Published online Feb 18, 2024. doi: 10.5312/wjo.v15.i2.180
Peer-review started: October 25, 2023
First decision: December 11, 2023
Revised: December 20, 2023
Accepted: January 22, 2024
Article in press: January 22, 2024
Published online: February 18, 2024
Processing time: 104 Days and 17.9 Hours
Total knee arthroplasty (TKA) is a mature procedure recommended for correcting knee osteoarthritis deformity, relieving pain, and restoring normal biomechanics. Although TKA is a successful and cost-effective procedure, patient dissatisfaction is as high as 50%. Knee pain after TKA is a significant cause of patient dissatisfaction; the most common location for residual pain is the anterior region. Between 4% and 40% of patients have anterior knee pain (AKP).
To investigate the effect of various TKA procedures on postoperative AKP.
We searched PubMed, EMBASE, and Cochrane from January 2000 to September 2022. Randomized controlled trials with one intervention in the experimental group and no corresponding intervention (or other interventions) in the control group were collected. Two researchers independently read the title and abstract of the studies, preliminarily screened the articles, and read the full text in detail according to the selection criteria. Conflicts were resolved by consultation with a third researcher. And relevant data from the included studies were extracted and analyzed using Review Manager 5.4 software.
There were 25 randomized controlled trials; 13 were comparative studies with or without patellar resurfacing. The meta-analysis showed no significant difference between the experimental and control groups (P = 0.61). Six studies were comparative studies of circumpatellar denervation vs non-denervation, divided into three subgroups for meta-analysis. The two-subgroup meta-analysis showed no significant difference between the experimental and the control groups (P = 0.31, P = 0.50). One subgroup meta-analysis showed a significant difference between the experimental and control groups (P = 0.001). Two studies compared fixed-bearing TKA and mobile-bearing TKA; the results meta-analysis showed no significant difference between the experimental and control groups (P = 0.630). Two studies compared lateral retinacular release vs non-release; the meta-analysis showed a significant difference between the experimental and control groups (P = 0.002); two other studies compared other factors.
Patellar resurfacing, mobile-bearing TKA, and fixed-bearing TKA do not reduce the incidence of AKP. Lateral retinacular release can reduce AKP; however, whether circumpatellar denervation can reduce AKP is controversial.
Core Tip: In our meta-analysis, we searched PubMed, EMBASE, and Cochrane from January 2000 to September 2022, and we included only high level randomized controlled trials in order to get more accurate results. We discussed the influence of multiple factors on anterior knee pain after total knee arthroplasty, with different results from previous studies.
- Citation: Feng H, Feng ML, Cheng JB, Zhang X, Tao HC. Meta-analysis of factors influencing anterior knee pain after total knee arthroplasty. World J Orthop 2024; 15(2): 180-191
- URL: https://www.wjgnet.com/2218-5836/full/v15/i2/180.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i2.180
Knee osteoarthritis is a chronic joint disease characterized by articular cartilage degeneration and secondary hyperosteogeny[1]. The primary symptom is pain during knee joint weight-bearing and activity, severely affecting the quality of life. In the early stage, conservative treatment with medication is effective; however, in the middle and late stages (especially in the end stage), knee pain is severe, and the effective treatment is knee replacement[2,3]. Total knee arthroplasty (TKA) is a mature procedure recommended for correcting knee osteoarthritis deformity, relieving pain, and restoring normal biomechanics[4]. The patients enjoy excellent long-term survival[5-8]. Although TKA is a successful and cost-effective procedure, patient dissatisfaction is as high as 50%. Knee pain after TKA is a significant cause of patient dissatisfaction; the most common location for residual pain is the anterior region[9]. Between 4% and 40% of patients have anterior knee pain (AKP)[10-12]. In this review, we searched PubMed, EMBASE, and the Cochrane database for randomized controlled trials related to AKP after TKA to explore the effects of various TKA approaches on AKP.
Studies were selected based on the following inclusion criteria: (1) Type of studies: A randomized controlled trial; (2) subjects: Patients undergoing TKA for the first time; (3) intervention: Not limited; (4) control group: Intervention different from the experimental group or no intervention; and (5) evaluation indicators: Occurrence of AKP (incidence and pain degree). The exclusion criteria were as follows: Patellar surgery, fracture history, high tibial osteotomy, no AKP, review or expert reports, cadaveric studies, model studies, and case reports.
PubMed, EMBASE, and the Cochrane Library were searched from January 2000 to September 2022. The keywords were “Total Knee Arthroplasty”, “Anterior Knee Pain”, and other related Medline search heading terms or expressions.
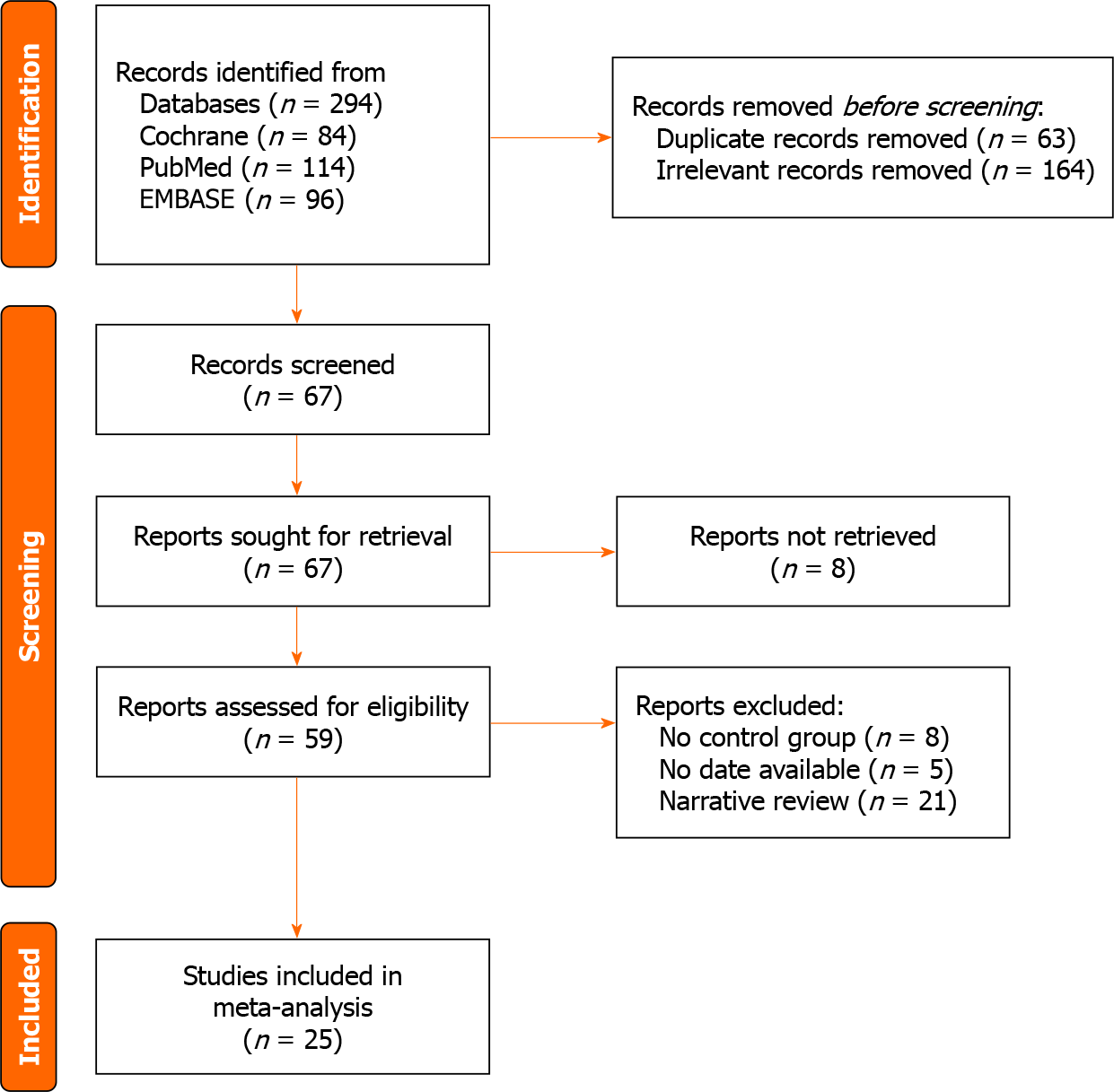
Two researchers independently read the title and abstract of the studies, preliminarily screened the articles, and read the full text in detail according to the selection criteria. Conflicts were resolved by consultation with a third researcher. We retrieved 294 articles from three databases. After reading the title and abstract, 67 articles were identified. After reading the full text, articles without AKP were excluded, and the controversies were resolved. Finally, 25 articles were included in this review. A flowchart of the studies considered for inclusion is shown in Figure 1.
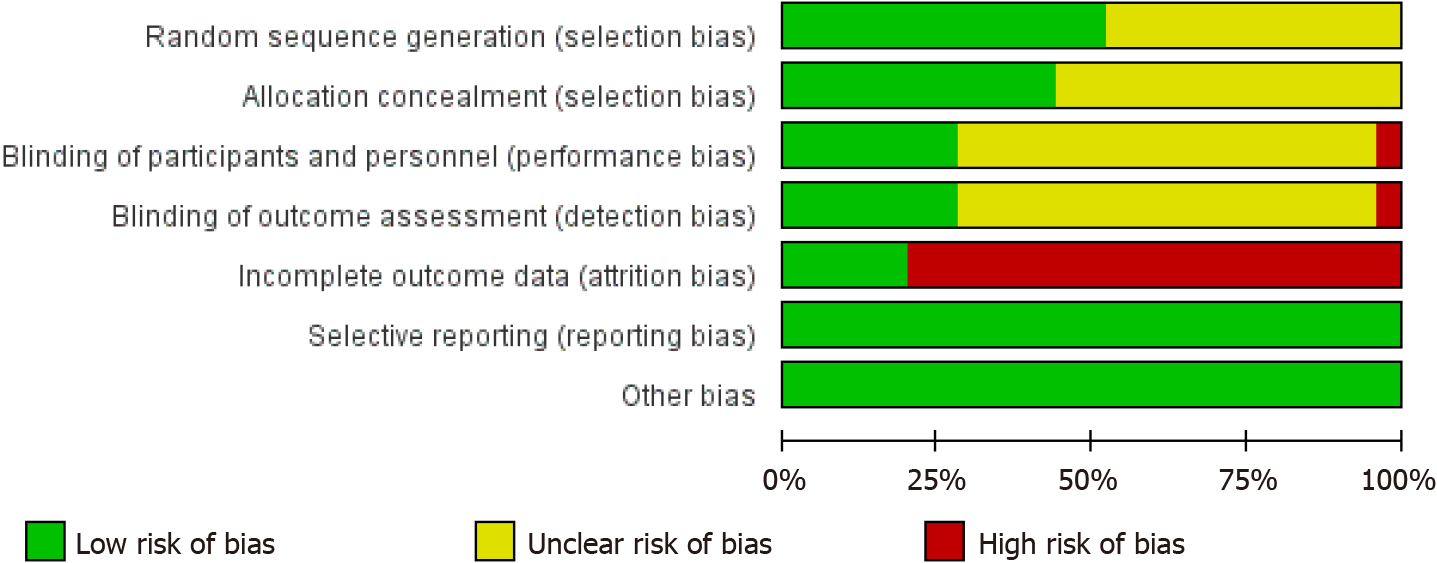
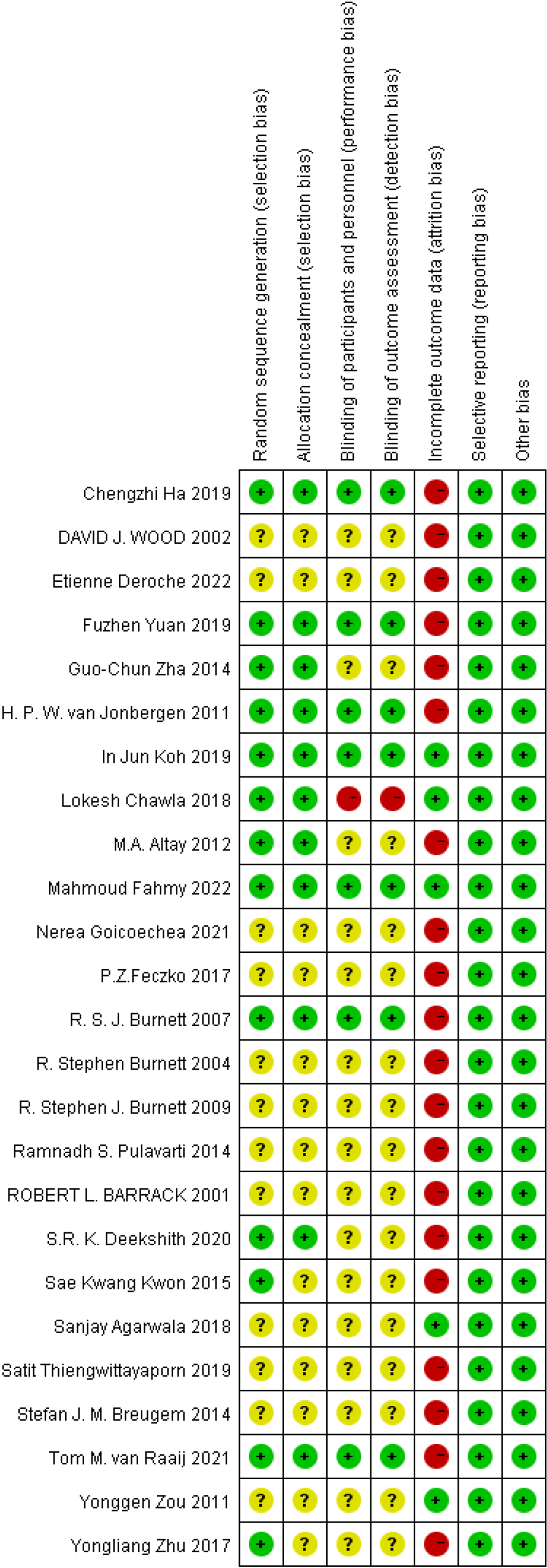
According to the Cochrane Risk of Bias tool, the risk of bias of each randomized controlled trial was graded as low, high, or unclear based on: (1) Random sequence generation; (2) allocation concealment; (3) blinding of participants and personnel; (4) blinding of outcome assessment; (5) incomplete outcome data; (6) selective reporting, and (7) other bias. The risk of bias assessments is shown in Figures 2 and 3.
Data on study design, study population, interventions, and outcomes were extracted from the included articles’ text, figures, and tables. Dichotomous outcomes were expressed as risk ratios with 95% confidence intervals (95%CIs), while continuous outcomes were expressed as mean or standard mean differences with 95%CI. Heterogeneity was expressed as P and I². This value of I² ranges from 0% (complete consistency) to 100% (complete inconsistency). If the P value of the heterogeneity test was < 0.1 or I² > 50%, a random-effects model was used in place of the fixed modality.
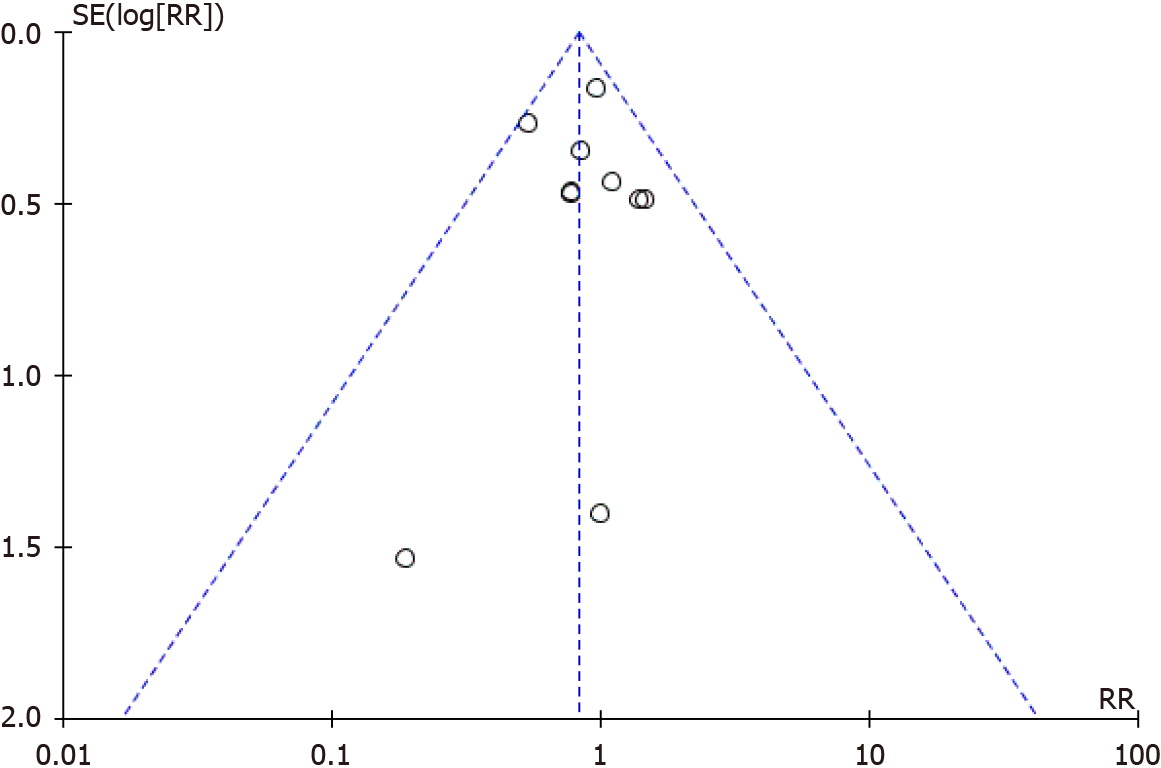
Publication bias was tested using funnel plots. Forest plots were used to graphically present the results of individual studies and the respective pooled effect size estimate. All statistical analyses were performed using Review Manager version 5.4.
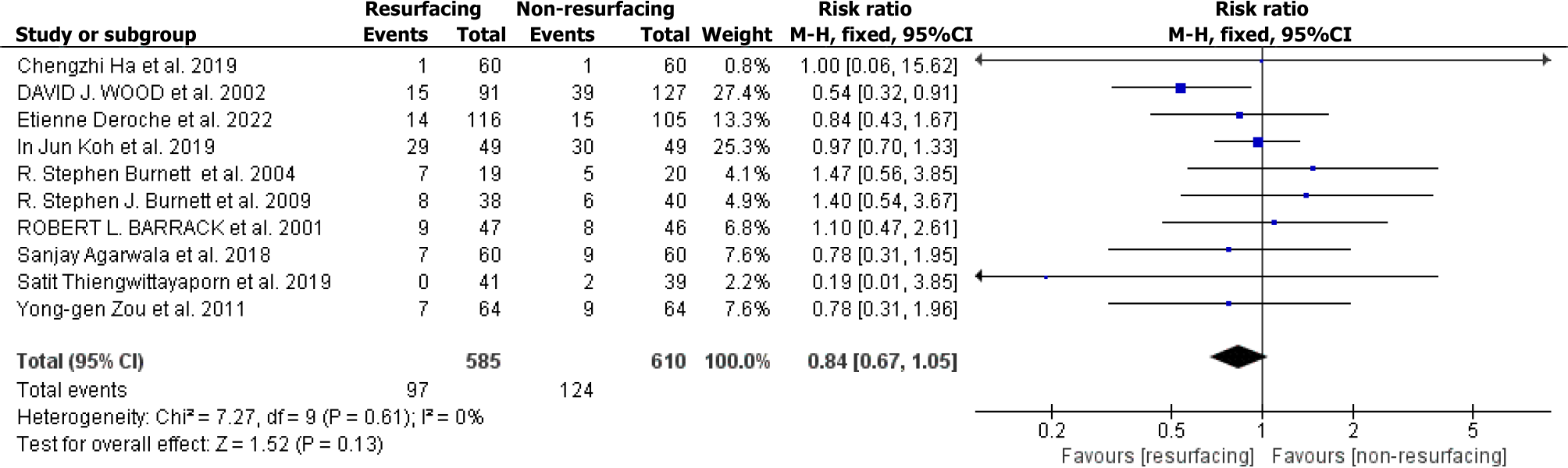
We included 13 studies on the effect of patellar replacement on AKP after TKA[4,13-24]. Ten reported the number of patients with AKP in each group, and the remaining three evaluated AKP using a visual analog scale (VAS) and hospital for special surgeries patellar score. These three studies did not conduct meta-analyses. There were 1197 TKA patients in these ten studies, including 586 TKA patients with patellar resurfacing (121 AKP) and 611 TKA patients without patellar resurfacing (100 AKP). The basic information of the ten studies (Table 1) and the forest plot (Figure 4) and funnel plot (Figure 5) of the meta-analysis are as follows (I² = 0%, using the fixed modality, P = 0.13, suggesting that there was no significant difference between the two groups. The funnel plot was symmetrical, suggesting no publication bias).
| Ref. | Follow-up time | Patients included (resurfacing/non-resurfacing) | Resurfacing | Non-resurfacing | ||
| Patients with AKP | Patients available | Patients with AKP | Patients available | |||
| Koh et al[16], 2019 | 5 yr | 49/49 | 29 | 49 | 30 | 49 |
| Thiengwittayaporn et al[15], 2019 | 1 yr | 42/42 | 0 | 41 | 2 | 39 |
| Ha et al[17], 2019 | 5 yr | 66/66 | 1 | 60 | 1 | 60 |
| Deroche et al[13], 2022 | 18.0 months (mean) | 123/123 | 14 | 116 | 15 | 105 |
| Agarwala et al[4], 2018 | 19.0 months | 60/60 | 7 | 60 | 9 | 60 |
| Zou et al[19], 2011 | 16.5 months (mean) | 64/64 | 7 | 64 | 9 | 64 |
| Burnett et al[22], 2004 | 10 yr | 50/50 | 7 | 19 | 5 | 20 |
| Burnett et al[20], 2009 | 10 yr | 59/59 | 8 | 38 | 6 | 40 |
| Barrack et al[24], 2001 | 70.5 months | 59/59 | 9 | 47 | 8 | 46 |
| Wood et al[23], 2002 | 48.0 months (mean) | 110/110 | 15 | 91 | 39 | 127 |
Six studies[25-30] compared circumpatellar denervation with non-denervation in TKA. The patellofemoral Feller score (PFS) was used to evaluate postoperative AKP in two studies, VAS was used in two studies, and the remaining two reported the number of cases of AKP in each group; therefore, they were divided into three subgroups for meta-analysis. The basic information of the six articles is presented in Tables 2 and 3.
| Ref. | Follow-up time | Patients available (denervation/non-denervation) | Score | Denervation | Non-denervation | ||
| Mean | SD | Mean | SD | ||||
| Kwon et al[26], 2015 | 5 yr | 50/50 | PFS | 14.10 | 1.00 | 14.20 | 1.20 |
| Goicoechea et al[25], 2021 | 1 yr | 88/81 | PFS | 12.60 | 3.50 | 13.60 | 2.70 |
| Altay et al[27], 2012 | 3 yr | 35/35 | VAS | 2.20 | 1.10 | 2.82 | 1.20 |
| Deekshith et al[30], 2020 | 2 yr | 50/49 | VAS | 1.34 | 0.47 | 1.60 | 0.53 |
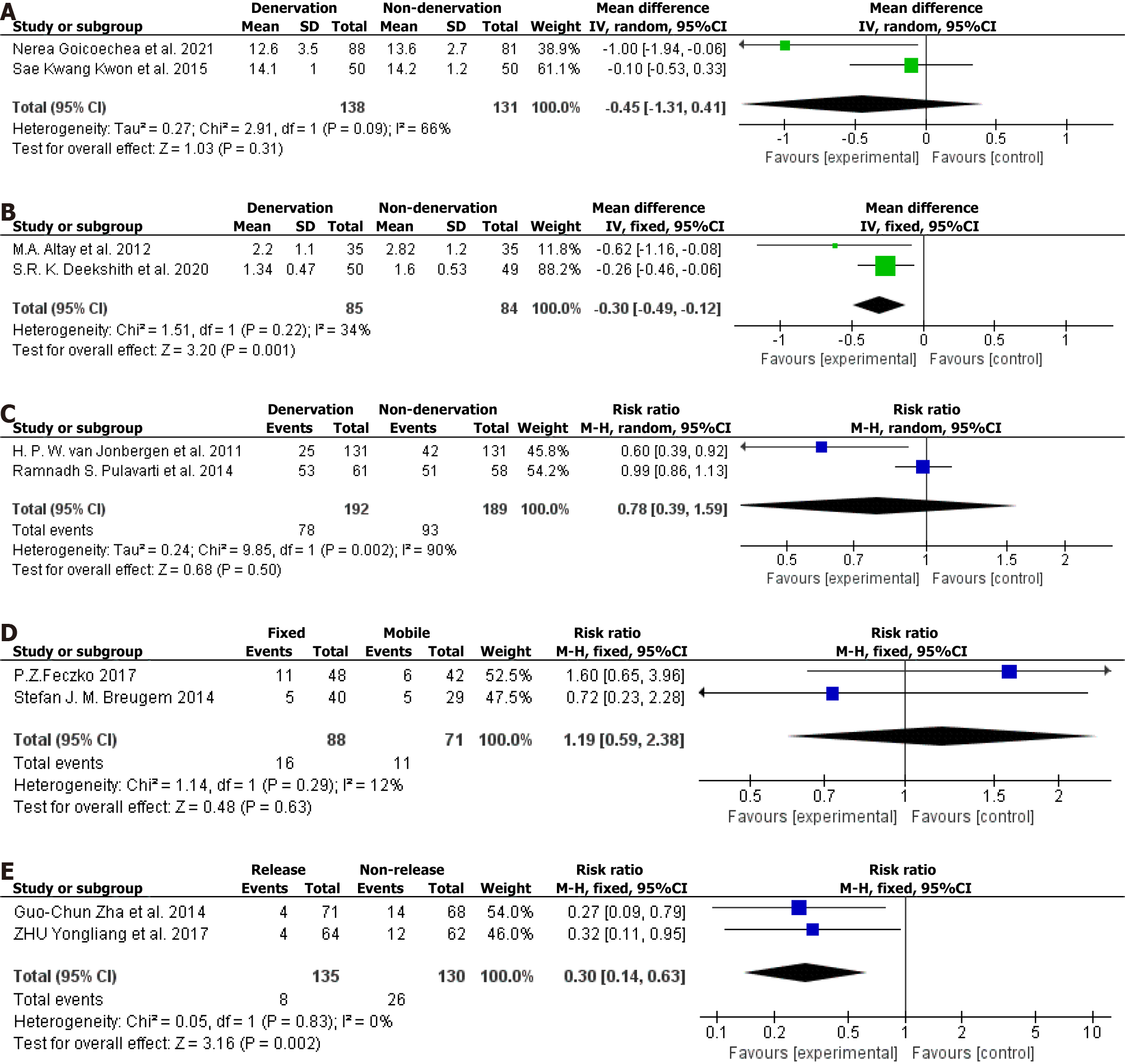
There were two studies[25,26] with 138 cases in the denervation group and 131 in the non-denervation group. The meta-analysis forest plot is shown in Figure 6A (I² = 66%, using the random-effects model, P = 0.31, suggesting no significant difference between the groups).
There were two studies with 85 patients in the denervation group and 84 in the non-denervation group[27,30]. The meta-analysis forest plot is shown in Figure 6B (I² = 34%, using the fixed modality, P = 0.001, suggesting that the difference between the groups was statistically significant).
There were two studies with 213 patients in the denervation group and 213 in the non-denervation group[28,29]. The meta-analysis forest plot is shown in Figure 6C (I² = 90%, using the random-effects model, P = 0.50, suggesting no significant difference between the groups).
There were two studies comparing mobile-bearing and fixed-bearing designs. There were 88 cases of fixed-bearing and 71 of mobile-bearing[31,32]. The basic information of the studies (Table 4) and the forest plot of meta-analysis (Figure 6D) are as follows (I² = 12%, using the fixed modality, P = 0.63, suggesting that there was no significant difference between the two groups).
We included two comparative studies of lateral retinacular release and non-release, with 135 cases in the release group and 130 in the non-release group[33,34]. The basic information of the two studies (Table 5) and the forest plot of meta-analysis (Figure 6E) are as follows (I² = 0%, using the fixed modality, P = 0.002, suggesting that the difference between the two groups was statistically significant).
Yuan et al[35] reported differences in patellofemoral function, clinical outcomes, and radiographic parameters between the freehand and cutting guide patellar resection techniques in patients undergoing TKA. The authors randomly assigned 100 patients to the freehand technique group and the cutting guide technique group, with 50 patients in each group. Finally, 42 patients in the cutting guide technique group and 44 patients in the freehand technique group were available for analysis. AKP occurred in 7.14% of the patients in the cutting guide technique group and 9.09% in the freehand technique group. There was no significant difference between the two groups. Fahmy et al[36] randomized into an experimental group, including patients with complete excision of the infrapatellar pad of fat (IPFP) and the control group with IPFP preservation. The authors randomly assigned 90 patients to the experimental and the control groups. At 6 months follow-up, 10 knees and 14 knees had AKP in IPFP preservation and excision group patients, respectively. The pain decreased during the follow-up period until the number of cases was almost equal at the final visit. There was no significant difference in AKP between the groups. Each group’s mean VAS pain scores were comparable throughout the recorded follow-up period.
Patellar resurfacing in TKA has long been controversial; some authors believe that patellar resurfacing can improve patient satisfaction, reduce postoperative AKP, and reduce the revision rate[37-40], while others hold the opposite view[41,42]. We analyzed 13 randomized controlled trials of patellar resurfacing and non-resurfacing. Of these, 12 showed no significant difference in postoperative AKP between the groups. Wood et al[23] showed that postoperative AKP was lower in the patellar resurfacing group than in the non-resurfacing group. In that study, surgery was performed by one of six experienced surgeons or their trainees under their supervision, and the follow-up time varied substantially (36-79 months, mean 48 months). Different surgeons have different surgical preferences, and the postoperative results also show substantial differences. The patients were followed up for a minimum of 36 months and a maximum of 79 months. The incidence of AKP and the severity of pain after TKA decreased with time. Therefore, comparing results at 36 and 79 months is not appropriate. These reasons may explain the different results between Wood et al[23] and other studies
Our meta-analysis showed no significant difference in the incidence of postoperative AKP between the patellar resurfacing group and the non-resurfacing group. Patellar resurfacing increases the operative time and blood loss. Furthermore, the patella in Asians is generally thin, leading to an increased risk of postoperative patellar fracture[41,42]. Therefore, we do not recommend patellar resurfacing in TKA.
The peripatellar soft tissue and retropatellar fat pad have been reported to be the source of AKP[43,44]. Immunohistochemical studies of nerve distribution in this area have shown the presence of substance-p nociceptive fibers in the peripatellar soft tissue[45]. Electrocautery disables these pain receptors and achieves desensitization or denervation of the anterior knee region. Thus, postoperative AKP can be reduced[46,47]. In our review, six studies compared circumpatellar denervation and non-denervation in TKA. Due to the inconsistency of the indicators to evaluate postoperative AKP, the meta-analysis was divided into three subgroups.
The results of the PFS score subgroup with AKP showed no significant difference between the denervation and non-denervation groups, while the VAS score subgroup showed that denervation was superior to non-denervation. Due to the large incision of TKA, peripatellar soft tissue and retropatellar fat pad are injured to a greater extent; therefore, achieving the surgical goal by performing only circumpatellar denervation is challenging. The heterogeneity among the six studies was considerable. The sample size was small, and the power of meta-analysis was weak; therefore, more studies are needed.
The theoretical advantage of the mobile-bearing TKA is the ability to self-align and accommodate minor mismatches[32]. The design of the mobile-bearing TKA could lead to a better range of motion during knee flexion activities[48]. Breugem et al[12] found that over a one-year follow-up, the incidence of postoperative AKP of mobile-bearing TKA was lower than that of fixed-bearing TKA. However, postoperative AKP tended to be the same over time[32]. This result is similar to other studies[49,50]. This review included two studies comparing fixed-bearing TKA and mobile-bearing TKA, with follow-up times of 5.0 and 7.9 years, respectively. The meta-analysis showed no difference in the incidence of AKP between the groups. Therefore, the advantage of mobile-bearing TKA might decrease over time.
Theoretically, proper lateral retinacular release improves patellar tracking and reduces patellofemoral contact pressure. These factors have been reported to be closely related to AKP[51,52]. In a prospective cohort study of 271 patients, Lee et al[51] found that patients who underwent patellar decompression had less AKP than those who did not. Wilson et al[52] found that patients with AKP had abnormal patellar tracking compared with patients without AKP. This review included two studies comparing lateral retinacular release and non-release in TKA. The meta-analysis showed that lateral retinacular release reduced AKP. No studies reported that lateral retinacular release produces adverse postoperative complications. Proper lateral retinacular release increases the intraoperative field of vision, which is conducive to successful outcomes.
In patellar resections when conducting TKA, a number of principles should be considered including restoring patellar height, performing a symmetric resection, avoiding under-resection, and minimizing over-stuffing of the patellofemoral joint[53]. Reasonable patellar excision is more beneficial to the installation of patellar components. At the same time, reasonable excision can reduce AKP, patellar fracture and patellar injury[54,55]. This review included one study comparing freehand and cutting guide patellar resection techniques in TKA. In their prospective randomized controlled trial, no statistically significant difference was observed in the incidence of AKP between the two groups. Therefore, better knee function may be more related to basic principles, including excellent lower limb alignment, proper prosthetic placement, intact ligaments, and greater lower limb strength[35].
The IPFP is a piece of fat tissue located between the patellar ligament, the inferior patellar end, and the proximal tibia. Anatomically, it is considered to be an intraarticular extrasynovial compartment that may support effective joint lubrication[56]. The sufficient surgical exposure often prompts many surgeons to remove it during surgery, as there is debate about the effectiveness of its removal, but there is not complete agreement. In the study of Fahmy et al[36], the difference of the postoperative AKP, range of motion, oxford knee score and the clinical outcomes whether infrapatellar fat pad was excised or not were statistically insignificant. Therefore, surgeons had better to save the IPFP if conventional exposure can be reached; otherwise, resection is preferred to improve exposure.
The exact pathogenesis of AKP may be multifactorial. Laubach et al[57] concluded that quadriceps muscle strength, inlay thickness, and the patella position might be of particular relevance in avoiding postsurgical AKP. The results of another study suggest that the successful repair of the medial patellofemoral ligament after using a medial parapatellar approach in TKA could reduce the high rate of postoperative AKP[58]. There are many other factors that may be related to AKP after TKA[59-61]. Due to the lack of randomized controlled trials in the exploration of these factors, they were not included in the meta-analysis of this study.
Our meta-analysis had several strengths. First, it resulted in a different conclusion from the 2 reached in earlier meta-analyses[62,63]. In the study by Duan et al[62], the results showed that patellar resurfacing had a significant protective effect on AKP with low heterogeneity and robust results. In our analysis, the incidence of AKP was not statistically significant with or without patellar replacement in TKA. A meta-analysis conducted by Xie et al[63]. concluded that patellar denervation could significantly relieve AKP during follow-up up to 12 months, but not beyond 12 months. We found that the results of different assessment methods for AKP were different. Second, only randomized controlled trials were included in our study, and the results obtained were more accurate. Third, the studies we included were screened independently by two researchers according to inclusion and exclusion criteria, we used Cochrane Risk of Bias tool to assess publication bias, and these results indicated that publication bias was well controlled. This meta-analysis also had limitations. First, only a small number of trials was analyzed since we only included randomized controlled trials. Second, there is no single definition of AKP, and distinguishing patellofemoral pain syndrome is difficult. Third, the studies included in the meta-analysis applied different techniques and diagnostic criteria to AKP, which could lead to performance bias. Given these limitations, more high-level research is still needed in the future.
This meta-analysis of currently available evidence indicates that patellar resurfacing, mobile-bearing TKA, and fixed-bearing TKA can’t relieve AKP postoperatively after TKA. We do not recommend patellar replacement in TKA unless patellar replacement is necessary. In evaluating the effect of patellar denervation on TKA, the results of different assessment methods for AKP were different. Therefore, future high-level research is warranted for validation. Besides, lateral retinacular release in TKA is recommended because it is safe and result in good clinical outcomes in controlling AKP.
Knee osteoarthritis seriously affects the quality of life of the elderly. Total knee arthroplasty (TKA) is an effective treatment for end-stage osteoarthritis. Anterior knee pain (AKP) after TKA is the main cause of dissatisfaction in the elderly. The management of AKP after total knee replacement is very important.
Although total knee replacement is very successful, postoperative AKP is common and a major cause of patient dissatisfaction. By studying the influencing factors of AKP after TKA, we can improve the quality of life of patients and improve the surgical methods.
To study the influencing factors of AKP after TKA. We identified certain intraoperative factors that may improve the occurrence of postoperative AKP. It provides some help for the management of AKP after TKA.
This study is a meta-analysis. We combined some previous randomized controlled trials to get new conclusions. We analyzed the influence of several different factors on AKP after TKA.
There are few randomized controlled trials for many factors, and more high-quality studies are needed to further explore.
We found that patellar replacement or not did not affect the incidence of postoperative AKP. We found that different assessment methods for AKP may produce different results.
More randomized controlled trials are needed for further validation in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ng BW, Malaysia;
| 1. | Hussain SM, Neilly DW, Baliga S, Patil S, Meek R. Knee osteoarthritis: a review of management options. Scott Med J. 2016;61:7-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 108] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Jang S, Lee K, Ju JH. Recent Updates of Diagnosis, Pathophysiology, and Treatment on Osteoarthritis of the Knee. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 288] [Article Influence: 72.0] [Reference Citation Analysis (0)] |
| 3. | Michael JW, Schlüter-Brust KU, Eysel P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch Arztebl Int. 2010;107:152-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 254] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 4. | Agarwala S, Shetty V, Karumuri LK, Vijayvargiya M. Patellar Resurfacing versus Nonresurfacing with Patellaplasty in Total Knee Arthroplasty. Indian J Orthop. 2018;52:393-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Gill GS, Joshi AB. Long-term results of cemented, posterior cruciate ligament-retaining total knee arthroplasty in osteoarthritis. Am J Knee Surg. 2001;14:209-214. [PubMed] |
| 6. | Pavone V, Boettner F, Fickert S, Sculco TP. Total condylar knee arthroplasty: a long-term followup. Clin Orthop Relat Res. 2001;18-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 112] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Rodriguez JA, Bhende H, Ranawat CS. Total condylar knee replacement: a 20-year followup study. Clin Orthop Relat Res. 2001;10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 172] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 8. | Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 299] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 9. | Park CN, White PB, Meftah M, Ranawat AS, Ranawat CS. Diagnostic Algorithm for Residual Pain After Total Knee Arthroplasty. Orthopedics. 2016;39:e246-e252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 10. | Popovic N, Lemaire R. Anterior knee pain with a posterior-stabilized mobile-bearing knee prosthesis: the effect of femoral component design. J Arthroplasty. 2003;18:396-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2003;85:212-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 205] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 12. | Breugem SJ, Sierevelt IN, Schafroth MU, Blankevoort L, Schaap GR, van Dijk CN. Less anterior knee pain with a mobile-bearing prosthesis compared with a fixed-bearing prosthesis. Clin Orthop Relat Res. 2008;466:1959-1965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Deroche E, Batailler C, Swan J, Sappey-Marinier E, Neyret P, Servien E, Lustig S. No difference between resurfaced and non-resurfaced patellae with a modern prosthesis design: a prospective randomized study of 250 total knee arthroplasties. Knee Surg Sports Traumatol Arthrosc. 2022;30:1025-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 14. | Raaij TMV, Meij EV, Vries AJ, Raay JJAMV. Patellar Resurfacing Does Not Improve Clinical Outcome in Patients with Symptomatic Tricompartmental Knee Osteoarthritis. An RCT Study of 40 Patients Receiving Primary Cruciate Retaining Total Knee Arthroplasty. J Knee Surg. 2021;34:1503-1509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Thiengwittayaporn S, Srungboonmee K, Chiamtrakool B. Resurfacing in a Posterior-Stabilized Total Knee Arthroplasty Reduces Patellar Crepitus Complication: A Randomized, Controlled Trial. J Arthroplasty. 2019;34:1969-1974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Koh IJ, Kim MS, Sohn S, Song KY, Choi NY, In Y. Patients undergoing total knee arthroplasty using a contemporary patella-friendly implant are unaware of any differences due to patellar resurfacing. Knee Surg Sports Traumatol Arthrosc. 2019;27:1156-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 17. | Ha C, Wang B, Li W, Sun K, Wang D, Li Q. Resurfacing versus not-resurfacing the patella in one-stage bilateral total knee arthroplasty: a prospective randomized clinical trial. Int Orthop. 2019;43:2519-2527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 18. | Chawla L, Bandekar S M, Dixit V, Ambareesh P, Krishnamoorthi A, Mummigatti S. Functional outcome of patellar resurfacing vs non resurfacing in Total Knee Arthoplasty in elderly: a prospective five year follow-up study. Journal Arthrosc Jt Surg. 2019;6:65-69. [DOI] [Full Text] |
| 19. | Zou YG, Chen ZW, Feng ZQ, Xing JS. Factors related to anterior knee pain after total knee arthroplasty. Nan Fang Yi Ke Da Xue Xue Bao. 2011;31:1428-1430. [PubMed] |
| 20. | Burnett RS, Boone JL, Rosenzweig SD, Steger-May K, Barrack RL. Patellar resurfacing compared with nonresurfacing in total knee arthroplasty. A concise follow-up of a randomized trial. J Bone Joint Surg Am. 2009;91:2562-2567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL. A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res. 2007;464:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 97] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 22. | Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. Patella resurfacing versus nonresurfacing in total knee arthroplasty: results of a randomized controlled clinical trial at a minimum of 10 years' followup. Clin Orthop Relat Res. 2004;12-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 114] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 23. | Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: a prospective, randomized trial. J Bone Joint Surg Am. 2002;84:187-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 163] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 24. | Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L. Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg Am. 2001;83:1376-1381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 181] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 25. | Goicoechea N, Hinarejos P, Torres-Claramunt R, Leal-Blanquet J, Sánchez-Soler J, Monllau JC. Patellar denervation does not reduce post-operative anterior knee pain after primary total knee arthroplasty with patellar resurfacing. Knee Surg Sports Traumatol Arthrosc. 2021;29:3346-3351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 26. | Kwon SK, Nguku L, Han CD, Koh YG, Kim DW, Park KK. Is Electrocautery of Patella Useful in Patella Non-Resurfacing Total Knee Arthroplasty?: A Prospective Randomized Controlled Study. J Arthroplasty. 2015;30:2125-2127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Altay MA, Ertürk C, Altay N, Akmeşe R, Işıkan UE. Patellar denervation in total knee arthroplasty without patellar resurfacing: a prospective, randomized controlled study. Orthop Traumatol Surg Res. 2012;98:421-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Pulavarti RS, Raut VV, McLauchlan GJ. Patella denervation in primary total knee arthroplasty - a randomized controlled trial with 2 years of follow-up. J Arthroplasty. 2014;29:977-981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | van Jonbergen HP, Scholtes VA, van Kampen A, Poolman RW. A randomised, controlled trial of circumpatellar electrocautery in total knee replacement without patellar resurfacing. J Bone Joint Surg Br. 2011;93:1054-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 30. | Deekshith SRK, Reddy KJ, Raviteja R. RETRACTED ARTICLE: Patelloplasty in total knee arthroplasty with circumpatellar denervation versus without denervation - a randomized prospective study. Arthroplasty. 2020;2:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Feczko PZ, Jutten LM, van Steyn MJ, Deckers P, Emans PJ, Arts JJ. Comparison of fixed and mobile-bearing total knee arthroplasty in terms of patellofemoral pain and function: a prospective, randomised, controlled trial. BMC Musculoskelet Disord. 2017;18:279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 32. | Breugem SJ, van Ooij B, Haverkamp D, Sierevelt IN, van Dijk CN. No difference in anterior knee pain between a fixed and a mobile posterior stabilized total knee arthroplasty after 7.9 years. Knee Surg Sports Traumatol Arthrosc. 2014;22:509-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 33. | Zhu Y, Li Y, Yan C, Du X, Xing Z, Chen P. Influence of lateral retinacular release on anterior knee pain following total knee arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017;31:541-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 34. | Zha GC, Sun JY, Dong SJ. Less anterior knee pain with a routine lateral release in total knee arthroplasty without patellar resurfacing: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. 2014;22:517-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 35. | Yuan F, Sun Z, Wang H, Chen Y, Yu J. Clinical and radiologic outcomes of two patellar resection techniques during total knee arthroplasty: a prospective randomized controlled study. Int Orthop. 2019;43:2293-2301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 36. | Fahmy M, Seifeldin AF. The impact of infrapatellar fat pad excision vs preservation after total knee replacement on anterior knee pain, functional outcome and patellar height: Randomized controlled trial. J Orthop, Trau and Rehabil. 2022;29. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 37. | Adravanti P, Tecame A, de Girolamo L, Ampollini A, Papalia R. Patella Resurfacing in Total Knee Arthroplasty: A Series of 1280 Patients at Midterm Follow-Up. J Arthroplasty. 2018;33:696-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Longo UG, Ciuffreda M, Mannering N, D'Andrea V, Cimmino M, Denaro V. Patellar Resurfacing in Total Knee Arthroplasty: Systematic Review and Meta-Analysis. J Arthroplasty. 2018;33:620-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 39. | Maney AJ, Koh CK, Frampton CM, Young SW. Usually, Selectively, or Rarely Resurfacing the Patella During Primary Total Knee Arthroplasty: Determining the Best Strategy. J Bone Joint Surg Am. 2019;101:412-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 40. | Migliorini F, Eschweiler J, Niewiera M, El Mansy Y, Tingart M, Rath B. Better outcomes with patellar resurfacing during primary total knee arthroplasty: a meta-analysis study. Arch Orthop Trauma Surg. 2019;139:1445-1454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 41. | Allen W, Eichinger J, Friedman R. Resurfaced versus Non-Resurfaced Patella in Total Knee Arthroplasty. J Knee Surg. 2019;32:611-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 42. | Grassi A, Compagnoni R, Ferrua P, Zaffagnini S, Berruto M, Samuelsson K, Svantesson E, Randelli P. Patellar resurfacing versus patellar retention in primary total knee arthroplasty: a systematic review of overlapping meta-analyses. Knee Surg Sports Traumatol Arthrosc. 2018;26:3206-3218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 43. | Maculé F, Sastre S, Lasurt S, Sala P, Segur JM, Mallofré C. Hoffa's fat pad resection in total knee arthroplasty. Acta Orthop Belg. 2005;71:714-717. [PubMed] |
| 44. | Lehner B, Koeck FX, Capellino S, Schubert TE, Hofbauer R, Straub RH. Preponderance of sensory versus sympathetic nerve fibers and increased cellularity in the infrapatellar fat pad in anterior knee pain patients after primary arthroplasty. J Orthop Res. 2008;26:342-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 45. | Wojtys EM, Beaman DN, Glover RA, Janda D. Innervation of the human knee joint by substance-P fibers. Arthroscopy. 1990;6:254-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 158] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 46. | Maralcan G, Kuru I, Issi S, Esmer AF, Tekdemir I, Evcik D. The innervation of patella: anatomical and clinical study. Surg Radiol Anat. 2005;27:331-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 47. | Vega J, Golanó P, Pérez-Carro L. Electrosurgical arthroscopic patellar denervation. Arthroscopy. 2006;22:1028.e1-1028.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 48. | Haas BD, Komistek RD, Stiehl JB, Anderson DT, Northcut EJ. Kinematic comparison of posterior cruciate sacrifice versus substitution in a mobile bearing total knee arthroplasty. J Arthroplasty. 2002;17:685-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 50] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 49. | Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD, Jacofsky DJ. Rotating platform knees did not improve patellar tracking: a prospective, randomized study of 240 primary total knee arthroplasties. Clin Orthop Relat Res. 2004;221-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 66] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 50. | Aglietti P, Baldini A, Buzzi R, Lup D, De Luca L. Comparison of mobile-bearing and fixed-bearing total knee arthroplasty: a prospective randomized study. J Arthroplasty. 2005;20:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 94] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 51. | Lee GW, Lee SM, Jang SJ, Son JH. The efficacy of patellar decompression for improving anterior knee pain following total knee arthroplasty without patellar resurfacing. Arch Orthop Trauma Surg. 2013;133:561-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 52. | Wilson NA, Press JM, Koh JL, Hendrix RW, Zhang LQ. In vivo noninvasive evaluation of abnormal patellar tracking during squatting in patients with patellofemoral pain. J Bone Joint Surg Am. 2009;91:558-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 53. | Rand JA. Patellar resurfacing in total knee arthroplasty. Clin Orthop Relat Res. 1990;110-117. [PubMed] |
| 54. | Fu C, Wai J, Lee E, Myden C, Batuyong E, Hutchison CR, Anglin C. Computer-assisted patellar resection for total knee arthroplasty. Comput Aided Surg. 2012;17:21-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 55. | Pagnano MW, Trousdale RT. Asymmetric patella resurfacing in total knee arthroplasty. Am J Knee Surg. 2000;13:228-233. [PubMed] |
| 56. | Yao B, Samuel LT, Acuña AJ, Faour M, Roth A, Kamath AF, Mont MA. Infrapatellar Fat Pad Resection or Preservation during Total Knee Arthroplasty: A Systematic Review. J Knee Surg. 2021;34:415-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 57. | Laubach M, Hellmann JT, Dirrichs T, Gatz M, Quack V, Tingart M, Betsch M. Anterior knee pain after total knee arthroplasty: A multifactorial analysis. J Orthop Surg (Hong Kong). 2020;28:2309499020918947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 58. | Keshmiri A, Dotzauer F, Baier C, Maderbacher G, Grifka J, Sendtner E. Stability of capsule closure and postoperative anterior knee pain after medial parapatellar approach in TKA. Arch Orthop Trauma Surg. 2017;137:1019-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 59. | Aliyev O, Sarıkaş M, Uçan V, Uzer G, Tuncay İ, Yıldız F. Sagittal Patellar Offset Ratio Can Be a Predictor of Anterior Knee Pain after Primary Total Knee Arthroplasty without Patella Resurfacing. Z Orthop Unfall. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 60. | Antinolfi P, Manfreda F, Ricchiuto I, Petruccelli R, Caraffa A. Role of positioning of femoral component in the anterior-posterior direction on postoperative anterior pain in TKA. Eur J Orthop Surg Traumatol. 2020;30:1049-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 61. | Ertürk C, Altay MA, Işikan UE. Patelloplasty with patellar decompression to relieve anterior knee pain in total knee arthroplasty. Acta Orthop Traumatol Turc. 2011;45:425-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 62. | Duan G, Liu C, Lin W, Shao J, Fu K, Niu Y, Wang F. Different Factors Conduct Anterior Knee Pain Following Primary Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. J Arthroplasty. 2018;33:1962-1971.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 63. | Xie X, Pei F, Huang Z, Tan Z, Yang Z, Kang P. Does patellar denervation reduce post-operative anterior knee pain after total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc. 2015;23:1808-1815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |