Published online Feb 18, 2024. doi: 10.5312/wjo.v15.i2.118
Peer-review started: October 13, 2023
First decision: December 7, 2023
Revised: December 15, 2023
Accepted: January 9, 2024
Article in press: January 9, 2024
Published online: February 18, 2024
Processing time: 116 Days and 12.3 Hours
Advances in implant material and design have allowed for improvements in total knee arthroplasty (TKA) outcomes. A cruciate retaining (CR) TKA provides the least constraint of TKA designs by preserving the native posterior cruciate liga
To assess both short-term and mid-term clinical outcomes and PROMs of a novel CR TKA design.
A retrospective, multi-surgeon study identified 255 knees undergoing a TKA utilizing a kinematically designed CR Knee System (JOURNEY™ II CR; Smith and Nephew, Inc., Memphis, TN) at an urban, academic medical institution between March 2015 and July 2021 with a minimum of two-years of clinical follow-up with an orthopedic surgeon. Patient demographics, surgical information, clinical outcomes, and PROMs data were collected via query of electronic medical records. The PROMs collected in the present study included the Knee Injury and Osteoarthritis Outcome Score for Joint Replacement (KOOS JR) and Patient-Reported Outcomes Measurement Information System (PROMIS®) scores. The significance of improvements in mean PROM scores from preoperative scores to scores collected at six months and two-years postoperatively was analyzed using Independent Samples t-tests.
Of the 255 patients, 65.5% were female, 43.8% were White, and patients had an average age of 60.6 years. Primary osteoarthritis (96.9%) was the most common primary diagnosis. The mean surgical time was 105.3 minutes and mean length of stay was 2.1 d with most patients discharged home (92.5%). There were 18 emergency department (ED) visits within 90 d of surgery resulting in a 90 d ED visit rate of 7.1%, including a 2.4% orthopedic-related ED visit rate and a 4.7% non-orthopedic-related ED visit rate. There were three (1.2%) hospital readmissions within 90 d postoperatively. With a mean time to latest follow-up of 3.3 years, four patients (1.6%) required revision, two for arthrofibrosis, one for aseptic femoral loosening, and one for peri-prosthetic joint infection. There were significant improvements in KOOS JR, PROMIS Pain Intensity, PROMIS Pain Interference, PROMIS Mobility, and PROMIS Physical Health from preoperative scores to six month and two-year postoperative scores.
The evaluated implant is an effective, novel design offering excellent outcomes and low complication rates. At a mean follow up of 3.3 years, four patients required revisions, three aseptic and one septic, resulting in an overall implant survival rate of 98.4% and an aseptic survival rate of 98.8%. The results of our study demonstrate the utility of this kinematically designed implant in the setting of primary TKA.
Core Tip: This study aimed to assess mid-term clinical and patient-reported outcomes of 255 total knee arthroplasties (TKAs) using a novel, kinematically-designed cruciate retaining total knee arthroplasty implant. With a mean time to follow-up of 3.3 years, there was a high implant survival rate of 98.4%. Four patients (1.6%) required a revision TKA surgery, including three (1.2%) revised for aseptic indications. Patients who received the kinematically-designed cruciate retaining TKA showed significant improvements in Knee Injury and Osteoarthritis Outcome Score for Joint Replacement, Patient-Reported Outcomes Measurement Information System (PROMIS®) Pain Intensity, PROMIS Pain Interference, PROMIS Mobility, and PROMIS Physical Health.
- Citation: Katzman JL, Habibi AA, Haider MA, Cardillo C, Fernandez-Madrid I, Meftah M, Schwarzkopf R. Mid-term outcomes of a kinematically designed cruciate retaining total knee arthroplasty. World J Orthop 2024; 15(2): 118-128
- URL: https://www.wjgnet.com/2218-5836/full/v15/i2/118.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i2.118
A cruciate retaining (CR) total knee arthroplasty (TKA) provides the least constraint of TKA designs by preserving the native posterior cruciate ligament[1]. One of the first CR TKA implants was designed in 1968 and has continued to evolve over the last few decades[2]. Improvements in polyethylene material, component surface metal alloy composition, and overall implant designs have attempted to improve patient satisfaction and TKA implant survival[3]. Despite the overall success, up to 25% of patients can be dissatisfied after undergoing a TKA[4-6]. Patients who are dissatisfied may require revision TKA, which is expected to increase in volume over the next several decades[7].
Bearing surface materials and implant designs have continued to evolve to improve implant survival and patient satisfaction. The development of highly cross-linked polyethylene liners has led to decreased wear and improved TKA survival[8,9]. Moreover, a variety of component surfaces have been developed in an attempt to improve implant wear[10-12]. Cobalt-chrome alloys (CoCr) have traditionally been utilized for TKA femoral components, but different material options have emerged. Titanium nitride is a coating applied to implants by physical vapor deposition aimed at improving the properties of traditional CoCr[13]. Oxidized zirconium (OXINIUMTM; Smith and Nephew, Inc., Memphis, TN) is a surface-modified metal that was introduced in 2004 with the goal of improving implant survival and longevity by decreasing adhesive and abrasive wear[12,14].
Implant design has progressively evolved with an emphasis on improving kinematics to better mimic the native knee. Some of the first TKA designs included hinged designs that fell out of favor due to their high rates of mechanical failure[15]. TKA designs were refined to minimize knee constraint in an attempt to decrease the rates of failure[15]. The CR TKA prosthesis that was assessed in this study was designed to replicate the shape and position of a native knee, especially coronal alignment and joint line obliquity, to aim for improved function of the knee. Smith et al[16] demonstrated that this prosthesis achieved increased posterior femoral rollback and axial rotation when compared to other CR TKA designs[16,17]. Similarly, the prosthesis also demonstrated better rotation flexion and muscle activation during free walking[18].
To our knowledge, sparse research exists that has examined clinical outcomes of a large cohort of patients undergoing a CR TKA utilizing a kinematically designed implant. Moreover, there is no large-scale study to our knowledge assessing patient reported outcome measures (PROMs) in patients with this implant design. Our study aimed to assess mid-term clinical outcomes and PROMs of this kinematically designed CR TKA implant.
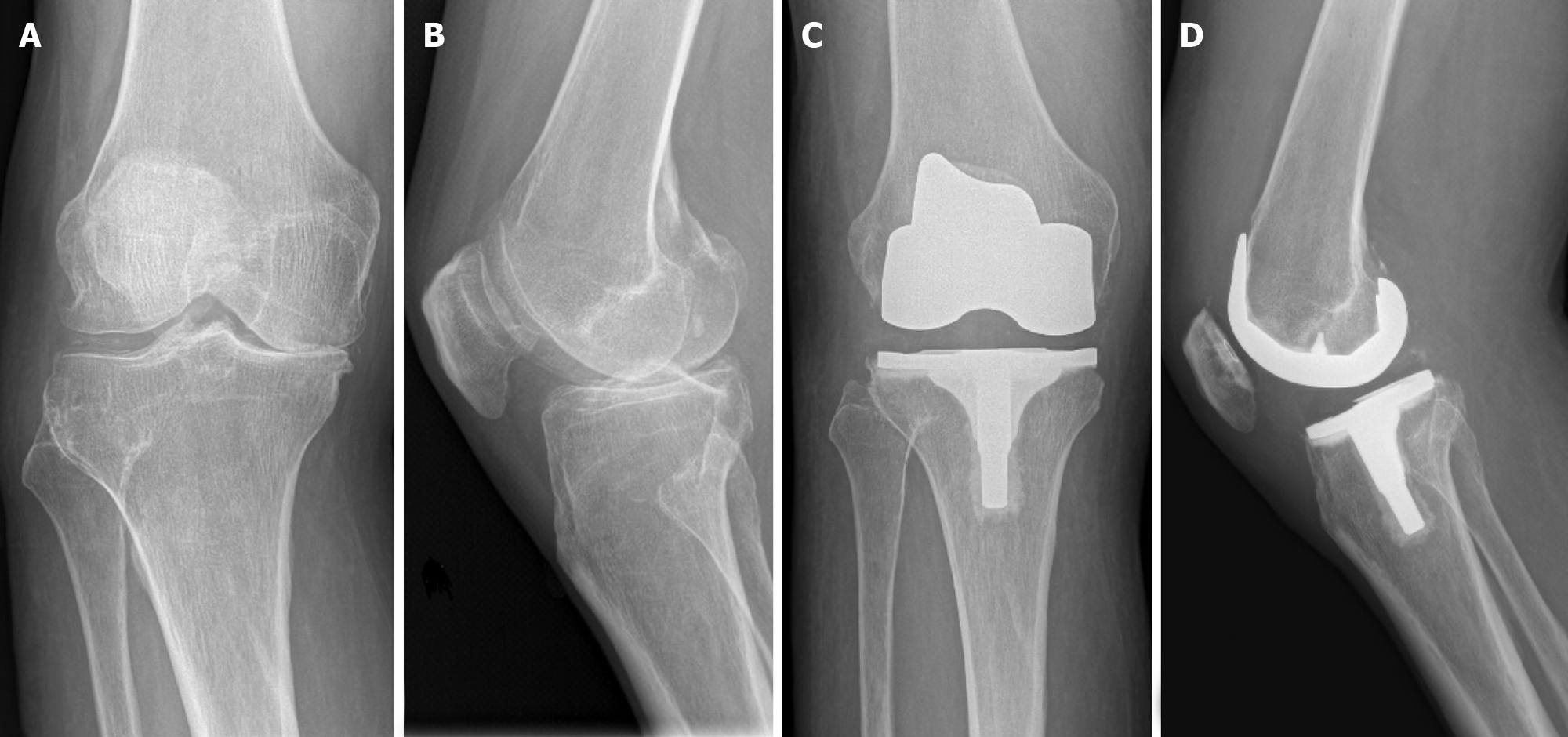
A retrospective, multi-surgeon study was designed to assess this kinematically designed CR Knee System (JOURNEY™ II CR; Smith and Nephew, Inc., Memphis, TN) (Figure 1) at an urban, academic medical institution. Institutional Review Board (IRB) approval was received prior to the initiation of the study. All procedures in this study were performed by fellowship-trained arthroplasty surgeons between 2015 and 2021. Only patients with a minimum of two-years of clinical follow-up with an orthopedic surgeon were included in this study. During the study period, multiple implant systems and designs were utilized for TKA in the authors’ institution. Only patients who received the study CR TKA system were included.
Generally, a standard medial parapatellar approach was utilized when performing a primary TKA on a native knee. After adequate exposure, the tibial and femoral bone cuts were made according to the preoperative planning. Component sizing, femoral bearing surface material (cobalt-chrome or oxidized zirconium), and liner constraint design (standard CR or deep dish) were based on surgeon preference at the time of the procedure.
Patient demographics, surgical information, and outcome data were queried from the institution’s electronic medical record (EPIC Systems, Verona, Wisconsin). Patient demographics included age, sex, race, smoking status, insurance, American Society of Anesthesiologists (ASA) score, body mass index (BMI), Charlson Comorbidity Index (CCI), and primary diagnosis at time of TKA. Surgical information included operative time from skin incision to skin closure, liner and femoral bearing surface type, anesthesia type, and use of technology. Clinical outcome data was collected during routine follow-up visits scheduled at the surgeon’s discretion. Outcome data included length of stay (LOS), discharge disposition, 90-d emergency department (ED) visits, 90-d readmissions, revisions, and PROMs. Revision surgery included any case in which a procedure was performed on the knee of the index procedure due to a complication.
The PROMs collected in the present study included Knee Injury and Osteoarthritis Outcome Score for Joint Replacement (KOOS JR) and Patient-Reported Outcomes Measurement Information System (PROMIS®) scores which are widely used and validated metrics for assessing preoperative and postoperative joint function. The KOOS JR is a 6-item questionnaire which has largely replaced the original 40-item KOOS. The 6-items feature answer choices on a 5-point Likert scale ranging from “None” to “Extreme” and cover domains of pain, function and activities of daily living. The survey asks patients to rate their degree of difficulty with activities such as going up and down stairs, bending to the floor and rising from a sitting position, among others. The summed raw score scales to an interval score between 0 and 100, where a score of 0 represents complete knee disability and a score of 100 indicates perfect knee function.
In addition to KOOS JR scores, PROMIS scores were collected in the present study as the PROMIS item banks can offer a more comprehensive assessment of patient perceptions compared to the joint-specific KOOS JR. PROMIS scores analyzed in the this study were pain intensity, pain interference, mobility, and physical health. PROMIS surveys ask patients on a scale of 1 to 5 to rate how much a particular statement applies to them. For example, on the PROMIS mobility survey, patients are asked to rate how often they experience difficulty when going up or down stairs on a scale of 1 (“Never”) to 5 (“Always”). These individual items are summed up to calculate a raw sum score which is then standardized to a T-score with a mean of 50 and standard deviation of 10. Higher PROMIS functional scores indicate higher levels of ability and higher PROMIS pain scores indicate greater levels of pain. All PROMs scores were collected preoperatively, at six months postoperatively, and at two-years postoperatively.
Averages and ranges or standard deviations were computed for all interval and ratio values including age, BMI, CCI, LOS, operative time, and PROMs. Percentages were computed for all nominal and ordinal variables including sex, race, smoking status, ASA score, insurance status, discharge disposition, ED visit rate, readmission rate, and revision rate. The significance of improvements in mean PROMs scores from preoperative scores to scores collected at six months and two-years postoperatively was analyzed using Independent Samples t-tests. Statistical analysis was done using Microsoft Excel software (Microsoft Corporation, Richmond, WA) and IBM SPSS Statistics (Version 28; IBM Corporation, Armonk, NY). P values less than 0.05 were considered statistically significant.
Of the 255 patients who received the study implant, 65.5% were female, 43.8% were White, and patients had an average age of 60.6 (range, 32 to 83) years. Most patients were never smokers (58.4%), had an ASA score of 2 (58.0%) or 3 (40.0%), and had an average BMI of 33.5 (range, 16.8 to 57.8) kg/m2. Primary osteoarthritis (96.9%) was the most common primary diagnosis (Table 1). The mean surgical time was 105.3 (range, 65 to 237) minutes with 83.5% of patients receiving a standard CR liner and 16.5% receiving a deep-dish CR liner. Most patients received a cobalt-chrome femoral bearing (77.6%) and the rest (22.4%) received an OxiniumTM femoral bearing. Computer-Assisted Navigation was utilized in 34.5% of cases and Robotic-Assisted Surgery was utilized in 3.1% of cases.
| Knees (n = 255) | |
| Sex, n (%) | |
| Male | 88 (34.5) |
| Female | 167 (65.5) |
| Age (yr) [range] | 60.6 [32-83] |
| Race, n (%) | |
| White | 112 (43.9) |
| African American | 63 (24.7) |
| Asian | 10 (3.9) |
| Other | 70 (27.5) |
| Smoking status, n (%) | |
| Current | 14 (5.5) |
| Former | 92 (36.1) |
| Never | 149 (58.4) |
| Insurance status, n (%) | |
| Medicare | 79 (31.0) |
| Medicaid | 32 (12.5) |
| Commercial | 144 (56.5) |
| ASA score, n (%) | |
| 1 | 4 (1.6) |
| 2 | 148 (58.0) |
| 3 | 102 (40.0) |
| 4 | 1 (0.4) |
| BMI (kg/m2) [range] | 33.5 [16.8-57.8] |
| CCI | 3.0 ± 2.2 |
| Primary diagnosis, n (%) | |
| Primary OA | 247 (96.9) |
| Post-Traumatic OA | 7 (2.7) |
| AVN | 1 (0.4) |
Mean LOS postoperatively was 2.1 (range, 0.3 to 19.5) d, and most patients were discharged home (92.5%) (Table 2). Within 90 d, 18 patients (7.1%) presented to the ED with 12 of these patients (4.7%) presenting for orthopedic-related complications. Three patients (1.2%) were readmitted within 90 d due to postoperative complications. One patient was readmitted for a gastric bleed due to non-steroidal anti-inflammatory drug (NSAID) use, one patient was readmitted for an acute kidney injury (AKI), and one patient was readmitted for a periprosthetic joint infection (PJI) (Table 3).
| Knees (n = 255) | |
| Operative time (min) [range] | 105.3 [65-237] |
| Liner, n (%) | |
| Standard | 213 (83.5) |
| Deep dish | 42 (16.5) |
| Anesthesia, n (%) | |
| General | 21 (8.2) |
| Spinal/Regional/Block | 234 (91.8) |
| Bearing surface, n (%) | |
| Oxidized Zirconium-on-Polyethylene | 57 (22.4) |
| Cobalt Chrome-on-Polyethylene | 198 (77.6) |
| Technology, n (%) | |
| Manual | 158 (62.0) |
| Computer navigation | 88 (34.5) |
| Robotic assistance | 9 (3.5) |
| Knees (n = 255) | |
| LOS (days) [range] | 2.1 [0.3-19.5] |
| Time to follow-up (years) [range] | 3.3 [2.1-6.6] |
| Discharge disposition, n (%) | |
| Home | 236 (92.5) |
| SNF | 16 (6.3) |
| ARF | 3 (1.2) |
| 90-d ED visits, n (%) | 18 (7.1) |
| Non-orthopedic related | 6 (2.4) |
| Orthopedic related | 12 (4.7) |
| Knee pain and swelling | 6 |
| Knee pain and erythema | 1 |
| Calf pain and lightheadedness | 1 |
| Groin pain | 1 |
| VTE | 1 |
| NSAID poisoning | 1 |
| Opioid poisoning | 1 |
| 90-d readmissions, n (%) | 3 (1.2) |
| PJI | 1 |
| AKI | 1 |
| Gastric bleed due to NSAID poisoning | 1 |
With mean time to latest follow-up of 3.3 (range, 2.1 to 6.6) years, the cohort exhibited a revision-free survivorship of 98.4%. Four patients (1.6%) required revision TKA surgery, all of which occurred within two-years of the primary TKA. The patient readmitted in the setting of PJI ultimately required multiple revision surgeries to treat the PJI; a debridement, antibiotics, and implant retention (DAIR) procedure was performed during the first readmission followed by a later two-stage revision arthroplasty followed by another DAIR. Additionally, two patients required revision surgery due to arthrofibrosis and one patient required revision surgery due to aseptic femoral loosening. One of the patients with arthrofibrosis received a manipulation under anesthesia four months after TKA and then, two months later, underwent scar resection and a liner exchange maintaining a CR design. The other patient who experienced arthrofibrosis had a revision surgery twelve months postoperatively that exchanged the polyethylene liner and the femoral component. The patient with aseptic femoral loosening underwent a replacement of the polyethylene liner and the femoral component thirteen months postoperatively (Table 4). Four patients (2.0%) out of the 198 patients who received cobalt chrome bearing surface femoral components required revision surgery, whereas none of the 57 patients who received oxidized zirconium bearing surface femoral components required revision (Table 5). Three patients (1.4%) out of the 213 patients who received standard CR polyethylene liners required revision surgery, and one patient (2.4%) of the 42 patients who received deep dish CR polyethylene liners required revision (Table 6).
| Knees (n = 255) | Mean time to revision (years) [range] | |
| Revisions, n (%) | 4 (1.6) | 1.1 [0.7-1.5] |
| Arthrofibrosis | 2 | 1.3 [1.1-1.5] |
| Aseptic femoral loosening | 1 | 1.1 |
| PJI | 1 | 0.7 |
| Cobalt chrome (n = 198) | Oxidized zirconium (n = 57) | |
| Revisions, n (%) | 4 (2.0) | 0 (0) |
| Arthrofibrosis | 2 | 0 |
| Aseptic femoral loosening | 1 | 0 |
| PJI | 1 | 0 |
| Standard (n = 213) | Deep dish (n = 42) | |
| Revisions, n (%) | 3 (1.4) | 1 (2.4) |
| Arthrofibrosis | 1 | 1 |
| Aseptic femoral loosening | 1 | 0 |
| PJI | 1 | 0 |
Compared to preoperative scores, at six months postoperatively there were significant improvements in KOOS JR (43.3 vs 56.5, P < 0.0001), PROMIS Pain Intensity (55.6 vs 50.1, P < 0.0001), PROMIS Pain Interference (65.3 vs 61.4, P < 0.0001), PROMIS Mobility (35.5 vs 38.1, P < 0.0001), and PROMIS Physical Health (39.5 vs 41.8, P = 0.029). At 2 years postoperatively, patients reported further improvements in KOOS JR and all PROMIS measures (Table 7).
| Knees (n = 255) | P value | |
| KOOS JR | ||
| Preoperative | 43.3 (13.0) | |
| 6 mo | 56.5 (16.1) | |
| 2 yr | 62.2 (13.9) | |
| Δ Preop to 6 mo | 13.2 (16.4) | < 0.0001 |
| Δ Preop to 2 yr | 18.9 (16.9) | < 0.0001 |
| PROMIS pain intensity | ||
| Preoperative | 55.6 (6.9) | |
| 6 mo | 50.1 (8.1) | |
| 2 yr | 48.6 (7.6) | |
| Δ Preop to 6 mo | -5.5 (8.2) | < 0.0001 |
| Δ Preop to 2 yr | -7.0 (6.7) | < 0.0001 |
| PROMIS pain interference | ||
| Preoperative | 65.3 (5.7) | |
| 6 mo | 61.4 (8.0) | |
| 2 yr | 59.5 (8.0) | |
| Δ Preop to 6 mo | -3.9 (7.5) | < 0.0001 |
| Δ Preop to 2 yr | -5.8 (6.3) | < 0.0001 |
| PROMIS mobility | ||
| Preoperative | 35.5 (4.1) | |
| 6 mo | 38.1 (4.3) | |
| 2 yr | 40.3 (5.6) | |
| Δ Preop to 6 mo | 2.6 (4.8) | < 0.0001 |
| Δ Preop to 2 yr | 4.8 (3.5) | < 0.0001 |
| PROMIS physical health | ||
| Preoperative | 39.5 (7.3) | |
| 6 mo | 41.8 (6.9) | |
| 2 yr | 42.0 (6.1) | |
| Δ Preop to 6 mo | 2.3 (6.6) | 0.029 |
| Δ Preop to 2 yr | 2.5 (5.4) | 0.045 |
Some of the earliest TKA implants were restrictive, hinged designs that progressively evolved to less restrictive CR TKA designs over the last few decades[15]. The kinematically designed TKA implant, offers a unique asymmetric design intended to replicate the shape and biomechanics of a native knee and reproduces the joint line obliquity. This design allows for improved femoral rollback and knee kinematics compared to other implants[16,18]. Di Benedetto et al[18] performed a pilot study comparing the study implant to a symmetric TKA implant design and demonstrated that the study implant offered better pain resolution, rotational flexion, and muscle activation during free walking[18]. Improved pain control and overall knee strength have been shown to improve the likelihood of home discharges[19]. These factors likely lead to the exceptional rate of home discharges seen in our patient cohort (92.5%) compared to a rate of 85.3% seen in national databases[20].
The implant design and materials utilized in TKA can have a significant influence on complication and revision rates postoperatively. D’Apuzzo et al[21] examined a state-wide database of primary TKA patients and found that there was a 1.8% rate of TKA-specific readmissions within 30 d of surgery[21]. Patients in our study had a 1.2% rate of readmission within 90 d of surgery. Koh et al[22] examined 11134 patients undergoing primary TKA and found that patients had a 1.9% cumulative incidence of revision within two-years. Moreover, their study demonstrated 1.03% of patients required septic revision surgery and 0.86% of patients required aseptic revision surgery[22]. With a mean time to latest follow-up of 3.3 years, our patient cohort had a lower all-cause revision rate of 1.6%, including a 0.4% septic revision rate and a 1.2% aseptic revision rate. Of the three aseptic revisions in the cohort, one was solely a liner exchange while the other two replaced the femoral component in addition to the liner. No tibial or patellar components were replaced in aseptic cases.
Although TKA remains a relatively successful orthopedic procedure, some patients can be dissatisfied after their procedure. Improving patient outcomes may result in decreased revision rates with Robertsson et al[4] demonstrating that patients with unrevised TKAs were comprised of a higher portion of satisfied patients compared to those that required a revision[4]. Our study demonstrated significant improvements in KOOS JR and PROMIS measures at 6 months postoperatively and further improvement at 2 years postoperatively. Similarly, Lutes and Fitch[23] performed a retrospective analysis comparing the studied CR TKA design with a conventional CR TKA design and demonstrated that patients with the kinematically designed TKA implant had significant improvement in short-term functional outcomes[23].
There are several limitations that should be acknowledged in our current study. The use of retrospective data for analysis imparts inherent limitations including data inaccuracies and missing information. Moreover, this study may not be able to appropriately control for confounding factors since it lacks a control group. The generalizability of our results may not be applicable to all patient populations outside of high-volume urban centers. Moreover, if patients received follow-up care such as revisions at other institutions, the data available may not capture these outside encounters. Finally, multiple surgeons were involved in this study, which may introduce heterogeneity into surgical technique and postoperative protocol, possibly influencing patient outcomes. However, most procedures were performed by a single surgeon who utilized computer navigation for mechanical alignment. Tibial cuts were performed in approximately neutral coronal alignment and a posterior femoral referencing guide in approximately 3° of external rotation was used to appropriately size and position the cutting block for the femoral cuts.
Our study demonstrated that the studied kinematically designed cruciate-retaining TKA is an effective implant design offering excellent clinical and patient-reported outcomes with low complication rates. Only four patients required revision surgery resulting in a revision-free survival rate of 98.4% with a mean follow-up time of 3.3 years. The results of our study demonstrate the utility of this kinematically designed implant in the setting of primary TKA.
This study investigates the effectiveness of a specialized knee implant in improving patient outcomes. Focusing on a kinematically designed cruciate retaining (CR) total knee replacement, the research explores its mid-term clinical performance and patient-reported outcomes. It addresses a gap in the existing literature by assessing the implant’s impact on patient satisfaction, functional improvement, and complications, emphasizing the need for comprehensive evaluation of specific implant designs to enhance total knee arthroplasty (TKA) procedures. Every novel implant should be evaluated and early and mid-term reports should be published in order to single out low performing implants and limit the effect on the public.
The research motivation lies in the need to address existing challenges in knee arthroplasty, particularly regarding implant design and patient outcomes. We think it is important to have early and midterm reports of novel implants in order to catch early failures and limit usage of failing implants. Key issues, such as achieving optimal knee functionality, improving patient satisfaction, and minimizing postoperative complications, serve as the primary focus. Solving these problems is critical for advancing the field of orthopedics, guiding future research in enhancing implant technologies, refining surgical techniques, and ultimately enhancing the quality of life for individuals undergoing knee replacement surgeries.
The primary aim was to evaluate the short-term and mid-term clinical outcomes as well as patient-reported outcome measures associated with a kinematically designed CR TKA. Through comprehensive clinical assessments and patient reported outcome measures (PROMs), the study aimed to ascertain the efficacy, functional improvements, and patient satisfaction levels achieved with this specific TKA design. This study is significant in the field of orthopedics because it provides empirical evidence regarding the performance and patient-reported experiences related to this particular kinematic design, thereby informing future TKA approaches and enhancing patient care in the orthopedic field.
In the conducted retrospective study, we analyzed a cohort of patients who had previously undergone CR TKA by collecting clinical and PROMs data from medical records to assess the short-term and mid-term outcomes. While the design of the study is well-established, the CR TKA implant analyzed is a novel, new device that has been introduced within the past decade and with little available published data on outcomes. Thus, this study will greatly assist surgeons who wish to make better-informed risk assessment when selecting this novel implant for their patients. As a result, this study is truly clinically relevant and innovative in the field of total joint arthroplasty.
Postoperative hospital stay averaged 2.1 d and most patients were discharged to home (92.5%). The 90 d emergency department visit rate was 7.1% and 90 d readmission rate was 1.2%. The overall revision-free survivorship rate was 98.4% with an average follow-up of 3.3 years. Significant improvements in patient-reported outcome measures [Knee Injury and Osteoarthritis Outcome Score for Joint Replacement (KOOS JR) and Patient-Reported Outcomes Measurement Information System (PROMIS®) scores] were observed at six months and further improvements at two-years postoperatively, indicating favorable surgical outcomes and patient satisfaction. This study contributes vital real-world data to the field of knee prosthetic design, showcasing a notably high revision-free survivorship rate of 98.4% over a 3.3-year average follow-up. However, challenges persist, notably in reducing the occurrences of complications like periprosthetic joint infections and addressing issues such as arthrofibrosis and aseptic loosening, which demand further investigation and targeted intervention strategies for improved patient care and long-term surgical success.
New theories proposed: The study doesn’t explicitly mention proposing new theories, but it does contribute to the growing body of evidence supporting the effectiveness of kinematically designed CR TKA implants. The findings suggest that this implant design offers favorable clinical outcomes, low complication rates, and notable improvements in PROMs for patients undergoing primary TKA. New methods used: The study employed a retrospective, multi-surgeon design that gathered data from 255 knees over a period from March 2015 to July 2021. The research collected patient demographics, surgical details, clinical outcomes, and PROMs data through electronic medical records. It specifically utilized the KOOS JR and PROMIS® scores to assess patient-reported outcomes. Statistical analysis, including Independent Samples t-tests, was used to determine the significance of improvements in PROMs scores.
Future research in this field should concentrate on extending long-term follow-up beyond the current mean of 3.3 years to evaluate sustained implant performance. A prospective study, tracking patients undergoing CR TKA from preoperative stages through long-term postoperative follow-up, could offer comprehensive insights into its performance, complications, and patient-reported outcomes, further solidifying its efficacy and addressing any evolving concerns in real-time. Comparative studies against existing TKA designs, assessment across diverse patient populations, and investigations into health economics and cost-effectiveness are essential for validating this implant design’s superiority, understanding its efficacy in varied demographics, and informing healthcare decisions. Additionally, biomechanical analyses to comprehend how the implant’s design influences joint mechanics could aid in further optimizing its performance and durability.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Torres RM, Portugal S-Editor: Fan JR L-Editor: A P-Editor: Yuan YY
| 1. | Marya SKS, Singh C. Options and limitations of implant constraint. J Orthop. 2021;23:18-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Richard S, Volatile T. Twelve Years’ Experience with Posterior Cruciate-retaining Total Knee Arthroplasty. Clin Orthop Relat Res. 1986;4. |
| 3. | Wong JM, Khan WS, Chimutengwende-Gordon M, Dowd GS. Recent advances in designs, approaches and materials in total knee replacement: literature review and evidence today. J Perioper Pract. 2011;21:165-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71:262-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 474] [Cited by in RCA: 489] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 5. | Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 738] [Cited by in RCA: 824] [Article Influence: 43.4] [Reference Citation Analysis (0)] |
| 6. | Lau RL, Gandhi R, Mahomed S, Mahomed N. Patient satisfaction after total knee and hip arthroplasty. Clin Geriatr Med. 2012;28:349-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Shichman I, Askew N, Habibi A, Nherera L, Macaulay W, Seyler T, Schwarzkopf R. Projections and Epidemiology of Revision Hip and Knee Arthroplasty in the United States to 2040-2060. Arthroplast Today. 2023;21:101152. |
| 8. | Greenwald AS, Bauer TW, Ries MD; Committee on Biomedical Engineering, Committee on Hip and Knee Arthritis. New polys for old: contribution or caveat? J Bone Joint Surg Am. 2001;83-A Suppl 2:27-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Brown TS, Van Citters DW, Berry DJ, Abdel MP. The use of highly crosslinked polyethylene in total knee arthroplasty. Bone Joint J. 2017;99-B:996-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Breugem SJM, Linnartz J, Sierevelt I, Bruijn JD, Driessen MJM. Evaluation of 1031 primary titanium nitride coated mobile bearing total knee arthroplasties in an orthopedic clinic. World J Orthop. 2017;8:922-928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Kennard E, Scholes SC, Sidaginamale R, Gangadharan R, Weir DJ, Holland J, Deehan D, Joyce TJ. A comparative surface topographical analysis of explanted total knee replacement prostheses: Oxidised zirconium vs cobalt chromium femoral components. Med Eng Phys. 2017;50:59-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Laskin RS. An oxidized Zr ceramic surfaced femoral component for total knee arthroplasty. Clin Orthop Relat Res. 2003;191-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 64] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Wisbey A, Gregson PJ, Tuke M. Application of PVD TiN coating to Co-Cr-Mo based surgical implants. Biomaterials. 1987;8:477-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 45] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Ries MD, Salehi A, Widding K, Hunter G. Polyethylene wear performance of oxidized zirconium and cobalt-chromium knee components under abrasive conditions. J Bone Joint Surg Am. 2002;84-A Suppl 2:129-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 79] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Ranawat AS, Ranawat CS. The history of total knee arthroplasty. The Knee Joint: Surgical Techniques and Strategies. New York: Springer, 2012: 699-707. |
| 16. | Smith LA, Nachtrab J, LaCour M, Cates H, Freeman MG, Komistek RD. In Vivo Knee Kinematics: How Important Are the Roles of Femoral Geometry and the Cruciate Ligaments? J Arthroplasty. 2021;36:1445-1454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A. A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res. 2004;180-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 199] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 18. | Di Benedetto P, Vidi D, Colombo A, Buttironi MM, Cainero V, Causero A. Pre-operative and post-operative kinematic analysis in total knee arthroplasty. A pilot study. Acta Biomed. 2019;90:91-97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 19. | Causey-Upton R, Howell DM, Kitzman PH, Custer MG, Dressler EV. Factors Influencing Discharge Readiness After Total Knee Replacement. Orthop Nurs. 2019;38:6-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | DeMik DE, Carender CN, Glass NA, Callaghan JJ, Bedard NA. More Patients Are Being Discharged Home After Total Knee Arthroplasty, However Rates Vary Between Large Databases. J Arthroplasty. 2021;36:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 21. | D'Apuzzo M, Westrich G, Hidaka C, Jung Pan T, Lyman S. All-Cause Versus Complication-Specific Readmission Following Total Knee Arthroplasty. J Bone Joint Surg Am. 2017;99:1093-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 22. | Koh CK, Zeng I, Ravi S, Zhu M, Vince KG, Young SW. Periprosthetic Joint Infection Is the Main Cause of Failure for Modern Knee Arthroplasty: An Analysis of 11,134 Knees. Clin Orthop Relat Res. 2017;475:2194-2201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 235] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 23. | Lutes W, Fitch D. Comparison of functional outcomes following total knee arthroplasty with a conventional implant design or one designed to mimic natural knee kinematics. Presented at: 39th SICOT Orthopaedic World Congress; 2018 Oct 10-13; Montreal, Canada. Available from: https://www.sicot.org/montreal. |