Published online Mar 18, 2024. doi: 10.5312/wjo.v15.i3.238
Peer-review started: October 22, 2023
First decision: December 28, 2023
Revised: January 7, 2024
Accepted: February 29, 2024
Article in press: February 29, 2024
Published online: March 18, 2024
Processing time: 145 Days and 1.2 Hours
Hallux valgus (HV) is a common foot deformity that manifests with increasing age, especially in women. The associated foot pain causes impaired gait and decreases quality of life. Moderate and severe HV is a deformity that is characterized by the involvement of lesser rays and requires complex surgical treatment. In this study, we attempted to develop a procedure for this condition.
To analyse the treatment results of patients who underwent simultaneous surgical correction of all parts of a static forefoot deformity.
We conducted a prospective clinical trial between 2016 and 2021 in which 30 feet with moderate or severe HV associated with Tailor’s bunion and metatarsalgia were surgically treated via a new method involving surgical correction of all associated problems. This method included a modified Lapidus procedure, M2M3 tarsometatarsal arthrodesis, intermetatarsal fusion of the M4 and M5 bases, and the use of an original external fixation apparatus to enhance correction power. Preoperative, postoperative, and final follow-up radiographic data and American Orthopaedic Foot and Ankle Society (AOFAS) scores were compared, and P values < 0.05 were considered to indicate statistical significance.
The study included 28 females (93.3%) and 2 males feet (6.7%), 20 (66.7%) of whom had a moderate degree of HV and 10 (33.3%) of whom had severe deformity. M2 and M3 metatarsalgia was observed in 21 feet, and 9 feet experienced pain only at M2. The mean follow-up duration was 11 months. All patients had good correction of the HV angle [preoperative median, 36.5 degrees, interquartile range (IQR): 30-45; postoperative median, 10 degrees, IQR: 8.8-10; follow-up median, 11.5 degrees, IQR: 10-14; P < 0.01]. At follow-up, metatarsalgia was resolved in most patients (30 vs 5). There was a clinically negligible decrease in the corrected angles at the final follow-up, and the overall AOFAS score was significantly better (median, 65 points, IQR: 53.8-70; vs 80 points, IQR: 75-85; P < 0.01).
The developed method showed good sustainability of correction power in a small sample of patients at the one-year follow-up. Randomized clinical trials with larger samples, as well as long-term outcome assessments, are needed in the future.
Core Tip: Although there are several methods of surgical correction for moderate and severe hallux valgus, not all patients achieve the desired treatment result. One of the reasons for this outcome is the involvement of almost all rays of the foot. To achieve a favourable treatment result in these patients, simultaneous correction of all the elements of the deformed forefoot is needed, considering the biomechanical association of this pathology, namely, high mobility of the first and fifth metatarsals.
- Citation: Zhanaspayev A, Bokembayev N, Zhanaspayev M, Tlemissov A, Aubakirova S, Prokazyuk A. Correction method for moderate and severe degrees of hallux valgus associated with transfer metatarsalgia. World J Orthop 2024; 15(3): 238-246
- URL: https://www.wjgnet.com/2218-5836/full/v15/i3/238.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i3.238
Hallux valgus (HV) deformity is present in 23%-35.7% of the adult population. The incidence of HV increases exponentially with age, and HV occurs most often in women. An analysis of age subgroups showed that the disease incidence was 7.8% among individuals under 18 years of age, 23% among adults aged 18-65 and 35.7% among those aged > 65 years[1].
An increase in the degree of HV is directly associated with the development of additional problems in the forefoot, such as metatarsalgia, Tailor’s bunion, and hammer toe deformity. Therefore, orthopaedists should not consider severe HV as a pathology involving only the first ray but rather as a complex problem of the entire forefoot. Metatarsalgia combined with HV deformity is a result of increased pressure and load transfer to the lateral metatarsal region. Load and pressure transfer from the big toe to the central metatarsal region has been described, indicating functional impairment of the big toe and simultaneous worsening of loading conditions at the metatarsals[2]. An increase in HV severity is significantly associated with increased metatarsalgia and decreased foot function[3]. Fifth ray deformities involving a valgus fifth metatarsal and a varus fifth toe are often associated with HV. These deformities are ascribable to the characteristics of the Lisfranc joint, allowing greater mobility of the first and fifth metatarsals in comparison to the central metatarsals[4].
Currently, there are hundreds of surgical techniques for treating HV, but arguably, no technique is significantly better than the others[5]. Arthrodesis of the first tarsal-metatarsal joint is one of these techniques. Previously, the Lapidus procedure was indicated for severe HV deformities and HV recurrence because of its ability to stabilize and correct the deformity at the first tarsometatarsal (TMT) joint[6-9]. Currently, the improved technique with multiplane correction has no restrictions in treating HV deformities, regardless of HV angle (HVA) or the magnitude of the intermetatarsal angle (IMA), and is the method of choice for all cases[10]. However, some studies have confirmed that central metatarsalgia may persist, intensify, or develop even after the most sophisticated surgery for HV[11].
Dissatisfaction with the outcomes of surgical intervention for moderate and severe HV that focuses solely on the first ray without addressing concurrent forefoot pathologies served as the impetus for the development of a comprehensive treatment approach targeting all aspects of this medical issue at the Lisfranc joint level. A distinctive aspect of the developed technique is the intraoperative utilization of an external device to augment the correction of the deformity and minimize the incidence of splayfoot.
This prospective case-series study was conducted at a regional traumatology and orthopaedics centre in Kazakhstan that serves a population of 610000 people. The inclusion criteria for patients were as follows: Symptomatic moderate or severe HV according to the traditional radiographic classification[12] (HVA ≥ 20 degrees or intermetatarsal angle (IMA) ≥ 11 degrees); pain under the heads of the second or second-third metatarsals (M2, M3); hammer toe deformity; Tailor’s bunion; and no previous surgical intervention.
The criteria for determining hypermobility of the first TMT joint as an indication for the Lapidus procedure are still controversial[13]. We chose the Romash classification[14] (types I and II) because, in our opinion, it is more independent and accurate than the other methods due to the use of X-rays in the assessment.
Patients with rheumatoid arthritis, gout, or osteoarthritis of the first metatarsophalangeal joint were excluded. Some of the included patients had HV deformities on both feet and underwent surgery at different times; thus, in this paper, we refer to the number of operated feet.
Information on metatarsalgia, plantar callosities, radiographic analysis, and complications was obtained before surgery, after surgery, and at the final follow-up. Clinical evaluation was performed using the American Orthopaedic Foot and Ankle Society (AOFAS) scale[15].
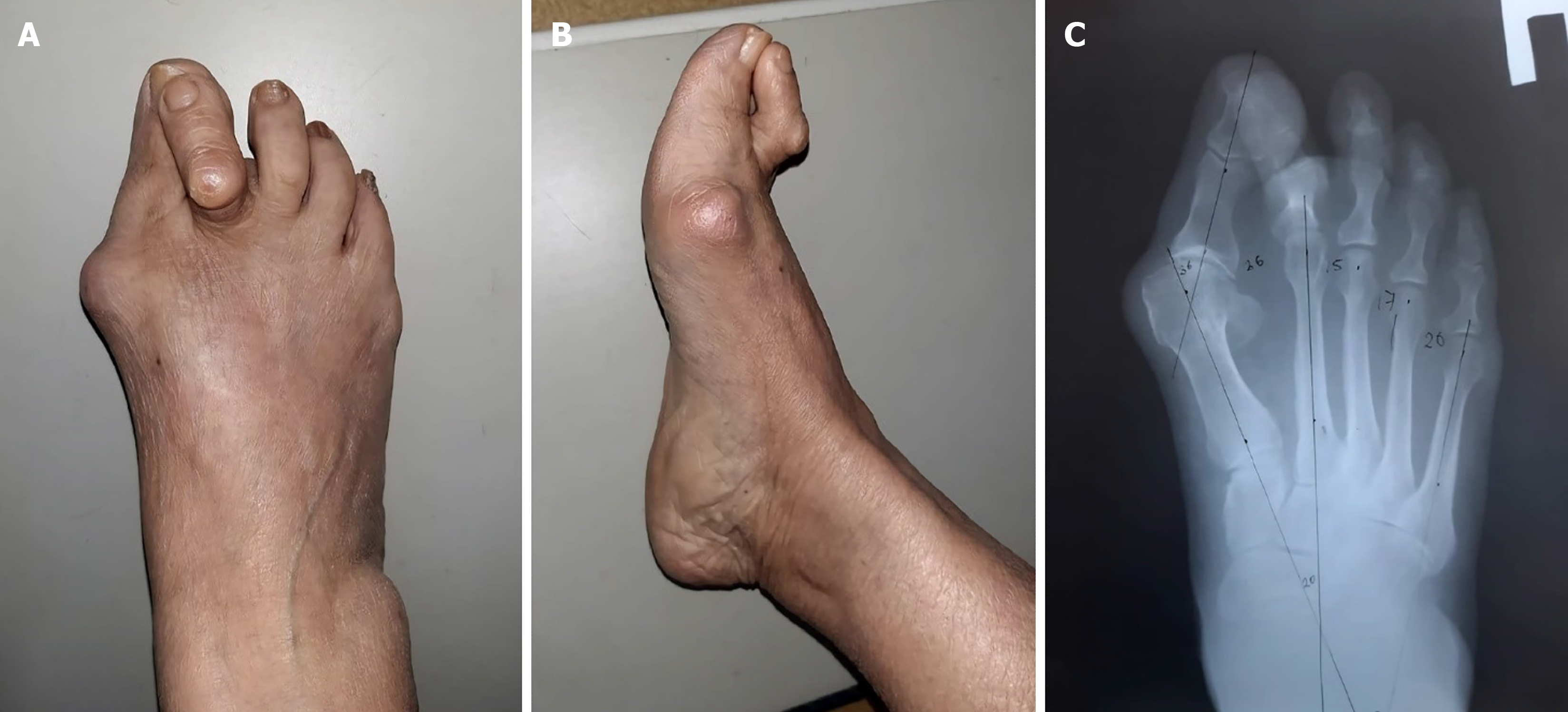
A representative case of the performance of the optimized surgical technique on a patient with moderate HV, painless Tailor’s bunion, M2-M3 metatarsalgia, and hammer deformity of the second toe is shown in Figure 1. Under spinal anaesthesia, resection of the M1 head exostosis was performed using an oscillating saw. The m. adductor hallucis tendon was mobilized with sesamoid hammock realignment. Then, as in the modified Lapidus arthrodesis procedure, we resected the articular surface of the M1 base and performed wedge-shaped osteotomy of the medial cuneiform bone. For all patients, we removed the cortex of the M4 and M5 bases in the intermetatarsal space, leaving the bone chips in situ, as was proposed for the M1-M2 bases in the original Lapidus procedure[16]. Next, wedge-shaped resection of the articular surfaces of the M2 and M3 bases and the medial and lateral cuneiform was performed depending on the presence of metatarsalgia for the dorsal displacement of heads.
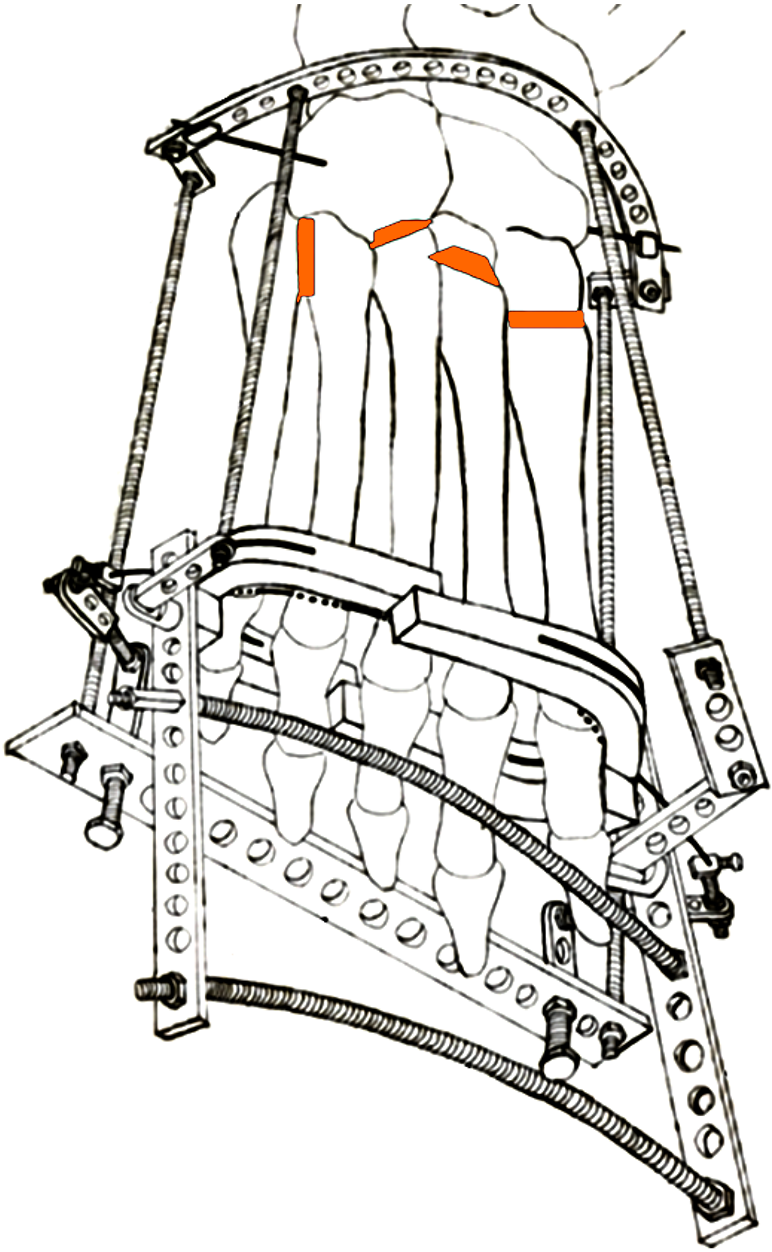
The next step of the procedure was the elimination of the metatarsus prima varus and metatarsus quintus valgus by installation of an external fixation device (developed in-house), and the K-wire was passed through the heads and necks of the metatarsal bones (Figure 2). Pronation of the first ray was manually corrected before passing through the K-wire, as proposed by DiDomenico et al[17]. At this time, the first metatarsal head was shifted laterally and on the plantar side. Angles M1M2 and M1M5 were corrected simultaneously. Finally, fixation in the corrected position was performed using four screws and a plate with angular stability placed on the medial surface, and one screw was used to fix M4-M5. Screws were placed through the metatarsals and cuneiform bones.
After disassembling the external fixation device, Akin osteotomy of the proximal phalanx of the first toe was performed, and a final X-ray was obtained (Figure 3). Intradermal sutures were used to close the wounds, and elastic tape and stockings were applied to improve lymphatic drainage and prevent venous thrombosis. In the early postoperative period, the patient was advised to ambulate with Barouk shoes. Passive motions in the toes and ankle joint were initiated on the second day after the operation. The patient had to wear elastic tape and Barouk shoes for 6-7 wk after surgery. Partial weight bearing was recommended as tolerated. The usual time to restore full weight-bearing was 10-12 wk.
All the statistical tests were performed and reviewed by a biomedical statistician using SPSS software (version 27.0; IBM Corp, Armonk, New York, United States). Owing to the small sample size, X-ray data before and after surgery and during the final follow-up were tested using the paired Wilcoxon criterion and independent samples t test at the 95% significance level. For all the data, P < 0.05 was considered to indicate statistical significance. Descriptive statistics for categorical variables are expressed as numbers (n) and percentages (%). Numerical variables are expressed as medians, standard deviations, minimum-maximum values, and interquartile ranges.
Thirty feet that underwent reconstruction for HV deformity between 2016 and 2021 were consecutively enrolled. HVA was prioritized over IMA for the inclusion of patients. According to the HVA, 20 (66.7%) feet had moderate HV (HVA 20-40 degrees), and 10 (33.3%) had a severe deformity (HVA ≥ 40 degrees). All feet, except for two, had an IMA > 10 degrees. In the two exceptions, the IMA was 10 degrees, but the HVAs were 25 and 28 degrees. All feet had an increased M4-M5 IMA and Tailor’s bunion; all but four (13.3%) of the cases were painless. M2 and M3 metatarsalgia was observed in 21 feet, and 9 feet experienced pain only under M2. The mean age of the patients was 52.8 years (range, 19-72). The left foot was operated on in 14 patients (46.7%), and the right foot was operated on in 16 patients (53.3%). There were 21 (70%) feet classified as Romash Type I and 9 feet classified as Type II (30%).
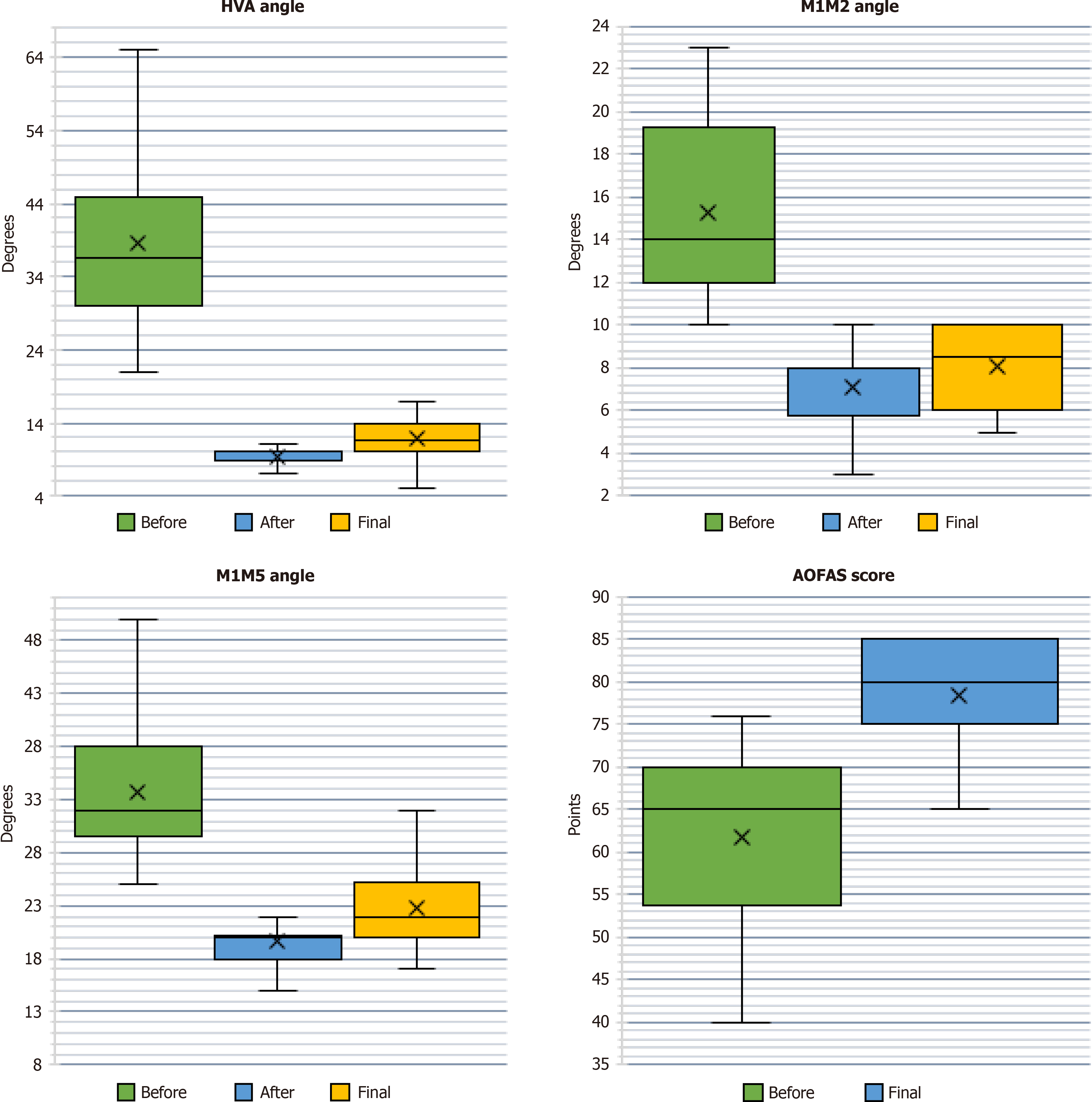
All feet underwent surgery and had a rehabilitation period, as described previously. The mean follow-up period was 11 months (range, 9-12 months). The results of the application of the developed treatment method are presented in the boxplots in Figure 4. After surgery, the HVA was restored to normal values in all patients. In addition, the loss of correction at follow-up (Z = -4.32; P < 0.001) did not lead to clinically significant deformation or a transition from one degree of severity to another. The proposed surgical method significantly improved the postoperative parameters of M1M2 (decreased at follow-up Z = -3.95; P < 0.001). Notably, there was a significant decrease in the M1M5 angle (decreased at follow-up Z = -4.21; P < 0.001); one of the goals of the operation was to correct splayfoot, which is an important type of deformation leading to foot dysfunction.
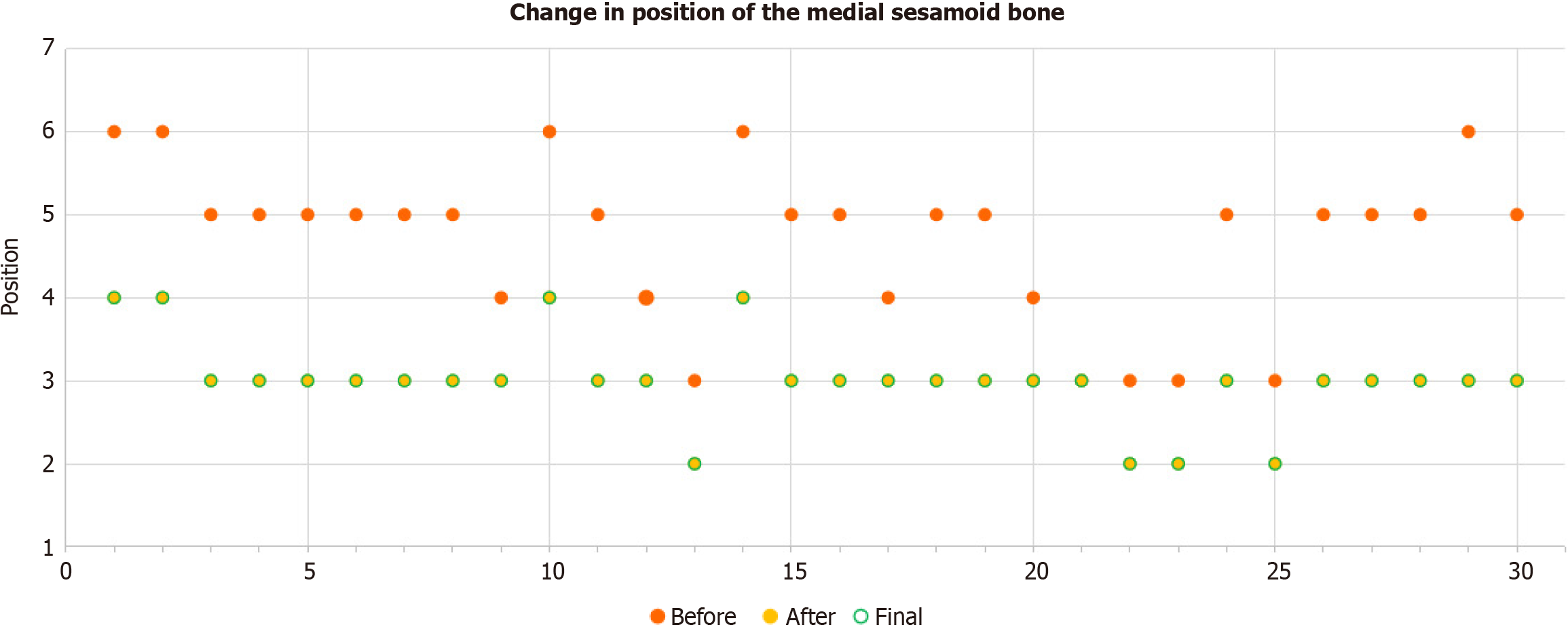
With respect to the measured angles, there was an improvement in the position of the medial sesamoid bone of the first metatarsophalangeal joint relative to the axis of the first metatarsal bone in all patients after the operation. Anteroposterior X-rays were graded using the Hardy and Clapham scale[18] (Figure 5). No changes were observed between the postoperative position and final follow-up.
Accordingly, correction of the radiological parameters of the foot improved its function, resulting in an increase in the AOFAS score. The average improvement in the long term was 15 points, partly due to the correction of metatarsalgia by targeting the small rays of the foot. For plantar callosities, the grading was as follows: (1) Grade 0: No callosity; (2) Grade 1: Painless callosity underneath one joint; (3) Grade 2: Painful callosity underneath one joint; and (4) Grade 3: Painful callosity underneath two or more joints[19]. In the preoperative period, Grade 2-3 callosity was observed in 86.7% of patients, and in the long-term postoperative period, only five patients (16.7%) had painful callosity under the head of one metatarsal bone (Table 1).
| Preoperative | Final follow-up | |
| Callosity grade | ||
| Grade 0 | 0 | 5 |
| Grade 1 | 4 | 20 |
| Grade 2 | 2 | 5 |
| Grade 3 | 24 | 0 |
| Metatarsalgia | 26 | 5 |
One patient with an M1 that was shortened by 6 mm and showed partial loss of reduction had recurrent metatarsalgia; however, HVA correction was better after surgery than before surgery (43 vs 22 degrees). No indications for further surgery were found. Another patient developed a stitch abscess that caused redness and oedema for 3 wk, and short-term oral antibiotics were prescribed after the symptoms resolved completely. Two patients developed ligature fistulas. Recurrence of mild HV was observed in 2 feet.
The effectiveness of the Lapidus procedure for the treatment of HV, especially during multiplane correction, has been repeatedly reported[10,20]. The correction power of metatarsal osteotomy increases when performed from distal to proximal. As shown in a meta-analysis[21], the mean angular correction of the IMA for all included feet subjected to the Lapidus technique was 9.82 degrees (confidence interval: 8.82–10.82). In our study, the median delta IMA correction was 6 degrees. In the treatment of transfer metatarsalgia, the same consideration is given to the osteotomy level of the lesser metatarsals. Proximal osteotomies are more powerful than distal osteotomies because smaller corrections at the metatarsal base result in larger corrections at the weight-bearing metatarsal head, secondary to the longer lever arm. In our series, performing the concomitant procedure on lesser rays resulted in resolution of metatarsalgia in all but five patients (83.3%), and notional improvement in the AOFAS score was achieved. Favourable HV correction with osteotomy of the lesser metatarsals has also been reported[22-25].
The absence of a negative effect of arthrodesis of the medial and middle columns of the Lisfranc joint has been reported in publications devoted to the treatment of dislocation of this joint[26]. Currently, minimally invasive surgery is the preferred surgical treatment. However, Lu et al[27] suggested in their meta-analysis that the use of minimally invasive surgery for the correction of HV deformity was the better choice for patients with symptomatic HV than traditional open methods, but the efficacy of minimally invasive surgery in moderate-to-severe HV (HVA ≤ 30°) was poor, and open surgery resulted in better outcomes in this cohort[28,29].
One of the disadvantages of our technique was the need to use an intraoperative corrective device, which slightly increased the overall duration of the procedure. Another disadvantage was the complexity of the surgical treatment, as the invasiveness of the procedure led to an increase in the inpatient length of stay for individual patients (mean ± SD: 5.8 ± 2.43 d; 12 d in two patients).
This study has several limitations. Our study presents the preliminary results on the use of a new method of treatment for a small number of patients and therefore has the limitations intrinsic to such research. We did not perform any biomechanical examinations, such as pedobarography, to prove a decrease in pressure below the lesser metatarsals.
The developed method of complex treatment for forefoot deformity includes a modified Lapidus procedure, M2-M3 TMT arthrodesis, intermetatarsal fusion of M4-M5 bases, and fixation with the original external apparatus, allowing for the resolution of problems caused by splayfoot.
Until now, the treatment of hallux valgus (HV) is considered by many clinicians as an isolated problem of the forefoot, while the deformation of the first toe brings with metatarsalgia, Tailor’s bunion, and hammer toe deformity. An important step is the comprehensive elimination of all the existing problems to achieve satisfactory clinical results.
In our study, all existing pathologies in the Lisfranc joint were eliminated simultaneously.
The main objective was to decrease the key angles [HV angle (HVA) and intermetatarsal angles (IMA)] and plantar callosities using a modified Lapidus procedure.
We did a Clinical Trials Study involving 30 patients in the setting of a regional traumatology and orthopaedics centre in Kazakhstan.
The modified Lapidus procedure with intraoperative utilization of the developed external device led to a decrease in HVA, IMA, and M1M5 with correction of splayfoot and pain reduction. There was also improvement in the position of the medial sesamoid bone in each operated foot.
The method used was promising and demonstrated the absence of significant drawbacks in a small sample size.
Further randomized controlled trials are required to assess effectiveness in large samples.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Kazakhstan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Primadhi RA, Indonesia S-Editor: Wang JJ L-Editor: A P-Editor: Zhao YQ
| 1. | Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010;3:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 410] [Cited by in RCA: 509] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 2. | Waldecker U. Metatarsalgia in hallux valgus deformity: a pedographic analysis. J Foot Ankle Surg. 2002;41:300-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 69] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Chang C, Wang QF, Guo JC, Li DD, Fan YB, Wen JM. The Biomechanical Relationship between Hallux Valgus Deformity and Metatarsal Pain. J Healthc Eng. 2020;2020:8929153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Martinelli B, Valentini R. Correction of valgus of fifth metatarsal and varus of the fifth toes by percutaneous distal osteotomy. Foot Ankle Surg. 2007;13:136-139. [DOI] [Full Text] |
| 5. | Wagner P, Ortiz C, Wagner E. Rotational Osteotomy for Hallux Valgus. A New Technique for Primary and Revision Cases. Tech Foot Ankle Surg. 2017;16:3-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Coetzee JC, Resig SG, Kuskowski M, Saleh KJ. The Lapidus procedure as salvage after failed surgical treatment of hallux valgus: a prospective cohort study. J Bone Joint Surg Am. 2003;85:60-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 84] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Ellington JK, Myerson MS, Coetzee JC, Stone RM. The use of the Lapidus procedure for recurrent hallux valgus. Foot Ankle Int. 2011;32:674-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Lapidus PW. A quarter of a century of experience with the operative correction of the metatarsus varus primus in hallux valgus. Bull Hosp Joint Dis. 1956;17:404-421. [PubMed] |
| 9. | Lapidus PW. The author's bunion operation from 1931 to 1959. Clin Orthop. 1960;16:119-135. [PubMed] |
| 10. | Smith WB, Santrock RD, Hatch DJ, Dayton P. Intraoperative Mulitplanar Alignment System to Guide Triplanar Correction of Hallux Valgus Deformity. Tech Foot Ankle Surg. 2017;16:175-182. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Bryant AR, Tinley P, Cole JH. Plantar pressure and radiographic changes to the forefoot after the Austin bunionectomy. J Am Podiatr Med Assoc. 2005;95:357-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Ray JJ, Friedmann AJ, Hanselman AE, Vaida J, Dayton PD, Hatch DJ, Smith B, Santrock RD. Hallux Valgus. Foot Ankle Orthop. 2019;4:2473011419838500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 13. | Wukich DK, Donley BG, Sferra JJ. Hypermobility of the first tarsometatarsal joint. Foot Ankle Clin. 2005;10:157-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Romash MM, Fugate D, Yanklowit B. Passive motion of the first metatarsal cuneiform joint: preoperative assessment. Foot Ankle. 1990;10:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3199] [Cited by in RCA: 3113] [Article Influence: 100.4] [Reference Citation Analysis (0)] |
| 16. | Symeonidis PD, Anderson JG. Original and Modified Lapidus Procedures: Proposals for a New Terminology. J Bone Joint Surg Am. 2021;103:e15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | DiDomenico LA, Fahim R, Rollandini J, Thomas ZM. Correction of frontal plane rotation of sesamoid apparatus during the Lapidus procedure: a novel approach. J Foot Ankle Surg. 2014;53:248-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Hardy RH, Clapham JC. Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br. 1951;33-B:376-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 512] [Cited by in RCA: 508] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 19. | Nakagawa S, Fukushi J, Nakagawa T, Mizu-Uchi H, Iwamoto Y. Association of Metatarsalgia After Hallux Valgus Correction With Relative First Metatarsal Length. Foot Ankle Int. 2016;37:582-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Liu GT, Chhabra A, Dayton MJ, Dayton PD, Duke WJ, Farber DC, Hatch DJ, Kile DA, Koay J, McAleer JP, Raissi A, Raspovic KM, Santrock RD, Taylor RP, VanPelt MD, Wukich DK. One- and Two-Year Analysis of a Five-Year Prospective Multicenter Study Assessing Radiographic and Patient-Reported Outcomes Following Triplanar First Tarsometatarsal Arthrodesis With Early Weightbearing for Symptomatic Hallux Valgus. J Foot Ankle Surg. 2022;61:1308-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Reference Citation Analysis (0)] |
| 21. | Pearce CJ, Calder JD. Metatarsalgia: proximal metatarsal osteotomies. Foot Ankle Clin. 2011;16:597-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Attar F. Radiological Outcome of Patients with Splay Foot Following 1st and 5th Metatarsal Osteotomies Performed Simultaneously on the Same Foot. MOJ Orthop Rheumatol. 2014;. [DOI] [Full Text] |
| 23. | DeSandis B, Ellis SJ, Levitsky M, O'Malley Q, Konin G, O'Malley MJ. Rate of Union After Segmental Midshaft Shortening Osteotomy of the Lesser Metatarsals. Foot Ankle Int. 2015;36:1190-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Galluch DB, Bohay DR, Anderson JG. Midshaft metatarsal segmental osteotomy with open reduction and internal fixation. Foot Ankle Int. 2007;28:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Yamamoto K, Imakiire A, Katori Y, Masaoka T, Koizumi R. Clinical results of modified Mitchell's osteotomy for hallux valgus augmented with oblique lesser metatarsal osteotomy. J Orthop Surg (Hong Kong). 2005;13:245-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Panagakos P, Patel K, Gonzalez CN. Lisfranc arthrodesis. Clin Podiatr Med Surg. 2012;29:51-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Lu J, Zhao H, Liang X, Ma Q. Comparison of Minimally Invasive and Traditionally Open Surgeries in Correction of Hallux Valgus: A Meta-Analysis. J Foot Ankle Surg. 2020;59:801-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 28. | Flores-Carrillo A, Farías Cisneros E, Ruiz Osuna C. [Minimally invasive treatment of mild and moderate hallux valgus]. Acta Ortop Mex. 2009;23:272-276. [PubMed] |
| 29. | Huang PJ, Lin YC, Fu YC, Yang YH, Cheng YM. Radiographic evaluation of minimally invasive distal metatarsal osteotomy for hallux valgus. Foot Ankle Int. 2011;32:S503-S507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |