 2023;57:309-313. [DOI] [Full Text] |
| 10. | Ayoubi R, Aouad D, Darwish M, Maalouly J, Hajj G, Daher M, Nehme A. Effect of the Innominate Bone Horizontal Rotation on Acetabular Version: A Retrospective Radiological Study on a Middle Eastern Population. Int J Clin Res. 2023;3:276-284. [DOI] [Full Text] |
| 11. | Hidayat T, Ismail R, Tauviqirrahman M, Saputra E, Ammarullah MI, Danny Pratama Lamura M, Bayuseno AP, Jamari J. Investigation of mesh model for a finite element simulation of the dual-mobility prosthetic hip joint. J Tribol. 2023;38:118-140. [DOI] [Full Text] |
| 12. | Ammarullah MI, Hidayat T, Lamura MDP, Jamari J. Relationship between deformation and running-in wear on hardon-hard bearings from metal, ceramic, and diamond materials for total hip prosthesis. J Tribol. 2023;38:69-81. |
| 13. | Ammarullah MI, Santoso G, Sugiharto S, Supriyono T, Kurdi O, Tauviqirrahman M, Winarni TI, Jamari J. Tresca stress study of CoCrMo-on-CoCrMo bearings based on body mass index using 2D computational model. J Tribol. 2022;33:31-38. [DOI] [Full Text] |
| 14. | Jamari J, Ammarullah MI, Santoso G, Sugiharto S, Supriyono T, Permana MS, Winarni TI, van der Heide E. Adopted walking condition for computational simulation approach on bearing of hip joint prosthesis: review over the past 30 years. Heliyon. 2022;8:e12050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 44] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 15. | Ammarullah MI, Hartono R, Supriyono T, Santoso G, Sugiharto S, Permana MS. Polycrystalline Diamond as a Potential Material for the Hard-on-Hard Bearing of Total Hip Prosthesis: Von Mises Stress Analysis. Biomedicines. 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 61] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 16. | Ammarullah MI, Afif IY, Maula MI, Winarni TI, Tauviqirrahman M, Akbar I, Basri H, van der Heide E, Jamari J. Tresca Stress Simulation of Metal-on-Metal Total Hip Arthroplasty during Normal Walking Activity. Materials (Basel). 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 92] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 17. | Ammarullah M, Santoso G, Sugiharto S, Supriyono T, Wibowo D, Kurdi O, Tauviqirrahman M, Jamari J. Minimizing Risk of Failure from Ceramic-on-Ceramic Total Hip Prosthesis by Selecting Ceramic Materials Based on Tresca Stress. Sustainability. 2022;14:13413. [DOI] [Full Text] |
| 18. | Salaha ZFM, Ammarullah MI, Abdullah NNAA, Aziz AUA, Gan HS, Abdullah AH, Abdul Kadir MR, Ramlee MH. Biomechanical Effects of the Porous Structure of Gyroid and Voronoi Hip Implants: A Finite Element Analysis Using an Experimentally Validated Model. Materials (Basel). 2023;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 41] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 19. | Tauviqirrahman M, Ammarullah MI, Jamari J, Saputra E, Winarni TI, Kurniawan FD, Shiddiq SA, van der Heide E. Analysis of contact pressure in a 3D model of dual-mobility hip joint prosthesis under a gait cycle. Sci Rep. 2023;13:3564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 23] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 20. | Jamari J, Ammarullah MI, Santoso G, Sugiharto S, Supriyono T, van der Heide E. In Silico Contact Pressure of Metal-on-Metal Total Hip Implant with Different Materials Subjected to Gait Loading. Metals (Basel). 2022;12:1241. [RCA] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 16.0] [Reference Citation Analysis (1)] |
| 21. | Jamari J, Ammarullah MI, Santoso G, Sugiharto S, Supriyono T, Prakoso AT, Basri H, van der Heide E. Computational Contact Pressure Prediction of CoCrMo, SS 316L and Ti6Al4V Femoral Head against UHMWPE Acetabular Cup under Gait Cycle. J Funct Biomater. 2022;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 71] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 22. | Jamari J, Ammarullah MI, Saad APM, Syahrom A, Uddin M, van der Heide E, Basri H. The Effect of Bottom Profile Dimples on the Femoral Head on Wear in Metal-on-Metal Total Hip Arthroplasty. J Funct Biomater. 2021;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 86] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 23. | Ammarullah MI, Afif IY, Maula MI, Winarni TI, Tauviqirrahman M, Jamari J. Tresca stress evaluation of Metal-on-UHMWPE total hip arthroplasty during peak loading from normal walking activity. Mater Today Proc. 2022;63:S143-S146. [DOI] [Full Text] |
| 24. | Abdeldayem SM, Zakaria ZM, Metwaly RG, Eid MA. Jet lavage in primary total knee arthroplasty: A comparative study. Curr Orthop Pract. 2018;29:157-159. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Duus BR, Boeckstyns M, Kjaer L, Stadeager C. Radionuclide scanning after total knee replacement: correlation with pain and radiolucent lines. A prospective study. Invest Radiol. 1987;22:891-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Rea P, Short A, Pandit H, Price AJ, Kyberd P, Beard DJ, Gill HS, Murray DW. Radiolucency and migration after Oxford unicompartmental knee arthroplasty. Orthopedics. 2007;30:24-27. [PubMed] |
| 27. | Tibrewal SB, Grant KA, Goodfellow JW. The radiolucent line beneath the tibial components of the Oxford meniscal knee. J Bone Joint Surg Br. 1984;66:523-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 115] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Mellema J, Zijlstra W, Raaij T van, Have B ten, Raay J van. Pulsed Lavage in Cementless Total Hip Arthroplasty Reduces the Incidence ofBrooker Grade 3 and 4 Heterotopic Ossifications. Open J Orthop. 2011;1:9-13. [DOI] [Full Text] |
| 29. | Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7683] [Cited by in RCA: 10700] [Article Influence: 1188.9] [Reference Citation Analysis (2)] |
| 30. | Clarius M, Hauck C, Seeger JB, James A, Murray DW, Aldinger PR. Pulsed lavage reduces the incidence of radiolucent lines under the tibial tray of Oxford unicompartmental knee arthroplasty: pulsed lavage versus syringe lavage. Int Orthop. 2009;33:1585-1590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 31. | Sneath RJ, Bindi FD, Davies J, Parnell EJ. The effect of pulsed irrigation on the incidence of heterotopic ossification after total hip arthroplasty. J Arthroplasty. 2001;16:547-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Thomas BJ. Heterotopic bone formation after total hip arthroplasty. Orthop Clin North Am. 1992;23:347-358. [PubMed] |
| 34. | Pellegrini VD Jr, Gregoritch SJ. Preoperative irradiation for prevention of heterotopic ossification following total hip arthroplasty. J Bone Joint Surg Am. 1996;78:870-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 78] [Article Influence: 2.7] [Reference Citation Analysis (0)] |